
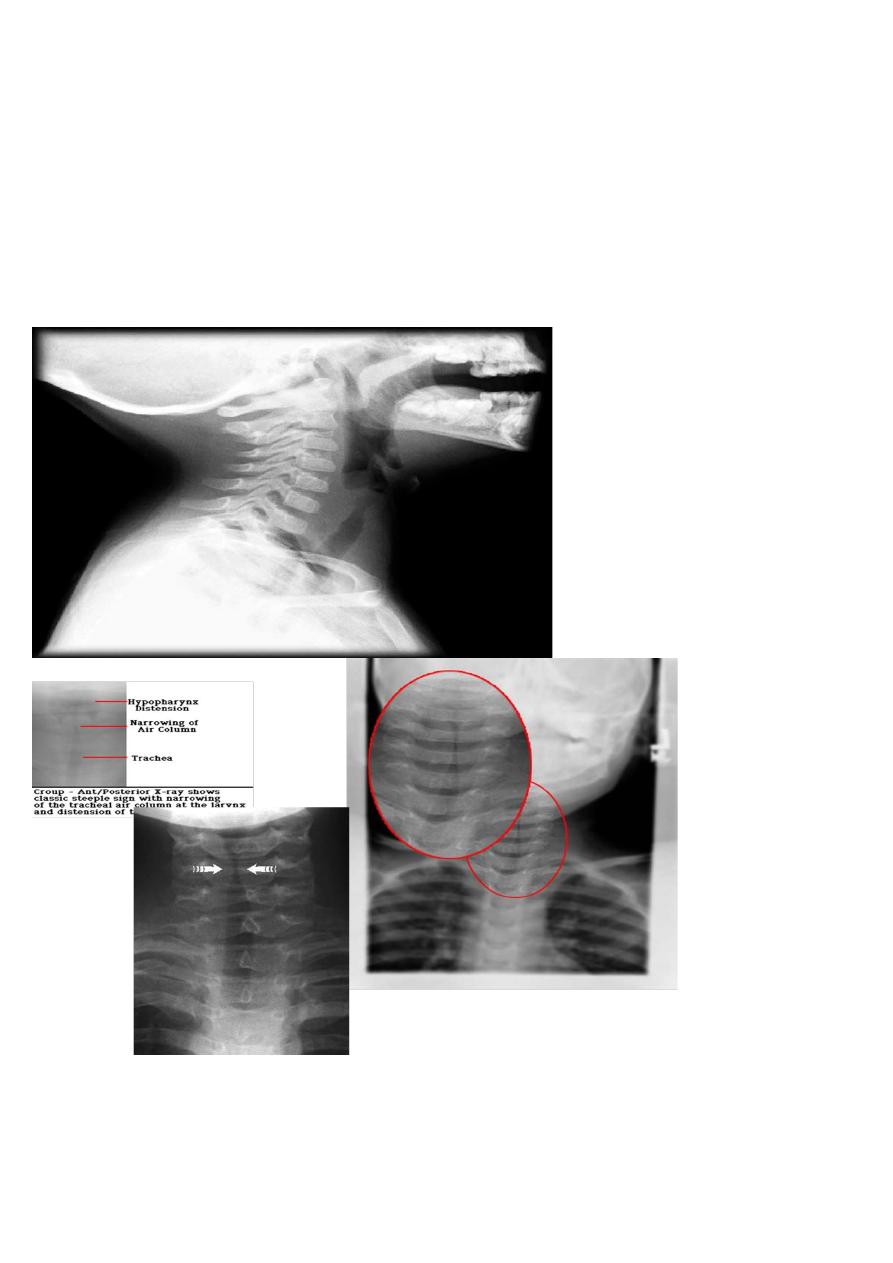
Treatments of croup :---
most afebrile children with spasmodic croup & mild ALTB can usually be safely effectively
managed at home
Treatments of underlying & often unsuspected G.E.R. may prevent spasmodic croup .
Treatment at home by :---
1-steam from a shower or bath in a close bath room. Or
2-steam from a vaporize or
3- cold steam from a nebulizer .
•
This will result in terminating in acute laryngeal spasm & respiratory distress within
minutes ( same effect by cold night air) G.O.R ( gastro esophageal reflux ).
•
Also can use IPECAC to induce vomiting resulting decreasing spasm, although vomiting
appear to break spasm .
•
In hypoxic infant , given O2 of less than 100% saturated with H2O vapor resulting in
mucosal cooling leading vaso constriction & decrease edema .
Treatments of patients at hospital :--
indication of admission :--
1- highly or suspected epiglotitis
2-
progressive strider
3- sever strider at rest
4-
sign of resp. distress like hypoxia , irritable , cynosis , sever pallor , depressed
sensorium .
For patients who admitted :--
1-
chart observation ( PR ,RR ):--.increasing resp. rate is first sign of hypoxia
2-
parenteral fluid :- given to replace insensible H2O loss or because of inability to take oral
feeding & decreased risk of aspiration pneumonia.
3-
sedation is Contra indication ( because of restless is used as clinical indices of severity of
obstruction & need for tracheostomy or endotracheal intubation )
4-
children should be kept calm as possible to reduce resp. effort
5-
O2 to alleviate hypoxia ( humidified O2 )
6-
brocho-dilator & expectorant are not helpful & A.B. is not indicated
7-
Racemic epinphrine ( o.25 -0.75 ml of 2.25% in 3 ml normal saline can be used every 20
minutes causing transient relief of symptoms through vasoconstriction of precapillary
arteriol leading fluid resorption from interstitial space and decrease edema .
•
Or used L-epinpherine ( 5 ml of 1:1000 solution ) is equally effective as Racemic
epinpherine . Nebulized epinpherine should still be used cautiously in patient
with
Tachycardia or heart condition like TOF, ventricular outlet obstruction .
8-
cortico steriod to reduce inflamatory edema & prevent destructed celiated epithilial ( 0ral
dexamethazone 0.6 mglKg as
Single dose & may be 0.15mglkg may be just effective .
I.M
decadron & nebulized budesonide have an equally effective
.
9- tracheostomy in sever cases with progressive strider & cynosis.
Indication of laryngoscope in croup :--
1-very young of less than 4 month of age .
2- if symptoms continue of more than one wk
3- patients with 2 or more episode of croup and that had history of intubation and age less than
3 years or had sever prolong disease required inpatient management .
• laryngoscopy is to exclude sub-glotic stenosis or hemangioma.
• Pt can be safely discharge after 2-3hr period of observation , if 1- normal air entery,2-
normal conscience,3- no strider at rest 4-,received steriod,5- normal pulse oximetry .
• N.T ; very young pts of less than 4 month of age or symptoms continue more than one week
, the pt should undergo laryngoscopy to exclude subglotic stenosis or hemangioma

Bacterial trachitis ;---
is acute bacterial infection of trachea which able to obstruct air way. Age of incidence of less
than 3 years but in more recent cases , the recently , the mean age between 5 & 7 years .
•
causes by staph. aureus (most common ) but PIV type 1 & H influenza , moraxalla
catarrhalis & anarobic organism also been implicated .
•
Usually follow viral resp. infection especially croup .
ClF :---
1- history of croup, followed by high fever , toxic associated respiratory distress or may occur
few days after improvement .
2- patients lie flat , not drool , no dysphagia .
3- not respond to general treatment of croup .
•
intubation & tracheostomy is usually required ( but in more recent series , only 50-60 % of
patients required intubation ).
Pathology :--
1- mucosal swelling at level of cricoid cartilage .
2- thick copious , purulent secretion .
Diagnosis :--
1- ClF
2- 2- WBC leucocytosis with band form
3- X-ray is not needed , &may show classical feature pseudomembrane detachment in the
larynx . 4- laryngoscopy shows purulant material bellow cord .
Treatment :--
1- supporting :- O2 therapy , I.V fluid , intubation in sever cases
2- specific therapy by A .B ( anti staph )
CX :---
1- resp. obstruction leading to resp. arrest
2- infection go down to parenchymal or bronchiol leading to pneu.
4- toxic shock syndrome
•
Now# emperical therapy :-vancomycin + naficilin or cloxacillin & artificial air way should
be strongly considered .

•
Prognosis :- become a febrile patient within 2-3 days but may be prolonged Hospitalization
may be nesessory ( mean duration is 12 days ).
Lower air way obstruction ;-
DD :-- of wheezing :---
1- infection :- bronchiolitis , pneumonia .
2- asthma
3-anotomical abnormalities like :-
A– central air way like malasia of larynx , trachea, bronchi .
B-extrinsic air way anomalies by compression like vascular ring , mediastinal LAB , F.B in
esophagus .
C- intrinsic air way anomalies like hemangioma , cyst , sequestration , F.B, CHD( LF to Rt shunt )
. 4- cystic fibrosis , bronchioactasis .
5- aspiration pneumonia , G.E.R 6- H.F 7- interstitial lung disease like bronchiolitis
obliterance 8- anaphylaxis .
Bronchiolitis :---
is common dis. of LRTI of infant , is resulting from inflammatory.
Obst. Of small air way and bronchiol , characterized by wheezing .
•
It occurs in Ist year of life with peak incidence of 6 month , Its incidence is highest in the
winter & early spring .
•
illness occurs sporadically & epidemically .
Etiology :-- is viral in origin in more than 50% by RSV, also can caused by PIV type 3 & some of
adeno virus , mycoplasma . is more common in male infant ( 3-6 month) who not breast fed
infant , lived in crowded condition . also other member of family is ill .
Pathophysiology :---
•
Invasion of bronchiol resulting in mucosal edema and accumulation of mucous and debris
lead to air way resistance in both inspiration and expiration but because of radius of air
way during expiration is smaller, resulting in ball valve like mechanism which allow to
enter air during inspiration and prevent to exist during expiration causing early air
trapping causing over inflation of chest and atelectasis may occur if obstruction is
completed leading to absorbed trapped air causing impairment of gas exchange i.e VPM
lead to hypoxia in early onset of diseases , where hypercapnia not usually occur except in
severely affected infant .
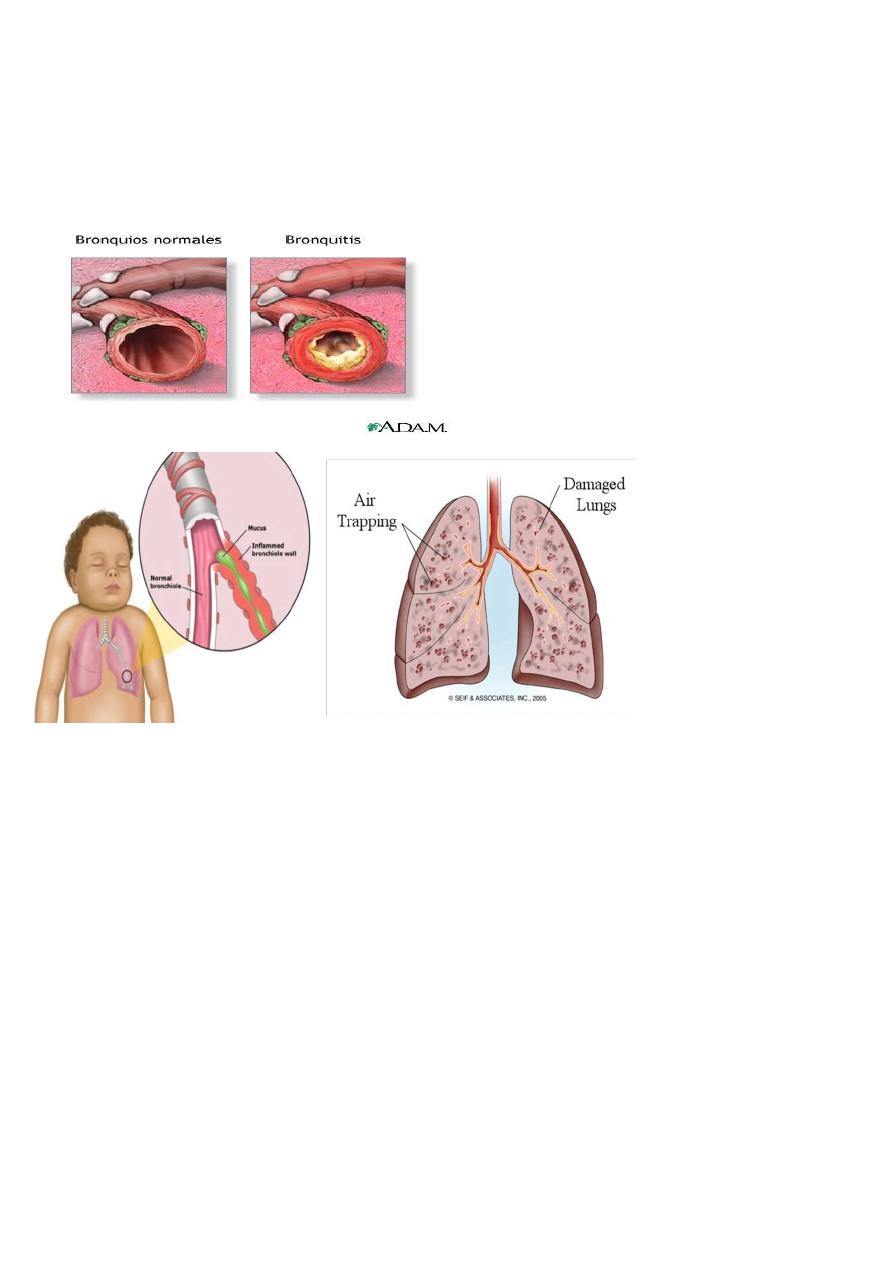
•
Higher respiratory rate lead to decreased arterial O2 tension ( where hypercapnia not
occur unless respiratory rate exceed 60 breath /min. and then increased in proportion to
tachypnea .
Inflamed bronchiol
ClF :--
1- usually other member of family were ill by viral infection .
2-usually proceeded by URTI of few days before onset of resp. distress which include dyspnea ,
tachypnea , wheezing , intermittent cynosis
3-low grade fever 38.5—39c & other systemic manifestations like vomiting & diarrhea are
usually absent.
•
Apnea more prominent than wheezing in early course of dis. In very young infant of less
than 2 month of age or former premature infant .
On Examination :- --
1- resp. distress which variable from mild to sever .
2- in sever distress with sever hypoxia lead to convulsion &dehydration due to insensible water
loss .

Diagnosis :----
1- ClF
2- X-ray finding ( hyper inflation of chest , scattered area of consolidation in 30% caused by
atelectasis which secondary to obstruction or inflammation of alveoli .
3- WBC & diffrential count are usually normal .
DD :--
1-asthma 2- bronchopneumonia 3- F.B aspira.
4- cong. H.F 5- poisoning 6- pertusis
7- cystic fibrosis
•
Note :-- 50% of sever bronchiolitis may going to asthma
•
Course :-- most critical period is 2-3 days after onset of cough & dyspnea. & then
improvement occurs rapidly & recovery is completely within several days ( 10-14 days )
•
Death rate :-- is less than 1
% ( higher figures associated with higher risk groups ) , caused
by :---
1- prolong apneic spell
2- sever uncompansated resp. acidosis
3- profound dehydration
•
Infant are more liable to morbidity & mortality if associated :-- 1-CHD 2- BPD
3-Cystic fibrosis 4- immune def. dis. 5-in first 3 month of age if developed H.F is rare CX
except if underlying heart dis.
•
Infant with bronchiolitis who developed asthma , are more likely to
have :-- 1-family history of asthma & allergy
2-prolong acute episode of bronchiolitis
3- exposure to cigarette smoking

Treatment of bronchiolitis :--
•
depend on severity of illness most children have mild illness & can be managed at home
with supporting measures .
•
5% of patients needs hospital admission :----
indication of admission :----
1-younger patients of less than 6 months .
2-moderate to marked resp. distress ( sleeping R.T of more than 50-60 breath / minutes or
higher)
3- hypoxemia ( po2 of less than 50-60 mmHg ) or o2 saturation of less than 92% on room ai
4- episode of apnea
5- inability to tolerate oral feeding
6-lack of appropriate care at home
•
(children with CHD, BPD , NMD, immune def. ---- increasing risk of sever potentially
sever dis.)
Supporting measures :--
1- adequate fluid to maintain normal hydration
2- antipyretic for febrile patients
3- humidified o2 in sufficient concentration to maintain pao2 70-90 mmHg & o2 saturation of
more than 92%
4- broncho-dilator like B-agonist produce short term improvement in clinical feature .
•
nebulized epinpherine may more effective than B-agonist, cortico-steriod are often
negative
5- frequent suction of noze & oral secretion is essential part and often provide relief of distress
or cynosis ( is essential part of treatment of bronchiolitis )
Specific therapy :--
1- ribavirine is antiviral agent administered by aerosol has been used for infant with CHD or
chronic lung dis.
2- no support for RSV immune globuline administered during acute episode of RSV .
prevention ;-
1-hyperimmune globulin to RSV, 2-palivizumam :IM monoclonal Abs during
and before season .
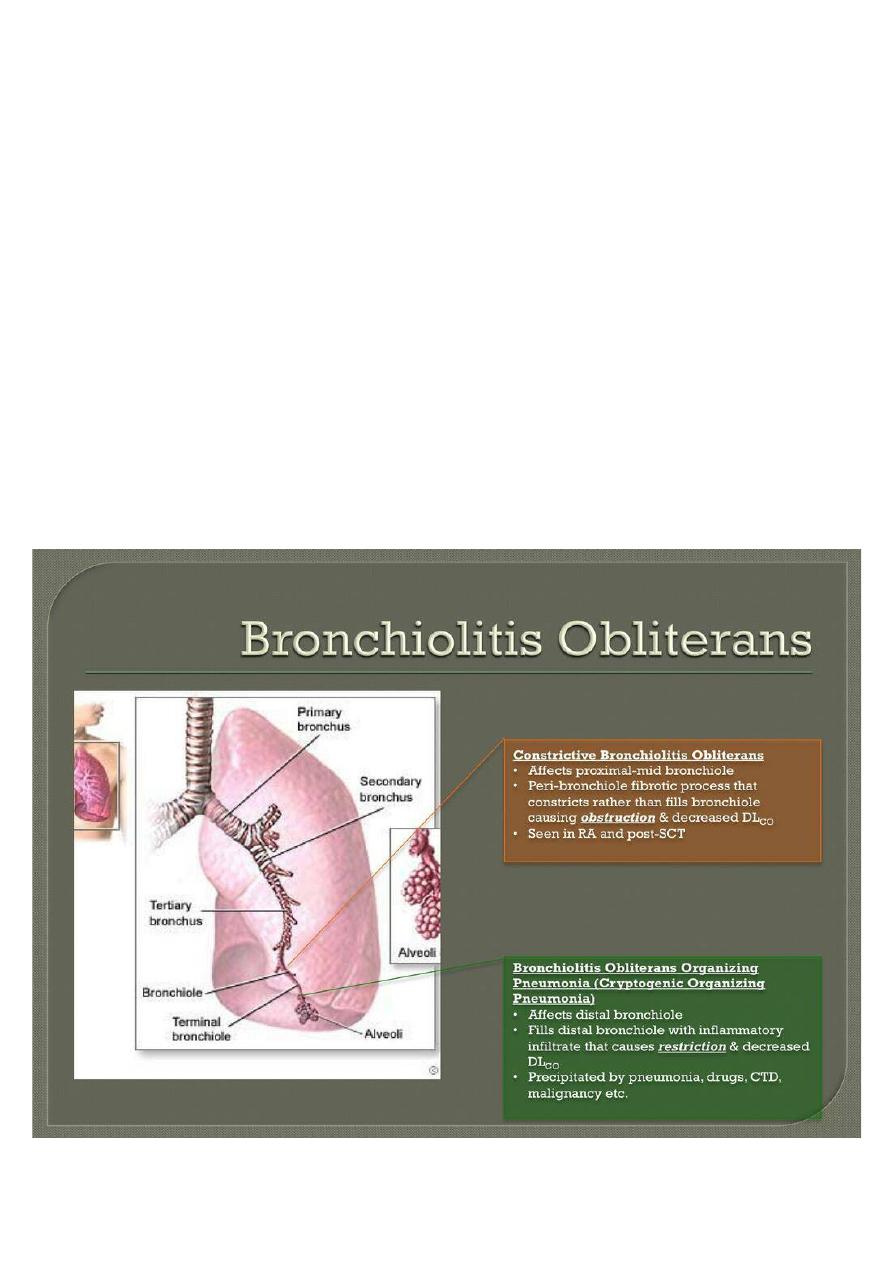
Bronchiolitis obliterane :--
caused by adeno virus , measles , pertusis , in which ,there is damage of bronchiol & smaller air
with attempt repaired by granulation tissue that obstruct the air way , evantually obliterate of
lumen with nodular masses of granulation & fibrosis .
ClF :--
•
gradual progressive resp. distress
•
X-ray :- ranged from normal to a pattern suggest of milliary T.B
•
Bronchography --- :-obstruct of bronchus
•
No specific therapy
Congenital lobar emphysema :---
•
is overinflation of one lobe ( most often left upper lobe ), which produced resp. distress
because of surrounding lung tissue become compressed leading to shifting mediastinum
•
Treatment by lobectomy may be required if resp. distress is sever or progressive .
