
INFECTIONS OF THE NERVOUS SYSTEM
• Nervous system infections are classified upon the location of the infection
into
1. Meningitis(infection of the meninges)
2. Encephalitis(infection of the parenchyma of the brain)
3. Brain abscess and subdural empyema
• The meningitic syndrome is simple triad: headache, neck stiffness and
fever. Photophobia and vomiting are often present. In acute bacterial
infection there is usually intense malaise, fever, rigors, severe headache,
photophobia and vomiting. This develops within hours or minutes. The
patient is irritable and often prefers to lie still. Neck stiffness and positive
Kernig's sign usually appear within hours.
VIRAL MENINGITIS
• Viral infection is the most common cause of meningitis, and usually results
in a benign and self-limiting illness requiring no specific therapy.
• A number of viruses can cause meningitis the most common being
enteroviruses.
• The condition occurs mainly in children or young adults.
• Characterized by acute onset of headache and irritability and the rapid
development of meningism.
• The CSF usually contains an excess of lymphocytes, normal glucose and
the protein level may be raised.
•
Treatment is symptomatic; the condition is usually benign and self-limiting.
Recovery usually occurs within days.
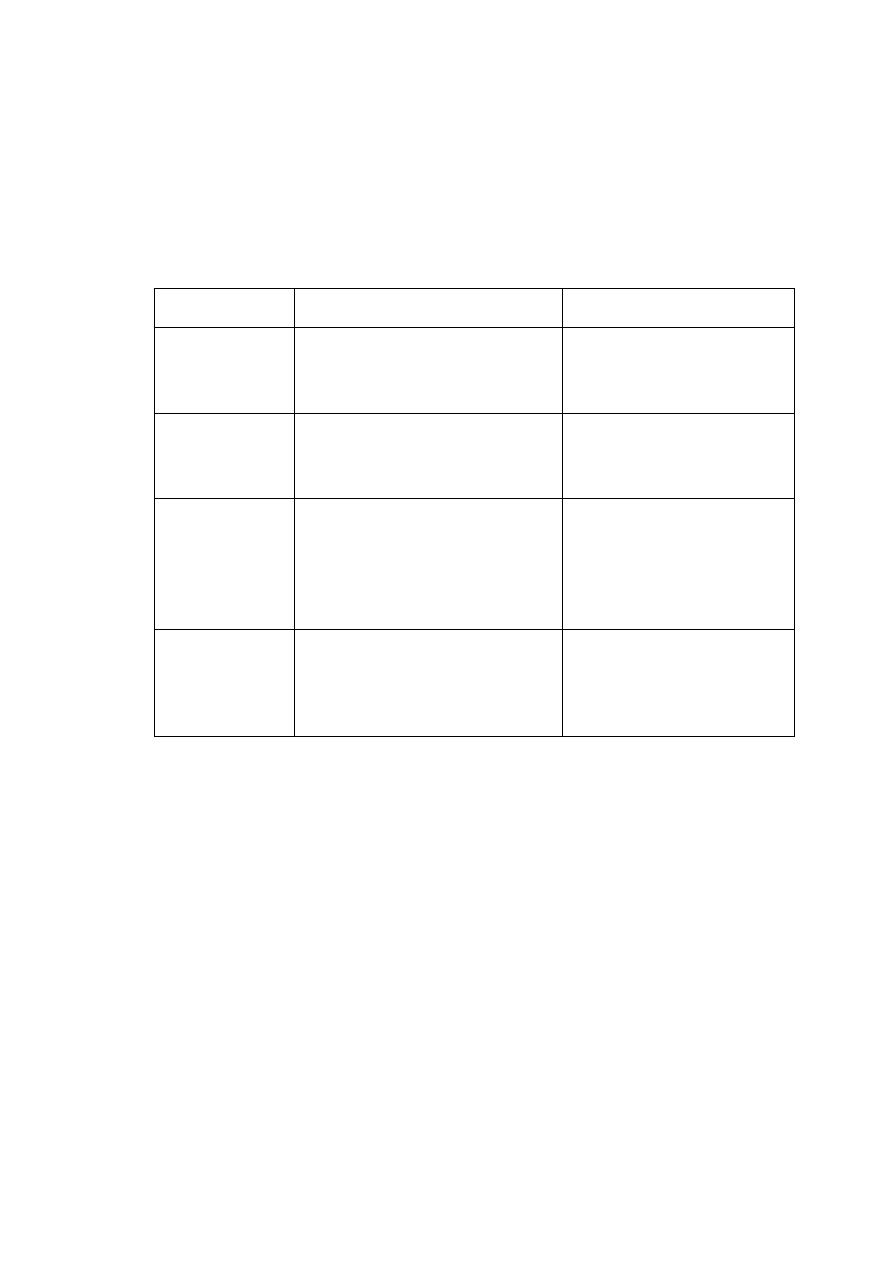
PYOGENIC BACTERIAL MENINGITIS
•
Many bacteria can cause meningitis
.
Age of onset
Common
Less common
Neonate
Gram-negative bacilli (Escherichia
coli, Proteus etc.)
Group B streptococci
Listeria monocytogenes
Pre-school child
Haemophilus influenzae
Mycobacterium tuberculosis
Neisseria meningitidis
Streptococcus pneumoniae
Older child and
adult
Neisseria meningitidis
Streptococcus pneumoniae
Listeria monocytogenes
Mycobacterium tuberculosis
staphylococcus aureus (skull
fracture)
Haemophilus influenzae
elderly
Streptococcus pneumoniae
Neisseria meningitidis
Gram-negative bacilli
Listeria monocytogenes
• Streptococcus pneumoniae is the most common cause of bacterial
meningitis, followed by Neisseria meningitidis.
• The meningococcus and other common causes of meningitis are normal
commensals of the upper respiratory tract. New and potentially pathogenic
strains are acquired by the air-borne route, but close contact is necessary.
• The organism invades through the nasopharynx, producing septicemia
that is usually associated with pyogenic meningitis.
• In pneumococcal and Haemophilus infections there may be an associated
otitis media. Pneumococcal meningitis may be associated with pneumonia
and occurs especially in older patients and alcoholics, as well as those
with asplenia.
• Listeria monocytogenes can cause meningitis
in the immunosuppressed,
diabetics, alcoholics, pregnant women, as well as in
the extremes of age.
Clinical features
•
Headache, drowsiness, fever and neck stiffness are the usual presenting
features
.
• In severe bacterial meningitis the patient may be comatose and later there
may be focal neurological signs.
• Meningococcal meningitis may be associated with a purpuric rash.
Investigations:
Symptoms& signs of meningitis
↓
Blood culture, throat swab
↓
Empirical antibiotics
↓
Brain CT scan to exclude space occupying lesions
↓
Lumbar puncture
• In bacterial meningitis the CSF is cloudy (turbid) due to the presence of
many neutrophils, so called septic meningitis.
• Gram stain and culture of CSF may allow identification of the organism.
• Polymerase chain reaction (PCR) techniques can be used on both blood
and CSF to identify bacterial DNA.
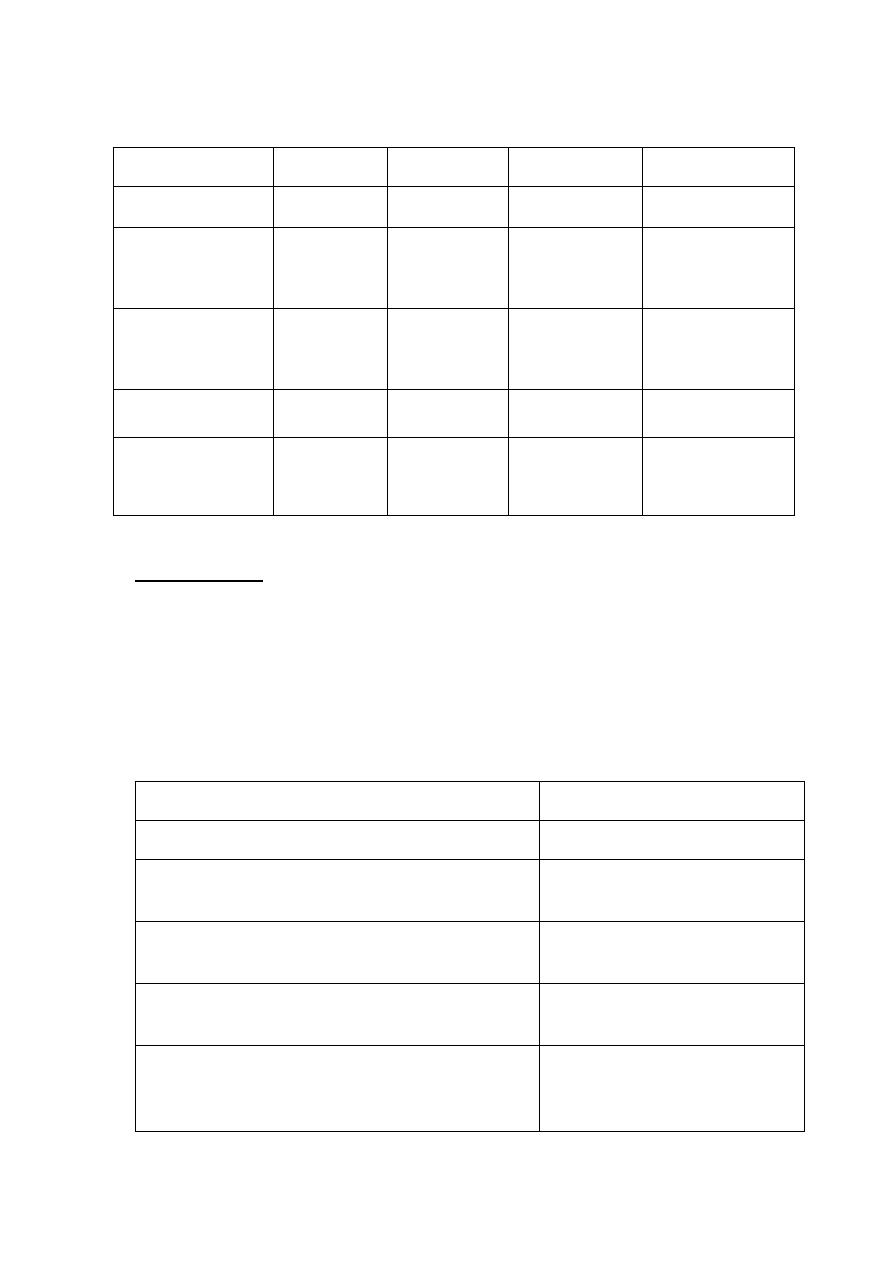
CSF character
Normal
Viral
Pyogenic
Tuberculosis
Appearance
Crystal-clear Clear/turbid Turbid/purulent
Turbid/viscous
Mononuclear cells
(Lymphocyte)
< 5/ mm
3
10-100/ mm
3
< 50 mm
3
100-300 mm
3
Polymorph cells
(neutrophil)
Nil
Nil
200-300/mm
3
0-200/mm
3
Protein
0.2-0.4 g/L
0.4-0.8 g/L
0.5-2.0 g/L
0.5-3.0 g/L
Glucose
≥ 60% blood
glucose
≥ 60% blood
glucose
< 60% blood
glucose
< 60% blood
glucose
Management:
• If bacterial meningitis is suspected, parenteral (i.v.) empirical antibiotics
should be given
immediately before the cause of meningitis is known.
Antibiotics Used in Empirical Therapy of Bacterial Meningitis
Indication
Antibiotic
Preterm infants to infants <1 month
Ampicillin + cefotaxime
Infants 1–3 mos
Ampicillin + cefotaxime or
ceftriaxone
Immunocompetent children >3 mos and adults <55
Cefotaxime or ceftriaxone +
vancomycin
Adults >55 and adults of any age with alcoholism or other
debilitating illnesses
Ampicillin + cefotaxime or
ceftriaxone + vancomycin
Hospital-acquired meningitis, posttraumatic or
postneurosurgery meningitis, neutropenic patients, or
patients with impaired cell-mediated immunity
Ampicillin + ceftazidime +
vancomycin
Patients with a clear history of anaphylaxis to
β-lactams
Chloramphenicol 25 mg/kg
i.v. 6-hourly
plus
Vancomycin 1 g i.v. 12-hourly
• The antibiotic regimen may be modified after identifying the infecting
organism.
• Duration of antibiotic treatment depends on the infecting organism, but
usually for 2-3 weeks.
•
Adjunctive corticosteroid therapy is useful in both children and adults.
Dexamethasone (10 mg intravenously) should be
administered 20 min
before or concurrent with the first dose of antibiotics and the same dose is
repeated every 6 h for 4 days.
• Household and other close contacts of patients with meningococcal
infections, especially children, should be given 2 days of oral rifampicin
(age 3-12 months 5 mg/kg 12-hourly, > 1 year 10 mg/kg 12-hourly, and
adults 600 mg 12-hourly). In adults, a single dose of 500 mg of
ciprofloxacin is an alternative.
Prognosis:
In general, the risk of death from bacterial meningitis increases with
(1) decreased level of consciousness on admission,
(2) Onset of seizures within 24 h of admission,
(3) Signs of increased ICP
(4) Young age (infancy) and age >50
(5) Delay in the initiation of treatment.
(6)Decreased CSF glucose concentration (<40 mg/dL)
(7) Markedly increased CSF protein concentration (>300 mg/dL)
CHRONIC MENINGITIS
Chronic meningitis is most commonly diagnosed when meningitic
syndrome exists for > 4 weeks and is associated with a persistent
inflammatory response in the (CSF). Causes include:
1-meningeal infections (e.g. TB, brucella, fungal).
2-malignancy (carcinomatous, leukemic)
3-noninfectious inflammatory disorders (sarcoidosis, SLE)
4-chemical meningitis (drugs)
5-parameningeal infections (otitis media, mastoiditis)
TUBERCULOUS MENINGITIS
• Tuberculous meningitis remains common in developing countries and is
seen as a secondary infection in patients with AIDS.
• Occurs most commonly shortly after a primary infection in childhood or as
part of miliary tuberculosis.
• The usual local source of infection is a caseous focus in the meninges or
brain substance adjacent to the CSF pathway.
• The brain is covered by greenish, gelatinous exudates, especially around
the base of the brain.
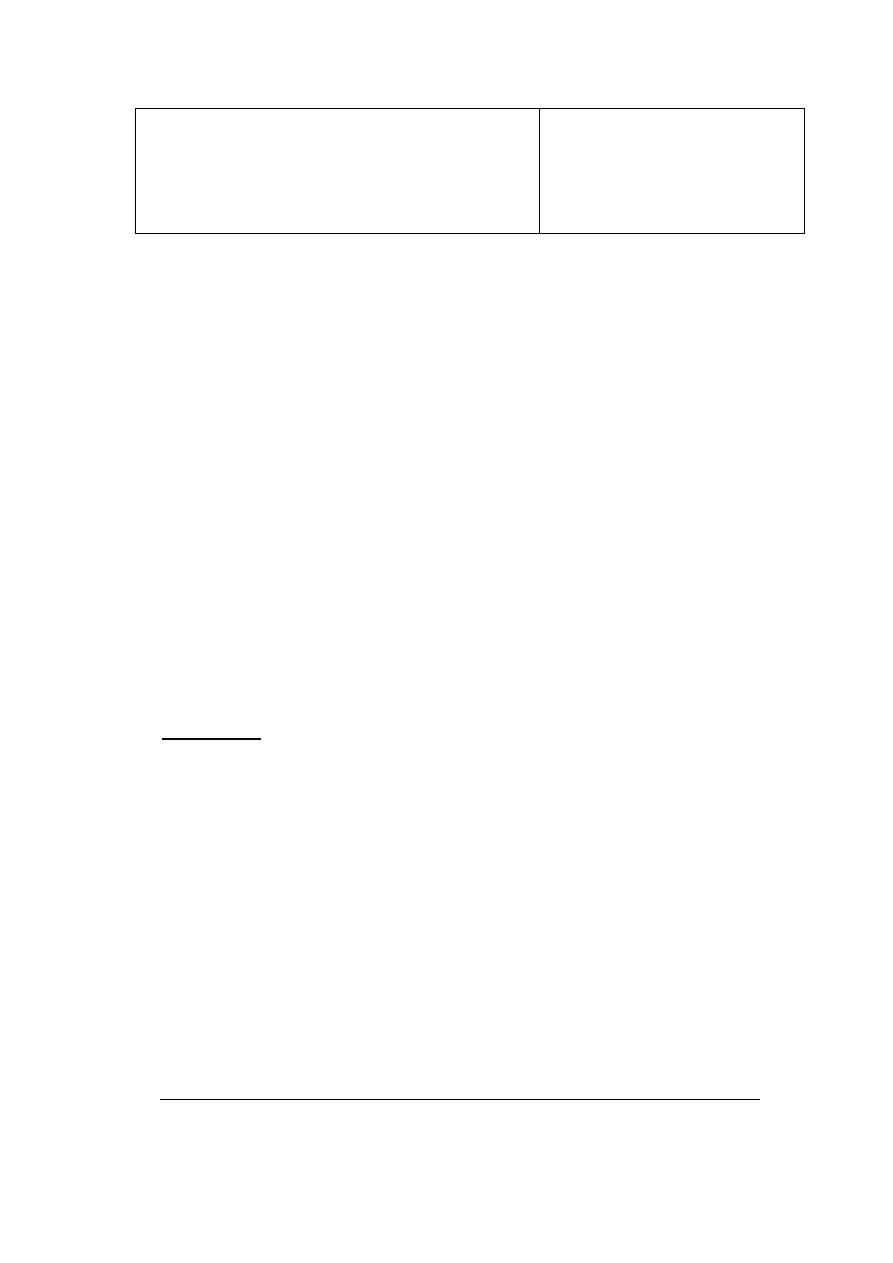
Clinical features of tuberculous meningitis:
Symptoms Signs
•
Headache Meningism
•
Vomiting Oculomotor palsies
•
Low-grade fever Papilloedema
•
Lassitude Focal hemisphere signs
•
Confusion Depression of conscious level
•
Behaviour changes
Investigations
•
Brain CT to exclude SOL. It may show hydrocephalus, tuberculoma.
•
CSF study: high CSF pressure, CSF is clear but, when allowed to stand, a
fine clot ('spider web') may form, up to 5 × 10
8
cells/litre, predominantly
lymphocytes, a rise in protein and a marked fall in glucose. AFB may be
positive in CSF smear.
•
Chest X-ray to exclude pulmonary TB.
Management
•
As soon as the diagnosis is made or strongly suspected, chemotherapy
should be started.
•
Initial therapy is a combination of isoniazid (300 mg/d), rifampin (10 mg/kg
per day), pyrazinamide (30 mg/kg per day in divided doses), ethambutol
(15–25 mg/kg per day in divided doses), and pyridoxine (50 mg/d). If the
clinical response is good, pyrazinamide and ethambutol can be
discontinued after 8 weeks and isoniazid and rifampin continued alone for
the next 6–12 months.
•
Adjunctive therapy with corticosteroid can be used for several weeks.
•
Surgical ventricular drainage may be needed if obstructive hydrocephalus
develops.
VIRAL ENCEPHALITIS
• Encephalitis is infection of the substance of the nervous system (mostly
the brain) producing symptoms of focal dysfunction (focal deficits and/or
seizures) with general signs of infection.
• Viruses are the most common cause.
• The most serious cause of viral encephalitis is herpes simplex which
probably reaches the brain via the olfactory nerves.
• In herpes simplex encephalitis, the temporal lobes are usually primarily
affected.
Clinical features:
• Acute onset of headache, fever with or without meningism.
• focal neurological signs (aphasia and/or hemiplegia) and seizures (focal or
generalized)
• Disturbance of consciousness ranging from drowsiness to deep coma, or
confusion.
Investigations:
• Brain CT scan
may show low-density lesions in the temporal lobes.
• MRI is more sensitive in detecting early abnormalities.
• Lumbar puncture
:
The CSF usually contains excess lymphocytes,
protein
content may be elevated but the glucose is normal.
Occasionally, the CSF
is normal.
• PCR is necessary for detection of CSF.
• The EEG is usually abnormal in the early stages.
Management:
• Herpes simplex encephalitis responds to acyclovir 10 mg/kg i.v. 8-hourly
for 2-3 weeks. This should be given early to all patients suspected of
suffering from viral encephalitis.
• Anticonvulsant treatment is often necessary.
• Raised intracranial pressure is treated with dexamethasone 8 mg 12-
hourly.
Prognosis:
Even with optimum treatment, mortality is 10-30% and significant proportions
of survivors have residual epilepsy or cognitive impairment.
