
Babylon collage of medicine
Osteoporosis

• Osteoporosis is a major public health problem in
and a life altering disease.
One out of every two women and one of every four
men over the age of 50 are at risk for osteoporosis,
low bone density, and will have a fracture.
Osteoporosis is often silent until someone breaks a
bone; but then, a fracture can change their life.
Every 20 seconds someone in USA will have a
preventable fracture. So during our time together
today, 180* Americans will have a fracture. Imagine
that!
Why bone health matters
What is osteoporosis
How to prevent bone loss
How is osteoporosis diagnosed
Treatments to prevent fractures
How to prevent falls
1
2
3
4
5
6
70%
of people over 65 with osteoporosis have never
been screened and don’t know they have
osteoporosis
Osteoporosis is a Serious Problem
Centers for Disease Control & Prevention 2016
Centers for Disease Control & Prevention, 2015
Centers for Disease Control & Prevention, 2015
National Osteoporosis Foundation, 2015
0
400,000
800,000
1,200,000
1,600,000
2,000,000
2,400,000
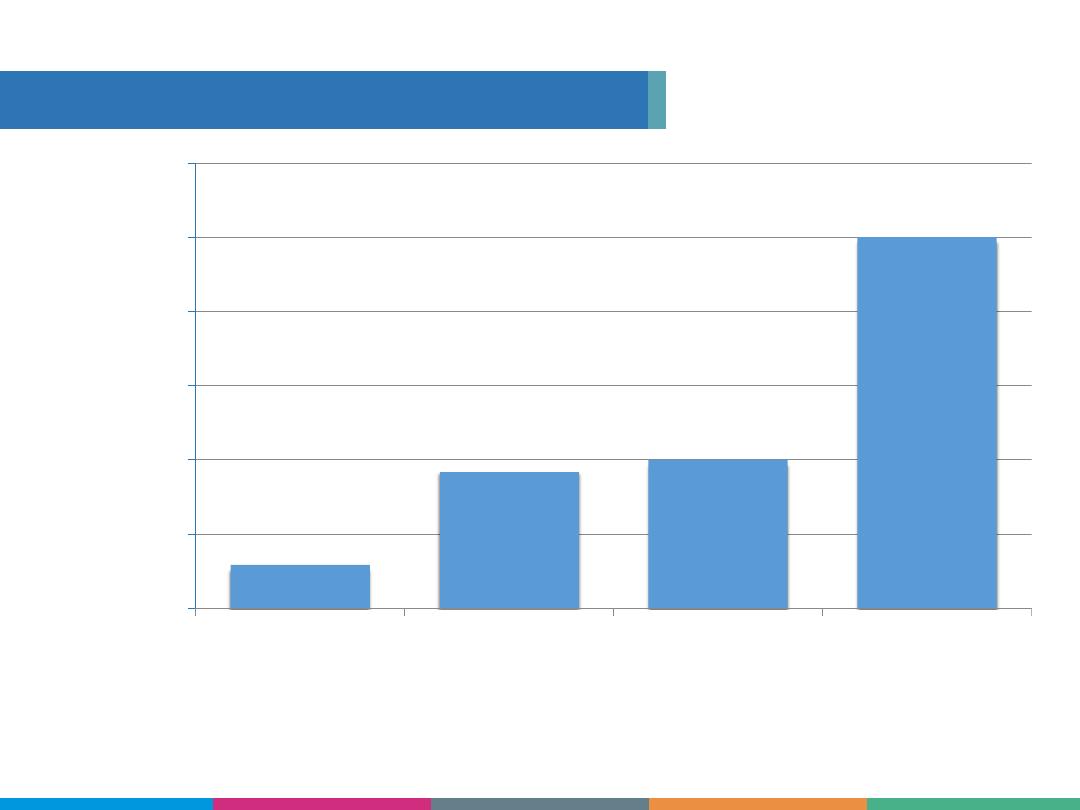
Breast Cancer
Heart Attacks
Strokes
Fractures
232,924
735,000
800,000
2,000,000
Compared to Other Health Issues
Annual occurrences
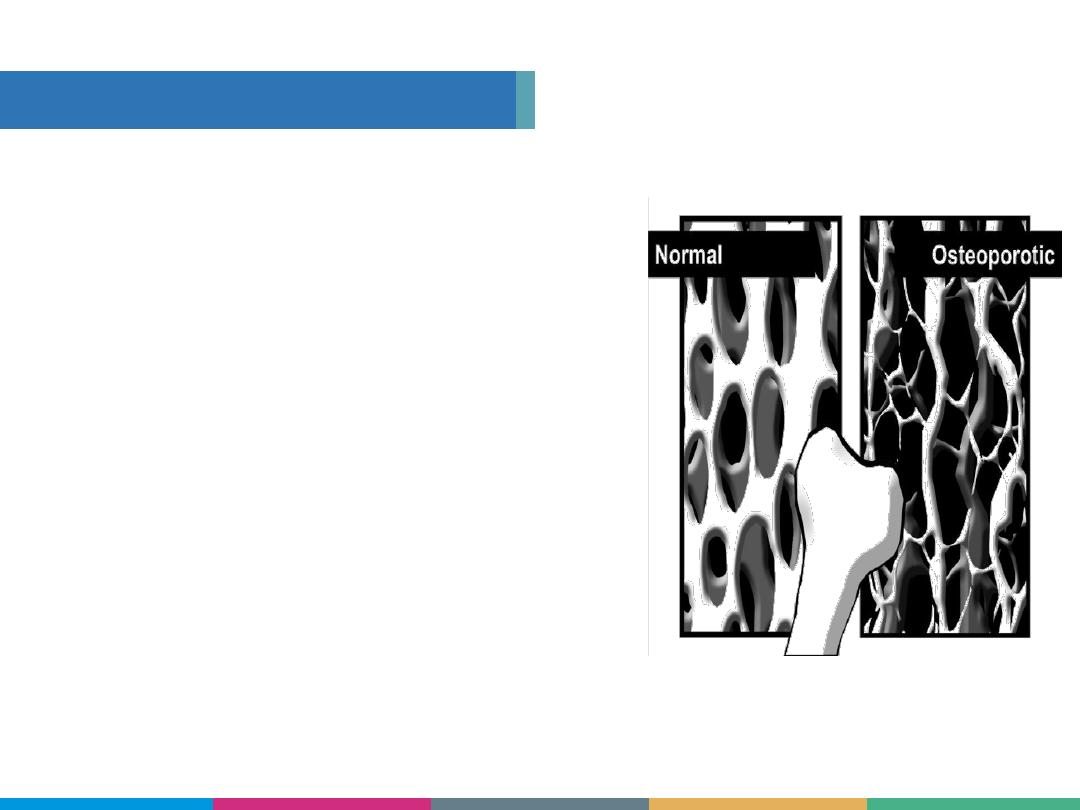
Osteoporosis is a Disease
When the skeleton loses
mineral density, the
structure becomes thin
and unable to take
normal weight, leaving
bones that break easily.
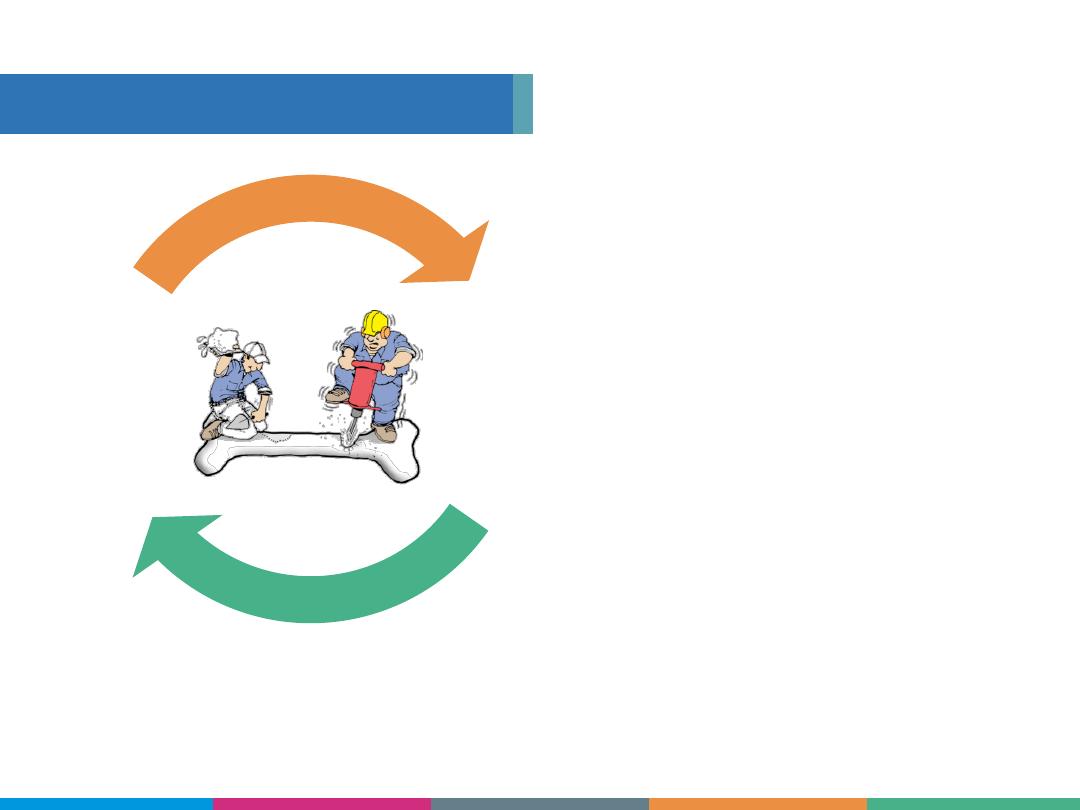
Bone
remodeling
means you have
the opportunity
to have
new bones
every
7-10 years!
Bones Are Living Tissue
Osteoclasts
Osteoblasts
Osteoblasts- build new bone
Osteoclasts- remove old or damaged bone
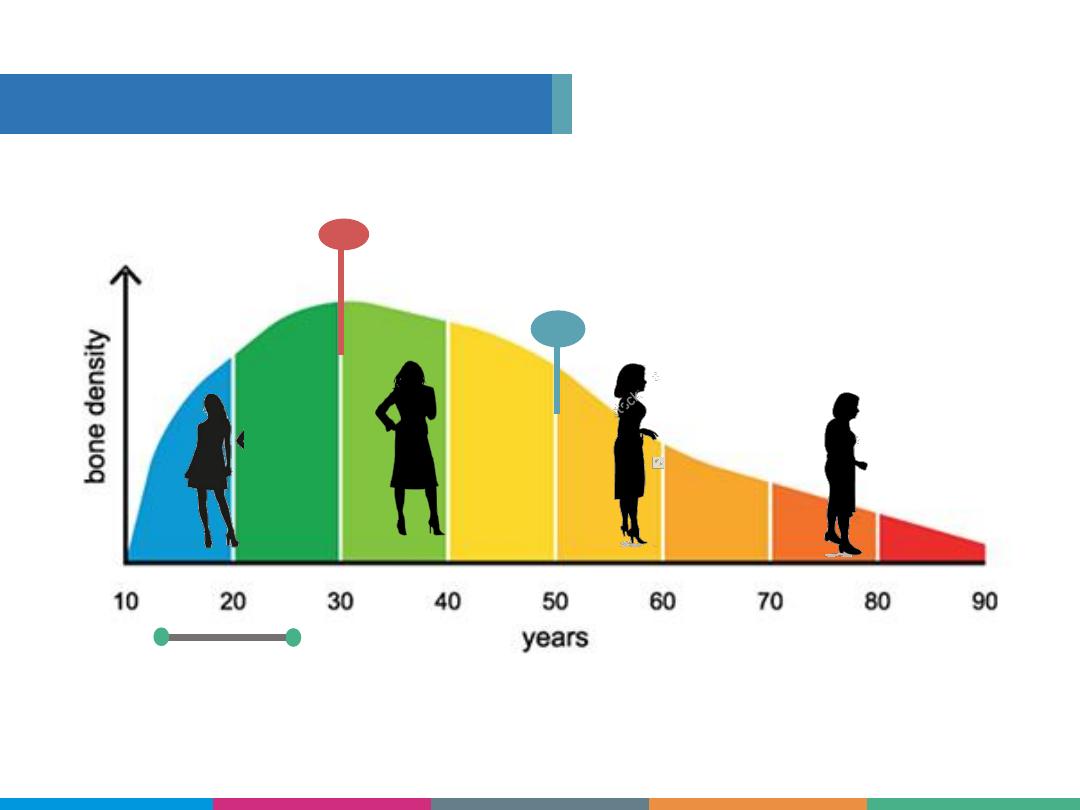
How the Skeleton Changes
Menopause
Peak Bone Mass
Rapid Bone
Building
Gender
Heredity
Age
Fracture history
Risk Factors for
Osteoporosis
Medical conditions
Medications
1
2
3
4
5
6
Things you
can’t
change
Risk Factors for Osteoporosis
Calcium consumption
Vitamin D intake
Quit smoking or vaping
Alcohol consumption
Physical activity
Posture
1
2
3
4
5
6
Things you
can
change
7
3
8
Low body weight (BMI <20)
Some medications
Risk Factors for
Osteoporosis
Risk Factors for Osteoporosis
Disordered eating
Alcoholism
Cancers
Celiac Disease
Crohn’s Disease
Cushing’s Disease
Hypogonadism
Hyperthyroidism
Liver Disease
Malabsorption
Rheumatoid Arthritis
Diabetes Type II
Risk Factors for
Osteoporosis
Conditions That Cause Bone Loss
PPIs
(Nexium, Prilosec, Zantac)
Anticoagulants
(Heparin)
Anticonvulsants
(Dilantin)
Chemotherapy drugs
Cyclosporine
Tamoxifen
(premenopausal use)
SSRIs
(Prozac, Zoloft, Paxil)
Lithium
Methotrexate
Oral steroids
(Prednizone)
Thyroxine - high doses
(Synthroid)
Aromatase inhibitors
Androgen
deprivation
therapy
Risk Factors for
Osteoporosis
Medications That Cause Bone Loss
Low Impact Fracture
More than 1½” Height Loss
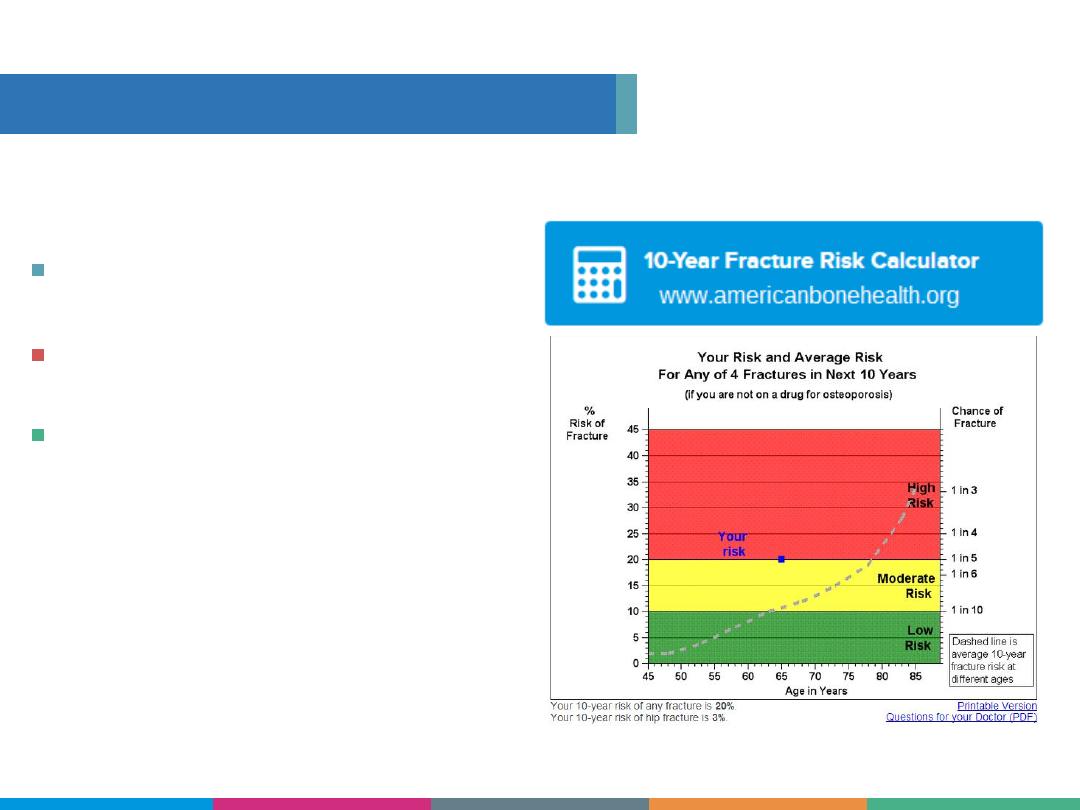
FORE Fracture Risk
Calculator™
The calculator gives an
estimate of your risk of
breaking a bone.
Risk Factors for
Osteoporosis
How You Might Know Your Risk

Get a Bone Mineral Density Test
(also known as DXA)
Covered benefit for
Women age 65+
Men age 70+
Anyone younger with a risk factor
This simple and painless test takes about 15 minutes.
Risk Factors for
Osteoporosis
How You Know For Sure

•
Excellent diagnostic tools
–
Bone densitometry with DXA –
noninvasive test
–
FRAX
®
– new tool to help with
management decisions in patients with
reduced bone mineral density

2018 Guidelines for Bone Density Testing
1. Adapted from
National Osteoporosis Foundation
. Clinician’s Guide to Prevention and Treatment of Osteoporosis.
Washington, DC: National Osteoporosis Foundation
;
2013. Available at: http://www.nof.org/hcp/clinicians-guide. Accessed
September 13, 2013.
2. US Preventive Services Task Force.
Ann Intern Med. 2002;137:526-528.
•
Screening
–
All women age 65 and older
1,2
–
All men age 70 and older
1
•
Test postmenopausal women and men >50 if
1
:
–
Fracture after age 50
–
Clinical risk factors for osteoporosis
–
Conditions/medications associated with bone loss
o
COPD, RA, hyperparathyroidism, celiac disease,
IBD
o
Oral glucocorticoids, anticonvulsants, proton
pump inhibitors, SSRIs, aromatase inhibitors
There is a difference between screening and
making a diagnosis of osteoporosis. Screening
tools may lead to a diagnosis, but the gold
standard is DXA which is X-ray technology. The
heel screening uses ultrasound and there is a
much lower correlation with T-scores.
“The only way you can know for sure is to get tested.
We diagnose osteoporosis with a Bone Mineral
Density Test or DXA. This test measures the amount of
bone density, usually in the spine and hip. It is simple
and painless, and takes about 15 minutes.
At the age of 65, Medicare fully covers a DXA scan
every 24 months at age 65 for women and age 70 for
men. If you are younger and have any ONE risk factor,
you should talk with your doctor about ordering this
test.
”
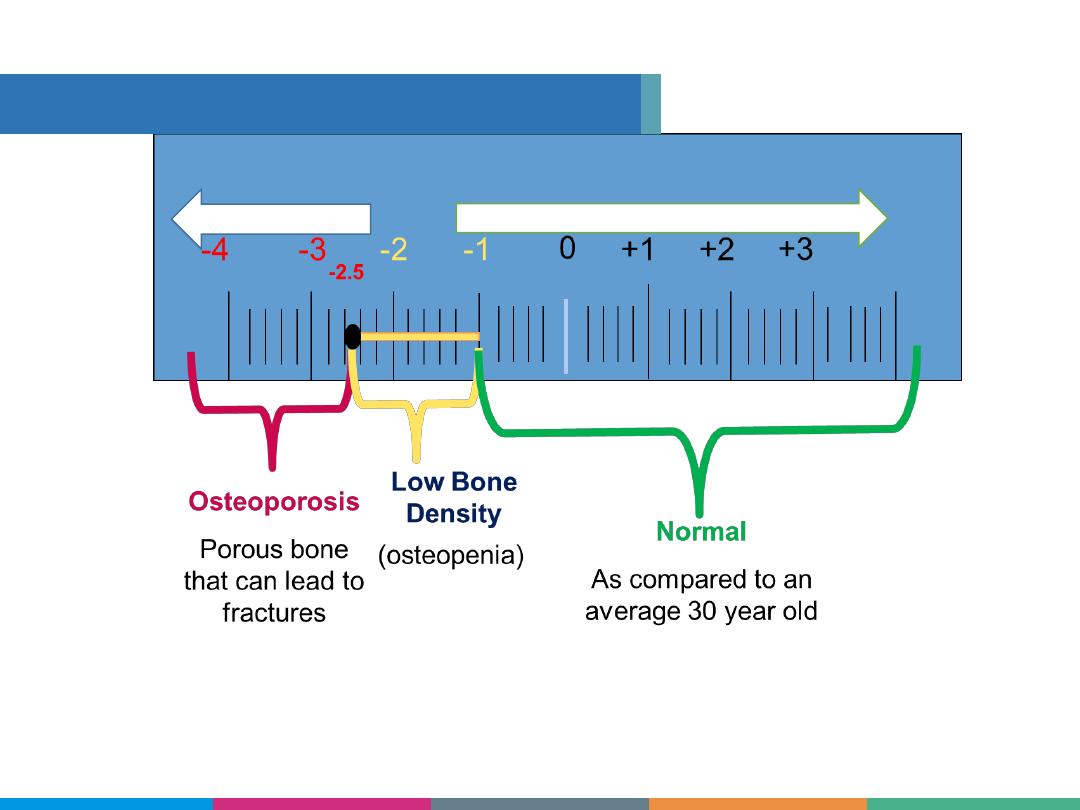
> -1.0 T-score
< -2.5 T-score
Even though you may have a low bone density,
you may not have an increased fracture risk.
Your peak bone density may never have reached the “normal”
range.
Risk Factors for
Osteoporosis
Understanding Your DXA Results
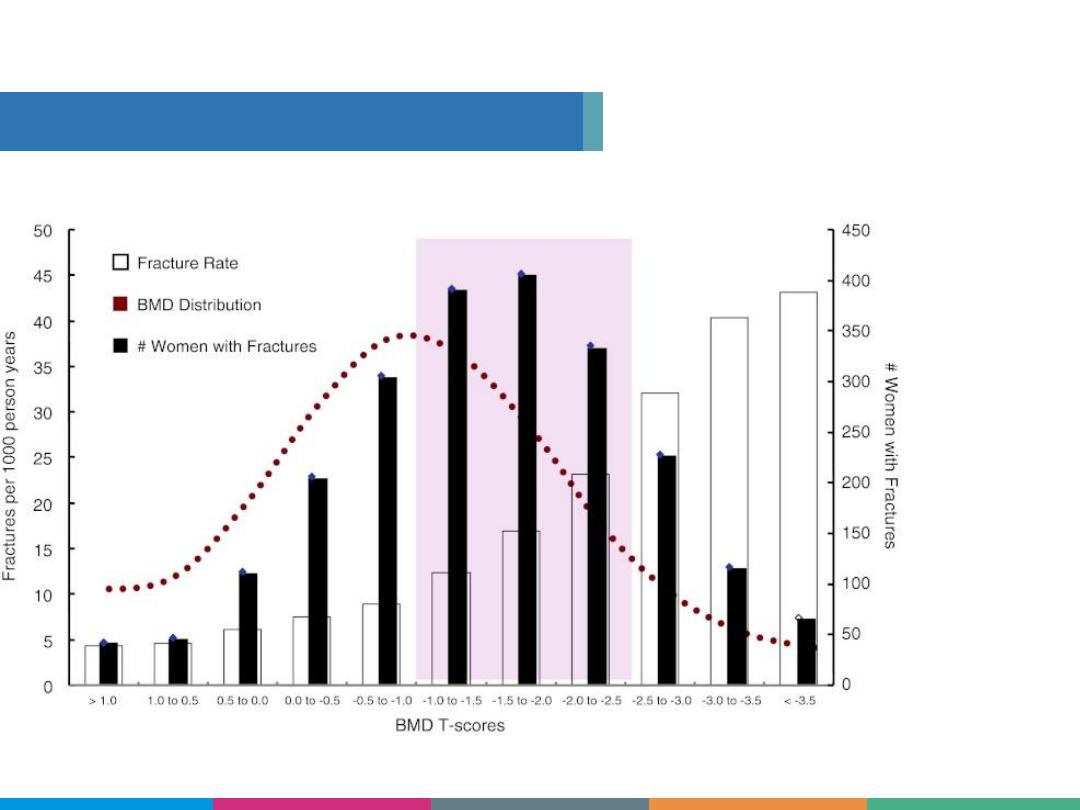
Fractures Happen at all BMDs

Statistically robust fracture risk prediction tool
developed by the WHO for world-wide use
Combines BMD + clinical risk factors to predict
fracture risk better than either alone
Predicts the 10-year probability of major
osteoporotic fracture
Hip, spine, wrist, or humerus
Use when the decision to treat is uncertain
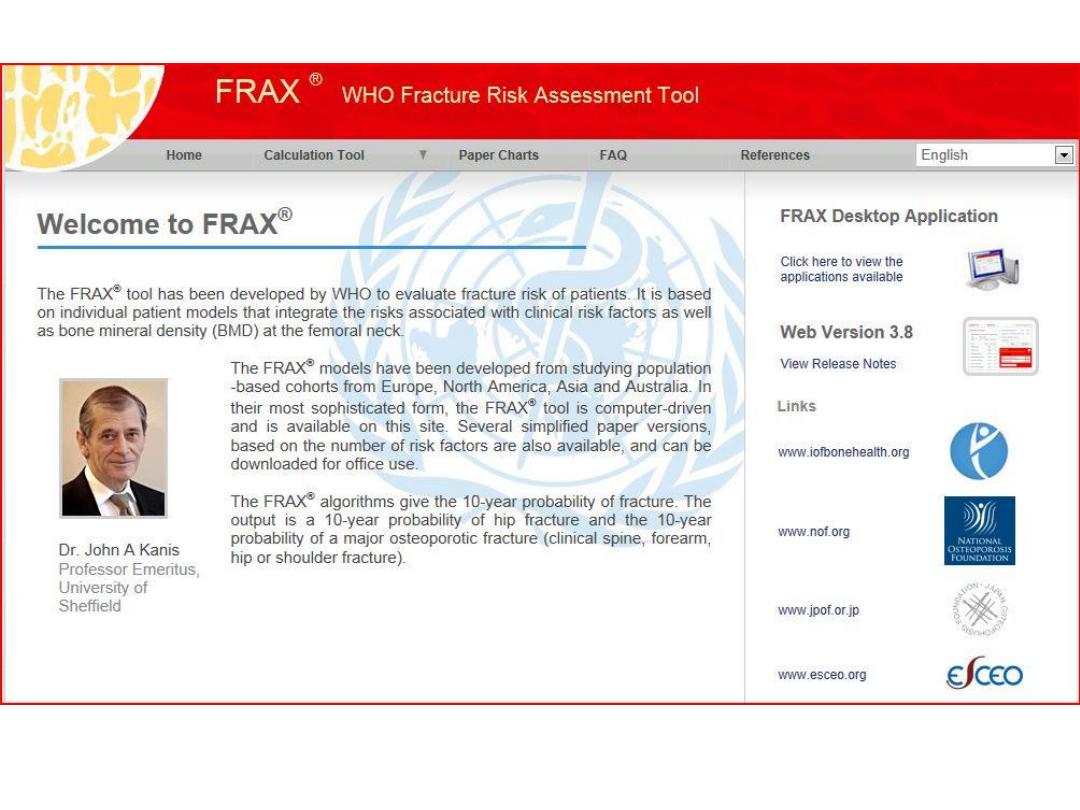
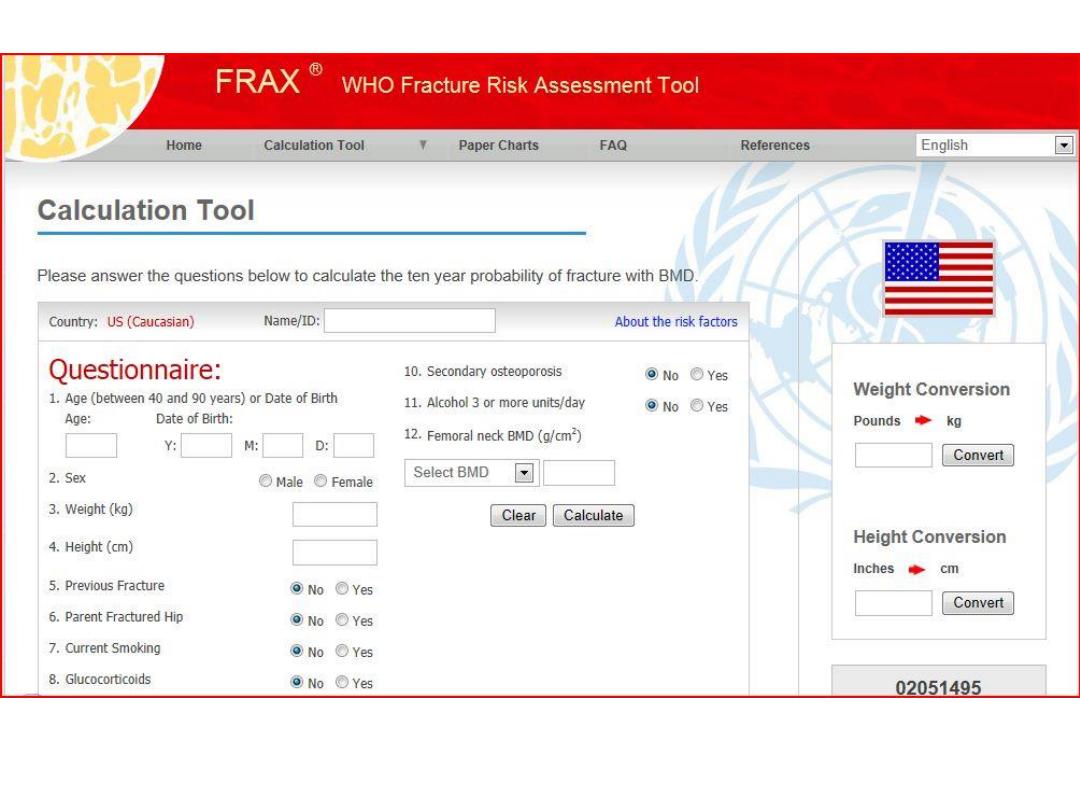
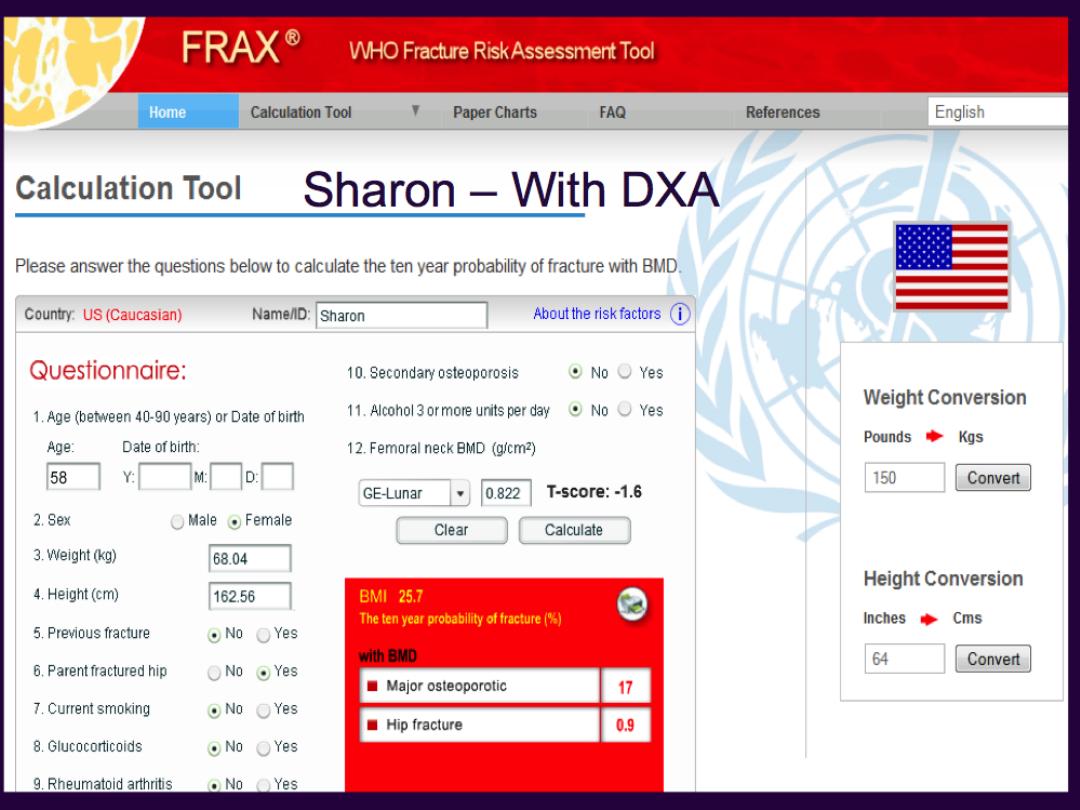

Benefits of FRAX
®
Treatment decisions in osteopenic patients
clearer
Decision is based on the risk of fracture, not T-
score alone
Identifies patients at high-risk for fractures to
ensure that they are offered treatment to
lower their risk
Helps avoid giving medication to those who are
at low risk and have little to gain from
treatment

Osteoporosis Management
•Nonpharmacologic
• Pharmacologic

Challenges With Current
Treatment Approaches
• Bone loss per se asymptomatic
• Patients may not appreciate fracture prevention
• No treatment agent meets the ideal profile—
inexpensive, easy to take, uniformly effective,
entirely free of risk
• Perceived risk of therapy may outweigh perceived
benefit
• Patient motivation to “adhere” and “persist” with
therapy may vary



Vitamin
D
3-4 servings of a calcium rich food = 1,000 -
1,200 mg
Nerves and muscles need calcium to function;
if not available, the body will take calcium from
bones
The current RDA is 1,000-1,200 milligrams per day
Risk Factors for
Osteoporosis
Calcium is the Principle Mineral of
Bone

Food
Item
Calcium Range
Dairy
Low Fat Yogurt, Milk, Cheese 150-400 mg
Proteins
Tofu (with Calcium),
Sardines (With Bones),
Garbanzo Beans, Almonds
75 - 400 mg
Vegetables Collards, Bok Choy, Kale,
Broccoli
20-260 mg
Other
Foods
Pizza, Lasagna, Mineral Water
(Gerolsteiner), Dried Figs
120 - 450 mg
Dietary Sources of Calcium
Risk Factors for
Osteoporosis
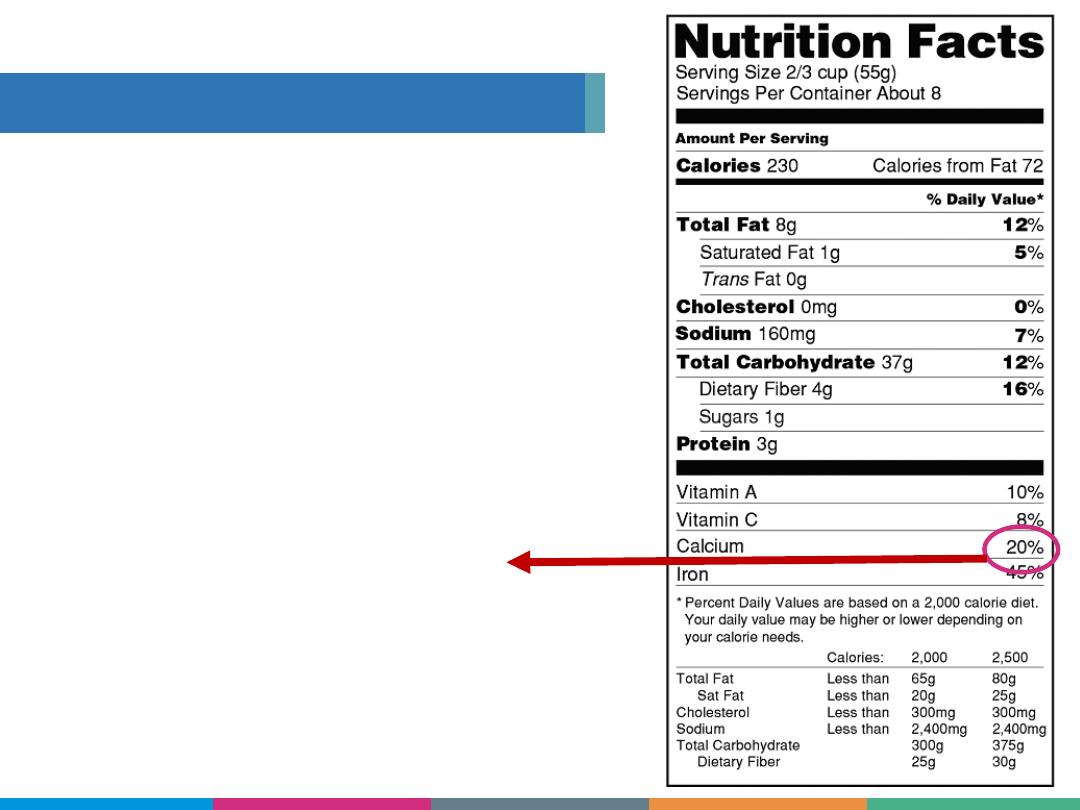
How To Read a Nutrition Label
Add a zero to the calcium
% to get milligrams per
serving.
20% + 0 = 200 mg
Risk Factors for
Osteoporosis
If You Need a Supplement
Body can only absorb 500-600 mg at a
time Do not take more than 1,500 mg/day
Two types of calcium supplement
Calcium carbonate
i.e., Caltrate
Less expensive,
Take with food
Calcium citrate
i.e., Citracal
Easier on stomach,
Take with or without food
1
2
If you don’t eat 2-3 servings of a calcium-rich food
every day, you may need a supplement.
RDA varies from 600- 2,000 International Units per day
Sunshine alone is not a reliable source of vitamin D
Calcium needs vitamin D to get absorbed in the intestine
Food
Item
Vitamin D Range
Fatty Fish
Salmon, Sardines,
150-500 IU
Dairy
Milk, Fortified with D
100-125 IU
Other Foods Fortified Cereals, Juices 50-75 IU
Protein
Egg Yolk
44 IU
It’s very hard to get enough vitamin D through diet!
Supplements are not expensive.
Risk Factors for
Osteoporosis
Vitamin D is Essential
Bones Like a Load
To build bone density, you
must do activities that
“surprise” and add weight to
the bone.
Activities that strengthen muscles,
strengthens bone.
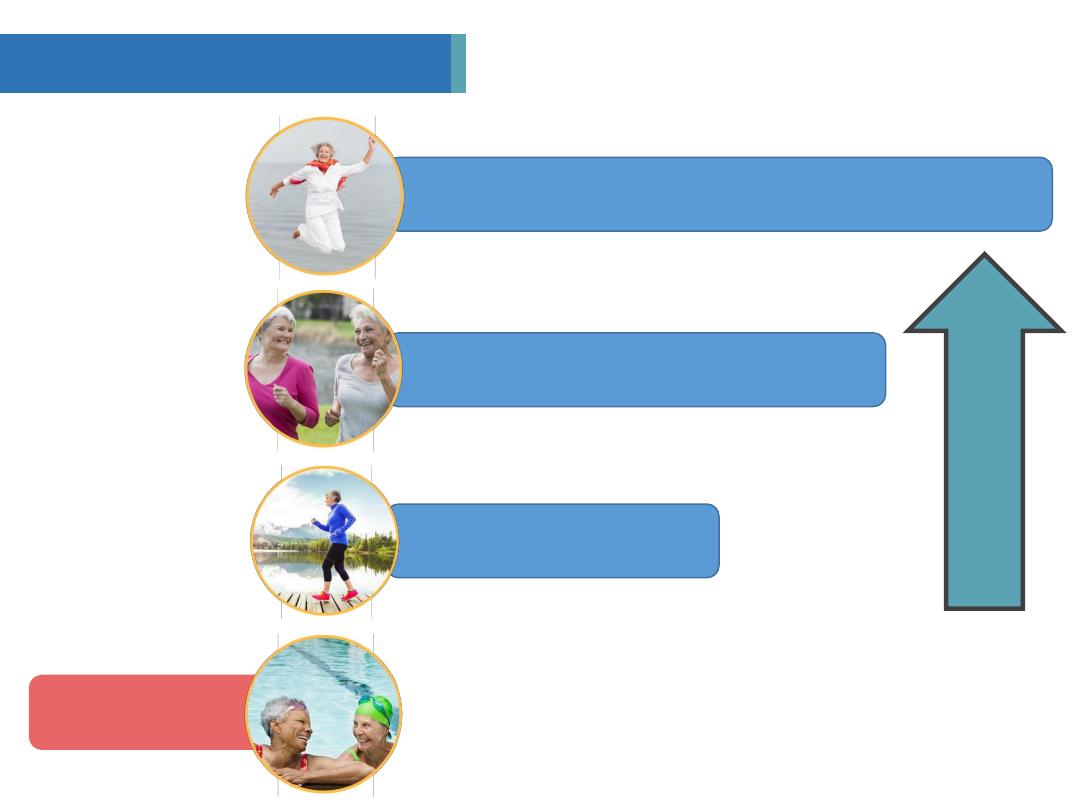
Levels of Load by Body Weight
Loads Vary by Activity
4+
3
Jump, strength train
1-2
<0
Run, jog
Brisk walk
Swim, cycle
Increasing effect on
bone density
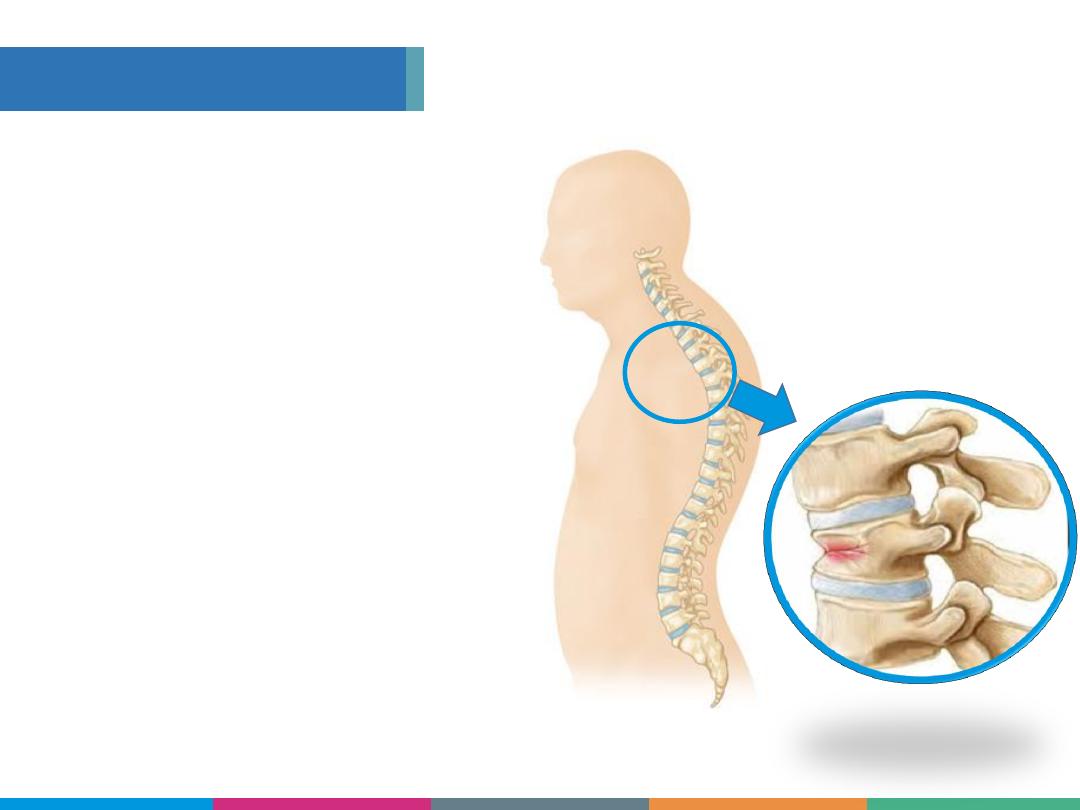
Load Safely
The spine is most
VULNERABLE
when rounding forward.
AVOID
compression
fractures.
ALWAYS
bend at the
hips with a straight
spine.

The spine bones, especially the smaller
bones in the thoracic spine between the
shoulder blades, [Point to thoracic spine]
are particularly vulnerable when you are
rounding forward. If you do not use proper
body mechanics, you can cause a
compression fracture [point to broken
vertebra

Practice great posture
1
2
3
4
5
Expand chest muscles
Strengthen back muscles
Use great body mechanics
Strengthen abs
(plank is great!)
Support the Spine Bones
Improve Posture
Standing “W” Exercise
Strengthen back muscles
Pull arms backwards,
pinch shoulder blades
Hold for 3 seconds. Breathe.
Repeat as often as you can!
Raise arms parallel to floor
1
2
3
4

Balance to Prevent Falls
Stop multi-tasking
2 million people land in the emergency room
from a fall. 500,000 falls result in hospital stays.
Risk Factors for
Osteoporosis
Prevent Falls to Prevent Fractures
1
2
3
4
5
Remove trip hazards
Get your eyes checked
Keep a night light on
Get your medications checked
Bisphosphonates
Alendronate, Actonel, Atelvia, Boniva, Fosamax,
Reclast, Zometa
SERM (Selective Estrogen Receptor Modulators)
Evista, Duavee
Denosumab
Prolia
Parathyroid Hormone
Forteo
Treatment Options
Knowing your fracture risk can help you decide
if you will benefit from a treatment.
• Calcitonin
•
PTH (teriparatide)
•
Denosumab
Prevention
• Alendronate
• Risedronate
• Ibandronate
• Zoledronic acid
• Raloxifene
• Can do both
• Estrogen
prevention only

Antiresorptive
Decrease bone resorption
Most treatment agents
Examples: Bisphosphonates,
SERMs, calcitonin, estrogen,
denosumab
Anabolic
Stimulate bone formation
Example: teriparatide

Alendronate: 10 mg daily (tablet) or 70 mg weekly
(tablet or liquid) for treatment, 5 mg daily or 35 mg
weekly for prevention
Risedronate: 5 mg daily or 35 mg weekly (tablet);
150 mg monthly (tablet)
Ibandronate: 150 mg monthly by tablet; 3 mg
intravenously over 15 to 30 seconds every 3
months
Zoledronic acid: 5 mg by intravenous infusion over
a minimum of 15 minutes once every year for
treatment—and every other year for prevention

Treatment and prevention of postmenopausal
osteoporosis
Alendronate, risedronate, ibandronate, zoledronic
acid
Prevention and/or treatment of glucocorticoid-
induced osteoporosis
Risedronate, zoledronic acid, alendronate
Treatment of men with low bone density
Alendronate, risedronate, zoledronic acid

Monoclonal antibody to RANKL
60 mg subcutaneous injection every 6 months
9% increase in spinal BMD after 3 years in the
pivotal FREEDOM trial; 4% to 5% increase in hip
BMD
Reduction in fracture risk after 3 years:
68% decrease in new vertebral fractures
40% decrease in hip fractures
20% decrease in nonvertebral fractures
8-year data: continued increase BMD, reduced
bone turnover, good safety

The right medication for the right patient
at the right time
Susceptibility to side effects
Past history of DVT – no estrogen or raloxifene
Esophageal stricture – use of IV bisphosphonates or
denosumab
Dosing/convenience
Adherence

Get
calcium and vitamin D
daily.
Food is best, supplement if
needed.
1
2
3
4
Do
weight-bearing and balance
exercises
everyday.
Know your T-scores
and keep a
copy of all your bone density tests.
Know your risk
for fractures, get
screened and diagnosed.
Risk Factors for
Osteoporosis
Important Things to Remember
