
Behçet
SYNDROME
By
Dr. Arwa Hamdan Al-Badran&ali alkazzaz
3/16/2020

Syndrome or Disease?
• Some experts felt a designation of ‘syndrome’
was more accurate for Behçet’s disease, actually
a constellation of symptoms.
• The presence of geographic differences in disease
expression, symptom clusters and differences in
drug response between different types of organ
involvement support this contention.
• An online vote was held which favored this
notion.
3/16/2020
Definition
• Behçet disease is a chronic systemic
vasculitic disorder that is characterized
by a triple-symptom complex of
recurrent
, genital
.
3/16/2020

Aetiology and pathogenesis
• Unknown aetiology.
It is reasonable to consider Behçet
syndrome as a polygenic autoinflammatory
disease .
Both genetic background and
environmental factors are thought to be
associated with the development and
progression of the disease.
3/16/2020

MHC-1-pathy
• Some of the inflammatory pathways
operative in the ankylosing spondylitis (AS)
and psoriatic arthritis (PsA), eg the IL-10 and
IL-23–IL-17 pathways, have also been
observed in Behçet syndrome.
• Acne and arthritis commonly occur in
patients with Behçet syndrome and these
patients also commonly have enthesitis,
which is a phenotypic feature related to the
SpA.
Remmers EF.
Nat. Genet. 42, 698–702 (2010)
Hatemi G.
Arthritis Rheum. 58, 1539–1545 (2008)
3/16/2020

A
microbial trigger?
• Mutations in FUT2, (fucosyltransferase 2) present in
intestinal and oral epithelial cells, reported in BS.
• This is also reported in Crohn’s disease.
• Epithelial α1,2-fucose molecules formed by the enzymatic
action of FUT 2 are important to bacterial symbiosis in the
gut and also form a barrier against pathogenic bacteria.
• Mutations in FUT2 impair this barrier.
• Infectious agents, such as
Streptococcus sanguis
,
Herpes
simplex virus, hepatitis viruses, and parvovirus B19 have
been implicated as causes of Behçet’s disease
3/16/2020

• The frequency of HLA-B*51 is
~60% even in areas where Behçet
syndrome is endemic.
• It is much lower in other regions.
• This frequency implies the HLA
B*51 association cannot wholly
explain BS.
• Becatti M.
Circulation 133, 302–311 (2015)
3/16/2020

Epidemiology
• (Silk Route disease) because of its frequency in
the Middle East and far-east Asia (endemic).
• ? Rare among blacks.
• The usual age of onset is between the second and
fourth decades. Younger patients (age of onset
≤24 years) have a higher prevalence of eye
disease and total clinical activity than older
patients (age of onset ≥25 years).
• The disease is more common in females in Asian
countries, while the opposite is true in the
Mediterranean population
.
3/16/2020
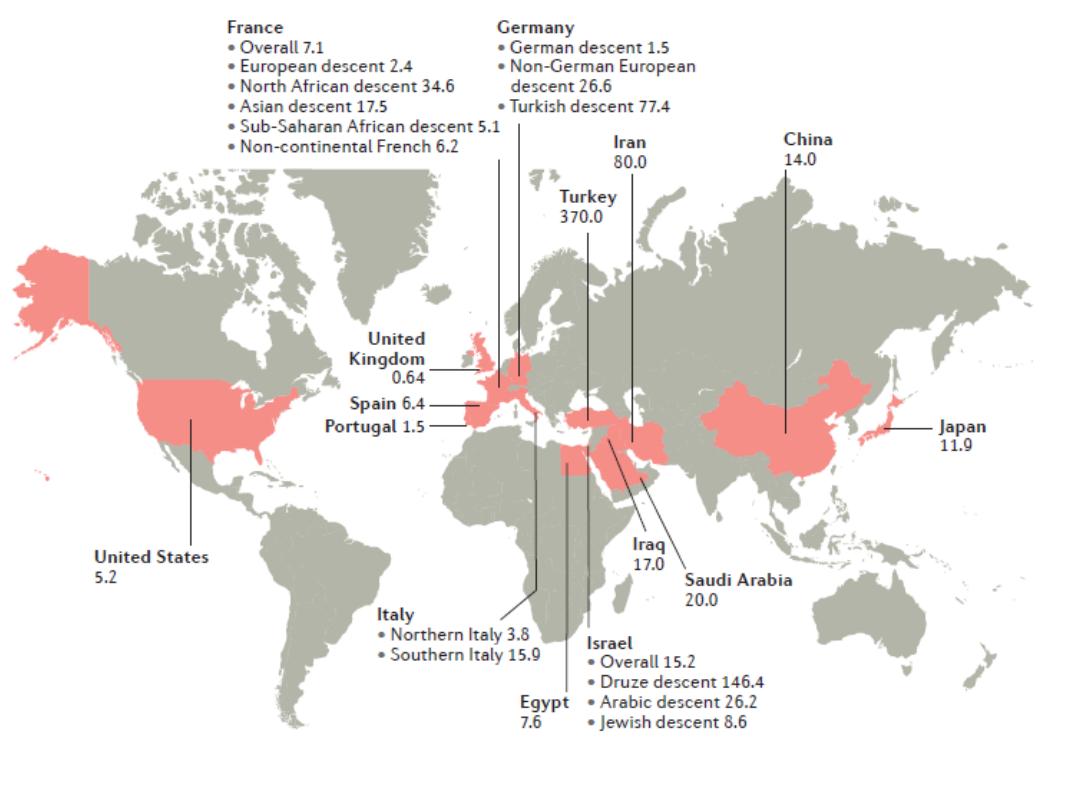
Behcet’s Prevalence per 100 000
From: Yazci H. Nature reviews | rheumatology vol14 feb 2018 | 112
3/16/2020
3/16/2020
3/16/2020
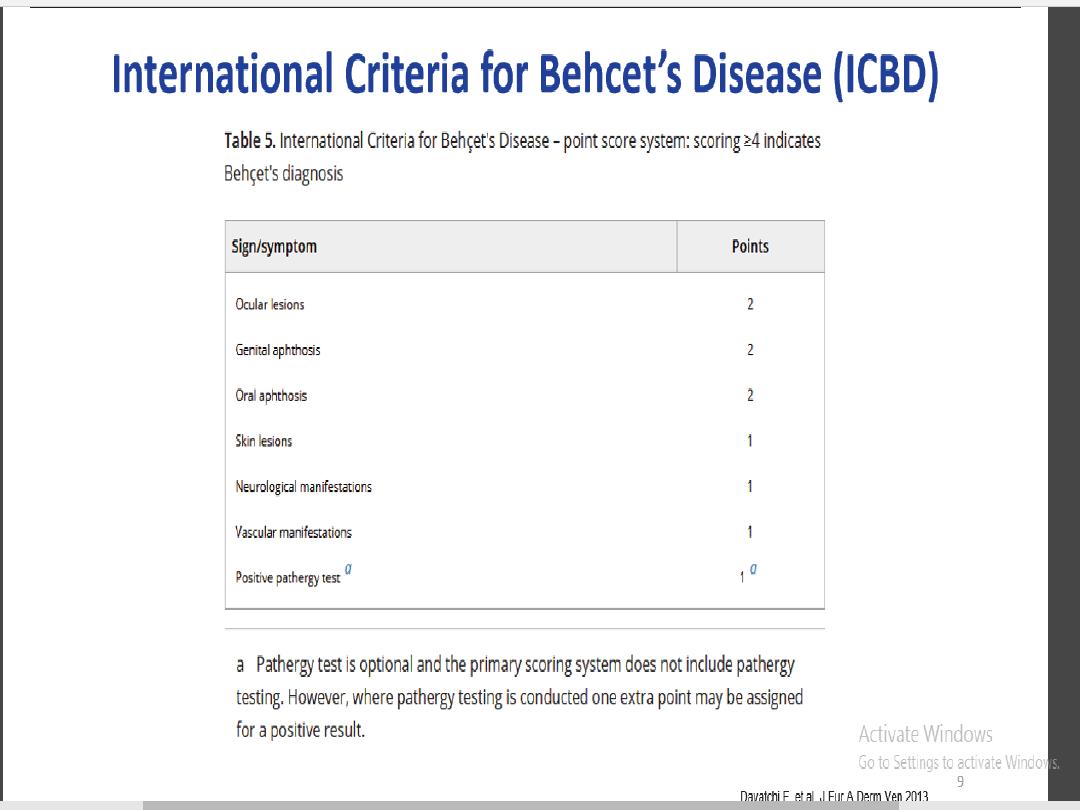
Clinical manifestations
• Are variable with unpredictable periods of
recurrences and remissions.
• The frequency and severity tend to decrease
with time.
• Skin-mucosa lesions are the most common
presenting symptoms
• Ocular, vascular and neurological
involvement are less common but more
serious.
3/16/2020

Mortality
• The overall mortality rate is significantly
increased among younger men (<25 years of age)
and early in the disease course among those with
major organ involvement
• Major causes of mortality:
– Large vessel disease
– Parenchymal CNS disease
• A French group showed a mortality rate of 5%
during a median follow-up of 8 years in a cohort
of 817 patients.
Saadoun D.
Arthritis Rheum. 62, 2806–2812 (2010)
3/16/2020

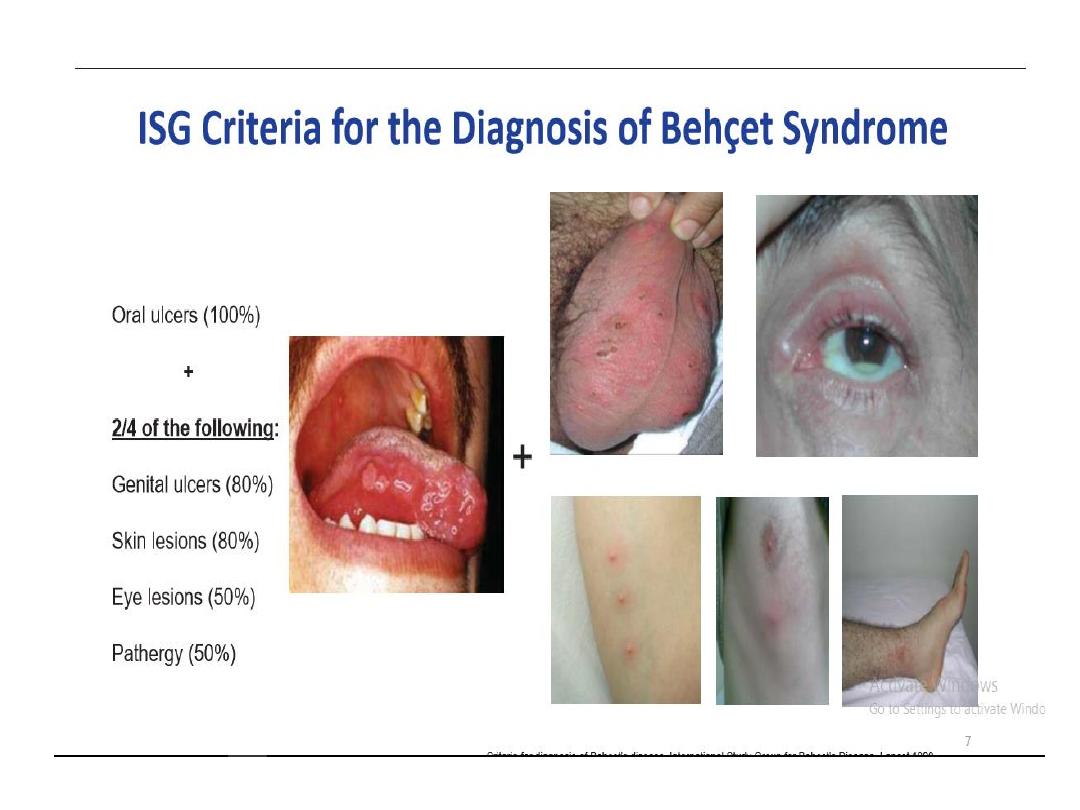
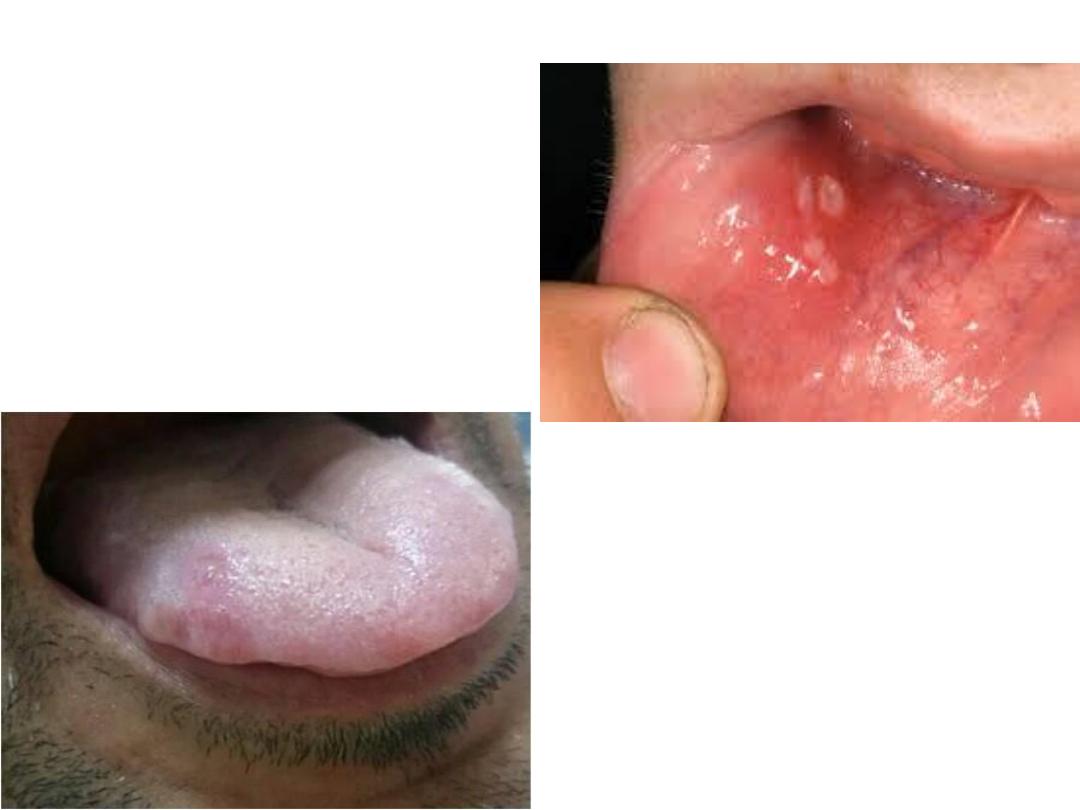
Oral ulcerations
• It is usually the initial symptom, and often precedes
diagnosis by several years.
• it can be seen in 97%–100% of the patients. Lesions may
occur singly or in crops, and subside within a few weeks.
• The most common sites are the tongue, lips, and gingival
and buccal mucosa, although involvement of the palate,
pharynx, and tonsil can also occur. It can be classified as
minor, major, or herpetiform based on their
characteristics. Minor ulcers are defined as isolated or
multiple, shallow, and small (<10 mm), and usually heal
without scarring. Major ulcers are larger (>10 mm), deeper,
and more painful than minor ulcers. Herpetiform ulcers
refer to numerous shallow, small, pinpoint (1–2 mm in
diameter) lesions, occurring as clusters.
3/16/2020

• Incidental trauma such as tooth brushing,
gum chewing, or eating foods with sharp and
rough textures can trigger the formation of
aphthous ulcers. Oral ulceration that recurs
more than three times in 1 year is required to
meet the diagnostic criteria for Behçet’s
disease.
3/16/2020
3/16/2020

Genital Ulcers
• Genital ulcers occur in more than 70% of
cases.
• They are similar to oral ulcers, but are
deeper, larger and can take longer to heal.
• Genital scarring is a strong evidence of the
presence of Behçet syndrome.
• Thy locate on the scrotum in men and in the
labia in women, but are more severe in men.
•
urethritis is not a feature of Behçet’s disease,
which may be useful in distinguishing it from
Reiter’s syndrome.
3/16/2020
3/16/2020

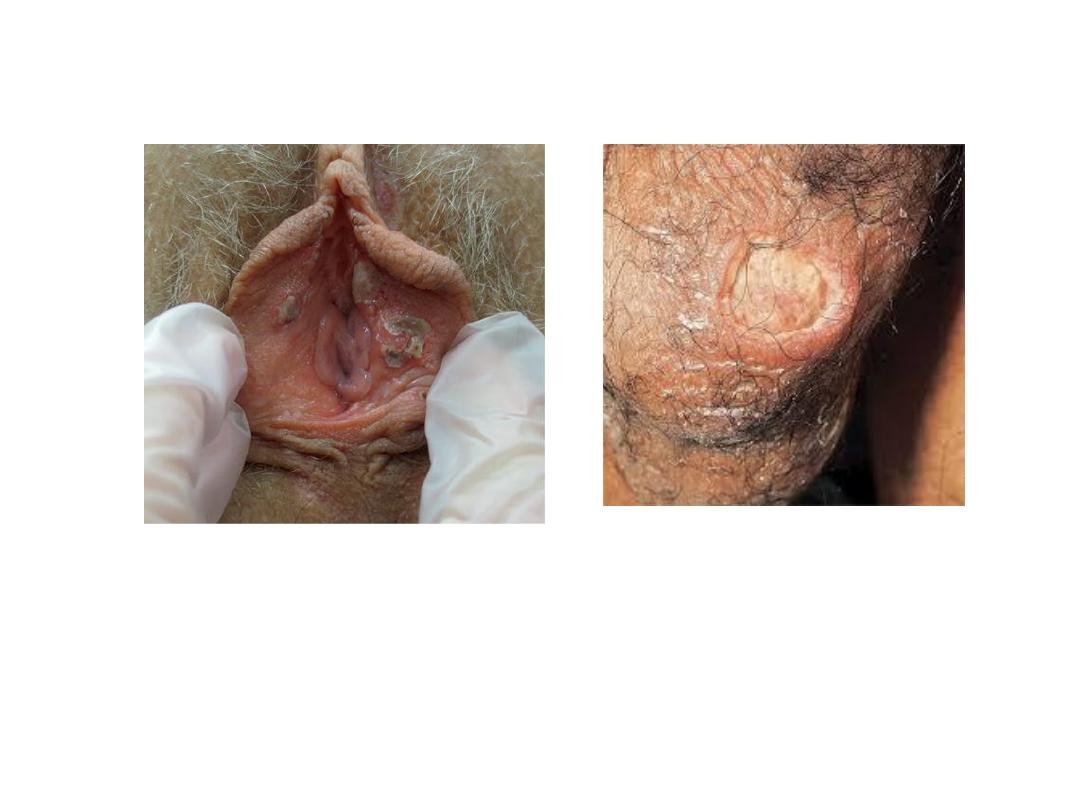
Eye involvement
• Eye involvement occurs in 30%–70% of patients with
Behçet’s disease, and it is more common and more
severe in men than in women. The typical form of
ocular involvement is a relapsing–remitting uveitis.
Chronic and recurrent anterior uveitis can result in
hypopyon, which is characterized by accumulation of
white blood cells in the anterior chambers of the eye.
• Frequently present at onset or first 2-3 yr
• – Rare after 5 yr
• – Bilateral in 90% • Hypopyon (20%)
3/16/2020
3/16/2020

Skin disease
• occurs in over 75% of patients with Behçet’s
disease. Erythema nodosum usually occurs in the
lower extremities. They are more commonly
observed in female patients, and they heal with
pigmentation in 1–6 weeks.
• Other skin lesions are acneiform lesions, although
its appearance is similar to ordinary acne, and it
appears on the usual acne sites, such as the face,
back, and chest, it also occurs on unusual sites such
as the arms and legs.
• Pathergy
3/16/2020

Musculoskeletal disease
• Non-erosive arthritis is seen in about 50% of
patients with Behçet’s disease. The arthritis is
usually monoarthritis or oligoarthritis, affecting the
medium and large joints such as knee, wrist, and
ankle.
• In contrast to HLA B-27-associated diseases,
sacroiliitis is rare in patients with Behçet’s disease.
• A recent study showed significant familial clustering
of acne/arthritis/enthesitis, which supports a
hypothesis that a common genetic pathway is
involved in its clinical presentation.
3/16/2020
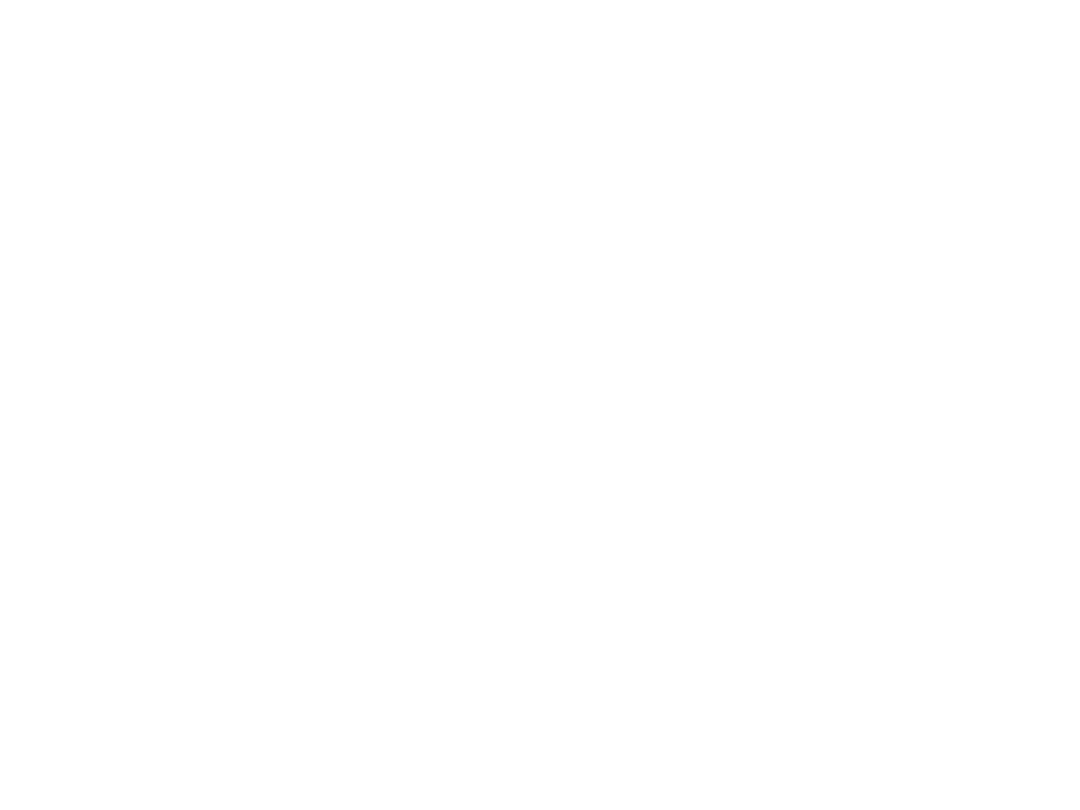
Vascular involvement
• Vascular involvement occurs in about 25% of
patients with Behçet’s disease, with a predilection
for veins.
• Lower extremity vein thrombosis (superficial and
deep) is the most common form of vascular
involvement and leads to severe post-thrombotic
syndrome and venous claudications.
• PAI can manifest as pulmonary arterial aneurysms
and single in situ pulmonary arterial thromboses.
• Mild elevation of pulmonary arterial pressure can be
associated with PAI and bronchial arterial collaterals
can cause of haemoptysis in patients with BS.
• Increased diameter of the aneurysms and PAH at
presentation are poor prognostic factors for survival.
3/16/2020

Vascular involvement
• Several types of vascular manifestation tend
to occur in the same individual, creating
statistically significant associations eg.
– Cerebral venous sinus thrombosis and
pulmonary artery involvement (PAI)
– Intracardiac thrombosis and PAI.
– Budd–Chiari syndrome and inferior vena cava
syndrome.
3/16/2020

• Budd–Chiari syndrome mostly involves the inferior
vena cava (the suprahepatic and hepatic segments)
and the hepatic veins.
• In patients who present with ascites, the mortality
rate is ~60% within a median of 10 months after
diagnosis.
• Budd–Chiari syndrome develops gradually without
ascites in some patients.
• US or CT show that these individuals have efficient
collateral formations.
• These ‘silent’ patients have more favourable
outcomes, with <10% expected mortality at 7 years.
3/16/2020
3/16/2020
A: Superficial and DVT. B: bilateral multiple PA aneurysm C: Bud Chiari w ascites< inferior
vena cava and all three hepatic veins occluded with thrombi
From: Yazci H. Nature reviews | rheumatology vol14 feb 2018 | 114

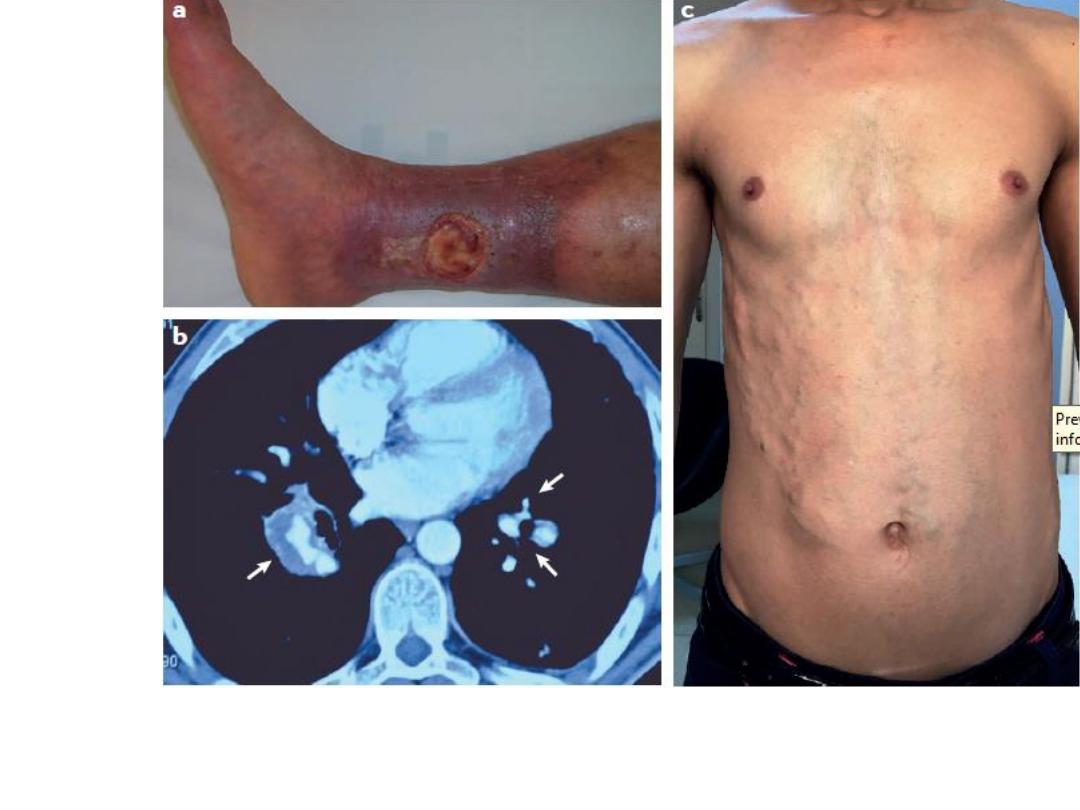
CNS involvement
• 5–10% of patients with BS, mostly parenchymal
brain involvement.
• Brainstem involvementis the most characteristic
type of involvement.
• Pyramidal signs, hemiparesis, behavioural–
cognitive changes, sphincter disturbances and/or
impotence .
• Psychiatric problems.
• Some clinical presentation of CNS disease in BS
can be mistaken for multiple sclerosis(MS), in
which case MRI findings are helpful.
3/16/2020

CNS involvement
• MRI findings in BS reveal large extensive lesions
of CNS, multiple sclerosis has more discrete and
smaller brainstem lesions.
• Optic neuritis, sensory symptoms and spinal cord
involvement, which are common in MS, are
seldom observed in BS.
• White matter lesions are also different: in MS,
lesions tend to be supratentorial and
periventricular with corpus callosum
involvement, whereas in BS lesions are small,
bihemispheric and subcortical.
Kikuchi H.
J. Neurol. Sci. 337, 80–85 (2014)
3/16/2020
MRI Changes in MS
3/16/2020
a: Axial View: Pontine and Cerebellar atrophy
B: Ischaemic lesion in Pons and 4
th
ventrile dilatatation
C: Sagittal view brain stem atrophy
From: Yazci H. Nature reviews | rheumatology vol14 feb 2018 | 115

CNS involvement
• The CSF also differs: pleocytosis is more
prominent in MS, whereas oligoclonal band
positivity (that is, the gold-standard test for MS)
is rarely observed in BS.
Siva A.
J. Neurol. 256, 513–529 (2009)
3/16/2020

Gastrointestinal involvement
• 10% of patients with inflammatory bowel
disease(IBD) who also had features of Behçet
syndrome tested positive to the pathergy skin
test.
• Showing how difficult it can be to differentiate
BS from IBD.
3/16/2020

Gastrointestinal involvement
• GI involvement in BS resemble Crohn’s disease, with abdo
pain and diarrhoea +_bleeding, and is an uncommon
manifestation in geographies other than in far-east Asia.
• BS causes round or oval ulcers in the terminal ileum. Ulcers
are deep, large and single with a tendency to perforate or
cause massive bleeding.
• Mucosal biopsies show chronic or active inflammation as
well as vasculitic findings.
• Faecal calprotectin levels are associated with disease
activity, similar to Crohn’s disease.
• Even with treatment, relapses occur in ~20% of patients.
Hatemi I.
Medicine 95, e3348 (2016)
3/16/2020

Treatment
3/16/2020

2018 UPDATE OF THE EULAR RECOMMENDATIONS FOR
THE MANAGEMENT OF BEHÇET’S SYNDROME
• RECOMMENDATION 1:
• MUCOCUTANEOUS INVOLVEMENT
Topical steroids should be used for the treatment of
oral and genital ulcers. Colchicine should be tried first
for the prevention of recurrent mucocutaneous
lesions especially erythema nodosum and genital ulcer.
Treatment of leg ulcers in BS should be planned with
the help of a dermatologist and vascular surgeon.
Drugs such as azathioprine, thalidomide,
interferon-alpha, tumour necrosis factor-alpha
inhibitors or apremilast should be considered in
selected cases.
3/16/2020

RECOMMENDATION 2: EYE INVOLVEMENT
Collaboration with ophthalmologists.
BS and inflammatory eye disease affecting the
posterior segment should be on a treatment
regime such as:
1.
azathioprine
2.
cyclosporine-A
3.
interferon-alpha or
4.
monoclonal anti-TNF antibodies.
Systemic glucocorticoids should be used only in
combination with azathioprine or other systemic
immunosuppressives
3/16/2020

Patients presenting with an initial or recurrent
episode of acute sight-threatening uveitis
should be treated with high-dose
glucocorticoids, infliximab or interferon-
alpha.
Intravitreal glucocorticoid injection is an option
in patients with unilateral exacerbation as an
adjunct to systemic treatment.
Glucocorticoids should never be used alone in
patients with posterior uveitis. Azathioprine,
cyclosporine-A, interferon-alpha, infliximab or
adalimumab should be used in such patients.
3/16/2020

Adalimumab seems to be an effective
alternative to infliximab.
Concomitant use of azathioprine
and/or cyclosporine-A with
monoclonal anti-TNF antibodies may
improve the outcome
.
3/16/2020

RECOMMENDATION 3:
ISOLATED ANTERIOR UVEITIS
• Isolated anterior uveitis in patients with BS
may be treated with topical agents.
• Systemic immunosuppressives could be
considered for those with poor prognostic
factors such as young age, male sex and
early disease onset.
3/16/2020

RECOMMENDATION 4:
ACUTE DEEP VEIN THROMBOSIS
• For the management of acute deep vein
thrombosis in BS, glucocorticoids and
immunosuppressives such as azathioprine,
cyclophosphamide or cyclosporine-A are
recommended.
• Cyclophosphamide may be reserved for patients
with extensive thrombosis of larger veins such as
vena cava due to its potential adverse events.
• Treatment with anticoagulant have no added
benefit.
3/16/2020

RECOMMENDATION 5:
REFRACTORY VENOUS THROMBOSIS
• Monoclonal anti-TNF antibodies could be
considered in refractory patients.
• Anticoagulants may be added, provided the
risk of bleeding in general is low and
coexistent pulmonary artery aneurysms are
ruled out.
3/16/2020

RECOMMENDATION 6:
ARTERIAL INVOLVEMENT
For the management of pulmonary artery aneurysms,
high-dose glucocorticoids and cyclophosphamide are
recommended.
Monoclonal anti-TNF antibodies should be considered in
refractory cases. For patients who have or who are at high
risk of major bleeding, embolisation should be preferred
to open surgery.
For both aortic and peripheral artery aneurysms, medical
treatment with cyclophosphamide and corticosteroids is
necessary before intervention to repair. Surgery or
stenting should not be delayed if the patient is
symptomatic.
3/16/2020

RECOMMENDATION 7:
GASTROINTESTINAL INVOLVEMENT
• Gastrointestinal involvement of BS should be
confirmed by endoscopy and/or imaging.
• NSAID ulcers, inflammatory bowel disease
and infections such as tuberculosis should be
ruled out.
3/16/2020

RECOMMENDATION 8:
REFRACTORY/SEVERE GASTROINTESTINAL
INVOLVEMENT
• Urgent surgical consultation is necessary in
cases of perforation, major bleeding and
obstruction.
• Glucocorticoids should be considered during
acute exacerbations, together with 5-ASA or
azathioprine.
• For severe and/or refractory patients,
monoclonal anti-TNF antibodies and/or
thalidomide should be considered.
3/16/2020

RECOMMENDATION 9:
NERVOUS SYSTEM INVOLVEMENT
Acute attacks of parenchymal involvement should be
treated with high-dose glucocorticoids followed by slow
tapering, together with immunosuppressives such as
azathioprine.
Cyclosporine-A should be avoided.
Monoclonal anti-TNF antibodies should be considered in
severe disease as first line or in refractory patients. ( III; C)
The first episode of cerebral venous thrombosis should be
treated with high-dose glucocorticoids followed by
tapering.
Anticoagulants may be added for a short duration.
Screening is needed for vascular disease at an extracranial
site
3/16/2020

RECOMMENDATION 10:
JOINT INVOLVEMENT
• Colchicine should be the initial treatment in BS
patients with acute arthritis.
• Acute monoarticular disease can be treated with
intra-articular glucocorticoids.
• Azathioprine, interferon-alpha or tumour necrosis
factor alpha inhibitors should be considered in
recurrent and chronic cases.
• If colchicine can not control articular symptoms, low
dose GCs, azathioprine, interferon-alpha or TNFis
can be used. (expert opinion) .
3/16/2020

References
Kelly Textbook of Rheumatology 2017.
Mirouse A, et al. Arthritis Rheum 2019
Fabiani C, et al. Clin Rheumatol 2017.
Ozguler Y, et al. Rheumatology 2018.
Hatemi G, Christensen R, Bang D
, et al,
2018
update of the EULAR recommendations for the
management of Behçet’s syndrome.
Annals of the
Rheumatic Diseases
Published Online First: 06
April 2018. doi: 10.1136/annrheumdis-2018-
213225.
3/16/2020
