
The knee
dr.Mushtaq Talib Hussein
F.I.B.M.S(Ortho.) C.A.B.O(Ortho.)
LESIONS OF THE MENISCI
The menisci have an important role in (1) improving articular congruency and
increasing the stability of the knee, (2) controlling the complex rolling and gliding
actions of the joint and (3) distributing load during movement.
The medial meniscus is much less mobile than the lateral, and it cannot as easily
accommodate to abnormal stresses. This may be why meniscal lesions are more
common on the medial side than on the lateral.
TEARS OF THE MENISCUS
The meniscus consists mainly of circumferential fibres held by a few radial strands. It
is, therefore, more likely to tear along its length than across its width.
Pathology
The medial meniscus is affected far more frequently than the lateral, partly because its
attachments to the capsule make it less mobile. Tears of both menisci may occur with
severe ligament injuries.
In 75 per cent of cases the split is vertical in the length of the meniscus. If the
separated fragment remains attached front and back, the lesion is called a bucket-
handle tear.
Horizontal tears are usually ‘degenerative’ or due to repetitive minor trauma. Some
are associated with meniscal cysts.
Most of the meniscus is avascular and spontaneous repair does not occur unless the
tear is in the outer third.
Clinical features
The patient is usually a young person who sustains a twisting injury to the knee on the
sports field. Pain(usually on the medial side) is often severe and further activity is
avoided; occasionally the knee is ‘locked’ in partial flexion. Almost invariably,
swelling appears some hours later, or perhaps the following day.
‘Locking’ – that is, the sudden inability to extend the knee fully – suggests a
bucket-handle tear.
On examination the joint may be held slightly flexed and there is often an effusion. In
longstanding cases the quadriceps will be wasted. Tenderness is localized to the joint
line, in the vast majority of cases on the medial side.
The history is helpful, and McMurray’s test, Apley’s grinding test or the Thessaly
test may be positive.
McMurray’s test is performed at varying angles of flexion.
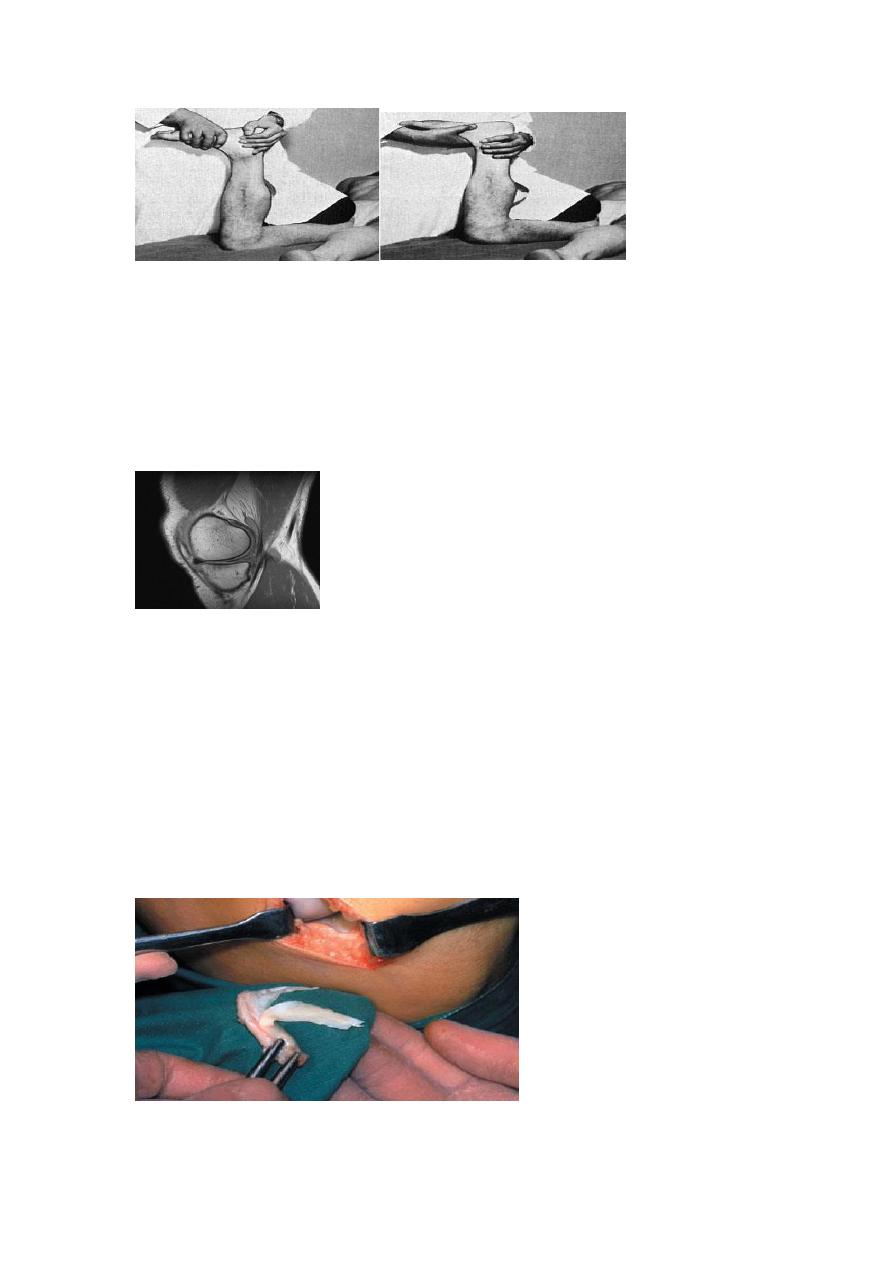
(a) (b)
(a)The grinding test relaxes the ligaments but compresses the meniscus – it causes
pain with meniscus lesions.
(b)The distraction test releases the meniscus but stretches the ligaments and causes
pain if these are injured.
Investigations
Plain x-rays are usually normal, but MRI is a reliable method of confirming the
clinical diagnosis, and may even reveal tears that are missed by arthroscopy.
Arthroscopy has the advantage that, if a lesion is identified, it can be treated at the
same time.
Treatment
Dealing with the locked knee Usually the knee unlocks spontaneously; if not, gentle passive
flexion and rotation may do the trick.
Conservative treatment If the joint is not locked, it is reasonable to hope that the tear is
peripheral and can therefore heal spontaneously.
Operative treatment Surgery is indicated (1) if the joint cannot be unlocked and (2) if
symptoms are recurrent. For practical purposes, the lesion is often dealt with as part of the
‘diagnostic’ arthroscopy.
Tears close to the periphery, which have the capacity to heal, can be sutured; at least one edge
of the tear should be red (i.e. vascularized).
Tears other than those in the peripheral third are dealt with by excising the torn portion (or the
bucket handle).
Recurrent dislocation of the Patella
In 15–20 per cent of cases (mostly children) the first episode is followed by recurrent
dislocation or subluxation after minimal stress. This is due, in some measure, to
disruption or stretching of the ligamentous structures which normally stabilize the
extensor mechanism.
predisposing factors are: (1) generalized ligamentous laxity; (2) under - development
of the lateral femoral condyle and flattening of the intercondylar groove; (3)
maldevelopment of the patella, which may be too high or too small; (4) valgus
deformity of the knee; (5) external tibial torsion; or (6) a primary muscle defect.
Dislocation is almost always towards the lateral side.
Clinical features
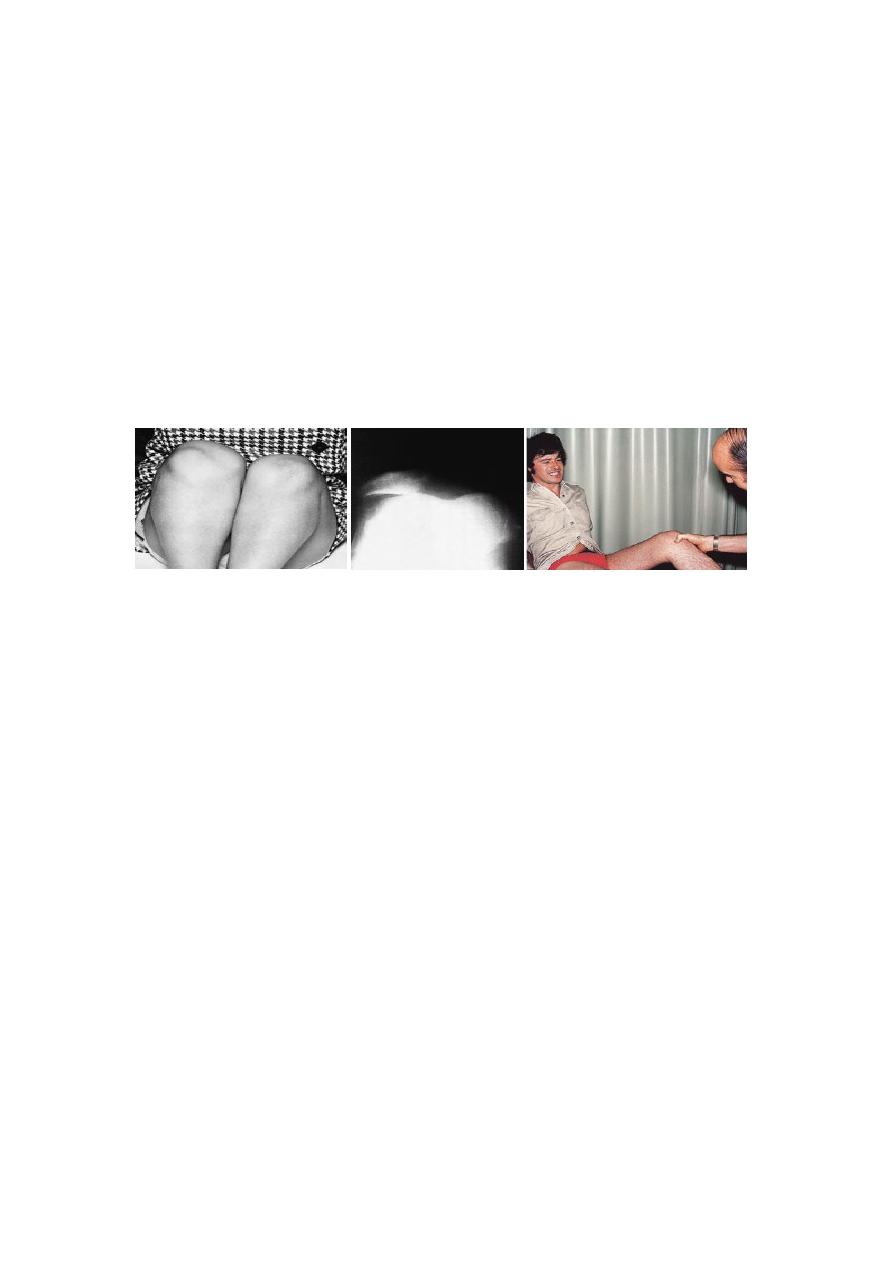
Girls are affected more commonly than boys and the condition may be bilateral.
Dislocation occurs unexpectedly when the quadriceps muscle is contracted with the
knee in flexion. There is acute pain, the knee is stuck in flexion and the patient may
fall to the ground.
The apprehension test:
More often the patella has reduced by the time the patient is seen. Tenderness and
swelling may still be present and the apprehension test is positive: if the patella is
pushed laterally with the knee slightly flexed, the patient resists and becomes anxious,
fearing another dislocation.
Treatment
If the patella is still dislocated, it is pushed back into place while the knee is gently
extended. The only indications for immediate surgery are (1) inability to reduce the
patella (e.g. with a rare ‘intra-articular’ dislocation), and (2) the presence of a
large, displaced osteochondral fragment.
A plaster cylinder or splint is applied and retained for 2–3 weeks;
Operative treatment
The principles of operative treatment are (a) to repair or strengthen the medial patello-
femoral ligaments, and (b) to realign the extensor mechanism so as to produce a
mechanically more favorable angle of pull.
LOOSE BODIES
The knee – relatively capacious, with large synovial folds – is a common haven for
loose bodies. These may be produced by: (1) injury (a chip of bone or
cartilage); (2)
osteochondritis dissecans (which may produce one or two fragments); (3)
osteoarthritis (pieces of cartilage or osteophyte); (4) Charcot’s disease (large
osteocartilaginous bodies); and (5) synovial chondromatosis (cartilage metaplasia in
the synovium, sometimes producing hundreds of loose bodies).
Loose bodies may be symptomless. The usual complaint is attacks of sudden locking
without injury.
X-ray Most loose bodies are radio-opaque. The films also show an underlying joint
abnormality.
Treatment
A loose body causing symptoms should be removed unless the joint is severely
osteoarthritic. This can usually be done through the arthroscope
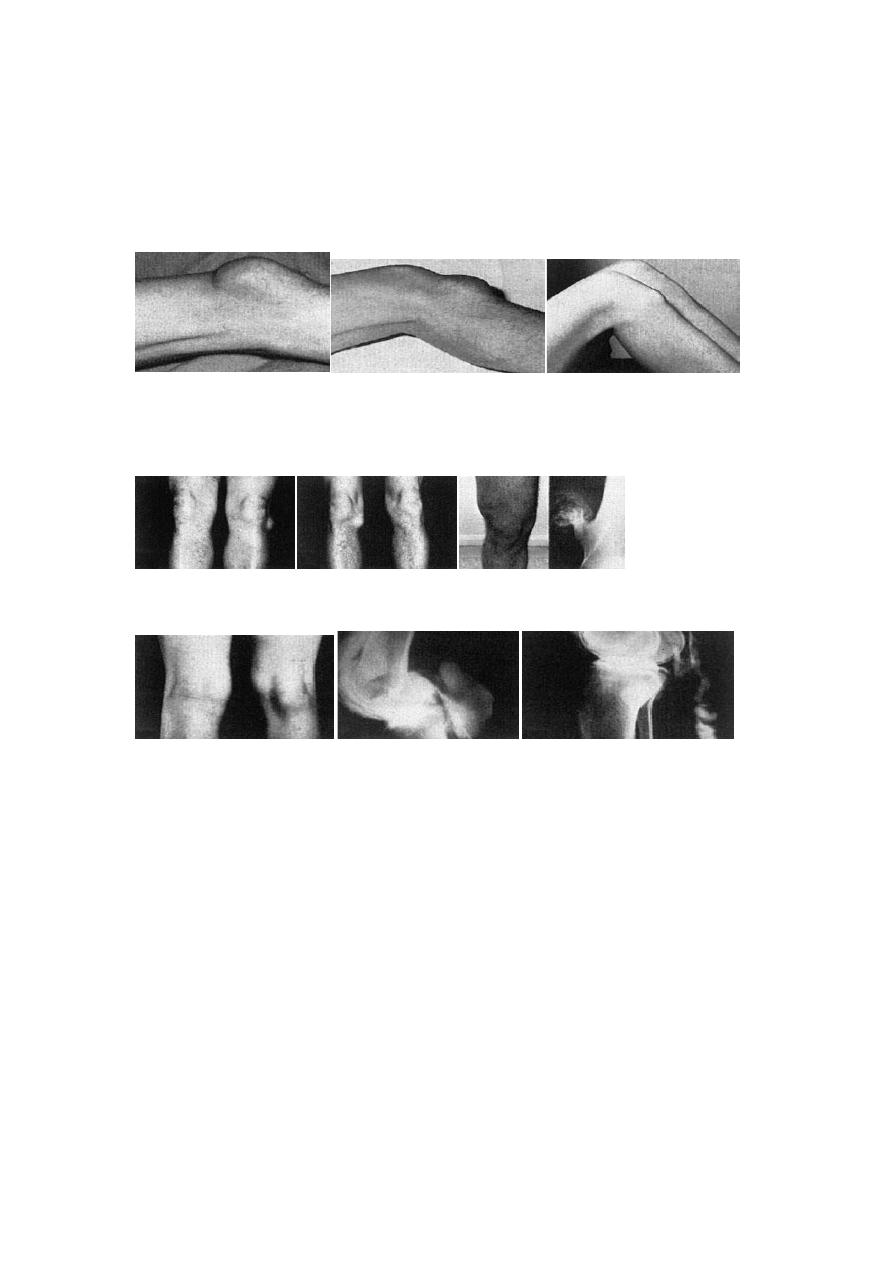
A b c
Lumps around the knee
In front:
(a)
prepatellar bursa;
(b)
infrapatellar bursa;
(c)
Osgood
–Schlatter disease.
D e f
On either side: (d) cyst of lateral meniscus; (e) cyst of medial meniscus; (f)
cartilagecapped exostosis.
G h i
Behind: (g) semimembranosus bursa; (h) arthrogram of popliteal cyst; (i) leaking cyst.
OSTEOARTHRITIS
The knee is the commonest of the large joints to be affected by osteoarthritis , often
there is a predisposing factor: injury to the articular surface, a torn meniscus,
ligamentous instability or preexisting deformity of the hip or knee, to mention a few.
However, in many cases no obvious cause can be found.
Osteoarthritis is often bilateral and in these cases there is a strong association with
Heberden’s nodes and generalized osteoarthritis.
Clinical features
Patients are usually over 50 years old; they tend to be overweight and may have
longstanding bow-leg deformity.
Pain is the leading symptom, worse after use, or (if the patello-femoral joint is
affected) on stairs. After rest, the joint feels stiff and it hurts to ‘get going’ after

sitting for any length of time. Swelling is common, and giving way or locking may
occur.
On examination there may be an obvious deformity(usually varus) or the scar of a
previous operation. The quadriceps muscle is usually wasted.
The natural history of osteoarthritis is one of alternating‘bad spells’ and ‘good
spells’.
X-ray
The anteroposterior x-ray must be obtained with the patient standing and bearing
weight
The tibio-femoral joint space is diminished(often only in one compartment) and there
is subchondral sclerosis. Osteophytes and subchondral cysts are usually present and
sometimes there is soft-tissue calcification in the suprapatellar region or in the joint
itself (chondrocalcinosis).
Treatment
If symptoms are not severe, treatment is conservative. Joint loading is lessened by
using a walking stick.
Quadriceps exercises are important. Analgesics are prescribed for pain, and warmth
(e.g. radiant heat or shortwave diathermy) is soothing.
Operative treatment
Persistent pain unresponsive to conservative treatment, progressive deformity and
instability are the usual indications for operative treatment.
Arthroscopic washouts
Patellectomy is indicated only in those rare cases where osteoarthritis is strictly
confined to the patellofemoral joint.
Realignment osteotomy is often successful in relieving symptoms and staving off the
need for ‘end-stage’ surgery. The ideal indication is a ‘young’ patient (under 50
years) with a varus knee and osteoarthritis confined to the medial compartment.
Replacement arthroplasty is indicated in older patients with progressive joint
destruction.
