
﷽
The hand
Dr.Mushtaq Talib Hussien
F.I.B.M.S (ortho.)
C.A.B.O (ortho.)

The hand is (in more senses than one) the medium of introduction to the outside
world. Its unique repertoire of prehensile movements, grasp, pinch, hook-action and
tactile acuity sets us apart from all other species.
CLINICAL ASSESSMENT
SYMPTOMS
Pain may be felt in the palm, the thumb or the finger joints.,or radiated pain.
Deformity may appear suddenly (e.g. due to tendon rupture) or slowly (suggesting bone or
joint pathology,
Swelling may be localized
constant or intermittent
Sensory symptoms and motor weakness provide welldefined clues to neurological disorders.
Loss of function takes various forms.
SIGNS
Both upper limbs should be bared for comparison. Before focussing on the hands take a quick
look at the shoulders and elbows and their range of movement. Also ask which is the
dominant hand
Look
Note how the patient holds the hand and uses it during the interview; the resting
posture may be suggestive of nerve or tendon damage. Ask the patient to place both
hands on the table in front of you, with the palms first upwards and then downwards.
Passive tenodesis
Note the resting position of the
fingers with the wrist
(a)
flexed,
(b)
extended.
Feel
The temperature and texture of the skin are noted and the pulse is felt. Swelling or
thickening may be in the subcutaneous tissue, a tendon sheath, a joint or one of the
bones.
Move
Passive movements The thumb and each finger are examined in turn and
the range of movement recorded. Note whether the movement causes pain.
Active movements Ask the patient to place both hands with the palms facing upwards,
Gross active movement (a)
Full extension.
(b)
Full flexion.
(c)
A good test for
abductor power is to have the patient spread his or her fingers as strongly as possible;
slowly push the hands together until the tips of the little fingers are forcefully
opposing one another; the weaker one will collapse
.
Grip strength
Grip strength is an important indicator of hand and wrist function.
Grip strength should be measured with a mechanical dynamometer; if this is not
available, an indication can be derived from having the patient squeeze .
Neurological assessment
If symptoms such as numbness, tingling or weakness exist – and in all cases of trauma
– a full neurological examination of the upper limbs should be carried out, testing
power, reflexes and sensation.
CONGENITAL HAND ANOMALIES
The incidence of congenital upper limb abnormalities is estimated to be about 1 in
600 live births. Some are confined to the hand but in most cases the wrist and forearm
are involved as well.
Congenital variations
Transverse failure
)
radial club hand and absent thumb,
constriction rings,
camptodactyly,
clinodactyly
ACQUIRED DEFORMITIES
Deformity of the hand may result from acquired disorders of the skin, subcutaneous
tissues, muscles, tendons, joints, bones or neuromuscular function.
SKIN CONTRACTURE
Cuts and burns of the palmar skin are liable to heal with contracture. Surgical
incisions should never cross skin creases perpendicularly; they should lie more or
less parallel or oblique to them, or in the mid-axial line of the fingers.
SUPERFICIAL PALMAR FASCIA(DUPUYTREN’S) CONTRACTURE
Hypertrophy and contracture of the palmar fascia may lead to puckering of the palmar
skin and fixed flexion of the fingers.
MUSCLE CONTRACTURE
VOLKMANN’S ISCHAEMIC CONTRACTURE
Contracture of the forearm muscles may follow circulatory insufficiency due to
injuries at or below the elbow. Shortening of the long flexors causes the fingers to be
held in flexion; they can be straightened only when the wrist is flexed so as to relax
the long flexors.
TENDON LESIONS
MALLET FINGER
This results from injury to the extensor tendon of the terminal phalanx. It may be due
to direct trauma, The terminal joint is held flexed and the patient cannot straighten it,
but passive movement is normal.
X-rays are taken to show or exclude a fracture. If there is a fracture but minimal
subluxation of the joint, it is treated by splintage with the DIP joint in extension for 6
weeks. Operative treatment is considered only if there is a large fragment (>50 per
cent) and subluxation of the DIP joint.

BOUTONNIER DEFORMITY
This lesion presents as a flexion deformity of the PIP joint and extension of the DIP
joint. It is due to interruption or stretching of the central slip of the extensor tendon
where it inserts into the base of the middle phalanx.
In the early post-traumatic case, splinting the PIP joint in full extension for 6 weeks
usually leads to healing;
SWAN-NECK DEFORMITY
This is the reverse of the boutonniere deformity; the PIP joint is hyperextended and
the DIP joint flexed. The deformity can be reproduced voluntarily by laxjointed
individuals.
If the deformity corrects passively, then a simple figure-of-eight ring splint to
maintain the PIP joint in a few degrees of flexion may be all that is required,
If the deformity is fixed, then it may respond to gentle manipulation supplemented by
temporary Kwire fixation in a few degrees of flexion;
JOINT DISORDERS
RHEUMATOID ARTHRITIS
Rheumatoid arthritis causes multiple, symmetrical deformities of both hands,
typically ulnar deviation of the MCP joints and boutonniere or swan-neck deformities
of the proximal finger joints
OSTEOARTHRITIS
Osteoarthritis, by contrast, affects mainly the DIP joints. It is common in
postmenopausal women and may cause deformity. The thumb CMC joint is another
common site,
NEUROMUSCULAR DISORDERS
SPASTIC PARESIS
Cerebral palsy, head injury and stroke may result in typical deformities of the hand.
The ‘intrinsic-plus’ posture is easily recognized. Another common disability is
‘thumb-in-palm’; the tendency to adduct and flex the thumb into the palm is increased
by activity, especially finger flexion.
PERIPHERAL NERVE LESIONS
The most common are drop-wrist and drop-fingers(radial nerve palsy), a simian
thumb and pointing index finger (median nerve palsy) and partial claw hand (ulnar
nerve palsy). The distribution of sensory loss helps to establish the site of the lesion.
DUPUYTREN’S CONTRACTURE
This is a nodular hypertrophy and contracture of the superficial palmar fascia (palmar
aponeurosis). The condition is inherited as an autosomal dominant trait and is most

common in people of European (especially Anglo-Saxon) descent. It is more common
in males than females; There is a high incidence in epileptics receiving phenytoin
therapy; associations with diabetes, smoking, alcoholic cirrhosis, AIDS and
pulmonary tuberculosis have also been described.
PATHOLOGY
The essential problem in Dupuytren’s disease is proliferation of myofibroblasts;
Clinical features
The patient – usually a middle-aged man – complains of a nodular thickening in the
palm.
The palm is puckered, nodular and thick. Sometimes the dorsal knuckle pads
are thickened (Garrod’s pads).
Similar nodules may be seen on the soles of the feet (Ledderhose’s disease).
Treatment
Operation is indicated if the deformity is a nuisance or rapidly progressing.
The aim is reasonable, not complete, correction. Surgery does not cure the disease, it
only partially corrects the deformity, and recurrence or extension is common.
TRIGGER FINGER (DIGITAL TENOVAGINOSIS
)
A flexor tendon may become trapped by thickening at the entrance to its sheath; on
forced extension it passes the constriction with a snap (‘triggering’).
More common in patients with diabetes and rheumatoid disease.
Clinical features
Any digit may be affected, but the thumb, ring and middle fingers most commonly;
sometimes several fingers are affected. The patient notices a click as the finger is flexed;
A tender nodule can be felt in front of the MCP.
Treatment In adults, early cases may be cured by an injection of corticosteroid
Refractory cases need operation,
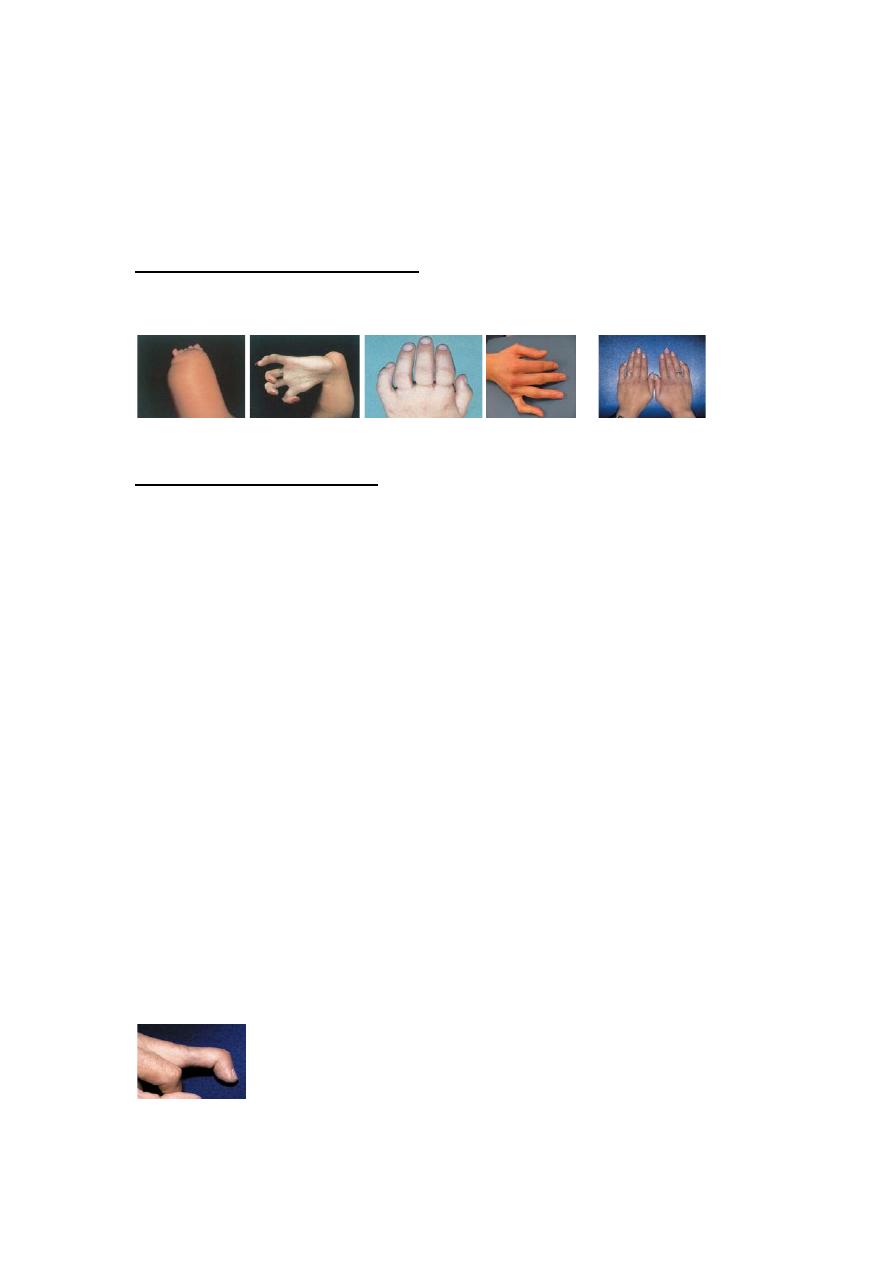
Rheumatoid hand
a
b
c
Rheumatoid arthritis
– clinical features (a)
Early case with typical features: radial deviation of the
wrist; subluxation of the radio-ulnar joint; swollen MCP joints and ulnar deviation of the fingers.
(b)
More
advanced changes, including subluxation of the MCP joints.
(c)
Dropped fingers due to rupture of
extensor tendons at the wrist.
In osteoarthritis
a
b c
Osteoarthritis(a,b)
The common picture is one of
‘knobbly finger-tips’ due to involvement of the DIP
joints (
Heberden
’
s nodes
).
(c)
In some cases the PIP joints are affected as well (
Bouchard
’
s nodes
).
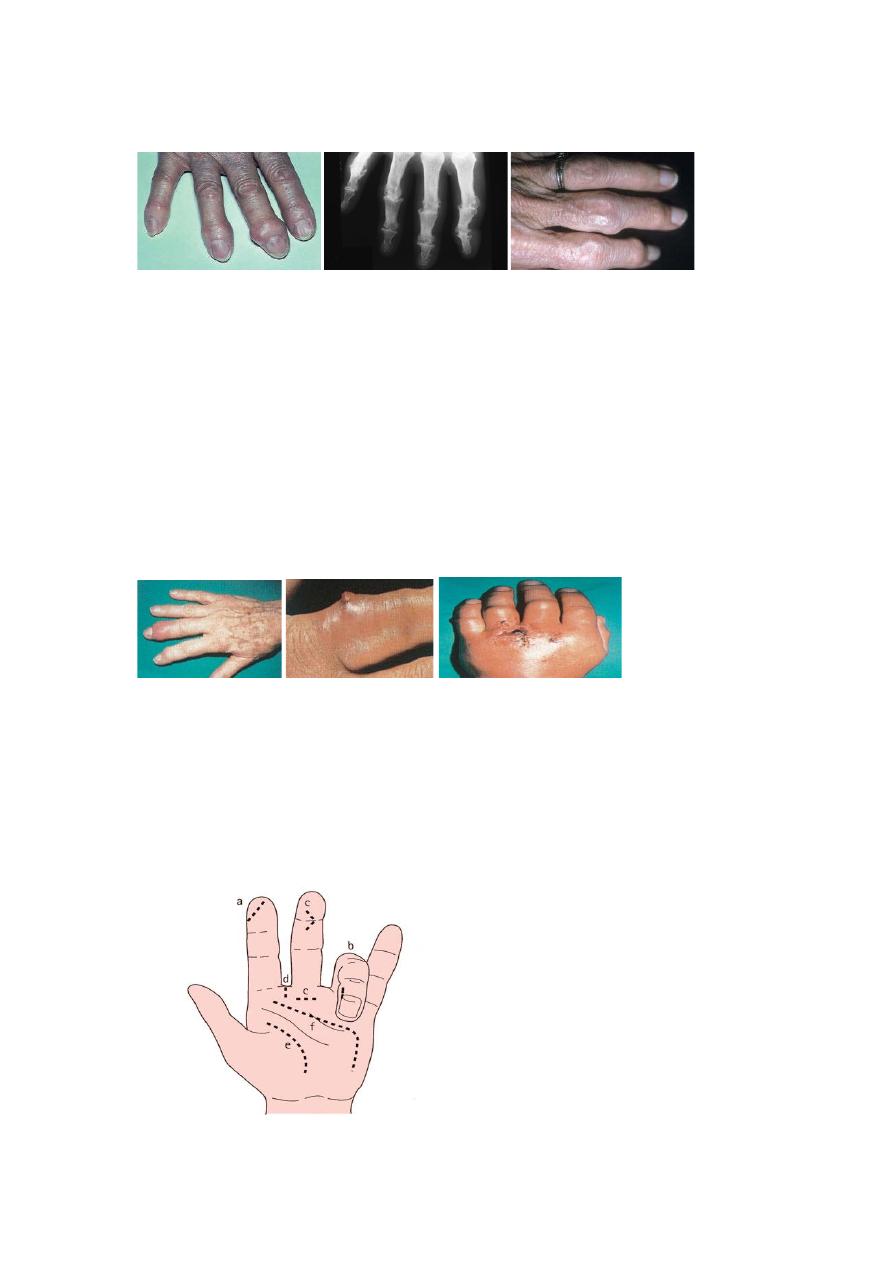
ACUTE INFECTIONS OF THE HAND
Infection of the hand is frequently limited to one of several well-defined
compartments: under the nail-fold (paronychia); the pulp space (felon) and in the
subcutaneous tissues elsewhere; the deep fascial spaces; tendon sheaths; and joints.
Usually the cause is a staphylococcus which has been implanted during fairly trivial
injury. However, cuts contaminated with unusual organisms account for about 10 per
cent of cases.
Clinical features
Usually there is a history of trauma (a superficial abrasion, laceration or penetrating
wound), but this may have been so trivial as to pass unnoticed. A few hours or days
later the finger or hand becomes painful and swollen.
Principles of treatment
Superficial hand infections are common; if their treatment is delayed or inadequate,
infection may rapidly extend, with serious consequences. The essentials of treatment
are:
•
antibiotics
•
rest, splintage and elevation
•
drainage
•
rehabilitation
The incisions for surgical drainage are shown here: a, pulp space (directly over the
abscess); b, nail-fold (it may also be necessary to excise the edge of the nail); c,
tendon sheath; d, web space; e, thenar space; f, mid-palmar space.
