م هللاْسِب
الرحمن الرحيم

Specific
Neurological
Infections

Tetanus
Epidemiology:
1 per million per year in the US
Not uncommon in developing countries
Cause:
Clostridium tetani ( G+ve rods, anaerobe, spore forming)
a commensal in the gut of humans and domestic animals.
Habitat
: heat and anti-septic –resistant spores in soil (mainly
through fecal material of animals, and human!; and human
reservoir
Entry to human body
; in anaerobic conditions like T. necrosis,
spores form bacteria which produce exotoxin
• Tetanus is often associated with
,
especially rusty nails. Although rust itself does
not cause tetanus, objects that accumulate
rust are often found outdoors or in places that
harbor anaerobic bacteria.
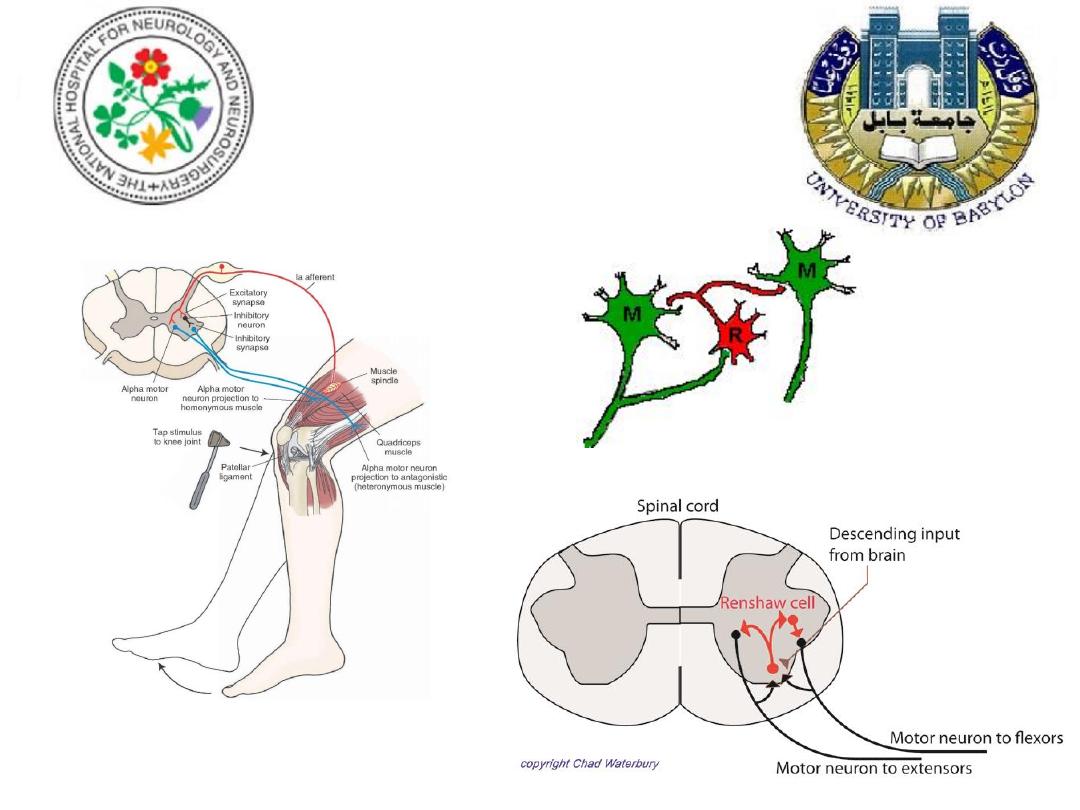
Pathophysiology
Exotoxin: tetano-spasmin
Blood-borne transport to local motor endplate
Retrograde axonal transport to CNS
Sites of action:
• Spinal cord and brainstem inhibitory neuron
( Renshaw cells)

Clinical features
Incubation period: 1-2 days to 1 month
Types:
Localized: benign course, resolution with no
residual effects, check for recruiting spasm and lock
jaw
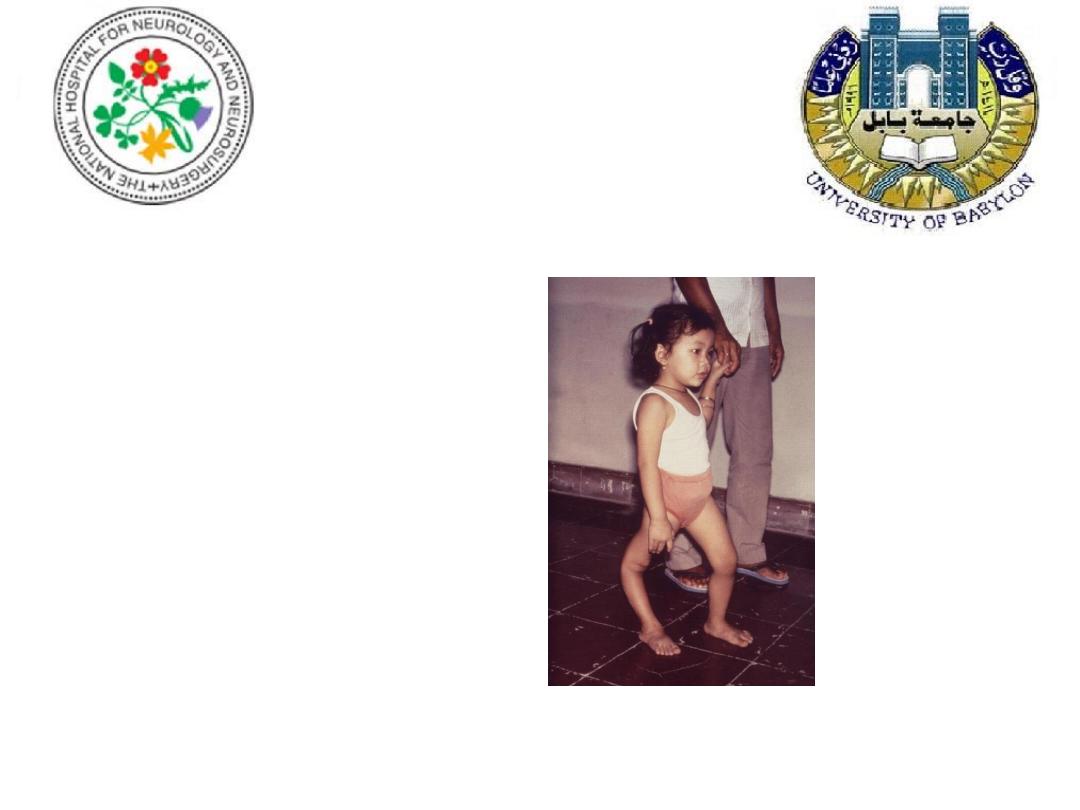
Generalized: severe, mild fever, neck stiffness, then
bulbar involvement then limb & trunk; can be seen
in neonates (
tetanus neonatorum
)
Cephalic: bulbar and facial weakness and spasms,
worst prognosis

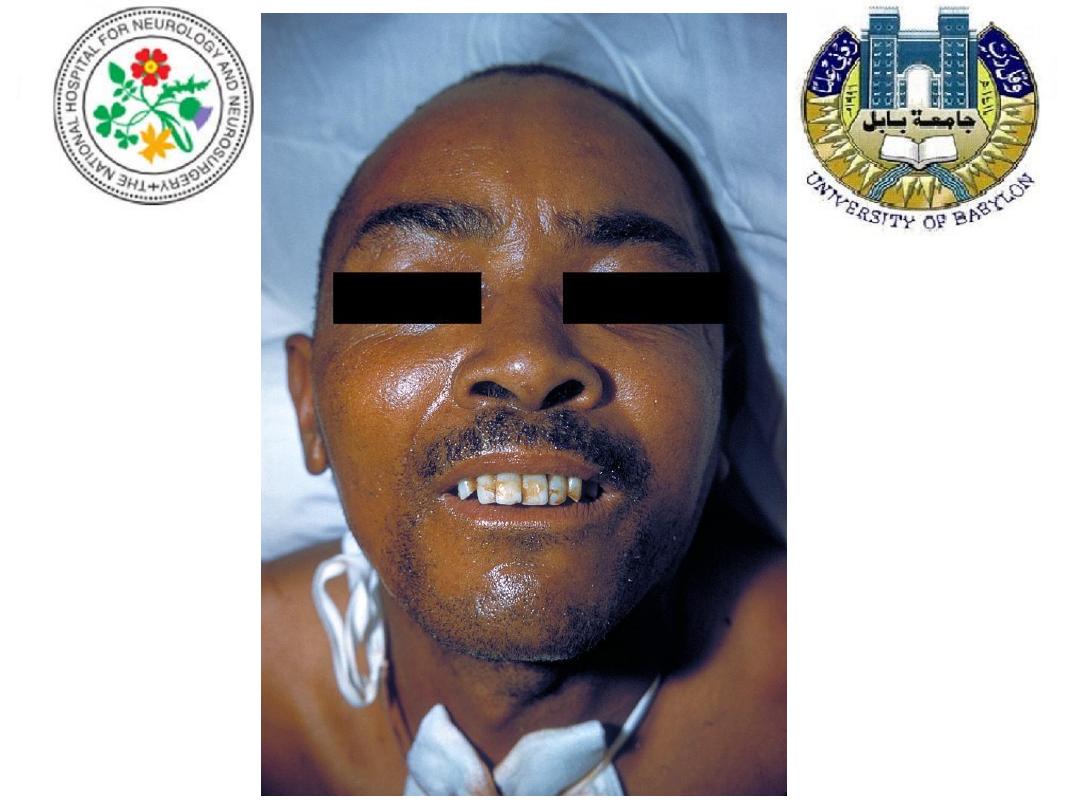
Risus sardonicus
( L: a sarcastic laugh)
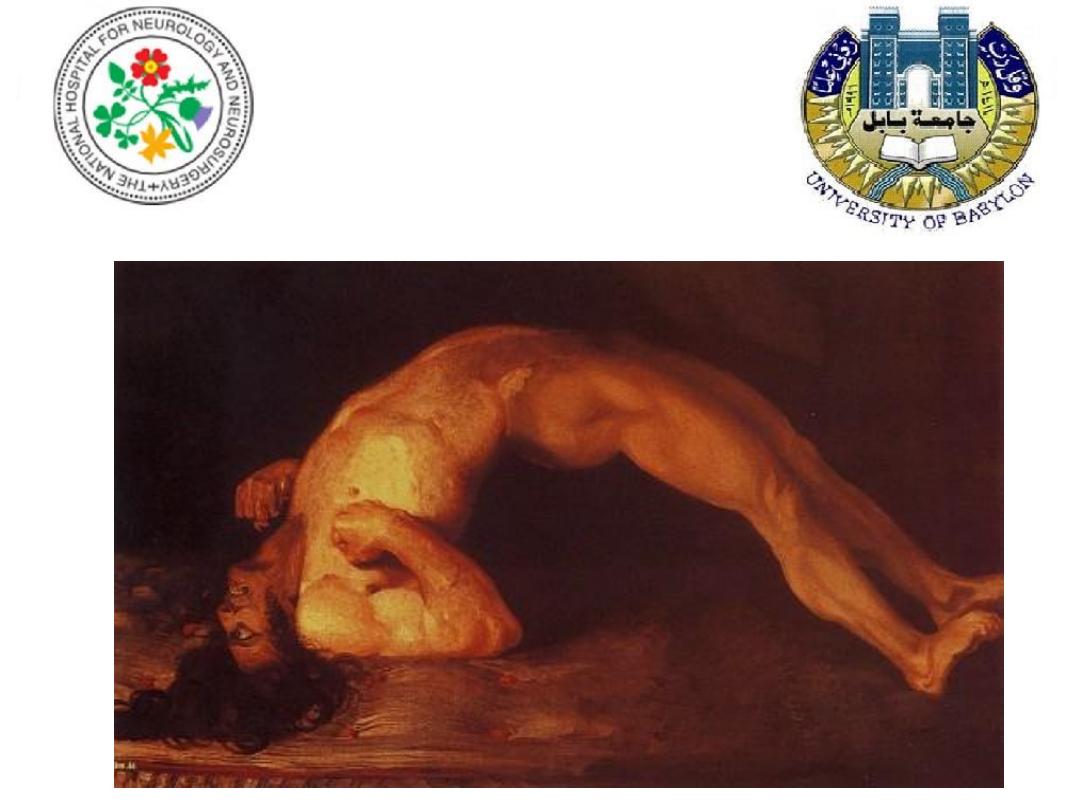
opsithotonus

In the severe cases, violent spasms lasting for few
seconds to 3-4 minutes occur spontaneously , or
may be induced by stimuli such as movement or
noises
Spasms are painful and exhausting

Diagnosis
A clinical one!
Organism rarely isolable by the time of
presentation.
Hx of injury; dirty wounds

Causes of death
• Laryngospasm, apnea
• Heart failure, arrhythmia
• Shock
• Aspiration pneumonia

Treatment
•Immediate measures
•Antitoxin (3000-6000 units, IV )
•Antibiotic (Penicillin, metronidazole or
tetracycline , 10 day course)
•Nurse in quiet dark room
•Debridement of wound, Rx of secondary
infections
•ICU nursing ( environment, tracheostomy)
•muscle relaxants like diazepam, phenobarbitone

Prevention
Active immunization (DTP); 3 doses; routine in Iraq
Every 10 years, a booster should be administered
Toxoid is indicated in
• moderate/high risk wounds when patient hasn’t
received a booster in the last 5 years
• any open wounds when patient hasn’t received a
booster within last 10 years
Patients with moderate/high wounds should receive IM
anti-toxin

Summary
The only vaccine preventable disease that is
infectious but not contagious!
Mortality : 50%,
tetanus neonatorum :100% in developing
countries
Good prognosis:
Localized, early treatment

Rabies
Latin: madness, fury, rage

Rabies
A zonoosis
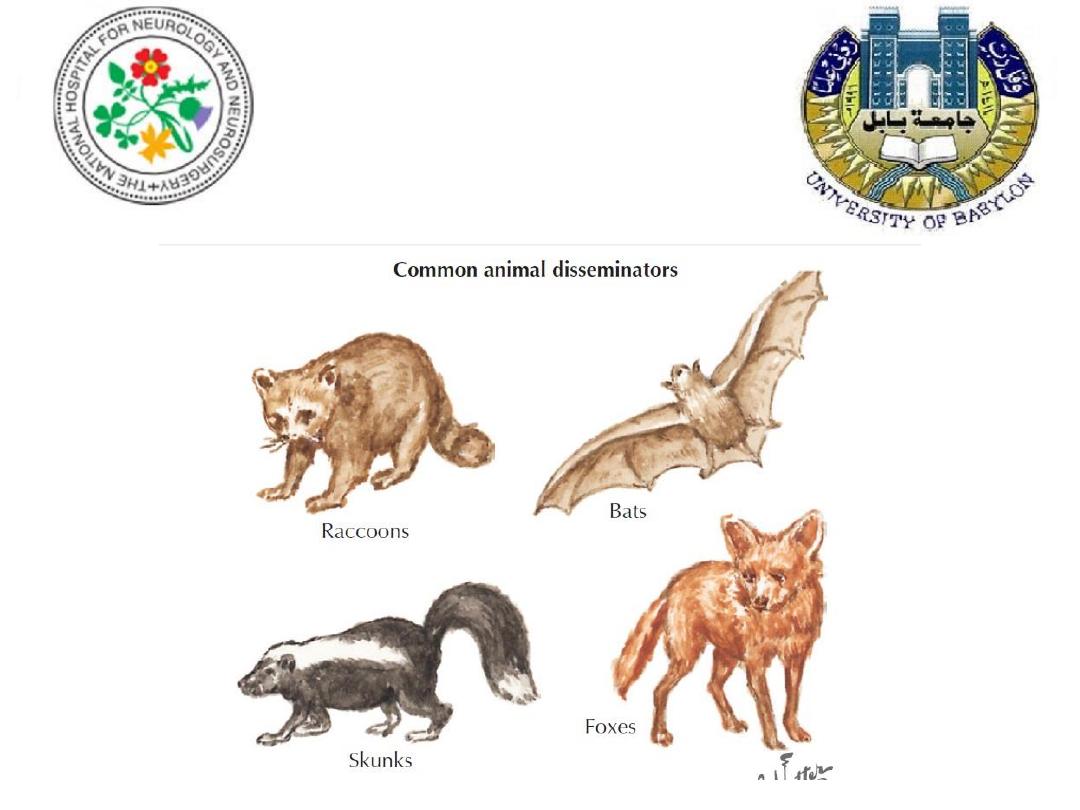
Maintenace hosts
wild: fox, raccoons, skunks, bats
Domestic: dogs, cats
Still common in developing countries
Mode of transmission
• Saliva ( bites, licks of broken skin or mucus
membrane)
• Iatrogenic (corneal transplants)

Aetiology
Pathophysiology
Causative agent: RNA virus, a Rhabdovirus
Retrograde axonal transport to CNS
Targets of infection: CNS( brainstem) and salivary
glands
Pathology:
• Rhombencephalitis
•
Negri bodies (hippocampus, Purkinji cells)

Clinical features
Incubation period: 4-8 weeks, as minimum as 9 days (multiple, necks,
face, scalp bites)
History of bite
Prodrome: fever, headache, parasthaesia around bite (characteristic)
Encephalitis versus paralytic phenotypes:
Furious/ rabid/ encephalitic rabies
: agitation, confusion, seizures,
insomnia, hallucinations, characteristic hydrophobia
Paralytic/ dumb
rabies: severe weakness, preserved sensorium
Coma
Death (100% of clinically evident cases) usually within 7 days of onset
of symptoms

Management
Diagnosis: a clinical one
PCR ( CSF, hair follicle, corneal smear preparation)
Post mortem examination for confirmation
What to do in established case?
Really nothing
Treatment is supportive and palliative,
isolation
Intensive care setting
Prevention
Wound washing with soap and benzyl ammonium chloride
Post-exposure:
Active: HDCV 1 ml IM, on day 0,3,7,14,28 (30), (90)
Passive: HRIG 20U/kg ½ IM, ½ infiltration around wound
If HRIG is not available, 0.1 ml of HDCV ID at 8 sites on day 1,
single boosters on day 7 & 28
If no human products available, observe the animal for 10 days
or euthanize if S&S of rabies!
Pre-exposure prophylaxis: HDCV 0.1 ml, two IM injections
Poliomyelitis
Greek: Polio: gray; Myelin: marrow
18
th
Dynasty
1403 - 1365 BC
Egypt

Poliomyelitis
Causative agent: 3 polioviruses….Enteroviridae.
( RNA viruses)
Mode of transmission: faeco-oral
Epidemiology: 3 countries are currently still
endemic ( Afghanistan, Pakistan and Nigeria),
reduced reports, from 350,000 cases in 1988 to
only 233 in 2012
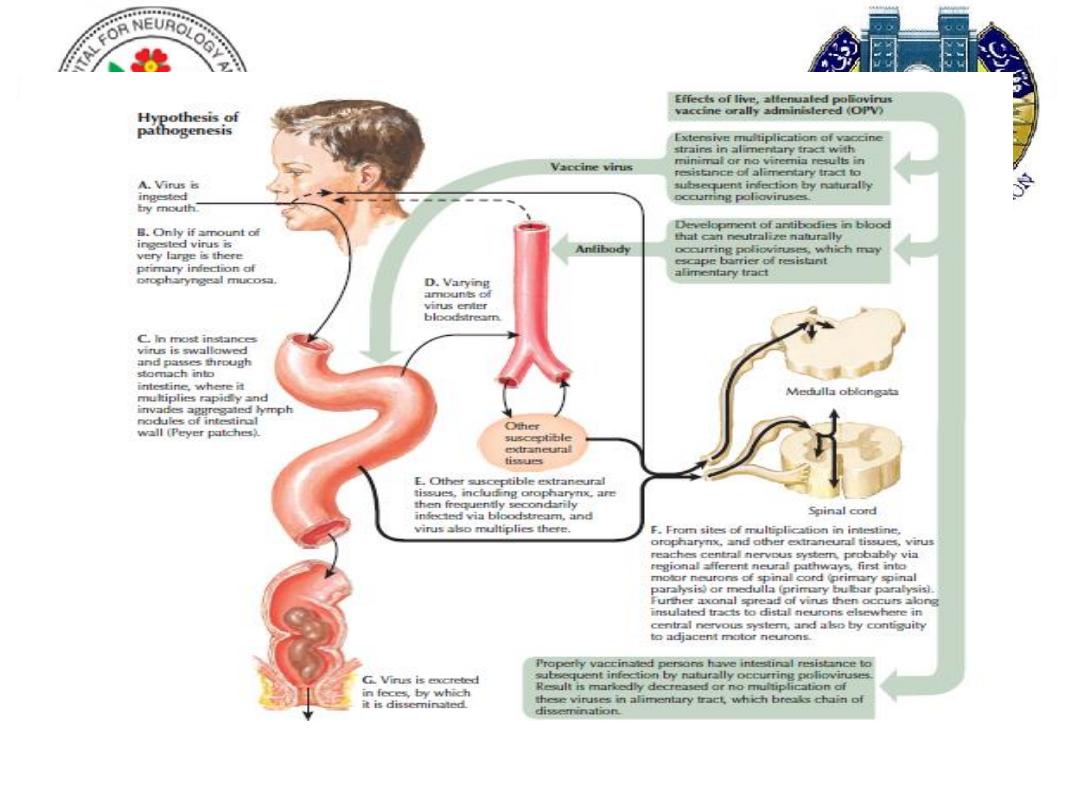
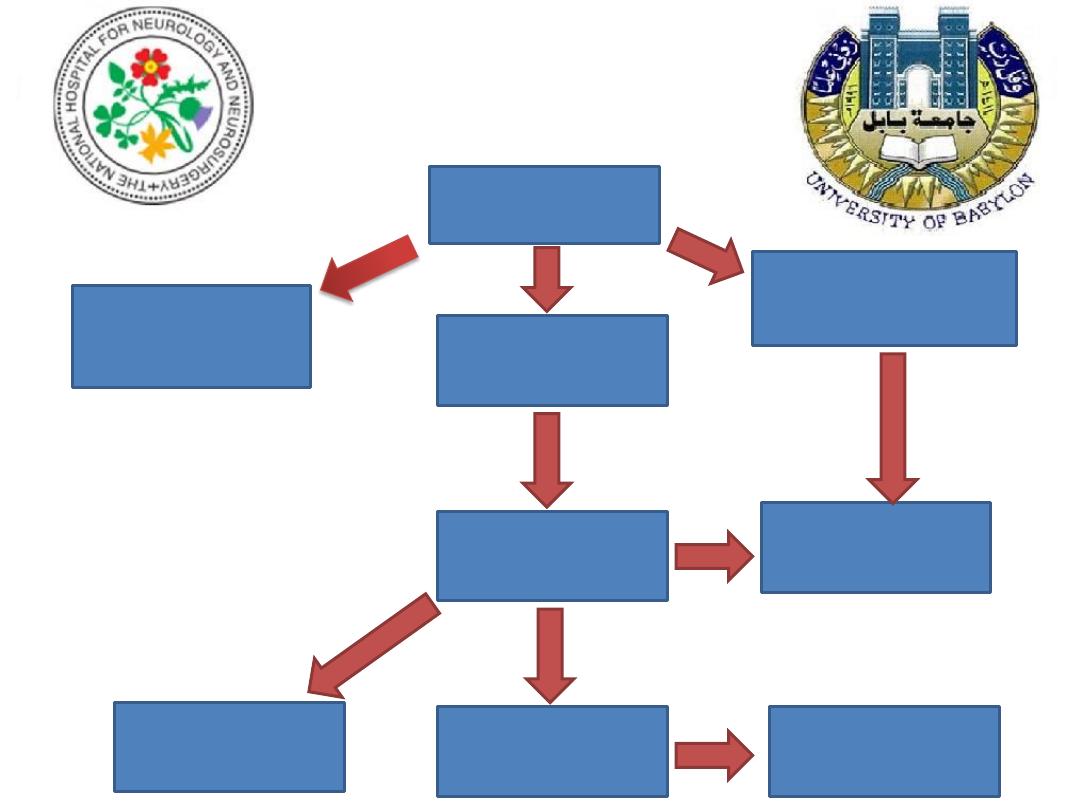
infection
Inapparent polio
90-95%
Abortive polio
4-8%
(minor febrile illness)
Aseptic meningitis
(1-2%)
recovery
Paralytic polio
(0.5%)
Recovery with
residual deficit
Death
5-10% of
paralysed
Post-polio
syndrome

Clinical features
Incubation period: 3-35 days, average 6-20 days
Pre-paralytic: pharyngitis, headache, fever, muscle aches,
tenderness
Paralysis: peaks with maximal fever, within 24-48 hours, doesn’t
progress when fever is settled for two days, asymmetrical,
proximal, lower limbs mainly flaccid weakness (injection, physical
activity are risk factors)
Wasting apparent after 3 weeks, maximal by 12-16 weeks
Three phenotypes:
Spinal(79%);Bulbar( 2%); Bulbospinal (19%)
Management
Diagnosis:
Isolation of virus from stool or pharynx
Rarely isolable from CSF!
CSF examination: lymphocytic pleocytosis
Treatment:
Supportive: avoid IM injection, exercise.
Prevention:
Sabin vaccine (OPV) live attenuated, (herd immunity),
Salk (IPV)

prognosis
Mortality due to respiratory failure, autonomic
dyregulation
• Children: 2-5%
• Adults: 15-30%
• Bulbar polio: 25-75%!!!
Differential diagnosis
• Guillian Barre’ syndrome (AIDP)
• Polio-like syndromes: Coxsackie A &B, Japanese encephalitis
West Nile virus

Subacute sclerosing panencephalitis
Rare progressive and eventually fatal illness
Is a complication of measles
May develop many years after the primary measles
Intellectual deterioration, apathy followed by
myoclonic jerks, rigidity and dementia
Antiviral therapy is ineffective

Prion diseases
Prions are unique amongst infectious agents in that
they’re devoid of any nucleic acid.
PrP
c
normal protein To abnormal PrP
sc
Accumulation of
PrP
sc causes a transmissible spongiform encephalopathy
Human prion diseases are characterized by the histopathological triad of cortical
spongiform change, neuronal loss and gliosis.

Creutzfeldt-Jakob disease
Is a human prion disease
10% due to mutation in the gene coding for prion protein
Middle age and elderly
Rapid progressive dementia, myoclonus, ataxia and visual
disturbance
Characteristic EEG abnormality
No treatment