Arrhythmia in pediatric age group
The normal heart rate varies with age. The younger the child, the faster the heart rate. Therefore, the
definitions of bradycardia (<60 beats/minute) and tachycardia (>100 beats/minute) used for adults do
not apply to infants and children. Tachycardia is defined as a heart rate beyond the upper limit of
normal for the patient's age, and bradycardia is defined as a heart rate slower than the lower limit of
normal
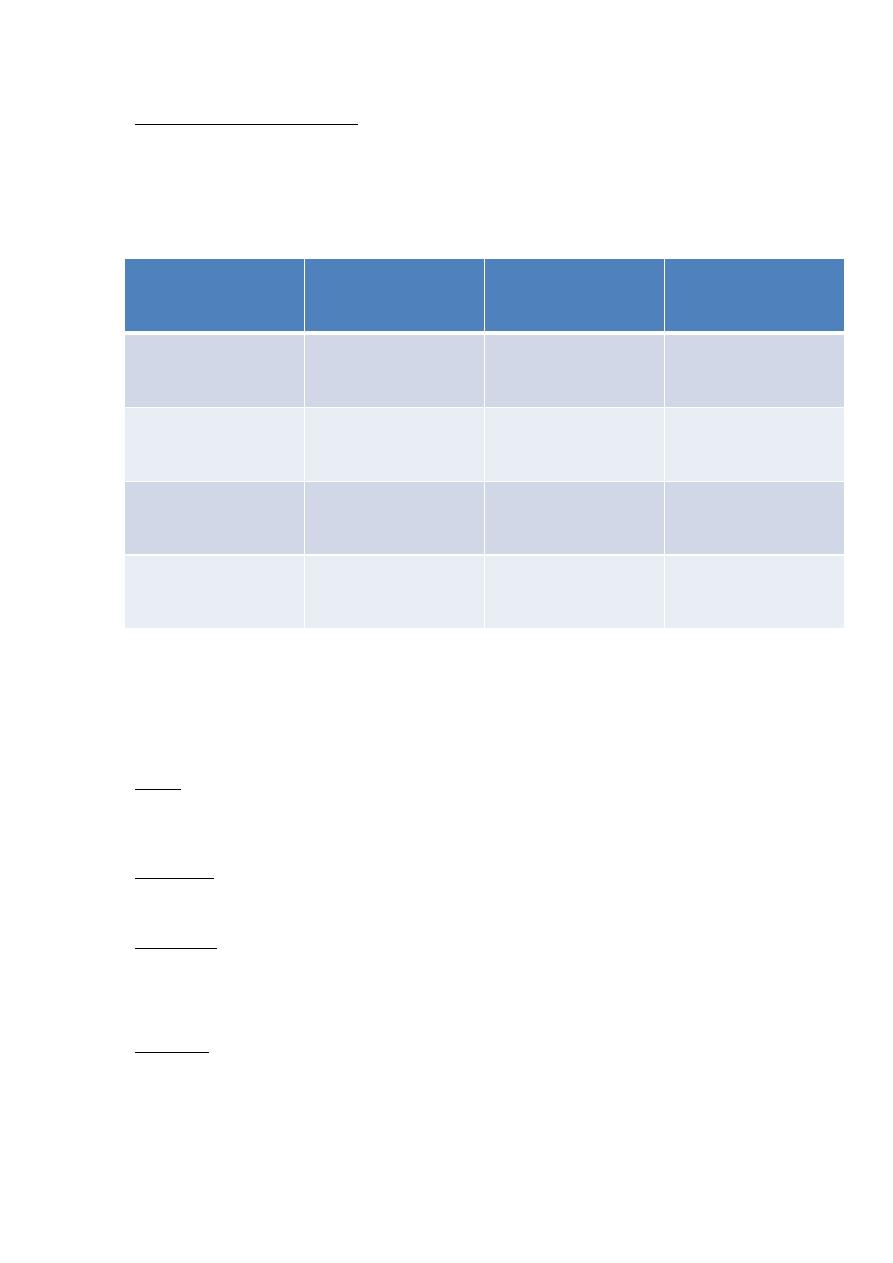
Age
Mean (range)
Age
Mean (range)
Newborn
145 (90–180)
4yr
108 (72–135)
6 mo
145 (106-185)
6yr
100 (65–135)
1 yr
132 (105-170)
10yr
90 (65–130)
2 yr
120 (90–150)
14yr
85 (60–120)
SINUS TACHYCARDIA
Characteristics of sinus rhythm are present . The rate is faster than the upper limit of normal for age .A
rate greater than 140 beats/minute in children and greater than 170 beats/minute in infants may be
significant. The heart rate is usually less than 200 beats/minute in sinus tachycardia
Causes
Anxiety, fever, hypovolemia or circulatory shock, anemia, congestive heart failure (CHF),
administration of catecholamines, thyrotoxicosis, and myocardial disease are possible causes.
Significance
Increased cardiac work is well tolerated by healthy myocardium.
Management
The underlying cause is treated
SINUS BRADYCARDIA
Description
The characteristics of sinus rhythm are present (see previous description), but the heart rate is slower
than the lower limit of normal for the age .A rate slower than 80 beats/minute in newborn infants and
slower than 60 beats/minute in older children may be significant

Causes
Sinus bradycardia may occur in normal individuals and trained athletes. It may occur with vagal
stimulation, increased intracranial pressure, hypothyroidism, hypothermia, hypoxia, hyperkalemia, and
administration of drugs such as digitalis and β-adrenergic blockers.
Significance
In some patients, marked bradycardia may not maintain normal cardiac output.
Management
The underlying cause is treated.
SUPRAVENTRICULAR TACHYCARDIA
The heart rate is extremely rapid and regular (usually 240 ± 40 beats/minute).
Causes
1-No heart disease is found in about half of patients. This idiopathic type of SVT occurs more
commonly in young infants than in older children.
2-WPW preexcitation is present in 10% to 20% of cases, which is evident only after conversion to
sinus rhythm.
3-Some congenital heart defects (e.g., Ebstein's anomaly, single ventricle, and congenitally
corrected transposition of the great arteries) are more susceptible to this arrhythmia.
4-SVT may occur following cardiac surgeries.
Significance
1-SVT may decrease cardiac output and result in CHF.
2-Many infants tolerate SVT well. If the tachycardia is sustained for 6 to 12 hours, signs of CHF
usually develop.
3-Clinical manifestations of CHF include irritability, tachypnea, poor feeding, and pallor. When
CHF develops, the infant's condition can deteriorate rapidly. Older children may complain of chest
pain, palpitation, and shortness of breath, lightheadedness, and fatigue.
Management
1-Vagal stimulatory maneuvers (unilateral carotid sinus massage, gagging, and pressure on an
eyeball) may be effective in older children but are rarely effective in infants. Placing an ice-water
bag on the face (for up to 10 seconds) is often effective in infants (by diving reflex).
2-Adenosine is considered the drug of choice. It has negative chronotropic, dromotropic, and
inotropic actions with a very short duration of action (half-life <10 seconds) and minimal
hemodynamic consequences. Adenosine is effective for almost all reciprocating SVT (in which the
AV node forms part of the reentry circuit) and for both narrow- and wide-complex regular
tachycardia. It is not effective for irregular tachycardia. It is not effective for non-reciprocating
atrial tachycardia, atrial flutter or fibrillation, and ventricular tachycardia, but it has differential
diagnostic ability. Its transient AV block may unmask atrial activities by slowing the ventricular
rate and thus help to clarify the mechanism of certain supraventricular arrhythmias
Adenosine is given by rapid IV bolus followed by a saline flush, starting at 50 μg/kg, increasing in
increments of 50 μg/kg every 1 to 2 minutes. The usual effective dose is 100 to 150 μg/kg with
maximum dose of 250 μg/kg.
3. If the infant is in severe CHF, emergency treatment is directed at immediate cardioversion. The
initial dose of 0.5 joule/kg is increased in steps up to 2 joule/kg.
4. Esmolol, other β-adrenergic blockers, verapamil, and digoxin have also been used with some
success. Intravenously administered propranolol has been commonly used to treat SVT in the
presence of WPW syndrome. IV verapamil should be avoided in infants younger than 12 months
because it may produce extreme bradycardia and hypotension in infants.
5. For postoperative atrial tachycardia (which requires rapid conversion), IV amiodarone may
provide excellent results. The side effects may include hypotension, bradycardia, and decreased
left ventricular (LV) function.
6. Overdrive suppression (by transesophageal pacing or by atrial pacing) may be effective in
children who have been digitalized.
7. Radiofrequency catheter ablation or surgical interruption of accessory pathways should be
considered if medical management fails or frequent recurrences occur. Radiofrequency ablation
can be carried out with a high degree of success, a low complication rate, and a low recurrence rate
After termination of SVT send child for
1- ECG to exclude prexcitation syndrome
2- Echo for structural heart disease as cardiomyopathy and Ebstien anomaly
3- Thyroid function test and serum electrolyte
Prevention of Recurrence of SVT
1-In infants without WPW preexcitation, oral propranolol for 12 months is effective. Verapamil
can also be used but it should be used with caution in patients with poor LV function and in young
infants.
2- In infants in CHF and ECG evidence of WPW preexcitation, one may start with digoxin (just to
treat CHF), but digoxin should be switched to propranolol when the infant's heart failure improves.
3- In infants or children with WPW preexcitation on the ECG, propranolol or atenolol is used in the
long-term management. In the presence of WPW preexcitation, digoxin or verapamil may increase the
rate of antegrade conduction of the impulse through the accessory pathway and should be avoided
ock
Heart bl
First-Degree Atrioventricular Block
Description.
The PR interval is prolonged beyond the upper limits of normal for the patient's age and heart rate
Causes.
First-degree AV block can appear in otherwise healthy children and young adults, particularly in
athletes. Other causes include congenital heart diseases (such as endocardial cushion defect, atrial

septal defect, Ebstein's anomaly), infectious disease, inflammatory conditions (rheumatic fever),
cardiac surgery, and certain drugs (such as digitalis, calcium channel blockers).
Significance.
First-degree AV block does not produce hemodynamic disturbance. It sometimes progresses to a more
advanced AV block.
Management.
No treatment is indicated, except when the block is caused by digitalis toxicity
Second-Degree Atrioventricular Block
MOBITZ TYPE I
Description.
The PR interval becomes progressively prolonged until one QRS complex is dropped completely
Causes.
Mobitz type I AV block appears in otherwise healthy children. Other causes include myocarditis,
cardiomyopathy, myocardial infarction, congenital heart defect, cardiac surgery, and digitalis toxicity.
Significance.
The block is at the level of the AV node. It usually does not progress to complete heart block.
Management.
The underlying causes are treated.
•
MOBITZ TYPE II
Description.
The AV conduction is “all or none.” AV conduction is either normal or completely blocked
Causes.
Causes are the same as for Mobitz type I.
Significance.
The block is at the level of the bundle of His. It is more serious than type I block because it may
progress to complete heart block
Management.
The underlying causes are treated. Prophylactic pacemaker therapy may be indicated
Third-Degree Atrioventricular Block
Description.
In third-degree AV block (complete heart block), atrial and ventricular activities are entirely
independent of each other

1
.
The P waves are regular (regular P-P interval), with a rate comparable to the normal heart rate
for the patient's age. The QRS complexes are also regular (regular R-R interval), with a rate
much slower than the P rate.
2
.
In congenital complete heart block, the duration of the QRS complex is normal because the
pacemaker for the ventricular complex is at a level higher than the bifurcation of the bundle of
His. The ventricular rate is faster (50 to 80 beats/minute) than that in the acquired type, and
the ventricular rate is somewhat variable in response to varying physiologic conditions.
3
.
In surgically induced or acquired (after myocardial infarction) complete heart block, the QRS
duration is prolonged because the pacemaker for the ventricular complex is at a level below
the bifurcation of the bundle of His. The ventricular rate is in the range of 40 to 50
beats/minute (idioventricular rhythm) and the ventricular rate is relatively fixed.
Causes
Congenital Type.
Causes are an isolated anomaly (without associated structural heart defect), structural heart disease
such as congenitally corrected transposition of the great arteries, or maternal diseases such as systemic
lupus erythematosus, Sjögren's syndrome, or other connective tissue disease.
Acquired Type.
Cardiac surgery is the most common cause of acquired complete heart block in children. Other rare
causes include severe myocarditis. Lyme carditis, acute rheumatic fever, mumps, diphtheria,
cardiomyopathies, tumors in the conduction system, overdoses of certain drugs, and myocardial
infarction. These causes produce either temporary or permanent heart block.
Significance
1
.
Congestive heart failure (CHF) may develop in infancy, particularly when there are associated
congenital heart defects.
2
.
Patients with isolated congenital heart block who survive infancy are usually asymptomatic
and achieve normal growth and development for 5 to 10 years. Chest x-ray films may show
cardiomegaly.
3
.
Syncopal attacks (Stokes-Adams attacks) may occur with a heart rate below 40 to 45
beats/minute. A sudden onset of acquired heart block may result in death unless treatment
maintains the heart rate in the acceptable range.
Management
1
.
Atropine or isoproterenol is indicated in symptomatic children and adults until temporary
ventricular pacing is secured.
2
.
A temporary transvenous ventricular pacemaker is indicated in patients with heart block, or it
may be given prophylactically in patients who might develop heart block.
3
.
No treatment is required for children with asymptomatic congenital complete heart block with
acceptable rate, narrow QRS complex, and normal ventricular function.
