
Sjogren’s Syndrome
Dr Ali Alkazzaz-Babylon collage of
medicine

• Sjögren syndrome is a systemic chronic
inflammatory disorder characterized by
lymphocytic infiltrates in exocrine organs.
The disorder most often affects women, and
the median age of onset is around 50 to 60
years. Most individuals with Sjögren
syndrome present with sicca symptoms, such
as xerophthalmia (dry eyes), xerostomia (dry
mouth), and parotid gland enlargement,

Etiology
• Sjögren syndrome can occur as a primary disease of
exocrine gland dysfunction or in association with
several other autoimmune diseases (eg, systemic
lupus erythematosus [SLE], rheumatoid arthritis,
scleroderma, systemic sclerosis, cryoglobulinemia,
polyarteritis nodosa). These primary and secondary
types occur with similar frequency, but more
severe symptoms in the primary form.

History
• The clinical presentation of Sjögren syndrome may
vary. Most patients are women, and onset is usually
at age 40-60 years, but the syndrome also can affect
men and children. The onset is insidious. The first
symptoms in primary Sjögren syndrome can be
easily overlooked or misinterpreted, and diagnosis
can be delayed for as long as several years.
• Xerophthalmia (dry eyes) and xerostomia (dry
mouth) are the main clinical presentations in adults.
Bilateral parotid swelling is the most common sign
of onset in children.

Patients may describe the effects dry mouth in the
following ways
Inability to eat dry food (eg, crackers) because it sticks
to the roof the mouth
Tongue sticking to the roof of the mouth
Putting a glass of water on the bed stand to drink at
night (and resulting nocturia)
Difficulty speaking for long periods of time or the
development of hoarseness
Higher incidence of dental caries and periodontal
disease
Altered sense of taste
Difficulty wearing dentures
Development of oral candidiasis with angular cheilitis,
which can cause mouth pain

Correct therapy depends on correct
diagnosis
a) New international criteria
b) Potential pitfalls in diagnosis
Epidemiology of Sjogren’s
1. Predominately women (9:1) with two
ages of median onset
In the 30’s and 50’s
2. Much of what we call
SLE
in the older
patient is actually
Sjogren’s syndrome
T
ime course of autoimmune response
• 1. Genetic factors predispose to Sjogren’s.
2. Environmental factors such as a viral infection
may lead to
formation of autoantibodies.
3. Antibodies precede disease (however, presence
of antibody does not
necessarily mean disease
Environmental
Factor
(virus-such as
EBV
)
(apoptotic fragment)
Genetic
Factors
(including sex)
(HLA-DR)
Immune
complex

Genetics
1. Most important is HLA-DR, which
correlates closely with ANA and anti-
SS-A antibody
2. Genes of B-cell activation similar to
SLE patients

Environmental
No single agent identified
Viral candidates may include EBV and
coxsackie viruses
Hepatitis C, HIV and HTLV-1 can
mimic
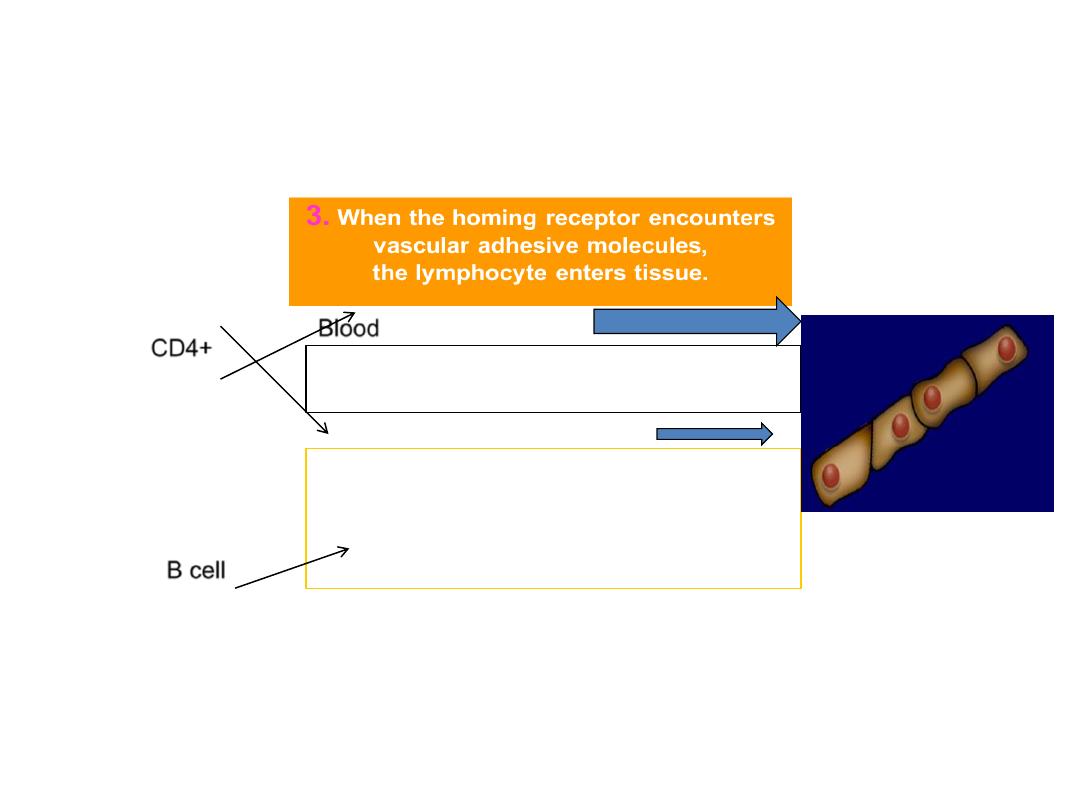
Part of the cause of Sjogren’s is that
lymphocytes “home” to the glands
CD4+
B cell
2.
Lymphs migrate through blood
to tissues.
1
. T- and B-cells have surface “homing
receptors” when generated in node or
marrow.
Blood

Clinical Manifestations
• Benign—glandular dryness
• Systemic--extraglandular

Sjogren’s syndrome
•The residual glandular cells are paralyzed by the
local
•immune reaction.
•Even though the acini/ducts
•are 50% present, their innervations and their
receptors
•for neurotransmitters are present
Clinical Key Points : Dry Mouth

Parotitis
• Patients with Sjögren syndrome may have a
history of recurrent parotitis, often bilateral.
Although in some patients the parotid glands
become so large that the patients report this
as a problem, more often the examining
physician discovers them.

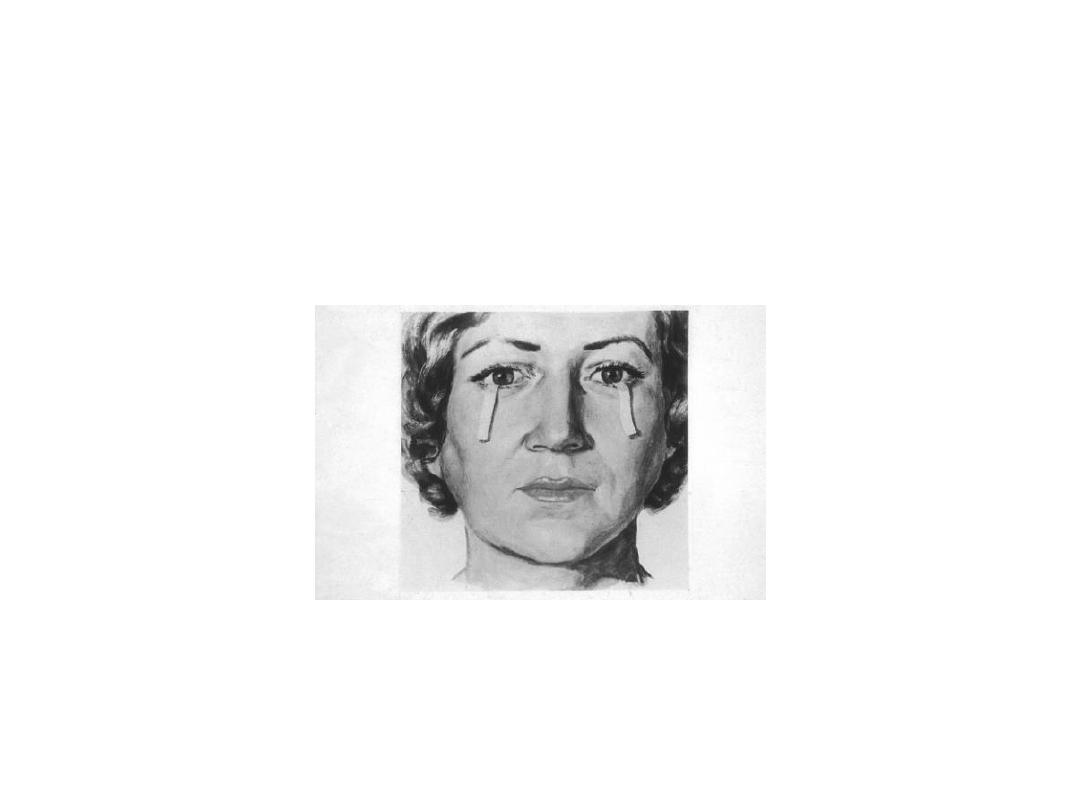
• Dry eyes may be described as red, itchy, and
painful. However, the most common
complaint is that of a gritty or sandy
sensation in the eyes. Symptoms typically
worsen throughout the day, probably due to
evaporation of the already scanty aqueous
layer. Some patients awaken with matting in
their eyes and, when severe, have difficulty
opening their eyes in the morning. Blepharitis
can also cause similar morning symptoms.
The upper lid
literally sticks to the
Epithelial surface
and pulls surface
mucin layers off.
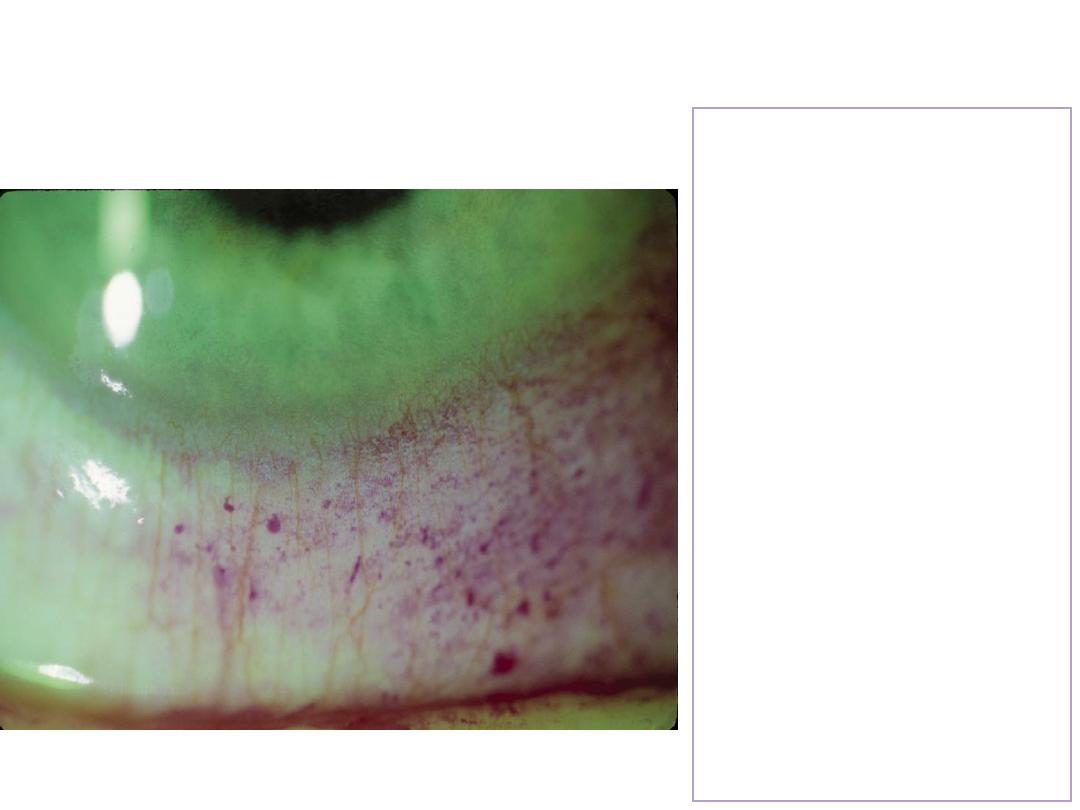
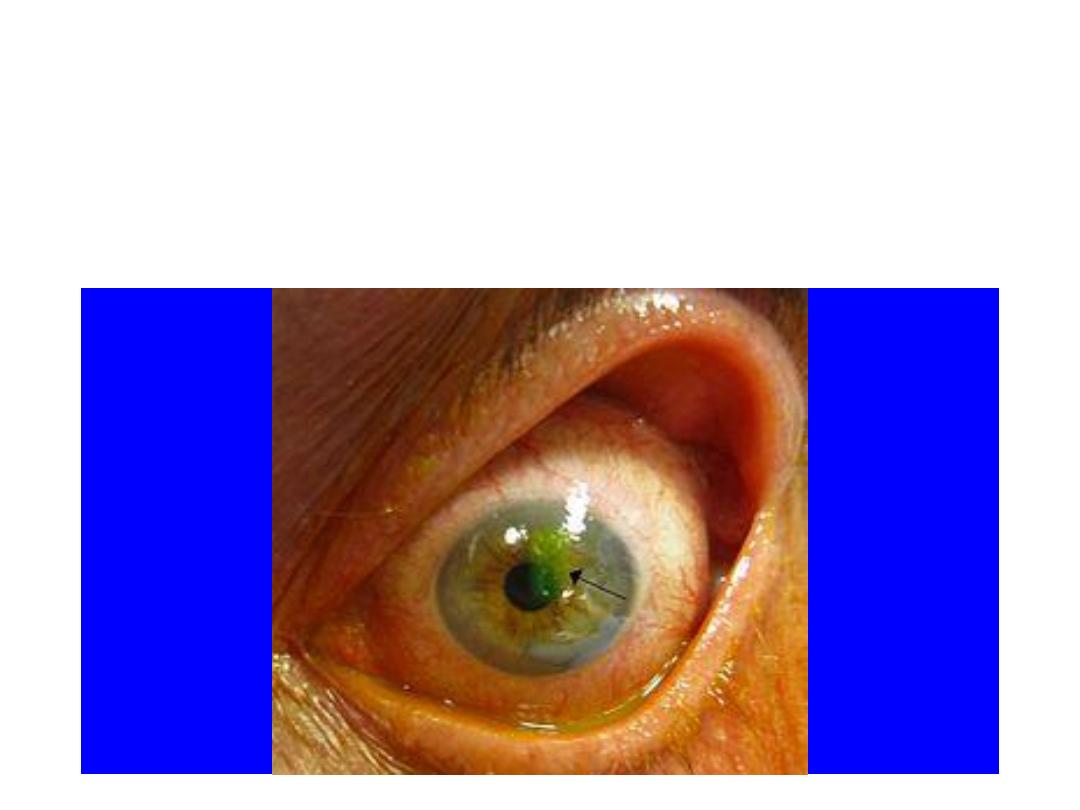
The Rose Bengal
dye retention test
is like
“rain water pooling
in a street pothole”
There is good agreement about diagnosis for the
patient with florid symptoms of
keratoconjunctivitis sicca (KCS), parotid swelling,
and high titer ANA with SS-A/SS-B.
The issue in these patients will be therapy
And the extent of extra glandular involvement.
Typical features of dry
eyes, dry mouth and swollen glands
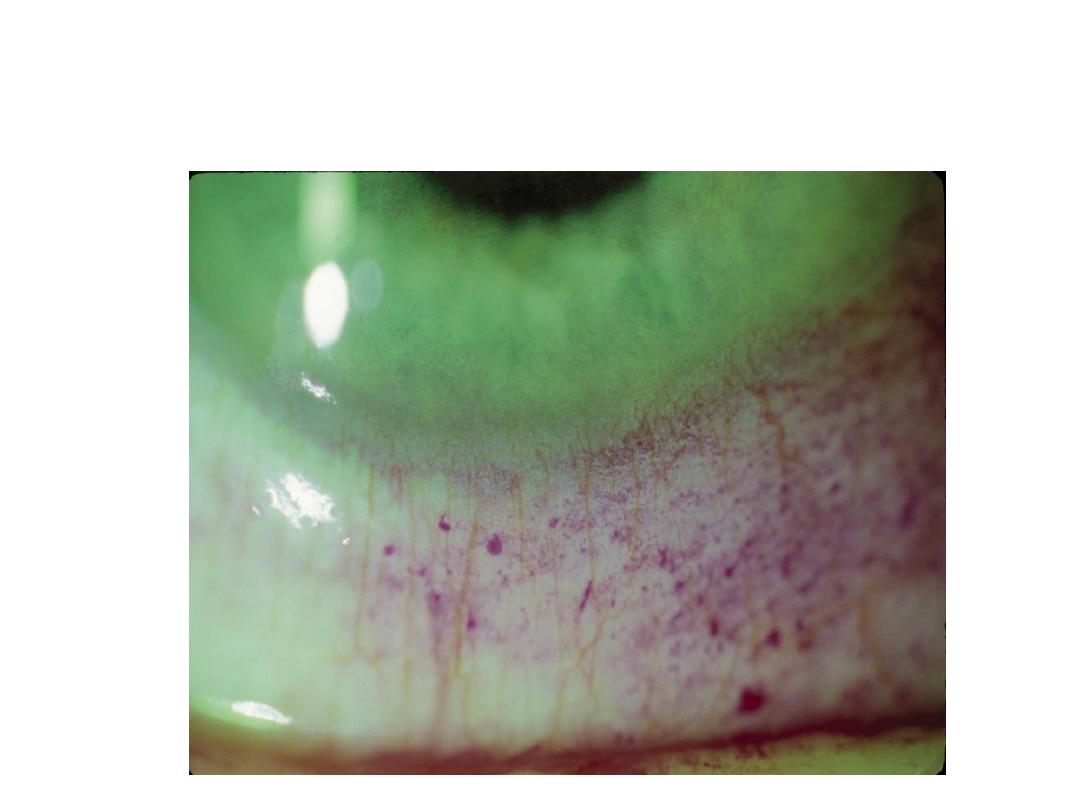
Dryness results in the clinical appearance of
keratoconjunctivitis sicca (KCS)
characteristic of Sjogren’s syndrome
conditions that require immediate Ophthalmologic
Evaluation
Corneal Abrasion (fluorescein

Severe Xerostomia with dry tongue

Sjogren’s syndrome
Eye and Oral Features
1. Most of these patients have a positive ANA with
positive
Anti-Sjogren’s SS-A/SS-B antibodies
2. They have specific needs for the eye and mouth
care
•
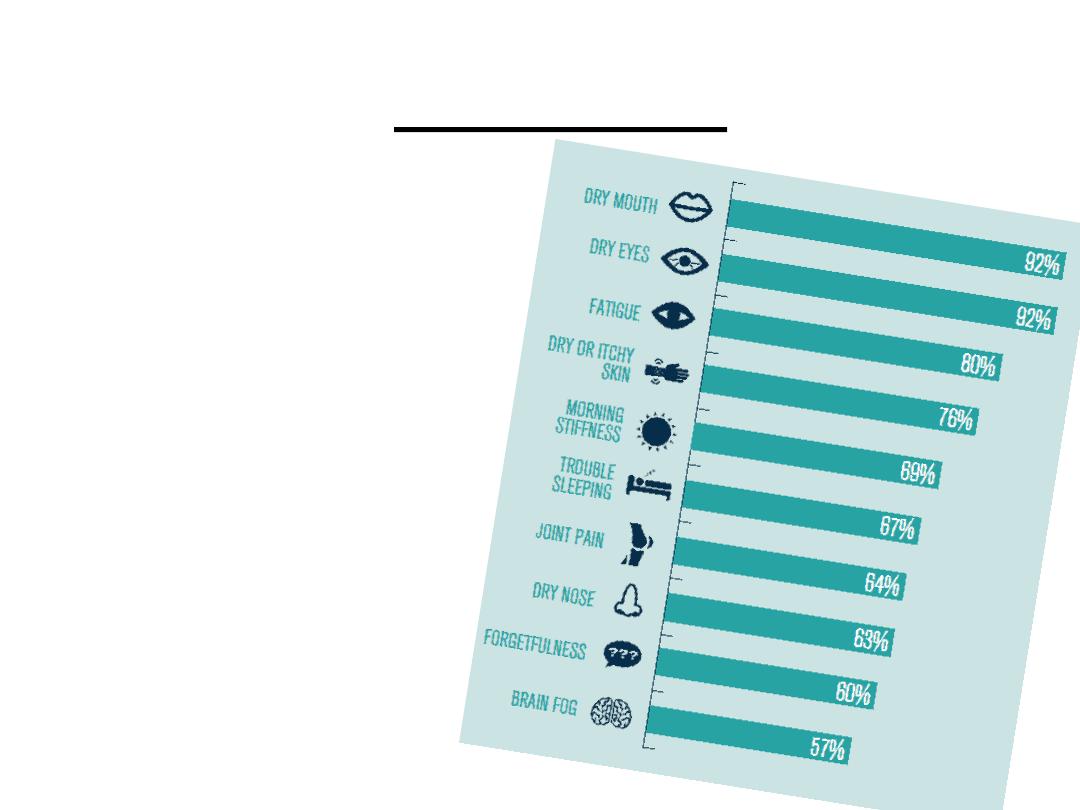
Top 4 Symptoms:
• Dry Eye – 92%
• Dry Mouth –
92%
• Fatigue – 80%
• Dry Skin – 76%
.
Patient Survey

glandular and extraglandular signs.
• patients with Sjögren syndrome should be referred
to an ophthalmologist for more formal testing of
keratoconjunctivitis sicca (KCS). This testing applies
grading criteria of inflammatory changes that can
direct therapy aimed at preventing corneal damage.
In addition, conditions that mimic KCS, such as
blepharitis, conjunctivitis, and uveitis can be ruled
out or treated.

Sjogren’s Syndrome- Cervical Dental Caries

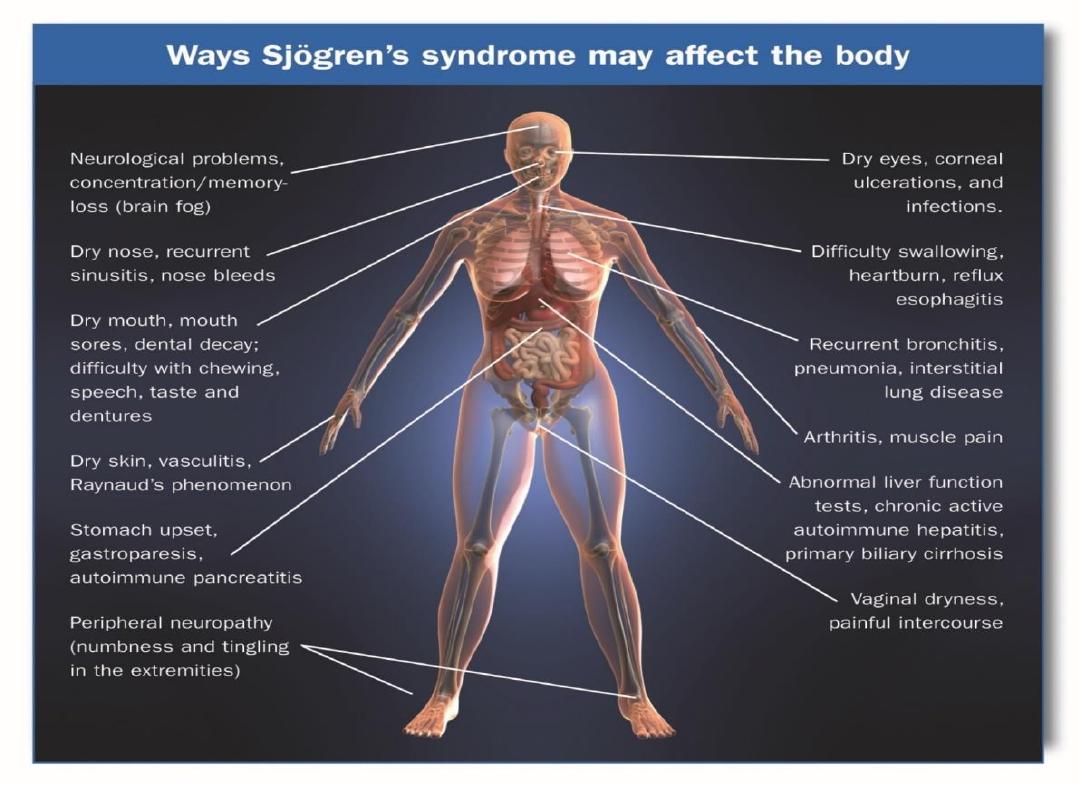
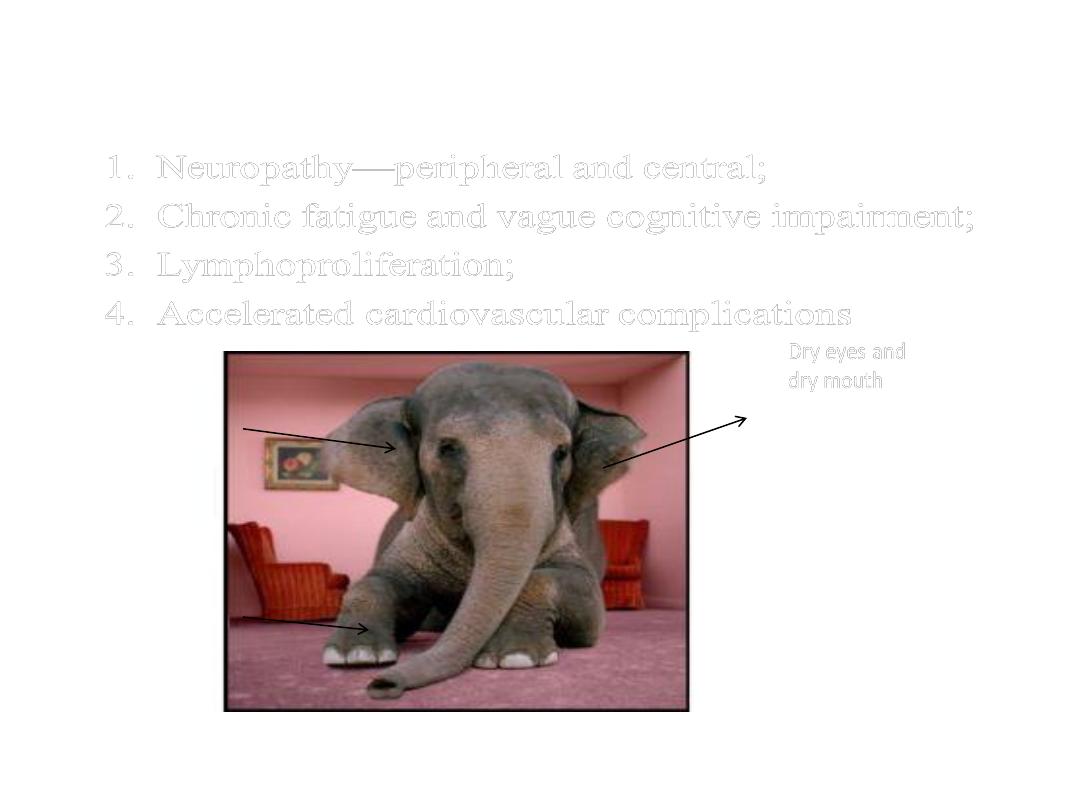
In addition to dry eyes and dry
mouth
These patients have signs and symptoms that affect
other parts of their body ranging from obvious
manifestation of skin vasculitis to vague symptoms
of fatigue and cognitive loss
Diagnostic Issues
In the patient with true Sjogren’s
Sjogren’s syndrome
Extent
Of
Extra glandular
Disease
Therapy
And
Education

Differential Diagnosis:
is the Dryness Due to Other Causes
Non Salivary Gland Disease
Drugs-esp.. BP and cardiac
muscle relaxants
antidepressants and
OTC meds for cold
Acute anxiety and
depression
Mouth breathing
Central lesions:
Multiple sclerosis
Alzheimer’s
Salivary Gland Disease
Hepatitis C
Sarcoidosis
Fatty Infiltrate of Gland
HIV disease
Lymphoma
Cancer of the Salivary
Gland
Infection of gland
(TBC, Actinomycosis)
Head & neck radiotherapy

The most difficult and common questions involve
the diagnosis and treatment of the patients with
vague complaints of dryness, fatigue, cognitive
dysfunction, arthralgias and low titer ANA
Clinical Issues of Diagnosis of fatigue
Primary Sjogren’s (high ESR, CRP)
Hypothyroid
Drug toxicity
Sleep disorder
(nocturnal myoclonus)
Fibromyalgia with
Low titer ANA
and
depression

• Past confusion over criteria
• San Diego criteria (0.5% incidence) versus
• Original EEC criteria (5% incidence)
• Now clarified
• With new proposed international
• criteria
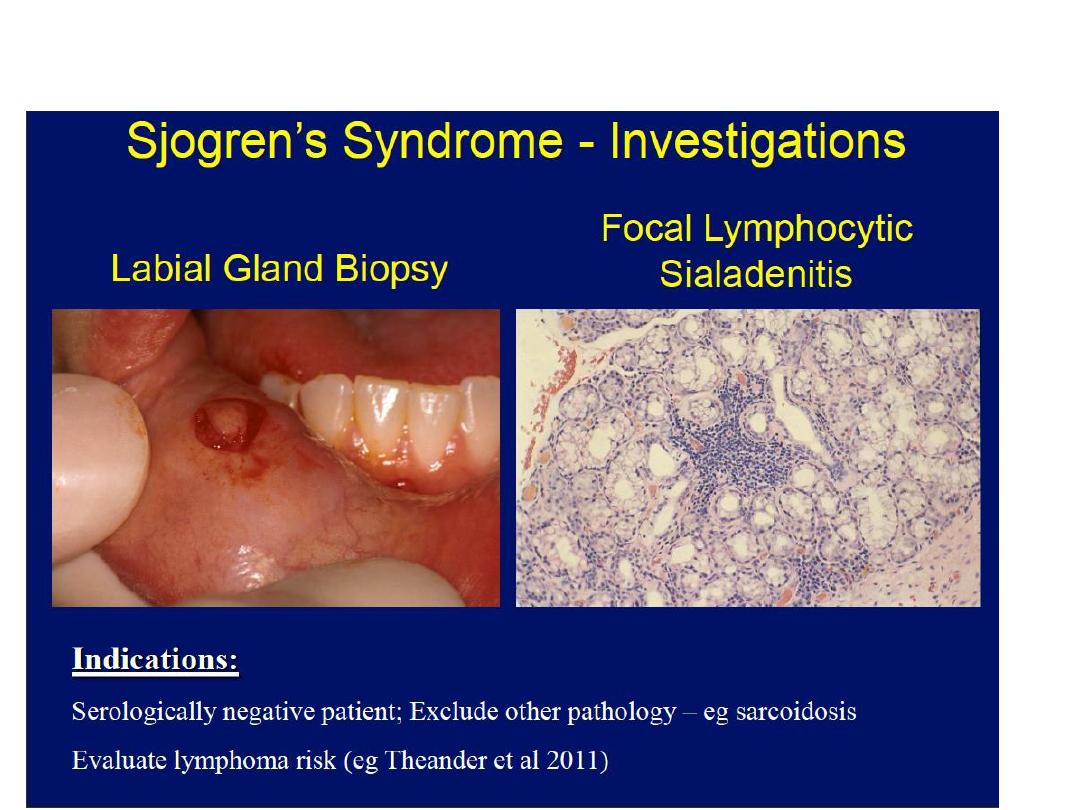
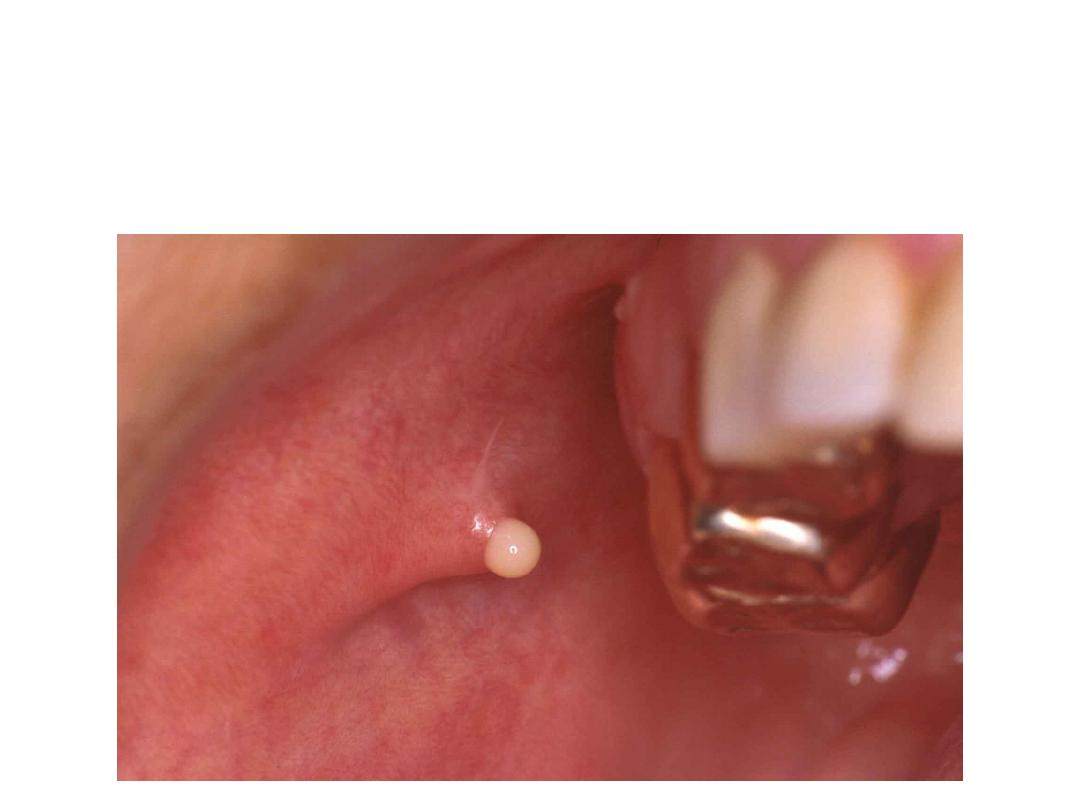
Submitted criteria (11/01) by International SS
advisory board
Will require either
A positive minor salivary gland biopsy
Or
Antibody against SS-A (Ro)
New international criteria-1
1. Ocular Symptoms
2. Oral Symptoms
3. Salivary gland function
(flow rate by flow rate, scan, or sialography)
AND
4. Histopathology (focus score > 1)
5. Autoantibody to SS-A or SS-B
New international criteria-2
New Criteria for SS (cont’d)
Exclusions
Pre-existing lymphoma, sarcoid
Hepatitis B or C
Drugs with Anticholinergic side effects
(measurements of tear/saliva with patient off drug
for 3 half lives)
Caution in interpreting studies on clinical associations
published during past several years-since results will
depend on the inclusion criteria
For example:
A) On disease associations (esp. liver-as hepatitis
C now now an exclusion)
B) “Primary” Fibromyalgia patients now excluded

How good are our tests?
The lip biopsy and the
the ANA and anti-SS A antibody
are often considered “specific” tests
but they are not specific
Pitfalls in diagnosis-1
A) Positive ANA does not mean Sjogren’s or SLE
These tests are sensitive but not specific
(only about 1:100 patients with ANA 1:320 will
have SS or SLE)
B) anti SS-A antibody more specific-but differences
between detection kits
The ANA is sensitive but not specific
The ANA should not be used as a screen
for Sjogren’s or SLE
but to confirm a clinical diagnosis
ANA 1:80 present in 20% of normals
(esp. in fibromyalgia patients)
This is important since some aggressive physicians
have actually treated fibromyalgia patients for their
fatigue with cyclophosphamide thinking that it was
CNS vasculitis
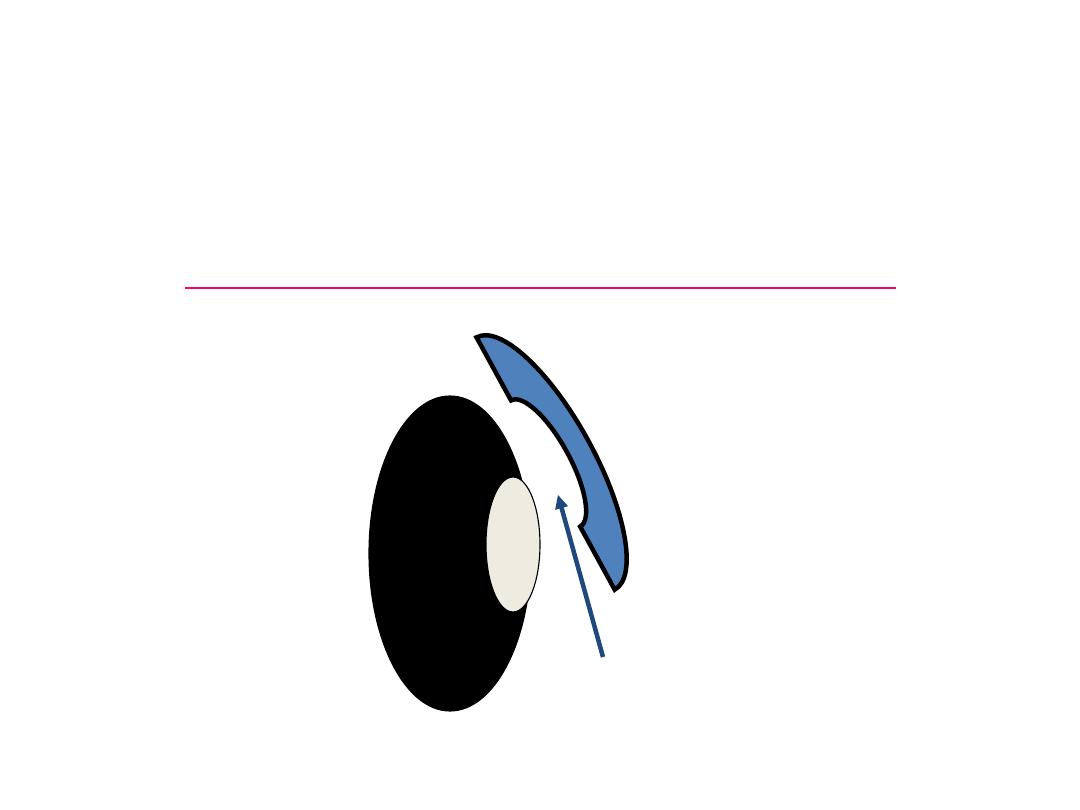
Normally the upper eyelid
glides over the globe on a coating called the tear film
composed
of water, protein, mucins
orbit
eyelid
Tear film
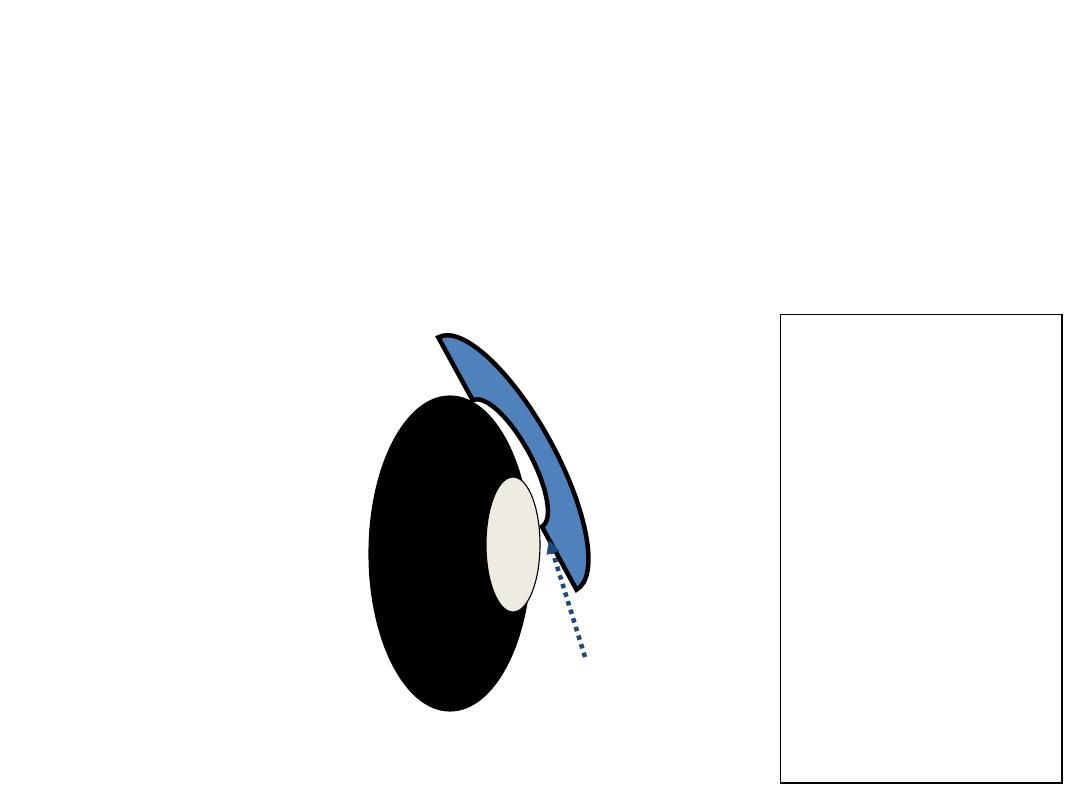
When the tear film is inadequate,
The upper lid sticks to the surface of the orbit and
Actually pulls of the surface layer of the ocular
surface
orbit
eyelid
Tear film
The
Sjogren’s
patient is
describing
increased
friction as
the upper
lid moves
over the globe
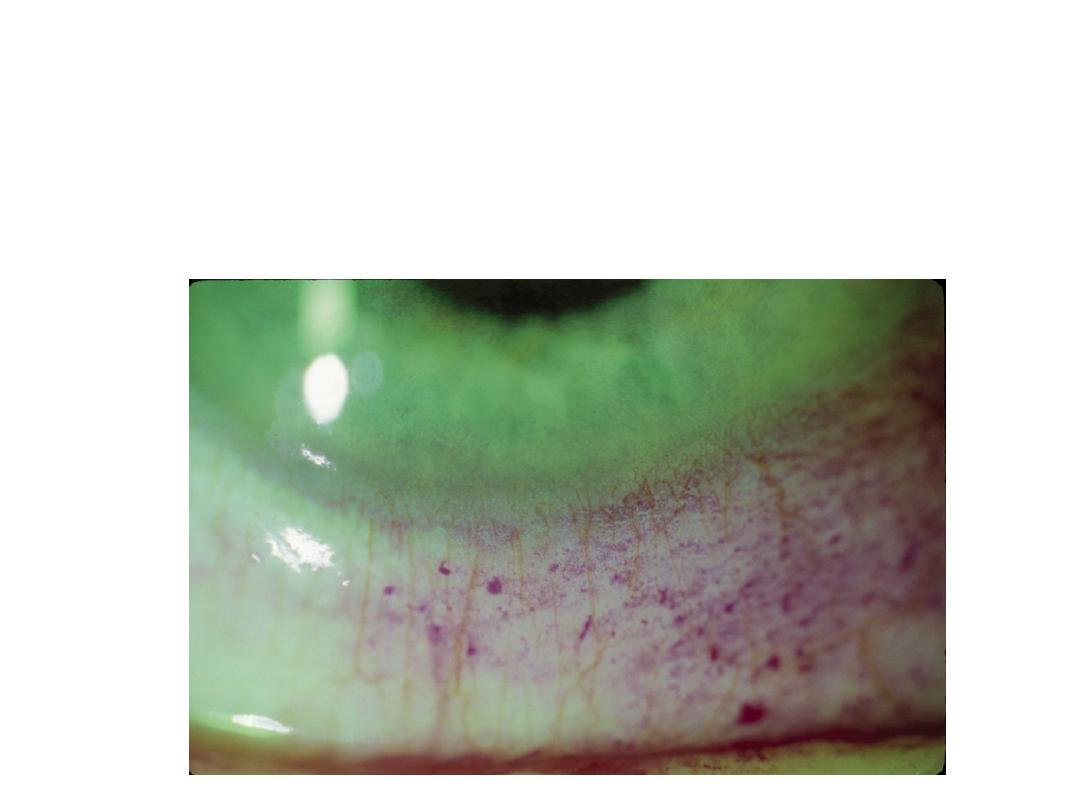
Dryness results in the clinical appearance of
keratoconjunctivitis sicca (KCS)
characteristic of Sjogren’s syndrome

The Sjogren’s Syndrome with
swollen parotid gland
The concern is infection or
lymphoma
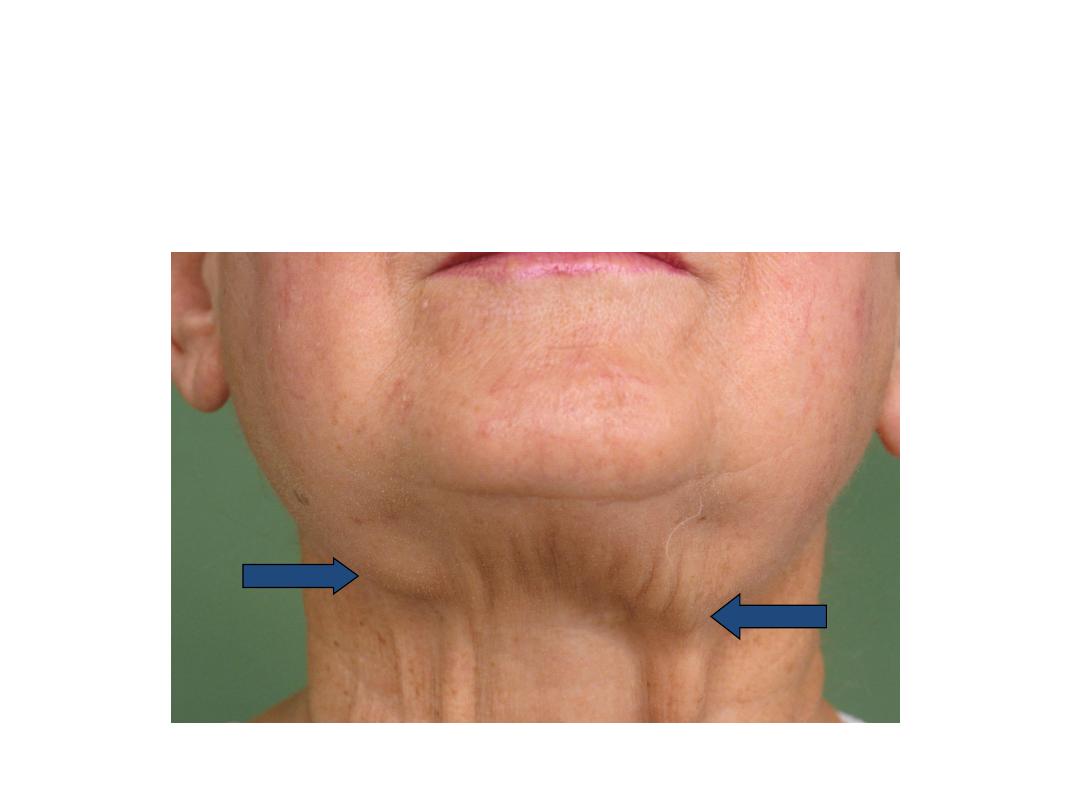
Sjogren’s Syndrome - Diffuse Submandibular
Salivary Gland Enlargement
Sjogren’s Syndrome - Ascending Salivary
Gland Infection
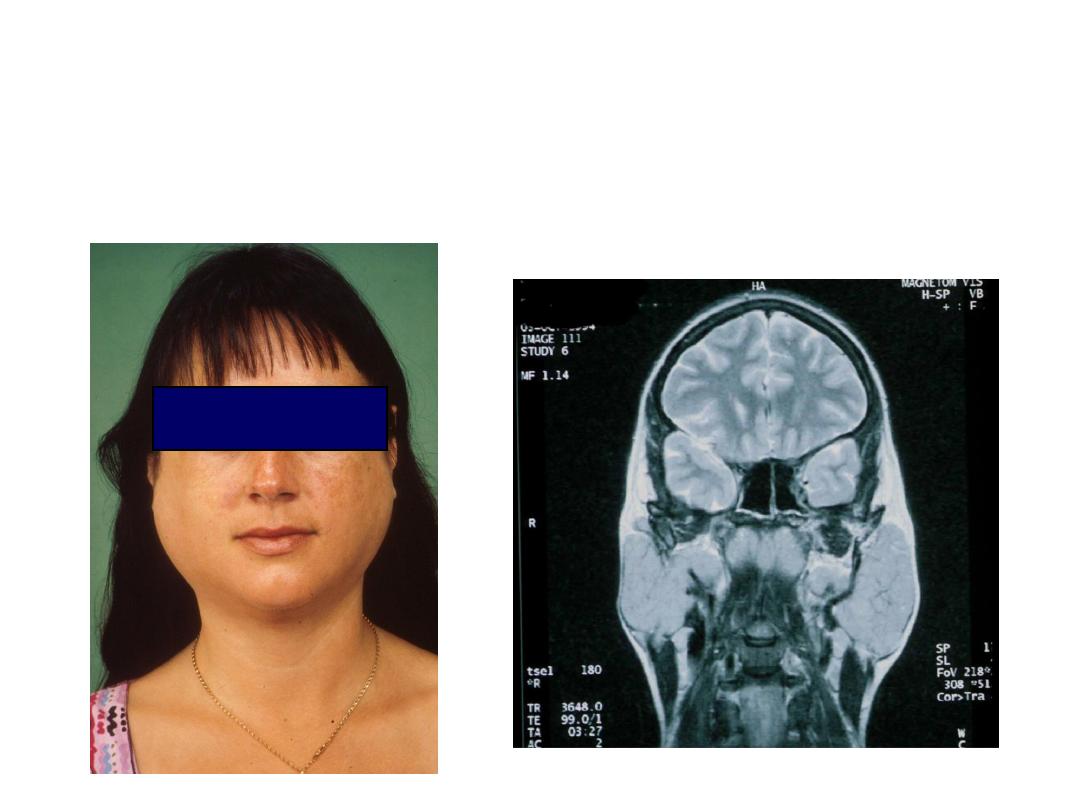
Sjogren’s Syndrome - Investigations
MRI

If you order an MRI
1. Ask for MRI -sialography (this is just a fat
suppression view to visualize the ducts). It takes
only 5 minutes more and no risk
2. Have the MRI printed out on CD and give copy to
patient for their record

Although the systemic manifestations
can occur in Sjogren’s as in SLE, there
are some subtle differences
Extraglandular Manifestations of Sjogren’s Syndrome
Is Sjogren’s syndrome just SLE with 4 criteria?
It is best to think of SLE as a disease mediated by
antibody and immune complex damage
It is best to think of Sjogren’s as a disease
mediated by cell infiltration into tissues
There is a great deal of overlap, but also
differences
SS
Lupus
Extraglandular manifestations
Sjogren’s syndrome
Skin-hyperglob purpura…….
Lung-interstitial pneumonitis
Renal-interstitial nephritis…
Cardiac-pulmonary
hypertension..
Hematologic--lymphoma….
Neurologic-peripheral
neuropathy
Esophageal-dysphagia and
tracheal reflux
SLE
Skin-leukocytoclastic
vasculitis
Lung-pleural effusions
Renal-
glomerulonephritis
Cardiac-pericarditis
Hematologic-ITP,
hemolytic anemia
Neuropathy-
mononeuritis multiplex

SS and SLE are more similar than dissimilar
•
The genetics of SS are remarkably similar to a
subset of SLE (i.e.. HLA-DR3)
•
The pattern of auto-antibodies are similar,
including SS-A in SLE patients
•
Most importantly, the response to therapies are
similar
Systemic therapy-1
In general, similar to SLE
Steroids work and the question is how to get the
patients off steroids
Systemic therapy-2
Usually start with hydroxychloroquine or
methotrexate for rash or arthralgias

Systemic therapy-3
For severe visceral vasculitis, still use
cyclophosphamide (pulse) But try to use less than 6
cycles and then try Leflunomide, mycophenolic acid
anti-CD20 (Rituxin)

Systemic therapy-4
Recent preliminary report that infliximab (Remicade)
Published (Steinberg, 2003)
But a larger multicenter trial
Presented at American College of Rheumatology
Did not show benefit of TNF inhibitor
difficult problems
Fatigue
Cognitive
Nerve
pain

Prognosis
• Sjögren syndrome carries a generally good
prognosis. In patients who develop a disorder
associated with Sjögren syndrome, the prognosis is
more closely related to the associated disorder (eg,
SLE, lymphoma). Interestingly, primary Sjögren
syndrome is associated with lower cardiovascular
risk factors and lower risk of serious cardiovascular
events such as myocardial infarction and stroke, in
comparison with SLE

Morbidity and mortality
• Morbidity associated with Sjögren syndrome is
mainly associated with the gradually decreased
function of exocrine organs, which become
infiltrated with lymphocytes. The increased
mortality rate associated with the condition is
primarily related to disorders commonly associated
with Sjögren syndrome, such as SLE, RA, and
primary biliary cirrhosis. Patients with primary
Sjögren syndrome who do not develop a
lymphoproliferative disorder have a normal life
expectancy

Lymphoma
• Among patients with Sjögren syndrome, the
incidence of non-Hodgkin lymphoma is 4.3% (18.9
times higher than in the general population), with a
median age at diagnosis of 58 years. The mean time
to the development of non-Hodgkin lymphoma
after the onset of Sjögren syndrome is 7.5 years.

Risk factors for lymphoma include the following;
Salivary gland enlargement
Regional or generalized lymphadenopathy
Hepatosplenomegaly
Palpable purpura
Leukopenia
Renal insufficiency
Loss of a previously positive polyclonal gammopathy
Development of a monoclonal gammopathy or a
monoclonal cryoglobulinemia
RF positivity
Anti-SSA/SSB positivity
Hypocomplementemia

Summary-1
1. New diagnostic criteria are developed that should
diminish confusion in clinical practice and in the
research literature
2. There is variability in reading minor salivary gland
biopsies and interpretation of positive ANA’s

Sjogren’s syndrome has clinical features and
treatment that are generally similar to SLE
But the Sjogren’s patient has particular needs in
terms of the medications they tolerate and particular
disease manifestations.

MCQ
• These suggest sjogren syndrome except
• 1-friction senseation of eye
• 2-candidasis of mouth
• 3-skin rash
• 4-postive HIV TEST
• 5-postive ANA TEST

• These suggest lymphoma in sjogren except
• 1-rash
• 2-hillar LN enlargment
• 3-splenomegaly
• 4-Increase parotid swelling
• 5-lymphopenia
• you have 2 disease select the best
statement for each from these
• A-LUPUS [ ][ ][ ][ ]
• B-SJOGREN[ ][ ][ ] [ ]
•
• a-antiDNA ,b-antiRo , ,c-schemer test, d-lip
biopsy ,e-MRI brain ,f-S creatinine ,g-lung
CT SCAN,H-Psychiatric assessment.
