Orthopaedics
د.عادل الهنداوي
The Hip
Clinical assessment:
Symptoms: Pain→ hip pain is felt in the groin, front of the thigh
&even the knee, while pain at back of hip is from lumbar spine.
Stiffness, Deformity & Snapping.
Signs:
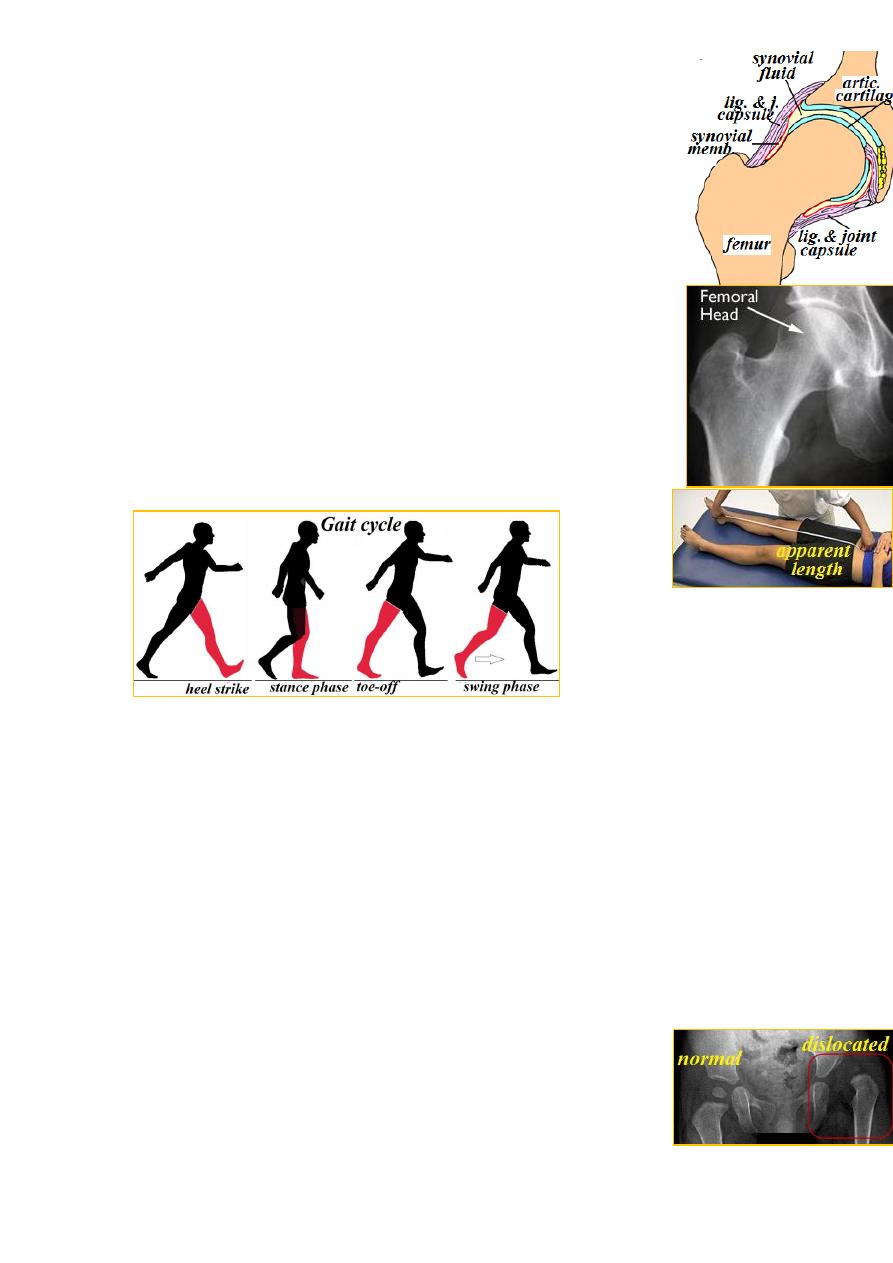
Gait→ normal gait has 4 phases: heel strike, stance phase,
toe-off & swing phase. Any abnormality in gait is called limp.
Causes of limping are: 1- pain anywhere( antalgic gait),
2- short leg.
3- hip problems→ abductor weakness, dislocation, sub-
luxation, pain, short neck. These cause Trendelenburg's gait.
.
Look: skin→ scar, sinus, crease.
Shape: wasting, swelling, position of the limb &limb length: in supine
position with both ASIS at the same level, measure the distance between
medial malleolus & ASIS.
Feel: skin temperature, tenderness, soft tissue &bony points.
Move: flexion, extension, abduction, adduction &rotation(in
flexion &in extension).
Investigations: x-ray, U/S, CT, MRI, arthrogram, arthroscopy, biopsy.
Developmental dysplasia of the hip(DDH)
Is a state of hip instability in the newborn. Normally, the hips are stable at
birth, but if dislocated, subluxated or dislocatable with or without
acetabular dysplasia, this means hip instability.
Incidence:
At birth →10/1000; after 3 wks( hip become ˃ stable): 1/1000.
It is ˃ common in female with a ratio of ♀7:1♂; more on left
side with ratio of Lt. 3:1 Rt.& bilateral 1 in every 5 cases.
families
: DDH tends to run in
factors
Genetic
-
1
:
Etiology
&populations (northern Italians).
in the level of estrogen,
↑
: before birth, there is
factors
Hormonal
-
2
progesterone &relaxin hormones in maternal blood→↑ ligament laxity in
infant. So DDH is rare in premature baby.
incidence in breech position.
↑
:
Intrauterine malposition
-
3
e.g.
: may play role in the persistence of instability
factors
Postnatal
-
4
societies that swaddle their babies → ↑ incidence while in those who
carry them astride the back with legs abducted will have ↓ incidence.
Pathology
: according to the age
At birth→ the hip is normal but the capsule is stretched.
During infancy: many changes will occur secondary to abnormal
position: the femoral head dislocate posteriorly &with hip extension it
becomes superolateral to acetabulum. The femoral neck become more
anteverted. The acetabulum become shallow &anteverted. The
capsule become more stretched. The lig. teres become elongated
&hypertrophied. The labrum is pushed into acet. by the FH(limbus).
After weight bearing: all these changes will ↑. The FH will form
a false socket above the true acet.; the capsule will be squeezed
between psoas muscle &the acet. taking the shape of hour glass.
The surrounding muscles with time will become shorter.
CF: every newborn should be examined for hip instability
especially if there is family history or breech position.
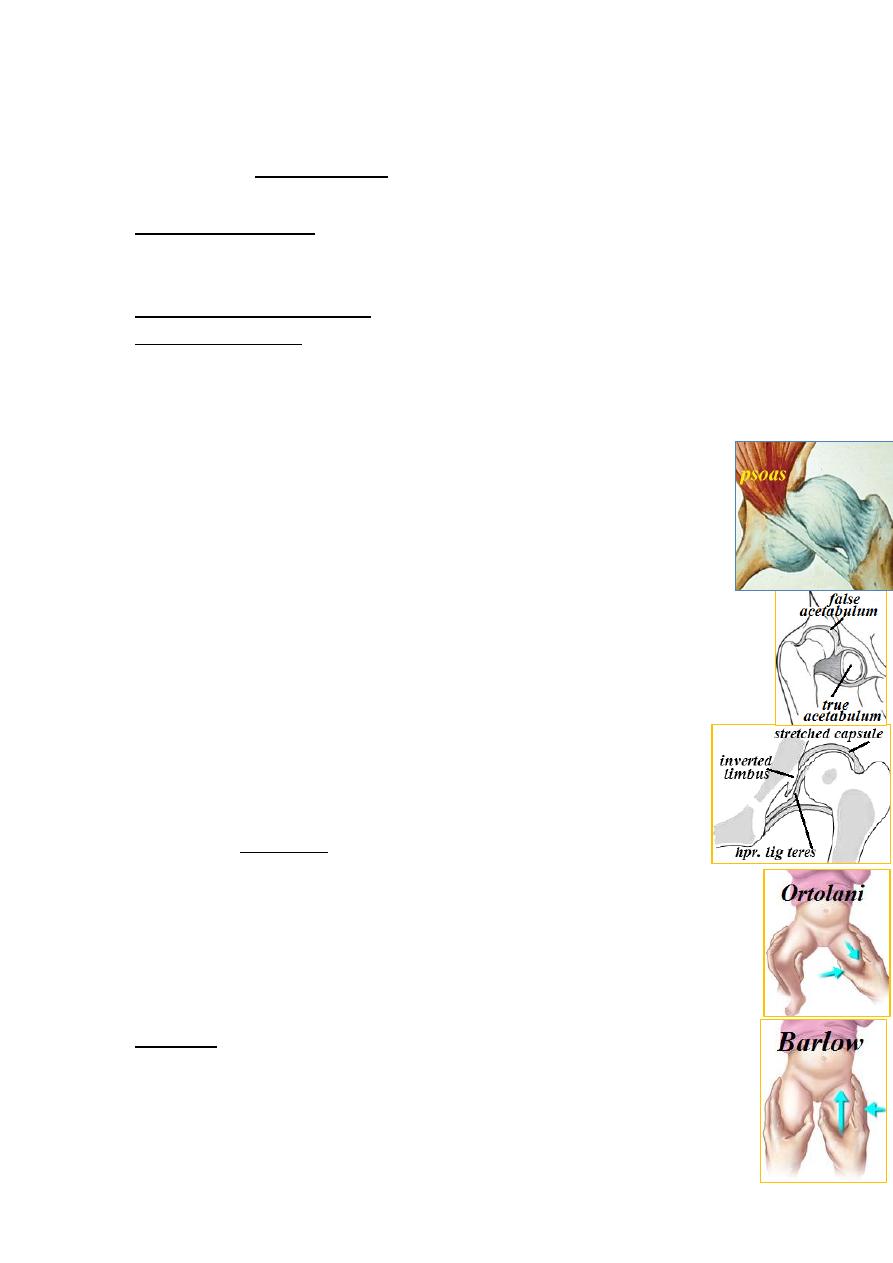
→ hold the thigh with
(for dislocated hip)
test
Ortolani's
:
In neonate
your thumb medially &other fingers on greater trochanter→ flex the hip
90ᵒ→ abduct the hip, normally abduction will reach 90 ᵒ. If stop
anywhere this means dislocation. Press on by your fingers on
grater trochanter to reduce the hip to complete the abduction
( reducible dislocation) otherwise it is irreducible dislocation.
ut push by
the same b
:(for dislocatable hip)
test
Barlow's
your thumb the FH out of the socket during adduction & return back
during abduction( dislocatable hip).
Late features: limited hip abduction, asymmetrical skin
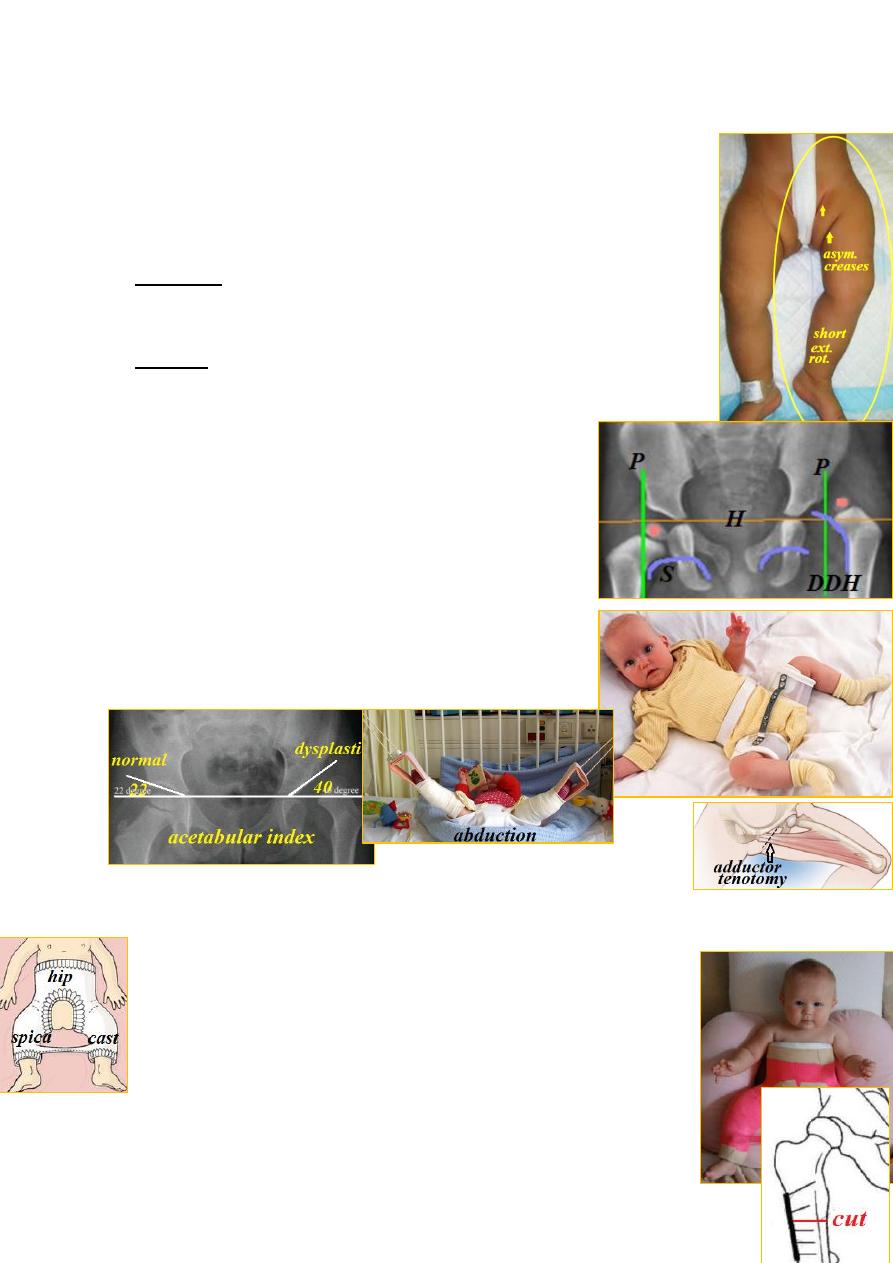
crease, short &externally rotated leg &limping. In
bilateral dislocation: wide perineal gap &waddling gait.
Imaging: during first 6 mths, x-ray is not useful because
both FH &acet. are cartilaginous, so U/S is the best.
After 6mths, X-ray become more useful:
normally, a line with inferior border of
:
line
Shenton's
femoral neck is continuous with inferior border of upper
pubic ramus, if broken→ dislocation or subluxation.
with
vertical
cartilage &
triradiate
with
: horizontal
line
Perkin's
acetabular edge. Normal position of FH is medial to vertical & below
horizontal; if not → dislocation or subluxation.
Management
: according to the age
0-6 months → 90% of unstable hips will be stabilized
spontaneously at 3 wks; So at 3 wks, if reduced &
stable→ observe till 6 mths.
If reduced &unstable(dislocatable)→ abduction splint.
If dislocated→ reduce & put in abduction splint.
Splint: either Pavlik harness, Von Rosen splint or
other hip abduction splint. The splint should be used
until x-ray shows good acetabular roof.
6-18 months→ hip dislocation must be reduced either by
closed or open method:
Closed reduction: this should be gradual. Apply traction
to both legs using vertical frame (Gallows traction) with
↑ abduction gradually for 3 weeks (adductor tenotomy may be
done if abduction is limited). Reduction is performed UGA &spica
cast is applied for 2-3 months → abduction splint for 3-6 months.
Open reduction: if closed reduction failed, do open reduction→
hip spica→ splint. Sometimes, for reduction to be stable, the leg
should be internally rotated, if so, femoral derotation osteotomy

in subtrochanteric region is done at the same time or later.
18mth- age limit→ is surgical by:
open reduction± femoral derotation(± varus) osteotomy±pelvic
osteotomy. Then hip spica for 3 mths → abduction splint for 3 mths.
Above age limit→ for unilateral dislocation, the age limit is 10 yrs. while
for bilateral dislocation is 6 yrs. because with bilateral, the deformity is
symmetrical &failure on one side will make it asymmetrical ¬iceable.
Persistent dislocation in adult→ THR.
Acetabular dysplasia &hip subluxation
:
the acet. is shallow & the femoral head is only partly covered.
Causes: 1- genetic factors; 2- incomplete reduction of DDH;
3-damage to the lateral acetabular epiphysis.
CF: infant→ limited abduction; child→ symptomless but painful hip
&limp following exercise. adult→ OA of the hip.
X-ray→ the roof of acet. is sloping &the head is uncovered.
If there is subluxation, the Shenton's line is broken.
Ŗ: Infant→ similar to DDH.
Children→ similar to DDH &may require acetabuloplasty ± varus
femoral osteotomy.
Adolescent & young adult→ acetabuloplasty, Chiarior shelf operation ±
varus femoral osteotomy.
Old adult→ THR for OA of the hip.
Acquired hip dislocation
: occurring after first year of life
is usually due to: 1- trauma; 2- muscle imbalance;
3- pyogenic arthritis.
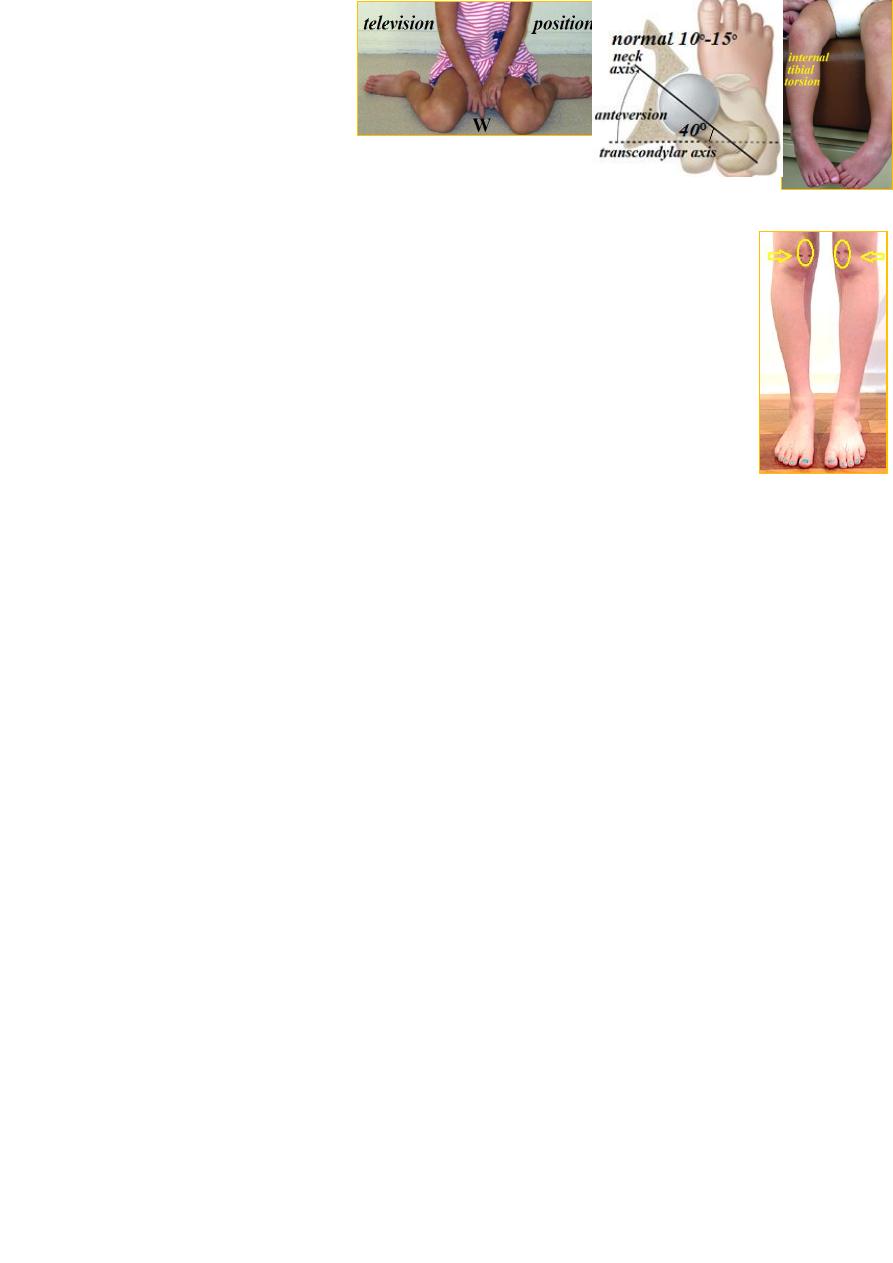
Femoral anteversion(in-toe gait)
The toes are directed inward during walking making the child
trips over
his feet during running.
Causes: below 3 yrs.→ forefoot adduction or tibial torsion.
Above 3 yrs.: excessive femoral neck anteversion (hip internal rotation).
CF: clumsy gait. The child sits in(Wposition) television position &when
standing both patellae directed inward (squinting patellae).
Diagnosis is clinical; to assess the degree of anteversion→CT to measure
the angle between the femoral neck & the transverse axis of femoral
condyles.
Ŗ→ it usually will correct Spontaneously with time.
If it persists above the age of 8 yrs: femoral corrective osteotomy may
needed.
(transient synovitis) :
Irritable hip syndrome
transient synovitis characterized by transient hip pain &limping in an
otherwise healthy child. It is the commonest cause of hip pain in children.
CF: usual age 6-12 yrs. Boys affected 3x than girls. The child presents
with groin, thigh or even knee pain with limping.
O/E: only the extreme of hip movements are painful.
The symptoms last 1-2 weeks, then subsides spontaneously
investigations are normal except U/S showing small joint effusion.
ÐḐ:1-Pyogenic arthritis: ill, toxic child with high fever &all hip ROM
are more severely restricted & painful, ESR ↑, WBC ↑, blood culture
50% +ve, ASO titer ↑.
2-Tuberculous arthritis: can be similar to transient synovitis because the
C.F. are subacute. ESR ↑. X-ray→ osteoporosis, lytic lesion &later joint
destruction. In difficult cases, bone &synovial biopsy are needed.
3-Perthes' disease: last ˃2 wks &x-ray: ↑ joint space.
4- Juvenile chronic arthritis: ESR ↑ with systemic features.
5- Slipped epiphysis: may presents as irritable hip, later x-ray is
characteristic.
Ŗ→ bed rest at home; in severe cases, admission for continuous traction.
Weight bearing is allowed only when symptoms &joint effusion resolve.
