1
د.عادل الهنداوي
Injuries of the knee &leg
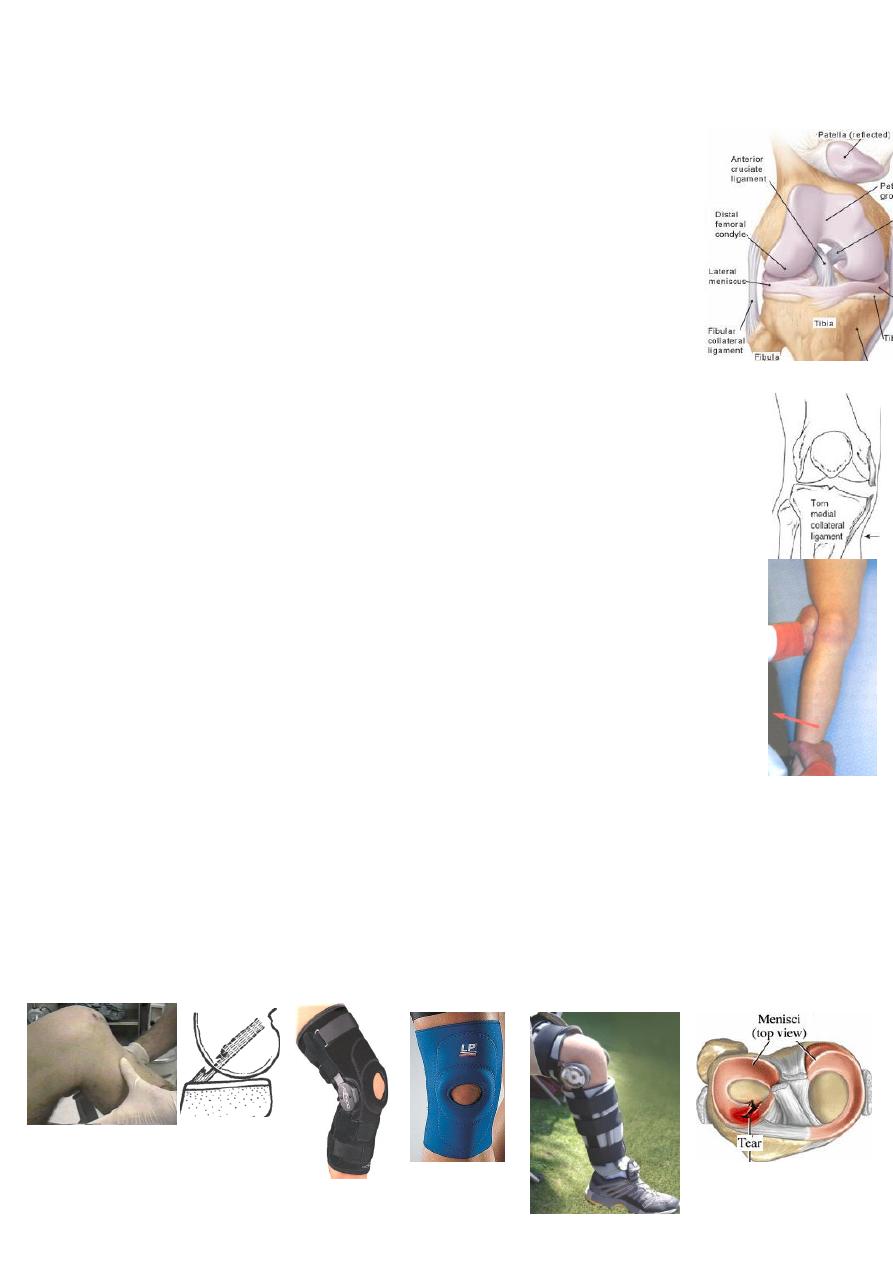
Acute knee ligament injuries:
common in sports &RTA.
Knee stability depends on joint capsule, intra-&extra-articular
ligaments &muscles rather than on bony structures.
MOI: Valgus force→ MCL tear; Valgus+rotation→ MCL+ACL tear;
Valgus+rotation+weight bearing→ MCL+ACL+medial meniscus tear;
Varus force→ LCL tear; Varus + rotation→ LCL + ACL tear;
Dashboard injury→ PCL tear.
CF: history of twisting injury→ immediate painful doughy swelling(hemarthrosis)
while in meniscus injury the swelling is late &fluctuant(synovial effusion).
Look for site of maximum tenderness, bruises &abrasion.
Test for ligament tear:
Partial tear is painful with no abnormal movement,if in doubt→ stress view.
Complete tear→ painless abnormal movement:
If the knee open with valgus or varus stress in 30°flexion→ only collateral tear;
If open in extension→ capsule + collateral + cruciate tear;
Anteroposterior stability: posterior sag→ PCL tear;
anterior drawer test→ ACL; Lachman test→ ACL.
Imaging: X-ray: may show avulsion fracture e.g. ACL may avulse tibial spine.
MRI: to differentiate partial from complete tear.
Arthroscopy: is not indicated in acute complete tear.
Treatment:
Partial tear: aspirate hemarthrosis→ 6weeks functional
brace or crepe bandage with early exercise.
Complete tear: MCL or LCL tear: 6weeks cast-brace→ exercise.
ACL or PCL tear: 6weeks cast-brace→ exercise; later if instability persists→
ligament reconstruction.
Combined collateral + ACL or PCL: 6weeks cast-brace→ exercise→ later
reconstruction.
Complications: 1-adhesion: occurs with partial tear because torn fibers
stick to surrounding structures; CF: attacks of pain &giving way; MRI differentiate
it from meniscus tear; Ŗ: physiotherapy.
2-instability: the knee continue to give way→ OA.
2
Fractured tibial spine:
is the adolescent variant of ACL tear.
MOI: ACL traction by severe twisting or varus/valgus force.
CF: swollen tender knee with doughy feel.
X-ray: the # may be missed; the spine(intercondylar eminence)
may be: І-undisplaced; П-hinged; Ш-completely displaced.
Treatment: UGA the joint is aspirated→ 6weeks plaster cylinder in full
extension. If there is block to full extension or the fragment is significantly
displaced→ ORIF.
Dislocation of the knee:
MOI: severe injury may tear cruciate &collateral lig.→ knee ≠.
CF: severe knee swelling, bruising &deformity. The popliteal artery
may be torn or obstructed. Peroneal &/or tibial nerve may be injured.
X-ray: the ≠ can be in any direction; tibial spine may be avulsed.
Treatment: Urgent CR UGA→ back-splint in 15°flexion-check
circulation in the1
st
week- when swelling subsided→ 12weeks cast.
If 1-CR fails, 2-vascular injury or 3-open ≠→ open reduction with
ligament repair. Complication: 1-knee instability & 2-knee stiffness.
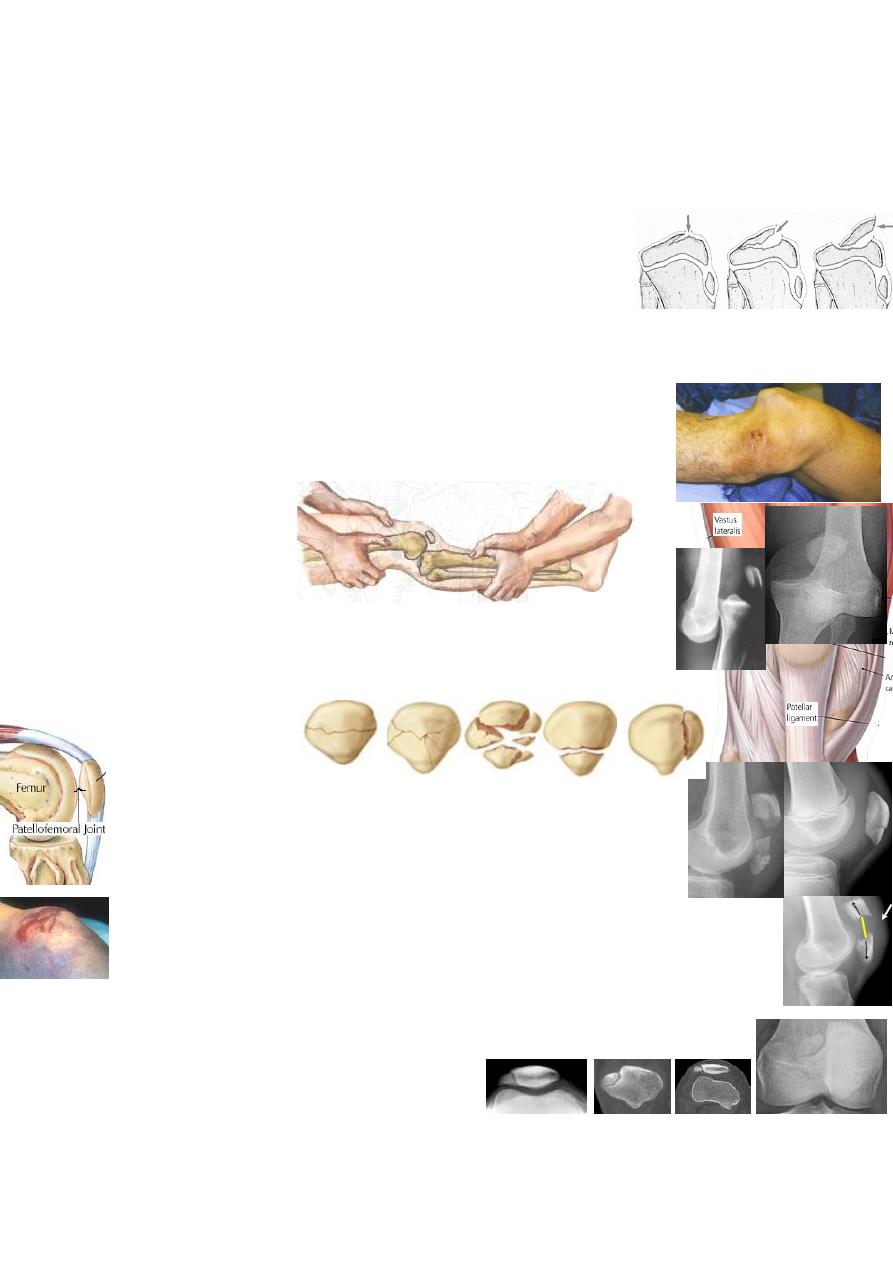
Fractured patella:
Anatomy: the patella is a sesamoid bone in the quadriceps tendon;
the vastus medialis &lateralis also inserted into medial &lateral sides
of the patella; the medial &lateral extensor retinacula are expansion
of quadriceps by passing the patella & inserting to the upper tibia.
MOI: either
Direct injury like dashboard blow or fall onto the knee→ either undisplaced
crack or comminuted(stellate) # with no tear of the extensor expansion.
Indirect injury by resisted quadriceps contraction→ transverse # with
gap due to tear of extensor expansion.
CF: swollen bruised knee; with direct injury the patient can lift his leg &no gap
can be felt in contrast to indirect injury. Aspiration→ blood with fat droplets.
X-ray: bi-, tri- or multi-partite patella(with smooth oblique line at supero-
lateral angle) should not be mistaken for #.
Treatment:
Undisplaced #→ aspirate hemarthrosis→ 3-6weeks cast with quadriceps exercise.
3
Comminuted #: if undisplaced → the same Ŗ.
If displaced→ immediate or late patellectomy(to avoid patellofemoral OA).
Transverse # with gap→ ORIF(2K-wires with tension band wiring) + repair of torn
extensor expansion.
Complication: patellofemoral OA.
Dislocation of the patella:
Is almost always a lateral ≠ with tear of medial retinaculum.
MOI: direct force is rare; often the ≠ is due to indirect(sport) injury:
quadriceps contraction while the knee in valgus &external rotation.
Risk factors: genu valgum, tibial torsion, patella alta, shallow
intercondylar groove, ligament laxity &muscle weakness.
CF: the patient fall to the ground; the patella can be felt on lateral side
of the knee; knee movement is impossible; bruises on medial side.
X-ray: the patella is displaced laterally &there may be osteochondral #.
Treatment: push the patella back into it's place→ 3weeks cast→ 3months
quadriceps exercise. Some prefer operative repair of medial ligaments to
prevent recurrent ≠ especially in severe injury. Complication: recurrent ≠(20%).
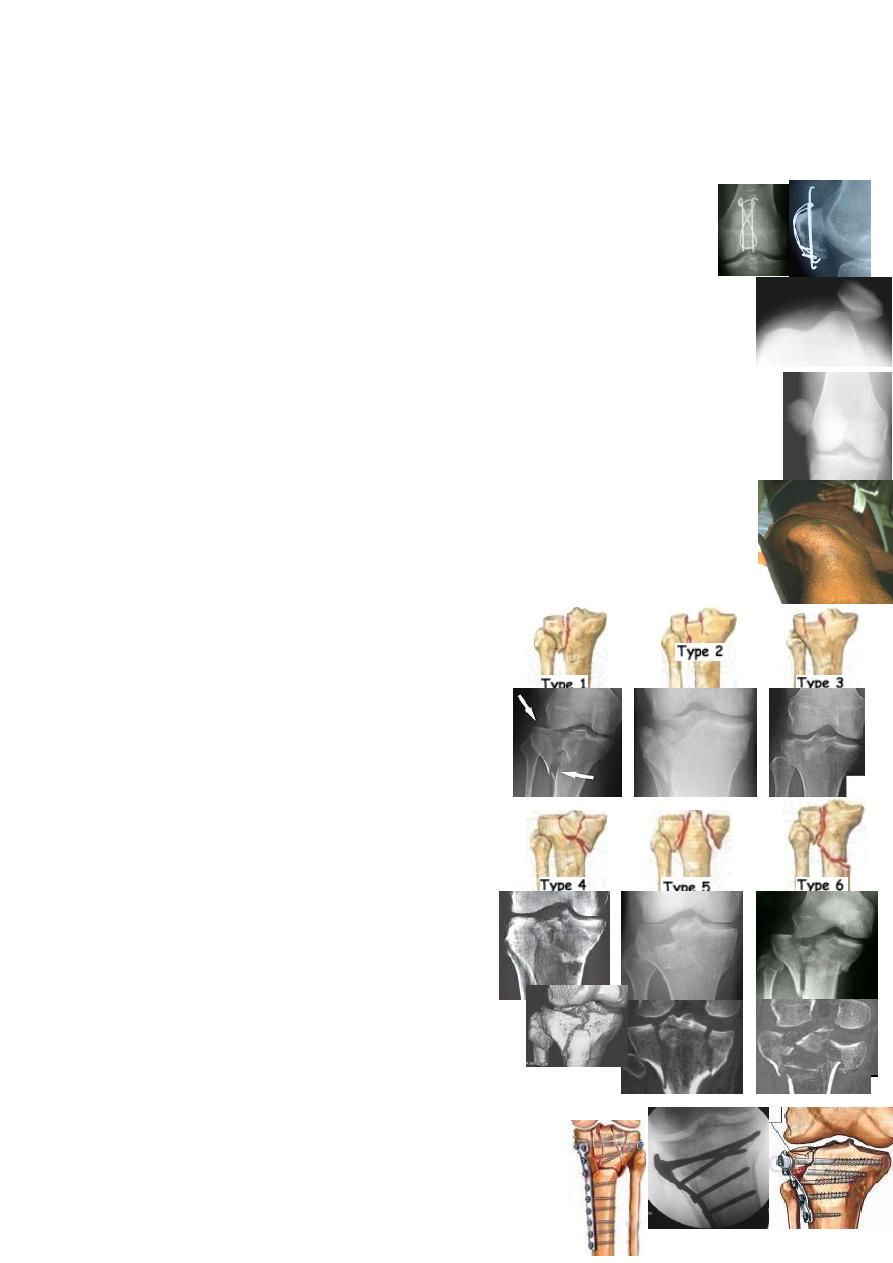
Tibial plateau fractures:
adults(50-60).
MOI: varus or vagus force + axial loading like
car striking a pedestrian(bumper #) or FFH.
Schatzker's classification:
Type 1 - lateral split #.
Type 2 - lateral # that is split and depressed.
Type 3 - lateral depressed fracture
Type 4 - medial #(split or depressed), LCL?
Type 5 - bicondylar
Type 6
– condyle +subcondylar fracture.
CF:
swollen, deformed &bruised knee
with doughy feel;
examine for ligament
tear &neurovascular
injury.
X-ray: AP, lateral &oblique views; CT &3D CT.
Treatment:
Conservative: aspirate the haemarthrosis & apply crepe
bandage→ 10days continuous passive motion(CPM) machine
3weeks hinged cast-brace→ 4weeks PWB→ FWB.
4
Operative: ORIF using lag screws or buttress plate +
elevation of any depression &support with bone graft.
Type І&ІV: if undisplaced → conservative
If displaced→ ORIF.
Type П&Ш: If depression >5mm &young→ ORIF.
if <5mm or elderly→ conservative.
Type V &VІ: if severe, there is a risk of compartment syndrome.
If undisplaced or slightly displaced in elderly→ conservative.
If displaced→ ORIF or circular-frame external fixation or
6weeks skeletal traction→ 6weeks PWB.
Complications:
Early: compartment syndrome: in closed type 5&6 due to excessive bleeding.
Late: joint stiffness, varus or valgus deformity &OA(after 5-10yrs).
Fractures of proximal end of fibula:
MOI: either direct or indirect twisting injury.
The isolated # is rare &needs no Ŗ but look for associated injuries:
1-ankle # or ligament tear(Maisonneuve #); always x-ray the ankle.
2-knee collateral ligament injury.
3-peroneal nerve injury.
late complication: peroneal nerve entrapment.
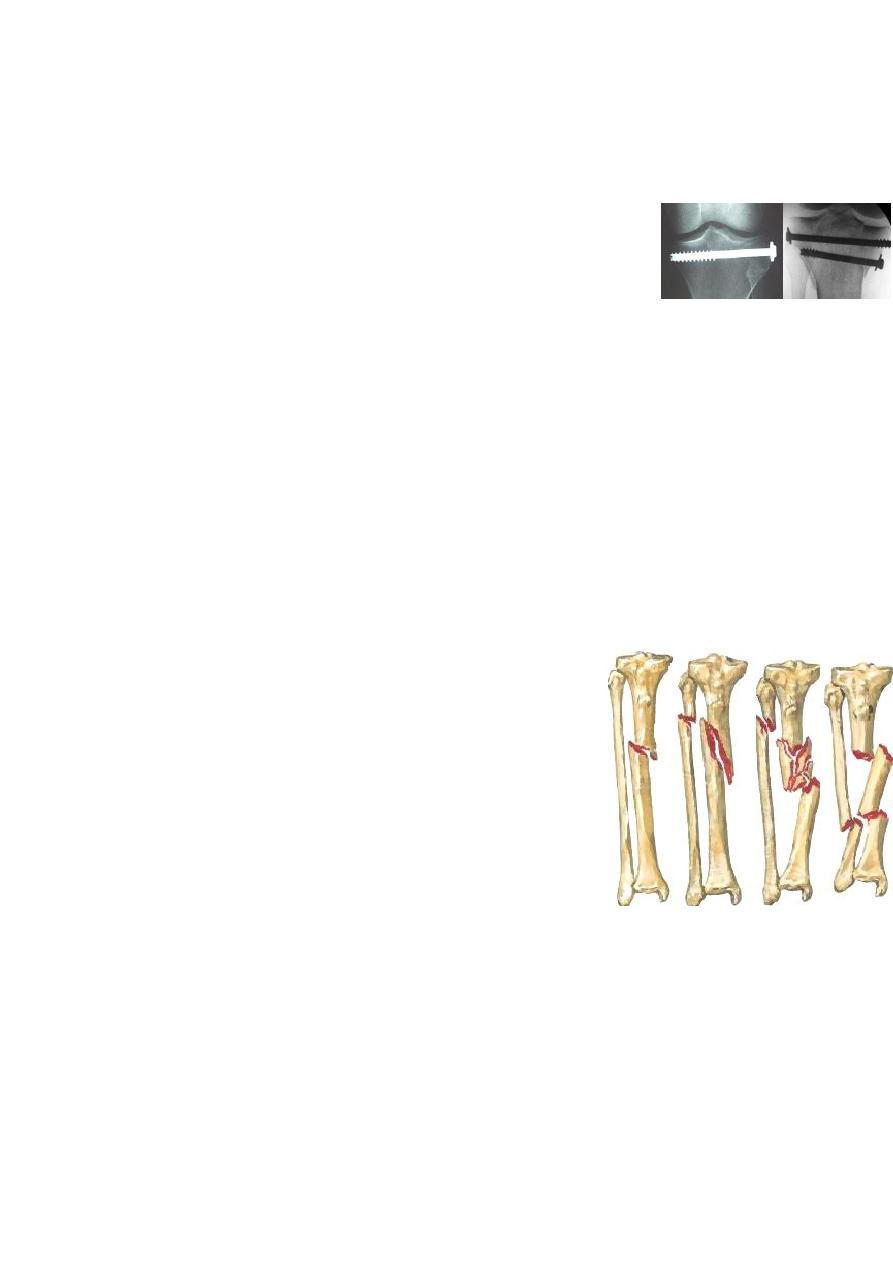
Fractures of the tibia &fibula:
is a common injury &
many times it is open because of it's subcutaneous position.
MOI: twisting force→ spiral # at different levels.
Angulation force→ transverse or oblique # at the same level.
Direct injury may crush or split the overlying skin.
Pathological anatomy: # healing depends on:
1-the severity of soft tissue injury: Tscherne's classification of skin damage in
closed # →
1-
no skin injury;
2-
contusion;
3-
localized degloving;
4-
extensive
degloving;
5-
necrosis from degloving. For open # → Gustilo's classification.
2-the severity of the #: high energy injury(direct force)→ comminuted &open(G
ШB or ШC). Low energy injury(indirect force)→ spiral &closed or open(GІ or П).
3-the stability of the #: transverse, spiral, butterfly or comminuted.
CF: swollen deformed leg &externally rotated foot.
Look for: open wound; skin bruising, crushing & tenting; circulatory changes,
nerve injury & compartment syndrome.
X-ray: the entire leg with knee &ankle should be seen.
5
Low energy #→ uncomminuted spiral #.
High energy #→ displaced transverse, short oblique or comminuted #.
Management:
Aim of treatment: 1-limit soft tissue damage &preserve the skin;
2-prevent compartment syndrome;
3-reduce &hold the #;
4-start early weight bearing;
5-early joint movement.
Conservative: full length cast(from upper thigh to metatarsal necks) &elevation
for 2weeks→ checking x-ray &change the cast as swelling↓→ 8-12weeks PWB. If
skin viability is doubtful→ 2weeks skeletal traction then casting.
Indications: 1-undisplaced &slightly displaced #; & 2-displaced # that can be
reduced(&remain stable) by manipulation.
Operative: indications: 1-failure of closed reduction; & 2-displaced high energy #
that are comminuted &unstable. Types of fixations: closed intramedullary
nailing with locking screws(for closed diaphyseal #, plate fixation(for
metaphyseal #) &external fixation(for open#-&closed comminuted #).
Complications:
Early: 1-vascular injury: proximal 1/3 # may injure the popliteal artery→ repair.
2-compartment syndrome(proximal #)→ fasciotomy→ external fixation.
3-infection: the incidence is 1% for G І &30% for G ШC.
Late: 1-malunion: 1.5cm shortening &7˚angulation are acceptable, if more or mal-
rotation→ tibial osteotomy.
2-delayed union &nonunion: especially in high energy #, infection or bone loss→
stable fixation &bone graft.
3-joint stiffness: of ankle may lasts 12months.
Fracture of the fibula alone:
MOI: 1-indirect→ spiral # as a part of ankle injury .
2-direct blow→ transverse #; CF: local tenderness,ankle &knee movements are
free; Ŗ: analgesia,elastic bandage or below-knee walking cast.
Fracture of the tibia alone:
MOI: direct blow→ transverse #(adults;)Indirect twisting injury→ spiral
#(children-toddle.
Treatment: CR +above-knee cast(12wk in adult &6wk in children.
Complication: nonunion(lower 1/3 #), Ŗ→ ORIF+2.5cm excision of fibula .

6
