Dr.Mushtaq Talib Hussein
F.I.B.M.S(Ortho.)- C.A.B.O(Ortho.)
THE WRIST
clinical assessment
history
■
Pain may be localized to the radial side (especially in tenovaginitis of the thumb tendons),
to the ulnar side (possibly from the radioulnar joint) or to the dorsum (the usual site in
disorders of the carpus).
■
Stiffness is often not noticed until it is severe
■
Swelling may signify involvement of either the joint or the tendon sheaths.
■
Deformity is a late symptom except after trauma.
■
Loss of function affects both the wrist and the hand. Firm grip is possible only with a
strong, stable, painless wrist that has a reasonable range of movement
.
Examination
Examination of the wrist is not complete without also examining the elbow, forearm and
hand. Both upper limbs should be completely exposed.
Imaging
X-rays are routinely obtained; often both wrists must be examined for comparison.
Magnetic resonance imaging (MRI) is useful for demonstrating soft-tissue lesions
Wrist deformities
Congenital variations
Embryonic abnormalities of the upper limb are likely to affect more than one segment (or
indeed the whole) of the limb; therefore, congenital anomalies often appear together in the
forearm, wrist and hand.
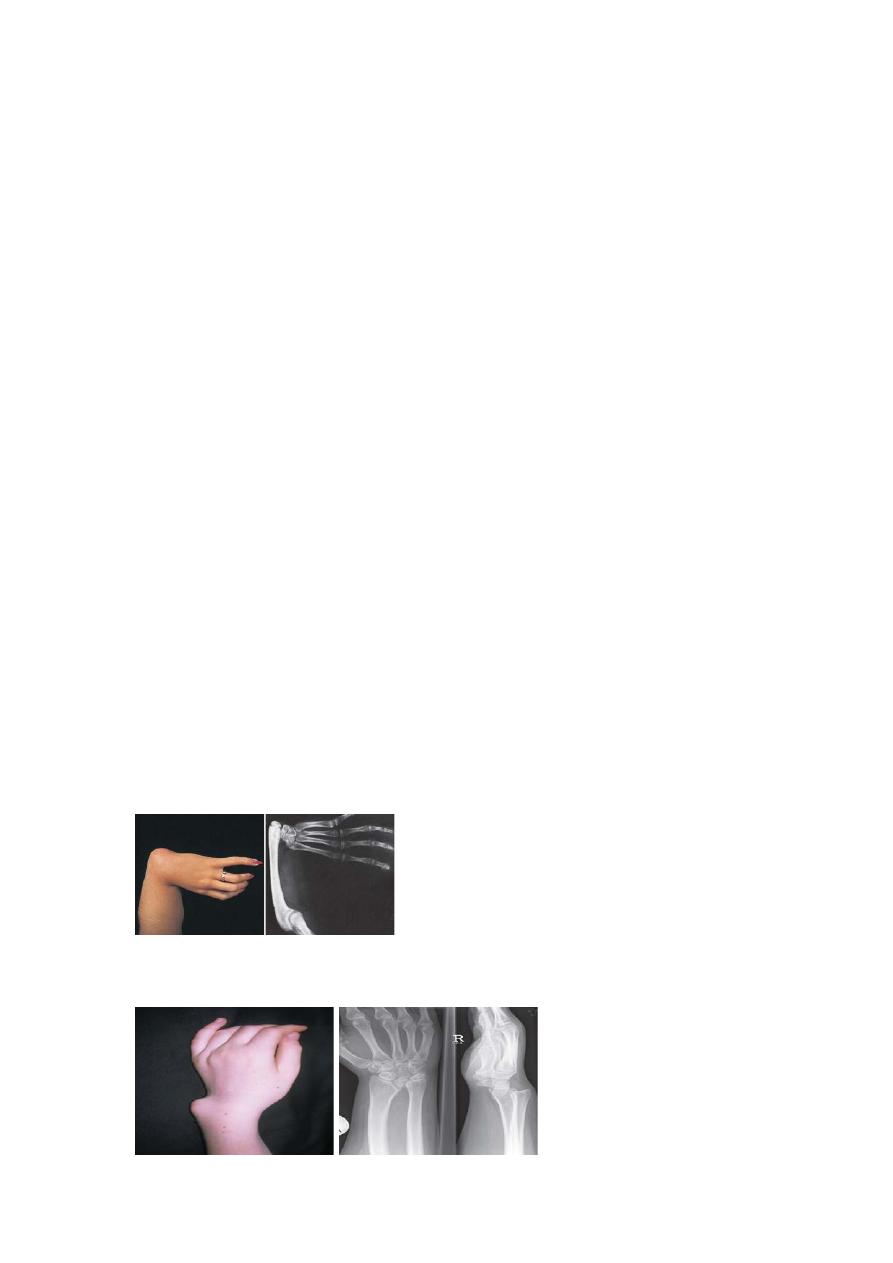
Radial dysplasia
The infant is born with the wrist in marked radial deviation, hence the common name radial
club-hand; one-half of the patients are affected bilaterally. There is absence of the whole or
part of the radius, and usually also the thumb.
Treatment in the neonate consists of gentle stretching and splintage. Serious cases can be
treated by distraction prior to a tension-free softtissue correction which has less effect on
growth of the carpus and distal ulna than the older technique of ‘centralizing’ the carpus over
the remaining forearm structures.
Madelung’s deformity
In this deformity the lower radius curves forwards(ventrally), carrying with it the carpus and
hand but leaving the distal end of the ulna projecting on the back of the wrist.
Acquired deformity
Physeal injuries can result in malunited fractures or subluxation of the distal radioulnar joint.
Osteotomy of the radius or stabilization of the ulna may be needed.
Non-traumatic deformities are seen typically in rheumatoid arthritis and cerebral palsy.
Tuberculosis
Tuberculous arthritis sometimes occurs at the wrist. Pain and stiffness come on gradually and
the hand feels weak. The forearm looks wasted; the wrist is swollen and feels warm.
X-ray examination shows localized osteoporosis and irregularity of the radiocarpal and
intercarpal joints, and sometimes bone erosion.
Treatment
Antituberculous drugs are given and the wrist is splinted. If an abscess forms, it must be
drained.
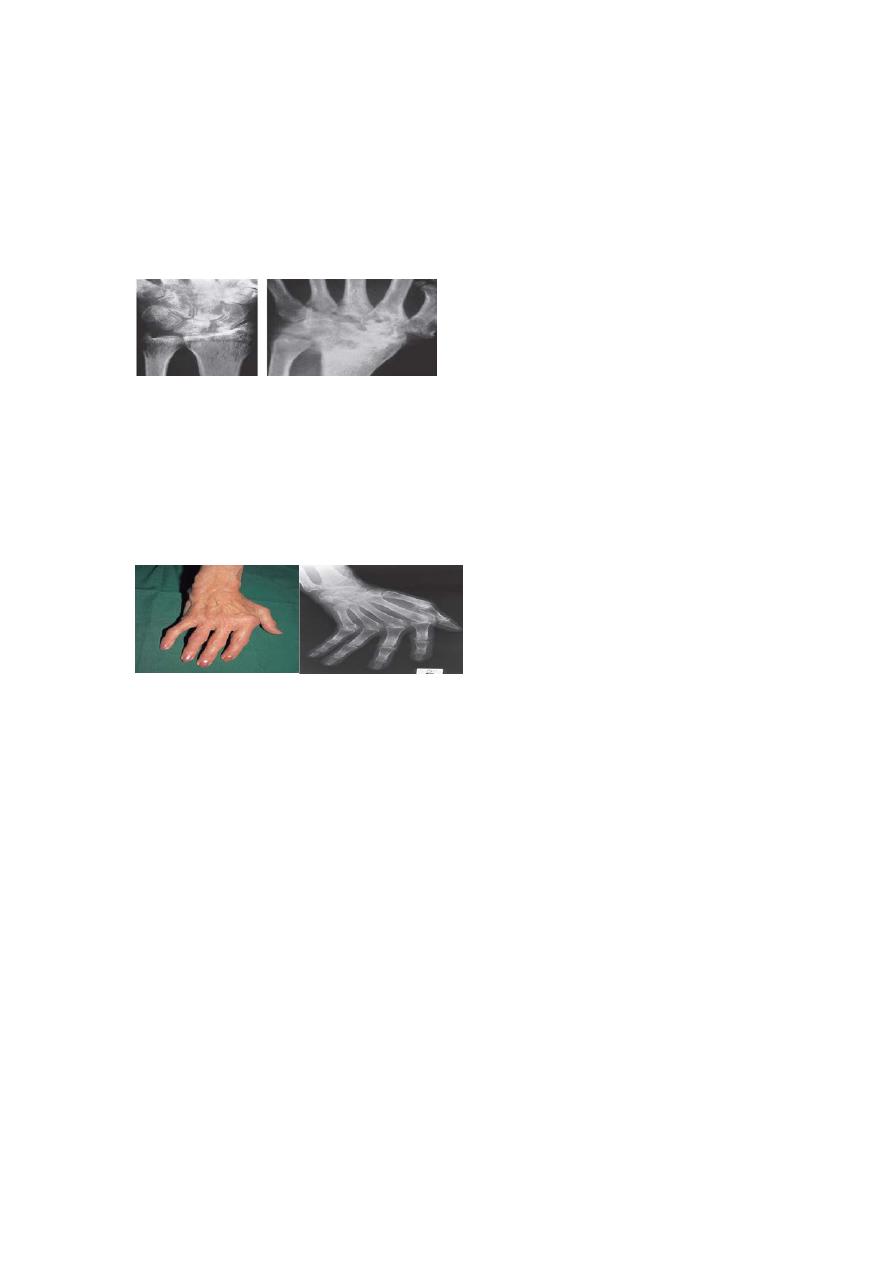
Rheumatoid arthritis
Clinical features
After the metacarpophalangeal joints, the wrist is the most common site of rheumatoid
arthritis. Pain, swelling and tenderness may at first be localized to the radioulnar joint, or to
one of the tendon sheaths. Sooner or later the whole wrist becomes involved and tenderness is
much more ill defined. In late cases the wrist is deformed and unstable.
X-rays show the characteristic features of osteoporosis and bony erosions.
Treatment
Management in the early stage consists of splintage and local injection of corticosteroids,
combined with systemic treatment. Persistent synovitis (usually affecting the extensor tendon
sheaths) may call for synovectomy and soft-tissue stabilization of the wrist.
In the late stage, tendon ruptures at the wrist, joint destruction, instability and deformity may
require reconstructive surgery, including either arthroplasty or arthrodesis.
Osteoarthritis
Osteoarthritis of the wrist joint proper is unusual except as a sequel to intra-articular injuries
of the distal radius or the carpal bones, or avascular necrosis of the lunate (Kienb
ِ◌ck’s
disease).
Osteoarthritis of the thumb carpometacarpal joint is common in postmenopausal women.
Careful examination will show that tenderness is sharply localized to the carpometacarpal
joint, about 1 cm distal to the radial styloid process.
Heberden’s nodes of the finger joints are common. In late cases, fixed adduction of the first
metacarpal produces a characteristic deformity. X-ray examination shows the usual features
of joint-space narrowing, sclerosis and osteophyte formation.
Treatment
Local injection of corticosteroid usually relieves pain, and movements may improve. If this
fails, operation may be advisable.
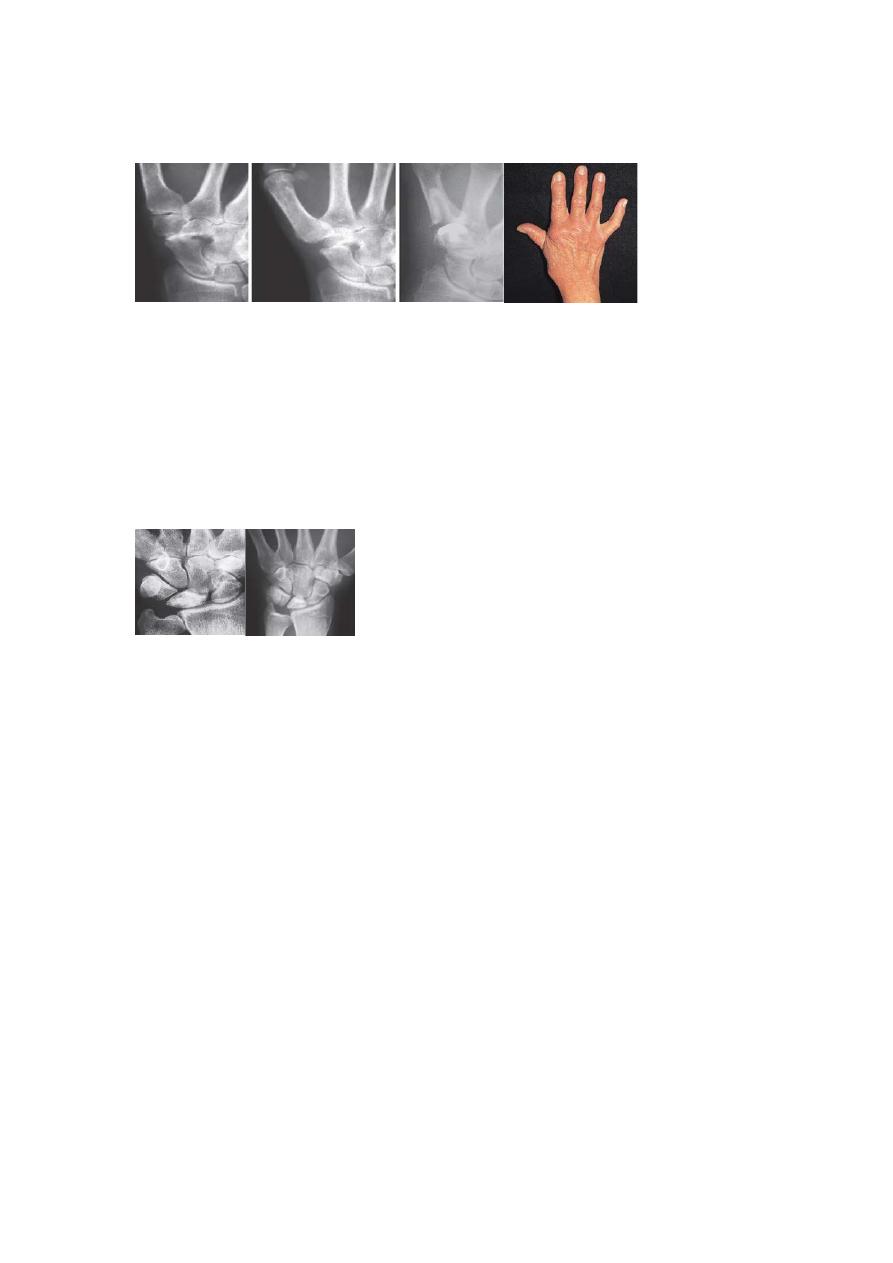
Kienböck’s disease
After injury or stress, the lunate bone sometimes develops a patchy avascular necrosis. A
predisposing factor may be relative shortening of the ulna (negative ulnar variance), which
could result in excessive stress being applied to the lunate where it is squeezed between the
distal surface of the (overlong) radius and the second row of carpal bones.
Clinical features
The patient, usually a young adult, complains of ache and stiffness. Tenderness is localized to
the centre of the wrist on the dorsum; wrist extension may be limited.
Imaging
The earliest signs of osteonecrosis can be detected only by MRI. Typical x-ray signs are
increased density in the lunate and, later, flattening and irregularity of the bone. Ultimately
there may be features of osteoarthritis of the wrist
.
Treatment
During the early stage, while the shape of the lunate is more or less normal, osteotomy of the
distal end of the radius may reduce pressure on the bone and thereby protect it from
collapsing. In late cases, partial wrist arthrodesis or proximal row excision or even joint
replacement are considered.
Tenosynovitis and tenovaginitis
The extensor retinaculum contains six compartments which transmit tendons lined with
synovium.
Tenosynovitis can be caused by unaccustomed movement; sometimes it occurs
spontaneously.
The resulting synovial inflammation causes secondary thickening of the sheath and stenosis
of the compartment, which further compromises the tendon. Early treatment, including rest,
anti-inflammatory medication and injection of corticosteroids, may break this vicious circle.
The first dorsal compartment (enclosing abductor pollicis longus and extensor pollicis brevis)
and the second dorsal compartment (extensor carpi radialis longus and brevis) are the ones
most commonly affected.
De Quervain’s disease
Tenovaginitis of the first dorsal compartment is usually seen in women between the ages of
30 and50 years. There may be a history of unaccustomed activity, such as pruning roses,
cutting with scissors or wringing out clothes. It is quite common shortly after childbirth.
Clinical features
Pain, and sometimes swelling, is localized to the radial side of the wrist. The tendon sheath
feels thick and hard. Tenderness is most acute at the very tip of the radial styloid.
The pathognomonic sign is elicited by Finkelstein’s test.

Treatment
In early cases, symptoms can be relieved by ultrasound therapy or a corticosteroid injection
into the tendon sheath, sometimes combined with splintage of the wrist. Resistant cases need
an operation, which consists of slitting the thickened tendon sheath.
Ganglion
The ubiquitous ganglion is seen most commonly on the back of the wrist. It arises from cystic
degeneration in the joint capsule or tendon sheath. The distended cyst contains a glairy fluid.
The patient, often a young adult, presents with a painless lump, usually on the back of the
wrist, but sometimes on the front. Occasionally there is a slight ache. The lump is well
defined, cystic and not tender. It may be attached to one of the tendons. The ganglion often
disappears after some months, so there should be no haste about treatment. If the lesion
continues to be troublesome, it can be aspirated; if it recurs, excision is justified, but the
patient should be told that there is a 30% risk of recurrence, even after careful surgery.
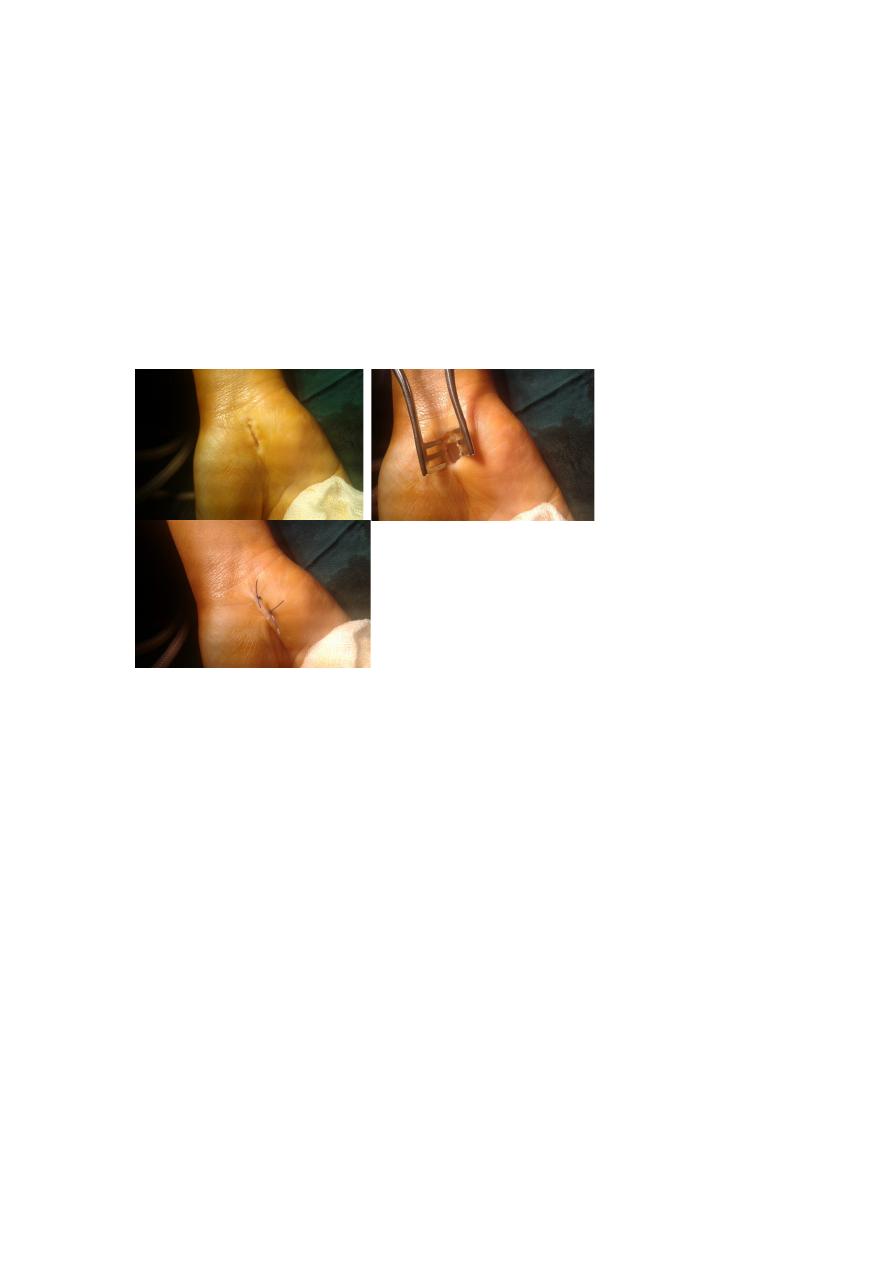
Carpal tunnel syndrome
This is the commonest and best known of all the nerve entrapment syndromes. In the normal
carpal tunnel there is barely room for all the tendons and the median nerve; consequently, any
swelling is likely to result in compression and ischaemia of the nerve. Usually the cause
eludes detection; the syndrome is, however, common in women at the menopause, in
rheumatoid arthritis, in pregnancy and in myxoedema. The usual age group is 40–50 years.
Clinical features
The history is most helpful in making the diagnosis. Pain and paraesthesia occur in the
distribution of the median nerve in the hand. Night after night the patient is woken with
burning pain, tingling and numbness. Patients tend to seek relief by hanging the arm over the
side of the bed or shaking the arm; however, merely changing the position of the wrist will
usually help.
Early on there is little to see, but there are two helpful tests: sensory symptoms can often be
reproduced by percussing over the median nerve (Tinel’s sign) or by holding the wrist fully
flexed for a minute(Phalen’s test). In late cases there is wasting of the thenar muscles,
weakness of thumb abduction and sensory dulling in the median nerve territory.
Electrodiagnostic tests, which show slowing of nerve conduction across the wrist, are
reserved for those with atypical symptoms.
Radicular symptoms of cervical spondylosis may confuse the diagnosis and may coincide
with carpal tunnel syndrome.
Treatment
Light splints that prevent wrist flexion can help those with night pain or with pregnancy-
related symptoms. Steroid injection into the carpal canal, likewise, provides temporary relief.
Open surgical division of the transverse carpal ligament usually provides a quick and simple
cure; this can usually be done under local anaesthesia.
