
The Shoulder
Dr.Mushtaq Talib Hussein
M.B.Ch.B ,F.I.B.M.S(ortho.),C.A.B.O (ortho.)
ADHESIVE CAPSULITIS (FROZEN SHOULDER)
The
term ‘frozen shoulder’ should be reserved for a well-defined disorder
characterized by progressive pain and stiffness of the shoulder which usually resolves
spontaneously after about 18 months.
The condition is particularly associated with diabetes, Dupuytren’s disease,
hyperlipidaemia, hyperthyroidism, cardiac disease and hemiplegia.
Clinical features
The patient, aged 40–60, may give a history of trauma, often trivial, followed by
aching in the arm and shoulder. Pain gradually increases in severity and often
prevents sleeping on the affected side. After several months it begins to subside, but
as it does so stiffness becomes an increasing problem, continuing for another 6–12
months after pain has disappeared.
The cardinal feature is a stubborn lack of active and passive movement in all
directions.
X-rays are normal unless they show reduced bone density from disuse. Their main
value is to exclude other causes of a painful, stiff shoulder.
Differential Diagnosis
Infection In patients with diabetes, it is particularly important to exclude infection.
Post-traumatic stiffness After any severe shoulder injury, stiffness may persist for
some months.
Diffuse stiffness If the arm is nursed over-cautiously(e.g. following a forearm
fracture) the shoulder may stiffen.
Reflex sympathetic dystrophy Shoulder pain and stiffness may follow myocardial
infarction or a stroke. The features are similar to those of a frozen shoulder and it has
been suggested that the latter is a form of reflex sympathetic dystrophy.
Treatment
CONSERVATIVE TREATMENT
Conservative treatment aims to relieve pain and prevent further stiffening while
recovery is awaited. It is important not only to administer analgesics and
antiinflammatory drugs but also to reassure the patient that recovery is certain.
Exercises are encouraged, the most valuable being‘pendulum’ exercises in which the
patient leans forward at the hips and moves his arm as if stirring a giant pudding (this
is really a form of assisted active movement, the assistance being supplied by
gravity).

The role of physiotherapy is unproven and the benefits of steroid injection are
debatable.
Manipulation under general anaesthesia may improve the range of movement.
An alternative method of treatment is to distend the joint by injecting a large
volume
(50–200 mL) of sterile saline under pressure.
Arthroscopy has shown that both manipulation and distension achieve their effect by
rupturing the capsule.
SURGICAL TREATMENT
Surgery does not have a well-defined role. The main indication is prolonged and
disabling restriction of movement which fails to respond to conservative treatment.
Arthroscopic capsular release is increasingly employed.
Instability of the shoulder
The shoulder achieves its uniquely wide range of movement at the cost of stability.
The humeral head is held in the shallow glenoid socket by the glenoid labrum, the
gleno-humeral ligaments, the coracohumeral ligament, the overhanging canopy of the
coracoacromial arch and the surrounding muscles.
Failure of any of these mechanisms may result in instability of the joint.
It recognizes that there are two broad reasons why shoulders become unstable: (1)
structural changes due to major trauma such as acute dislocation or recurrent micro-
trauma; and (2) unbalanced muscle recruitment (as opposed to muscle weakness)
resulting in the humeral head being displaced upon the glenoid.
TRAUMATIC ANTERIOR INSTABILITY
This is far and away the commonest type of instability, accounting for over 95 per
cent of cases. Traumatic anterior instability usually follows an acute injury in which
the arm is forced into abduction, external rotation and extension.
In recurrent dislocation the labrum and capsule are often detached from the anterior
rim of the glenoid (the classic Bankart lesion). In addition there may be an
indentation on the posterolateral aspect of the humeral head (the Hill–Sachs lesion), a
compression fracture due to the humeral head being forced against the anterior
glenoid rim each time it dislocates.
Clinical features
The patient is usually a young man or woman who gives a history of the shoulder
‘coming out’, perhaps during a sporting event.
On examination, between episodes of dislocation, the shoulder looks normal and
movements are full.
Clinical diagnosis rests on provoking subluxation. In the apprehension test, with the
patient seated or lying, the examiner cautiously lifts the arm into abduction, external
rotation and then extension; at the crucial moment the patient senses that the humeral
head isabout to slip out anteriorly and his or her body tautens in apprehension.
The test should be repeated with the examiner applying pressure to the front of the
shoulder; with this manoeuvre, the patient feels more secure and the apprehension
sign is negative.
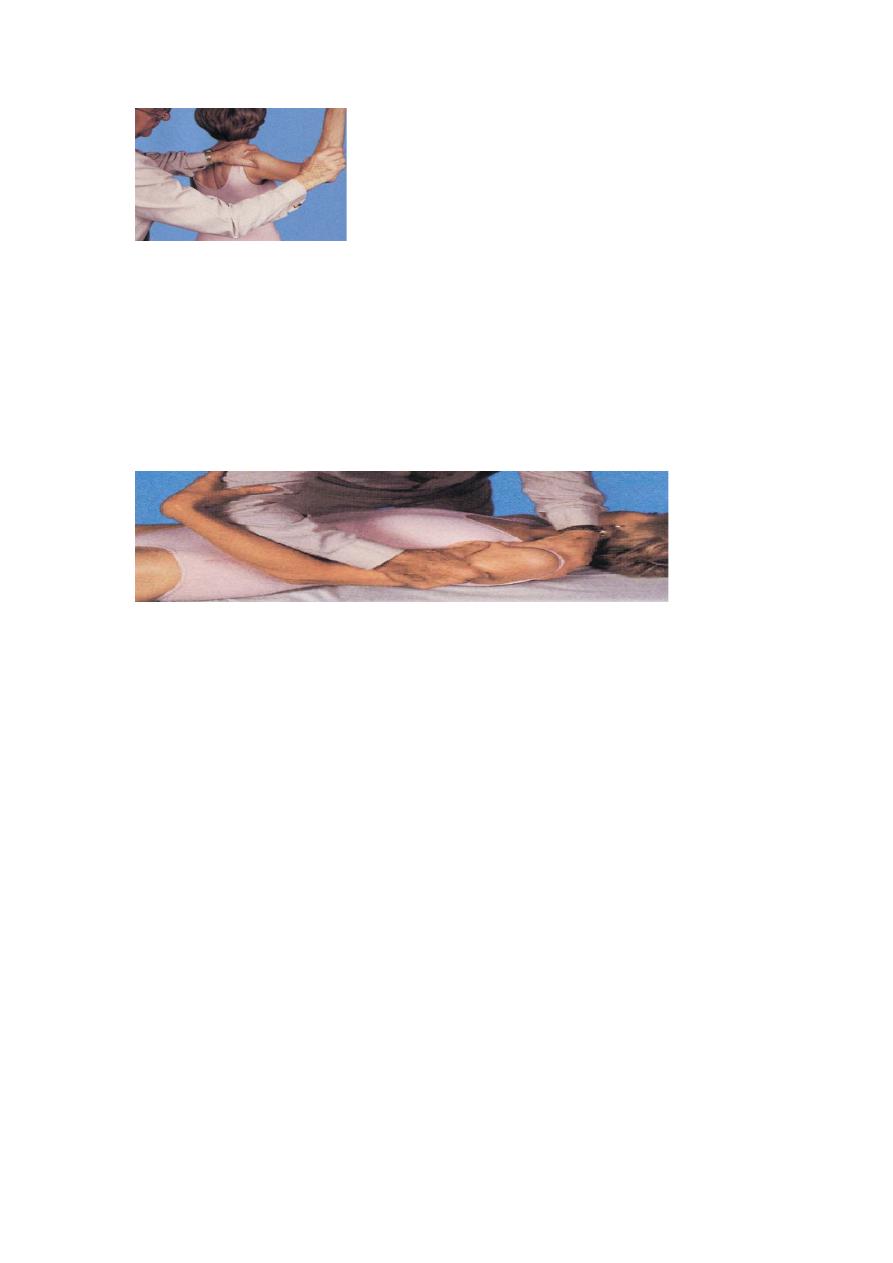
The same effect can be demonstrated by the fulcrum test. With the patient lying
supine, arm abducted to 90 degrees, the examiner places one hand behind the
patient’s shoulder to act as a fulcrum over which the humeral head is levered
forward by extending and laterally rotating the arm; the patient immediately becomes
apprehensive.
If instability is marked the drawer test may be positive ,With the patient supine, the
scapula is stabilized with one hand while the upper arm is grasped firmly with the
other so as to manipulate the head of the humerus forwards and backwards (like a
drawer).
Investigations
Most cases can be diagnosed from the history and examination alone. The Hill–Sachs
lesion (when it is present) is best shown by an anteroposterior x-ray with the shoulder
internally rotated, or in the axillary view.
Subluxation is seen in the axillary view.
MRI or MR arthrography is useful for demonstrating bone lesions and labral tears.
Arthroscopy is sometimes needed to define the labral tear.
Examination under anaesthesia can help to determine the direction of instability.
This forms an essential part of assessing instability. Both shoulders need to be
examined. Reports have demonstrated sensitivities and specificities of 100 per cent
and 93 per cent, respectively.
Treatment
If dislocation recurs at long intervals, the patient may choose to put up with the
inconvenience and simply try to avoid vulnerable positions of the shoulder.
OPERATIVE TREATMENT
The indications for operation include frequent dislocation, especially if this is
painful, and recurrent subluxation or a fear of dislocation sufficient to prevent
participation in everyday activities, including sport.
Anatomical repairs These are operations that repair the torn glenoid labrum and
capsule, e.g. the Bankart procedure .

Non-anatomical repairs These procedures are designed to counteract the pathological
tendency to joint displacement:
(a) operations that shorten the anterior capsule and subscapularis by an overlapping
repair (e.g. the Putti–Platt operation);
(b) operations that reinforce the anteroinferior capsule by redirecting other muscles
across the front of the joint (e.g. the Bristow–Laterjet operation); and (c) a bone
operation to correct a reduced retroversion angle of the humeral head by osteotomy
(Kronberg and Brostrum,).
POSTERIOR INSTABILITY
Pathology
This condition is usually due to a violent jerk in an unusual position or following an
epileptic fit or a severe electric shock. Dislocation may be associated with fractures of
the proximal humerus, the posterior capsule is stripped from the bone or stretched,
and there may be an indentation on the anterior aspect of the humeral head. Recurrent
instability is almost always a posterior subluxation with the humeral head riding back
on the posterior lip of the glenoid.
DISORDERS OF THE GLENOHUMERAL JOINT
TUBERCULOSIS
Tuberculosis of the shoulder is uncommon. It usually starts as an osteitis but is rarely
diagnosed until arthritis has supervened. This may proceed to abscess and sinus
formation, but in some cases the tendency is to fibrosis and ankylosis.
RHEUMATOID ARTHRITIS
This is the most common arthropathy to affect the shoulder complex; 90 per cent of
patients with rheumatoid arthritis have involvement of the acromioclavicular joint, the
shoulder joint and the various synovial pouches around the shoulder.
OSTEOARTHRITIS
Osteoarthritis of the gleno-humeral joint is more common than is generally
recognized. It is usually secondary to local trauma, recurrent subluxation or
longstanding rotator cuff lesions. Often chondrocalcinosis is present as well but it is
not known whether this predisposes to osteoarthritis or appears as a sequel to joint
degradation.
RAPIDLY DESTRUCTIVE ARTHROPATHY (MILWAUKEE SHOULDER)
Occasionally, in the presence of longstanding or massive cuff tears, patients develop a
rapidly progressive and destructive form of osteoarthritis in which there is severe
erosion of the gleno-humeral joint, the acromion process and the acromioclavicular
joint –what Neer and his colleagues (1983) called a cuff tear arthropathy.
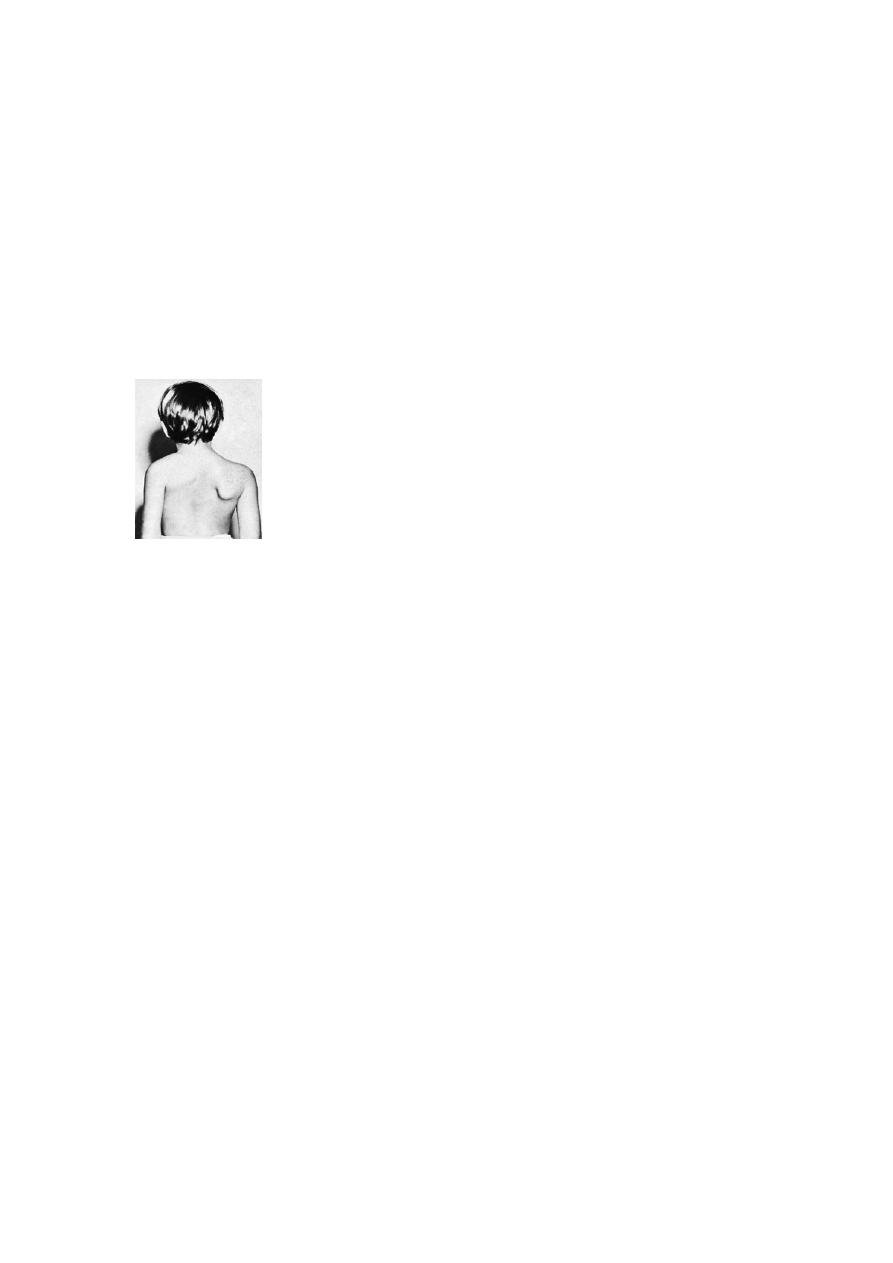
CONGENITAL ELEVATION OF THE
SCAPULA
The scapulae normally complete their descent from the neck by the third month of
fetal life; occasionally one or both scapulae remain incompletely descended.
Associated abnormalities of the cervical spine are common and sometimes there is a
family history of scapular deformity.
