Acute Osteomyelitis
Acute
osteomyelitis
is
infection
of
bone.
Osteo = bone
Myelo = bone marrow
Itis = inflammation
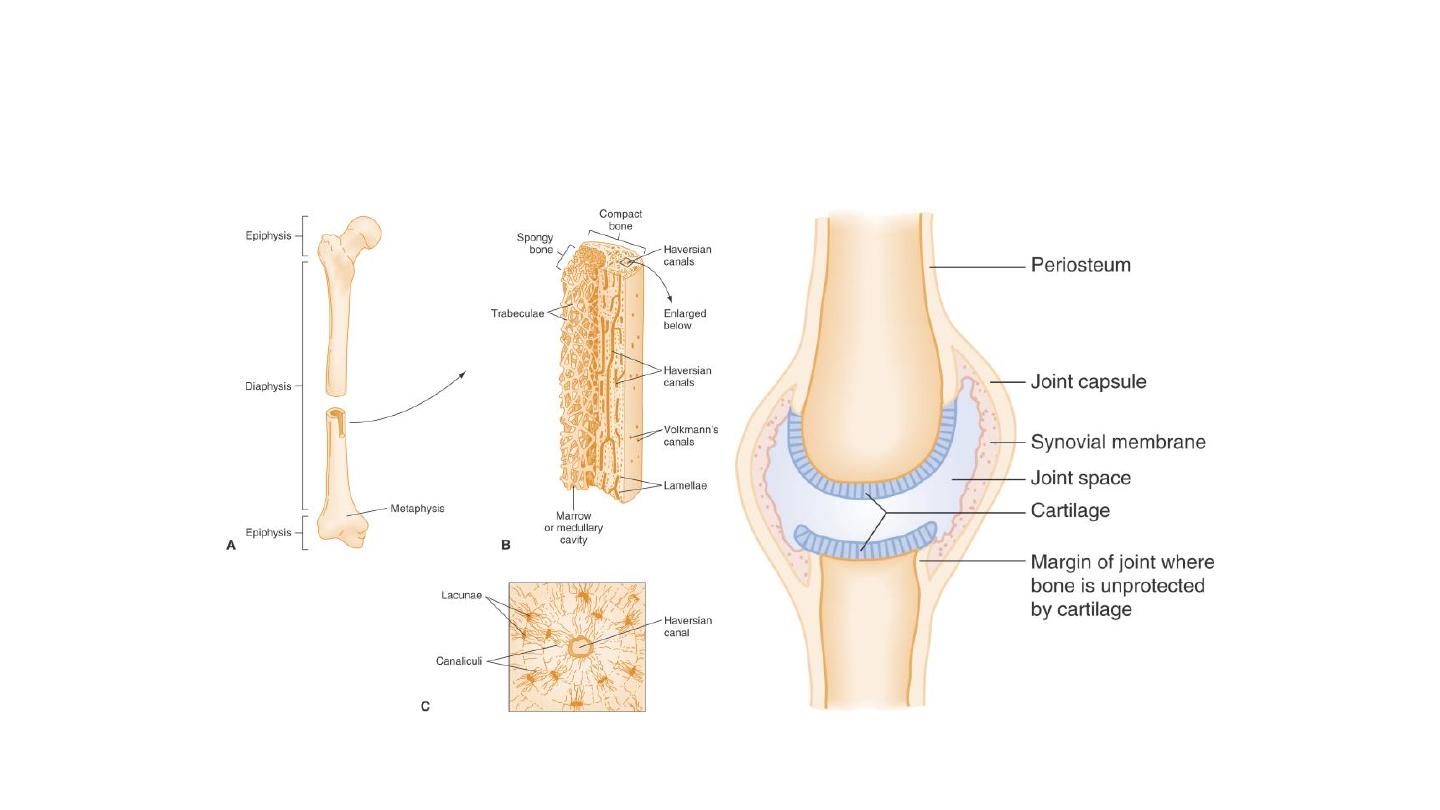
Anatomy Review - FYI

Etiology
• •
Staphylococcus aureus is the most common organism in all age groups
• • Salmonella
is
commonest
organism
in
sickle cell
anemia
patients
• • Pseudomonas aeurogenosa is
commonest
organism
in
Drug
abusers
• • Animal bite
–
Pasteurella
multiocida
• • Human bite
–
Eikenella
corrodens
• • Diabetic
ulcer
and
Fight
bites
–
Anaerobes
• • Immunocompromised (HIV) –
Staphylococcus aureus
• • Post-traumatic osteomyelitis/Post-surgical osteomyelitis –
• S. aureus
• • Open injuries –
Staphylococcus
• • Foot
injuries –
Pseudomonas
Pathology
• • Most common mode of
infection
is
hematogenous
• • In
children
metaphysis
of
long bone (usually
lower end femur >
upper
end tibia) is
earliest
and
most commonly involved
site
• • In
adults
commonest
site of
infection
is
thoracolumbar spine

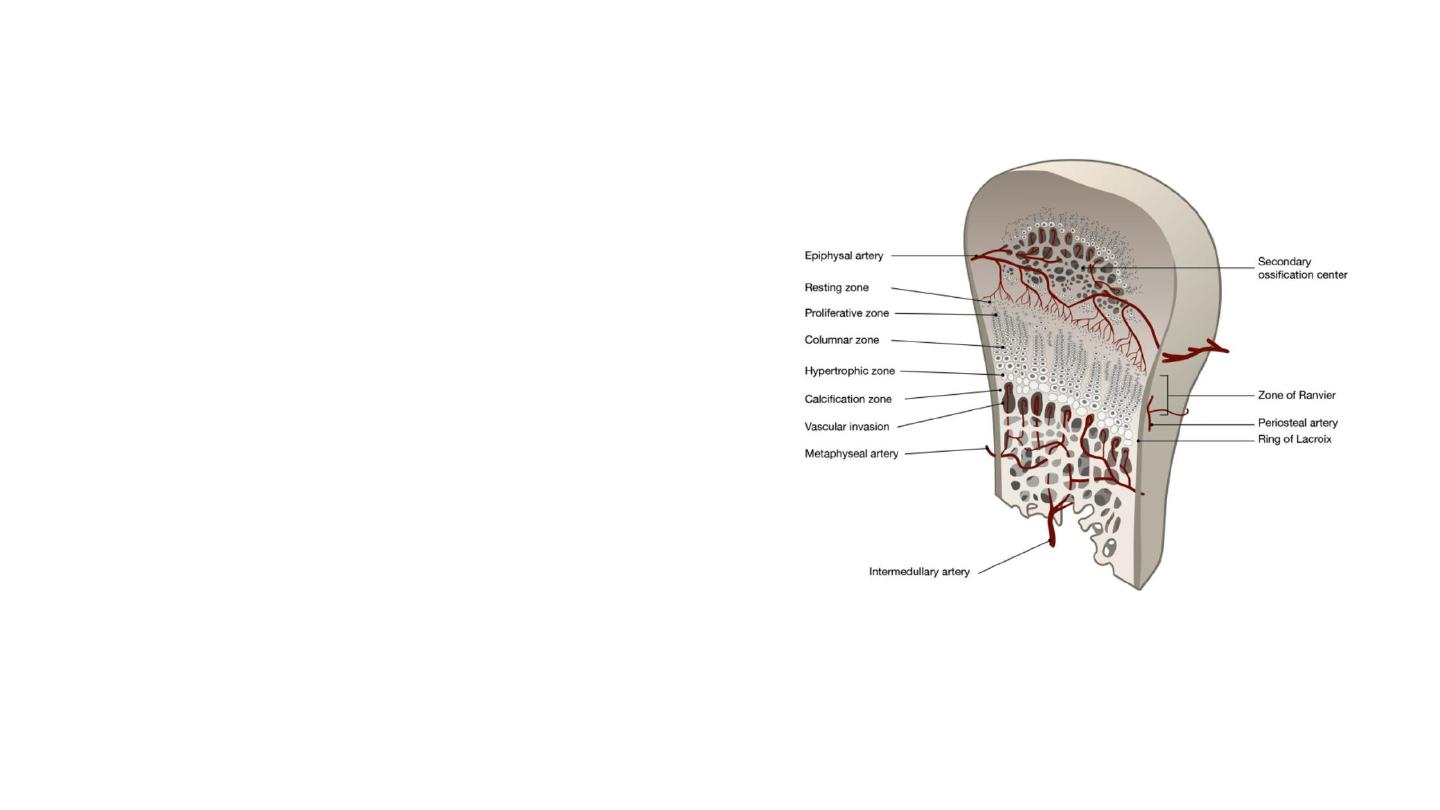
Starts in Metaphysis Because of:
• • Defective phagocytosis
in
metaphysis
(Inherently
depleted Reticuloendothelial System)
• • Rich blood
supply
• • Hair pin bend of
metaphyseal
vessels
(leads
to
vascular stasis)
• • Metaphyseal
hemorrhage
due to
repeated
trauma
(acts as
culture
media)
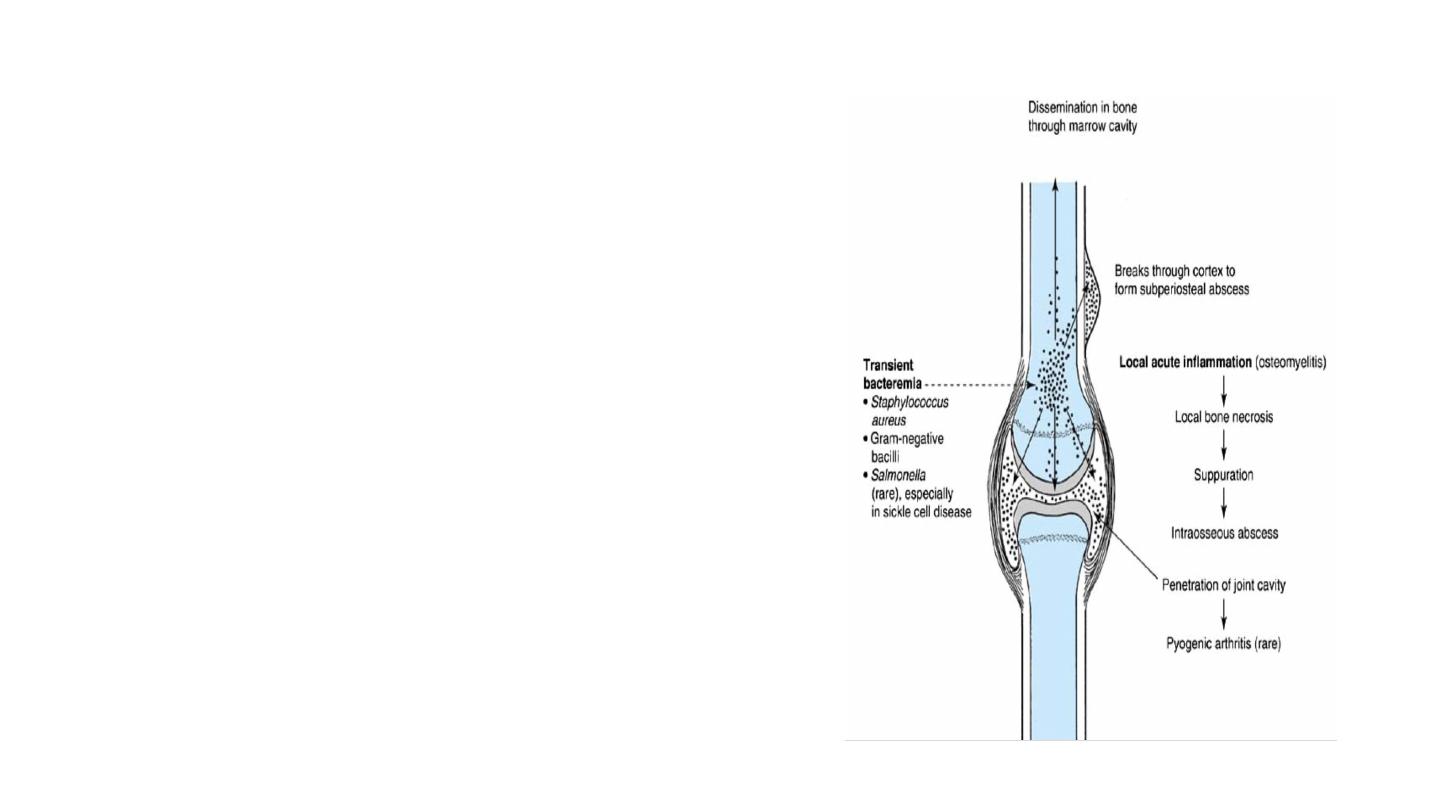
Pathophysiology
• i.
Metaphyseal Abscess is formed initially and it
spreads Subperiosteally
in children
because periosteum
is
loosely
attached to
bone
in
children and
in
adults pus
spreads to
Medullary
cavity
involving
the
Diaphysis.
• ii. Infectionrarely crosses growth plate
because it
has
no
blood
vessels and
periosteum
is
firmly
attached to
the
plate
at
this
level.
• iii. Joint
involvement
can
take
place
if metaphysisis
intracapsular
(e.g.
hip,
shoulder,
elbow).
• iv. The
pathological
sequence
is
inflammation,
suppuration,
necrosis,
reactive new
bone
formation
and
ultimately
resolution
and
healing. (Same sequence is seen in
HIV
positive patient also).
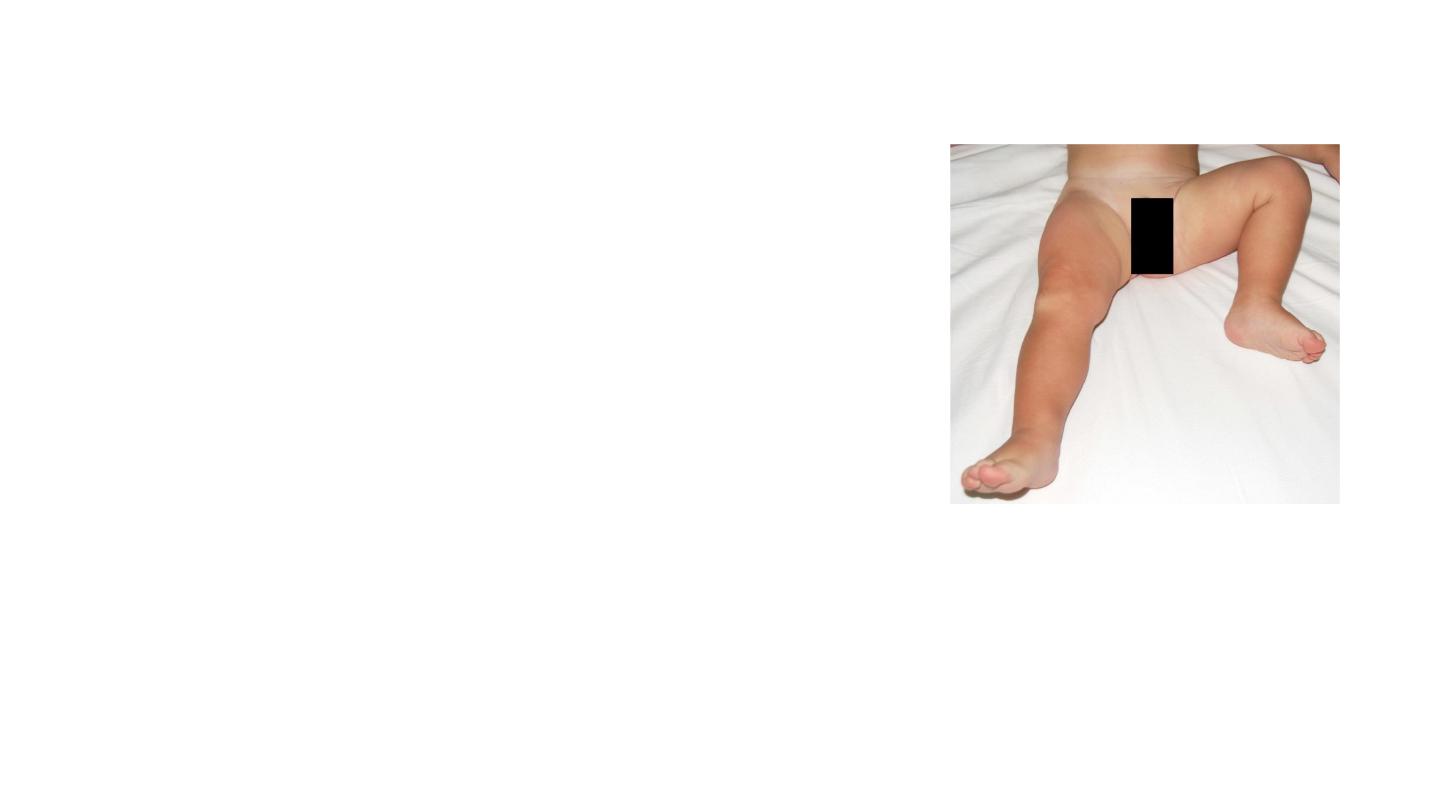
Clinical Feature
• • Fever (>38.3°C),
• swelling
of
the
limb,
• pain,
• systemic symptoms
(Toxic child)
• Note:
Systemic
signs are
absent in
immunocompromised
and
neonates.
• • Absent movements of
a
limb after
ruling out
trauma
in
pediatric
population
is
osteomyelitis till
proved
otherwise.

Investigation
•
increased
levels
of
Total
leucocyte
counts,
•
ESR
and
CRP.
•
X-rays
in
<24
hours
is
normal
•
•
1st change on X-rays is loss of soft tissue planes.
•
•
1st bony change is Periosteal reaction seen on day 7–10
(2nd week or day 10) Solid Periosteal Reaction.

• • Later features of
bone destruction
appear.

• MRI
is
considered
the best radiological
investigation
for
bone infections because
it
can identify
marrow edema
(seen
within
6
hours)
and soft tissue
extension in
bone
infections.
• • Tc99-MDP, Ga-67-
citrate
or
Indium
111 labelled
leucocytes
(Best out of
3)
are the
2nd best radiological
investigation.
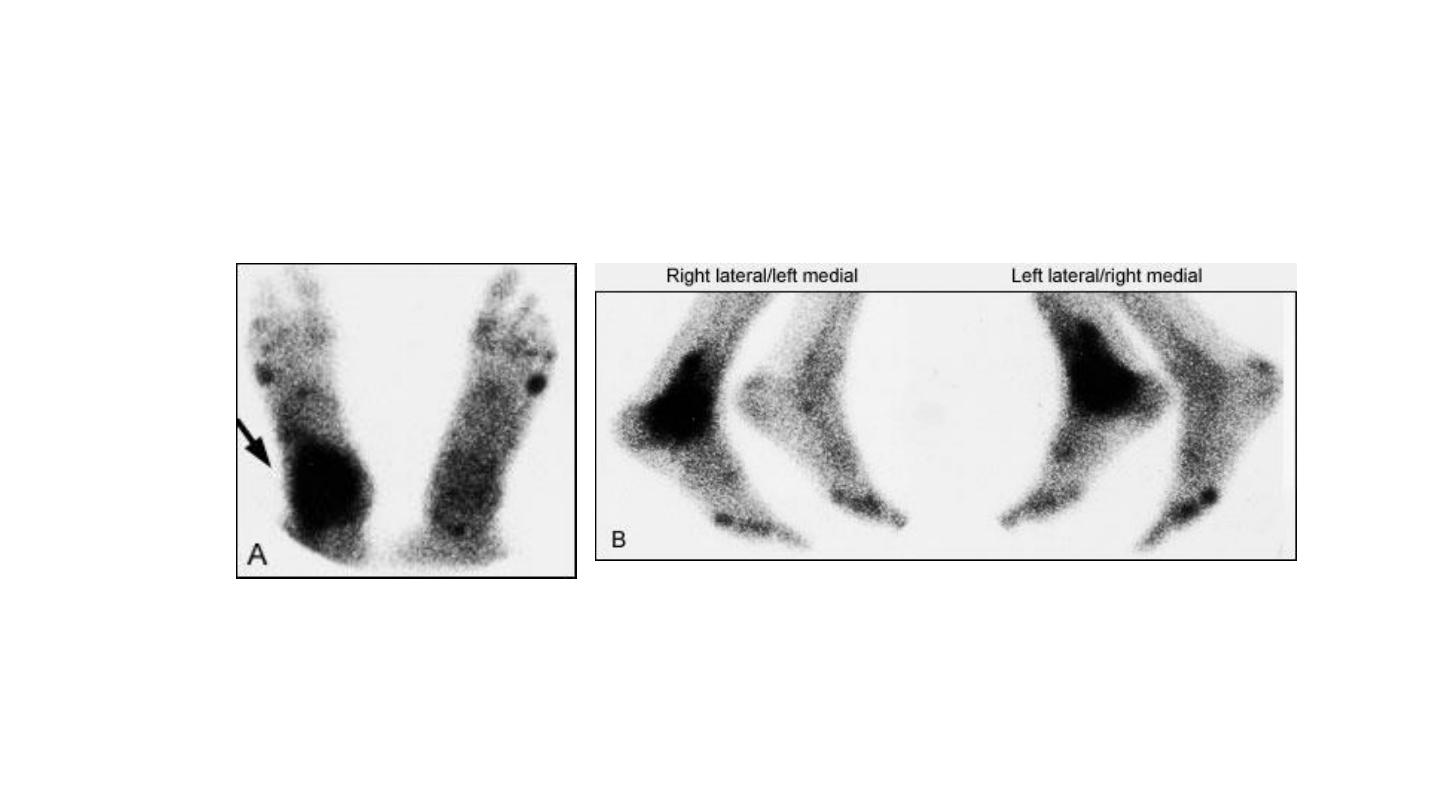
Bone scans, both anterior (A) and lateral (B), showing the
accumulation of radioactive tracer at the right ankle
(arrow). This focal accumulation is characteristic of
osteomyelitis.

• • Gold standard is always tissue diagnosis (from the lesion)
hence growth of organism on culture media is the best
investigation for infections.
• • Blood
Culture
is
positive
in
60% cases.

“Criteria for Diagnosis of Osteomyelitis”
•
Definite: Pathogen
isolated
from bone or
adjacent soft tissue
or
there is
histologic evidence of
osteomyelitis. –
Probable: Blood
culture
positive
+
Clinical
(absent
movements
of
the limb) +
Radiological
diagnosis. –
•
Likely: Typical clinical
findings
and
definite
radiographic
evidence of
OM +
Response to
antibiotics.

Treatment
• Osteomyelitis < 24 Hours
• • X-ray –
No
Loss of
Soft tissue planes
• • MRI –
Marrow
changes
in
metaphysis
• • Bone Scan –
Increased activity
• • Treatment is
started
with, IV
antibiotics
until condition begins
to
improve
or
CRP values
return
to
normal,
usually
for
2
weeks.
There after
antibiotics are given orally for
another
4
weeks.
•

• The
CRP increases within
6
hours
of
infection, reaches
a
peak elevation 2
days after
infection, and returns
to
normal
within
1
week after adequate treatment has begun.
So
CRP
is
better
indicator of
infection as
compared
to
ESR.
• • Peak elevation of
the ESR occurs
at
3–5 days
after infection and returns
to
normal
approximately 3
weeks
after treatment is
begun.
•
If
antibiotics are given early (<24
hours),
drainage is
often unnecessary.

• • Change
of
antibiotics or
Surgery
is
considered if
no improvement
occurs
within
48 hours
of
antibiotics.
• Osteomyelitis > 24 Hours
• • X-ray – Loss of Soft tissue planes
• • MRI –
Marrow
changes in
metaphysis
• • Bone Scan –
Increased activity

Treatment
•
Evacuation and Exploration
of
pus drainage is
followed by antibiotics course of antibiotics is
same as
Osteomyelitis < 24
Hours, i.e. for 2 weeks
I/V and 4
weeks
oral. The antibiotics that
cover staphylococcus aureus
are preferred and
ones that have both Oral and injectable preparation
are preferred, e.g. Amoxy-Clavulanic

SUBACUTE OSTEOMYELITIS (Brodie’s Abscess)
• Seen in Immuno-Competent Host!
• • It
is
long standing localized pyogenic
abscess
in
the bone (long standing
because of
strong
defence
mechanism
of
body).
• • It
usually
involves long bones
(metaphysis
or
diaphysis) e.g. Upper
end tibia.
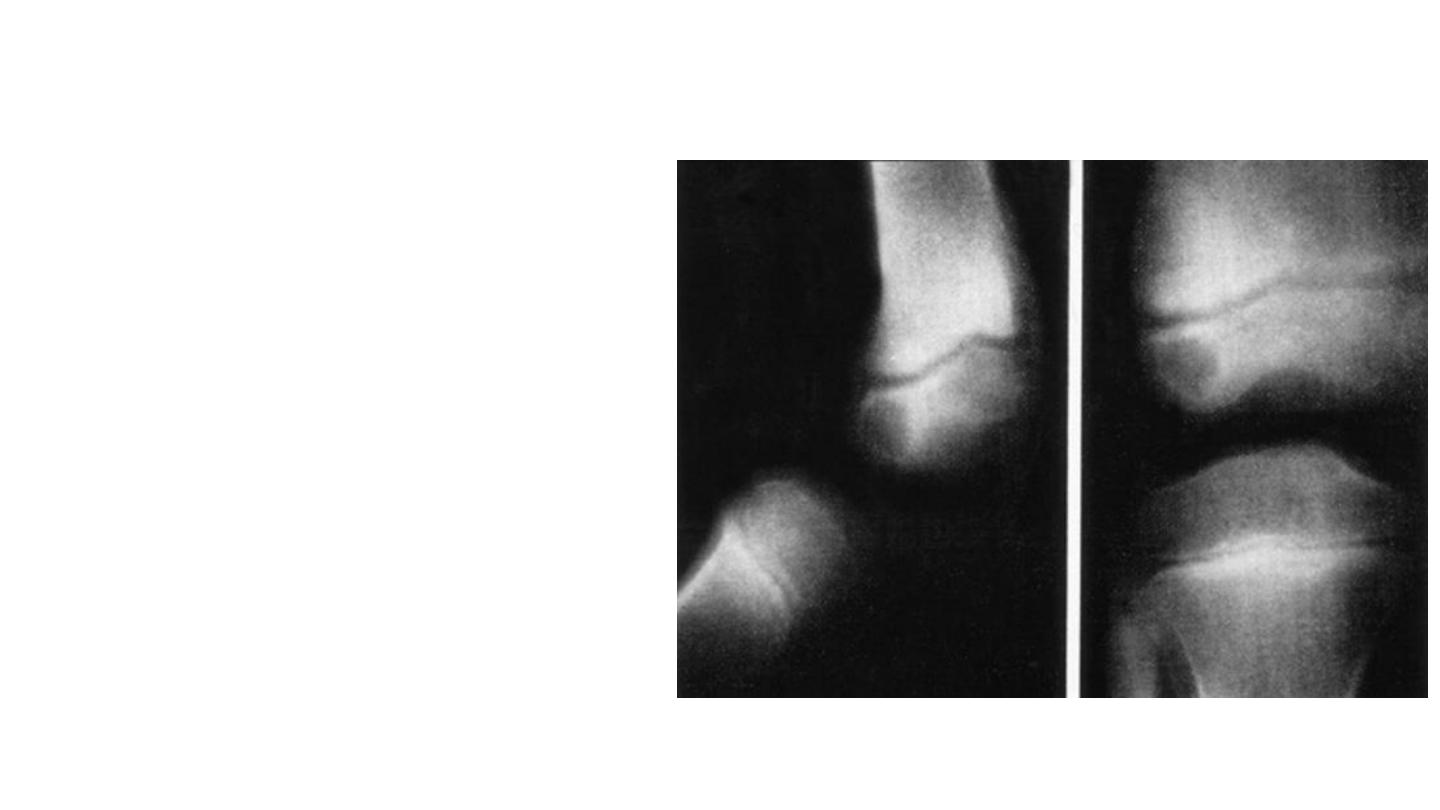
• • Classical Brodie’s
abscess
looks like a
small walled
off
(Sclerotic margins)
cavity
in
bone
with little or
no
periosteal reaction.

Treatment
• Trial
of
injectable antibiotics is
given if
it
fails
curettage of
the cavity
is
carried
out.
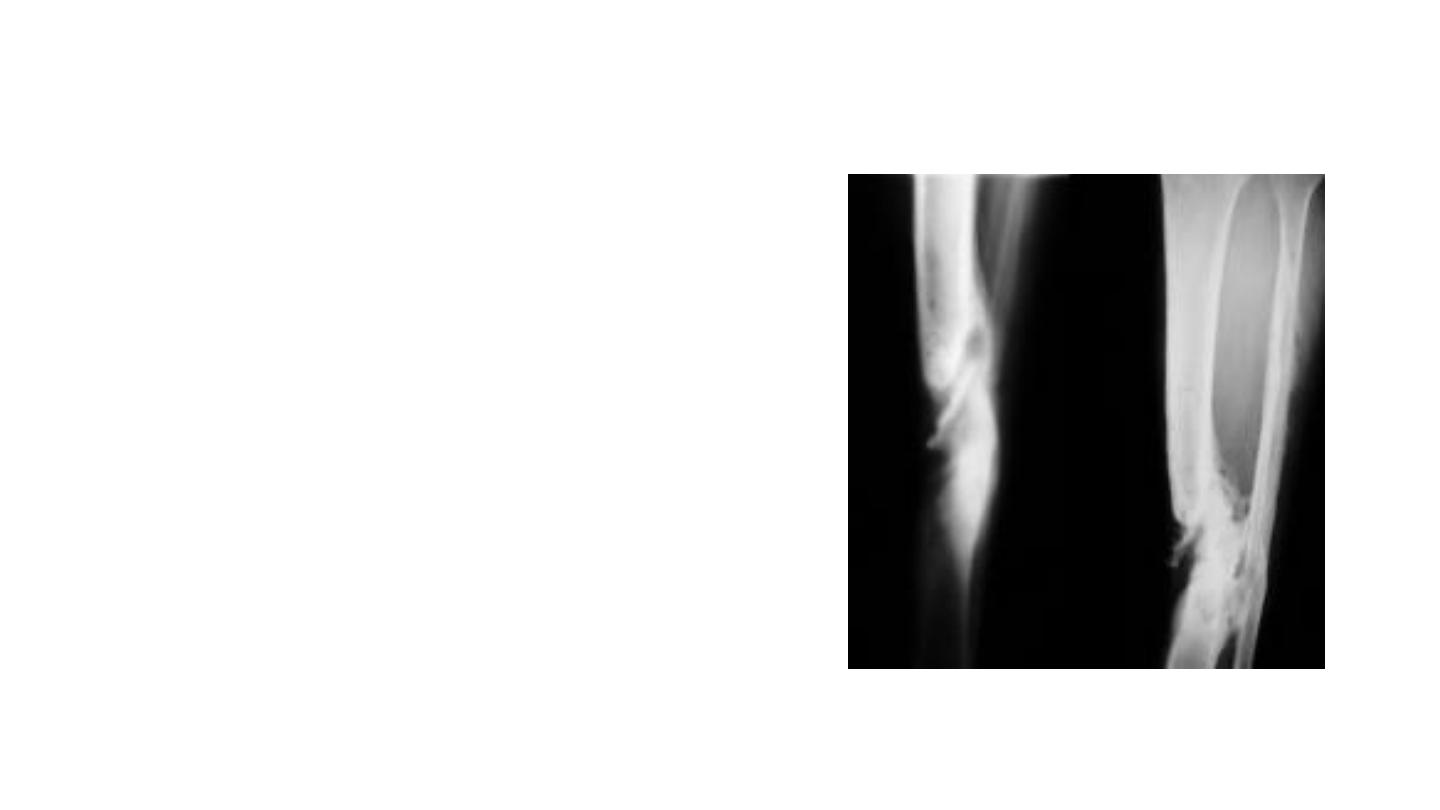
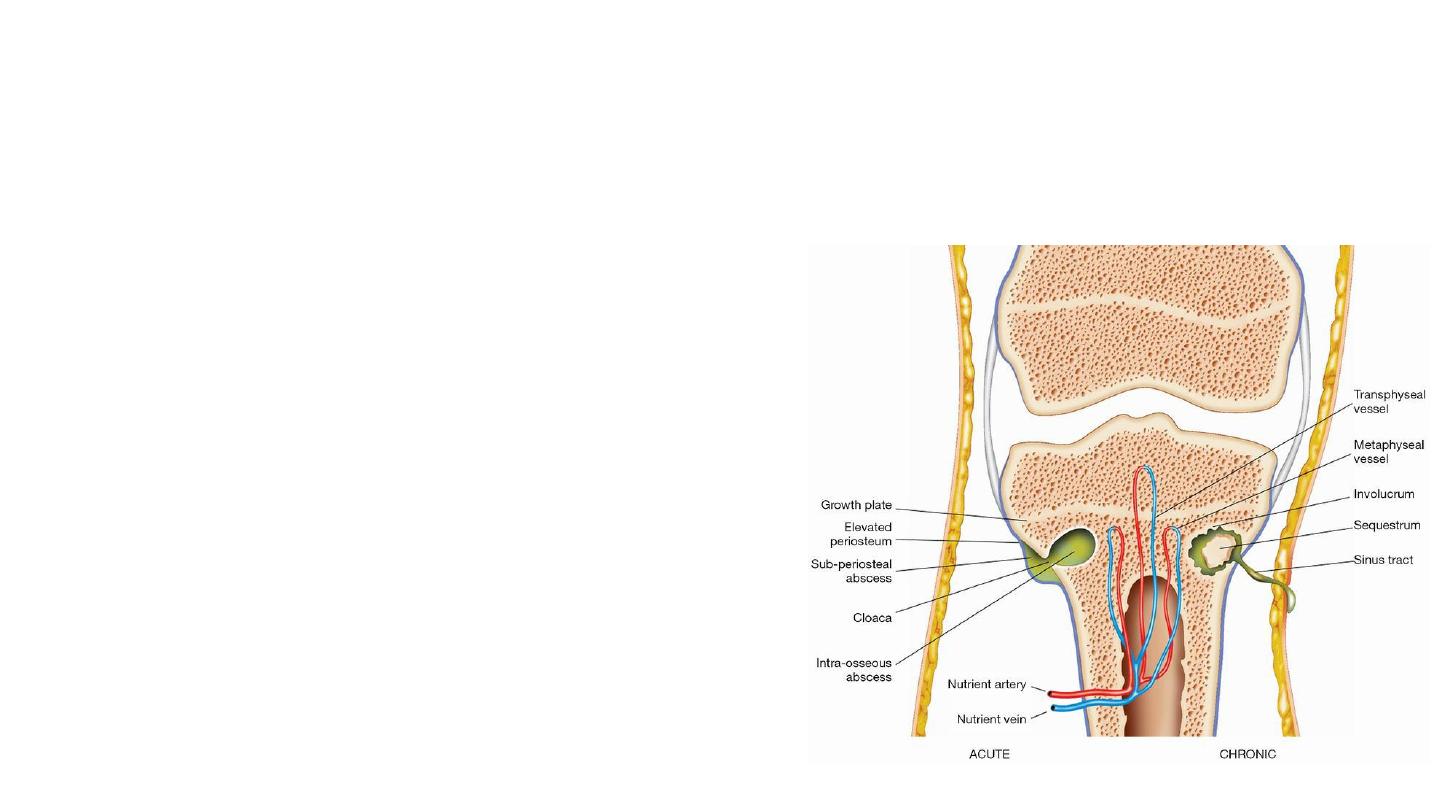
CHRONIC OSTEOMYELITIS
• “USUALLY A SEQUELAE OF
INADEQUATELY TREATED ACUTE
OSTEOMYELITIS”
• Sequestrum: Avascular piece of
bone surrounded by
granulation tissue, it
is
pathognomic
of
chronic
osteomyelitis.
• • It
acts as
nidus of
infection
and is
most
common
cause of
non-
healing
sinus in
chronic
osteomyelitis.
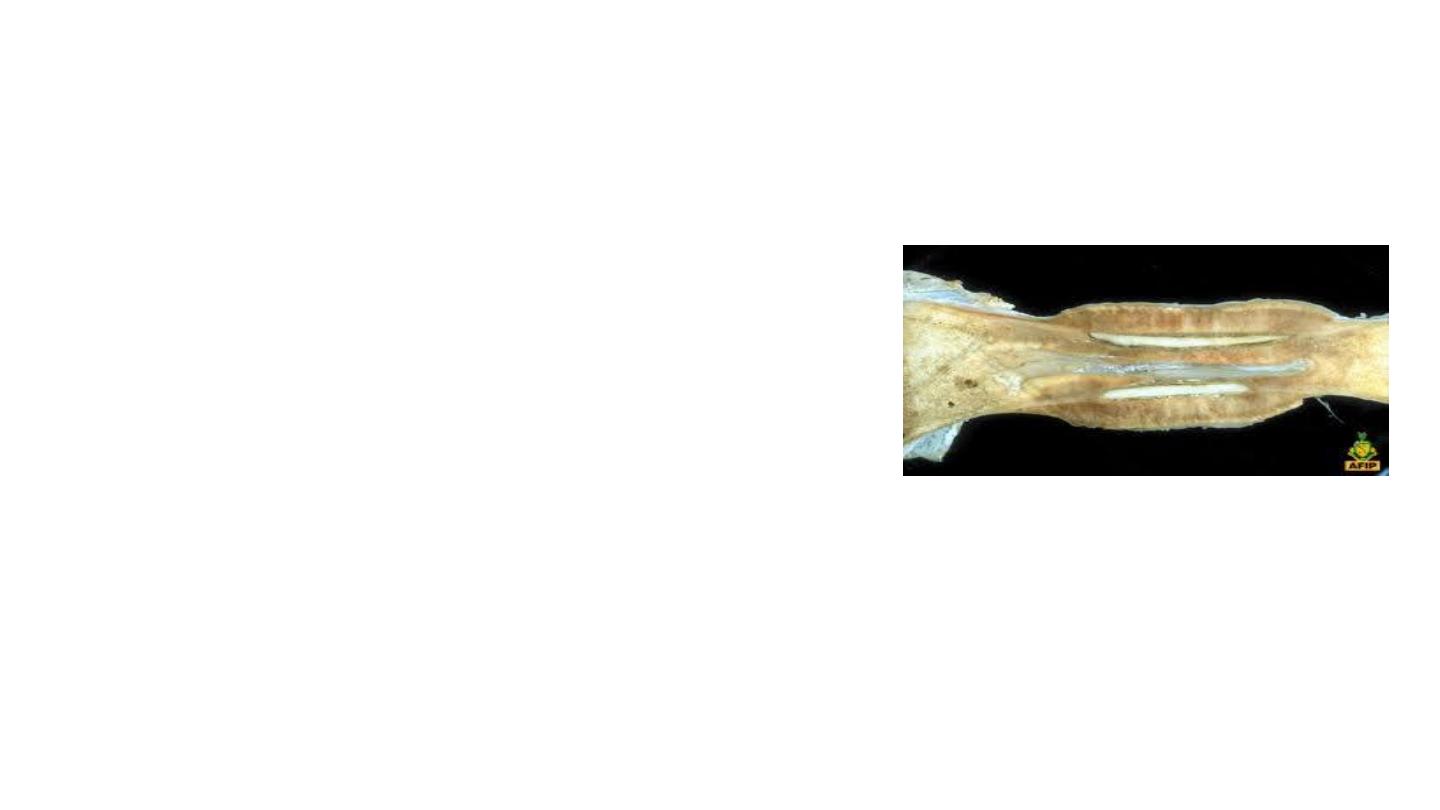
• Involucrum
is
dense sclerotic
new bone surrounding the
sequestrum
formed
from
deep layers of
stripped
periosteum (usually
obvious
by
the
end of
2nd
week).
At
least 2/3rd
surface
of
sequestrum
should
be
surrounded by
involucrum before
carrying
out
sequestrectomy
(Removal
of
Sequestrum).
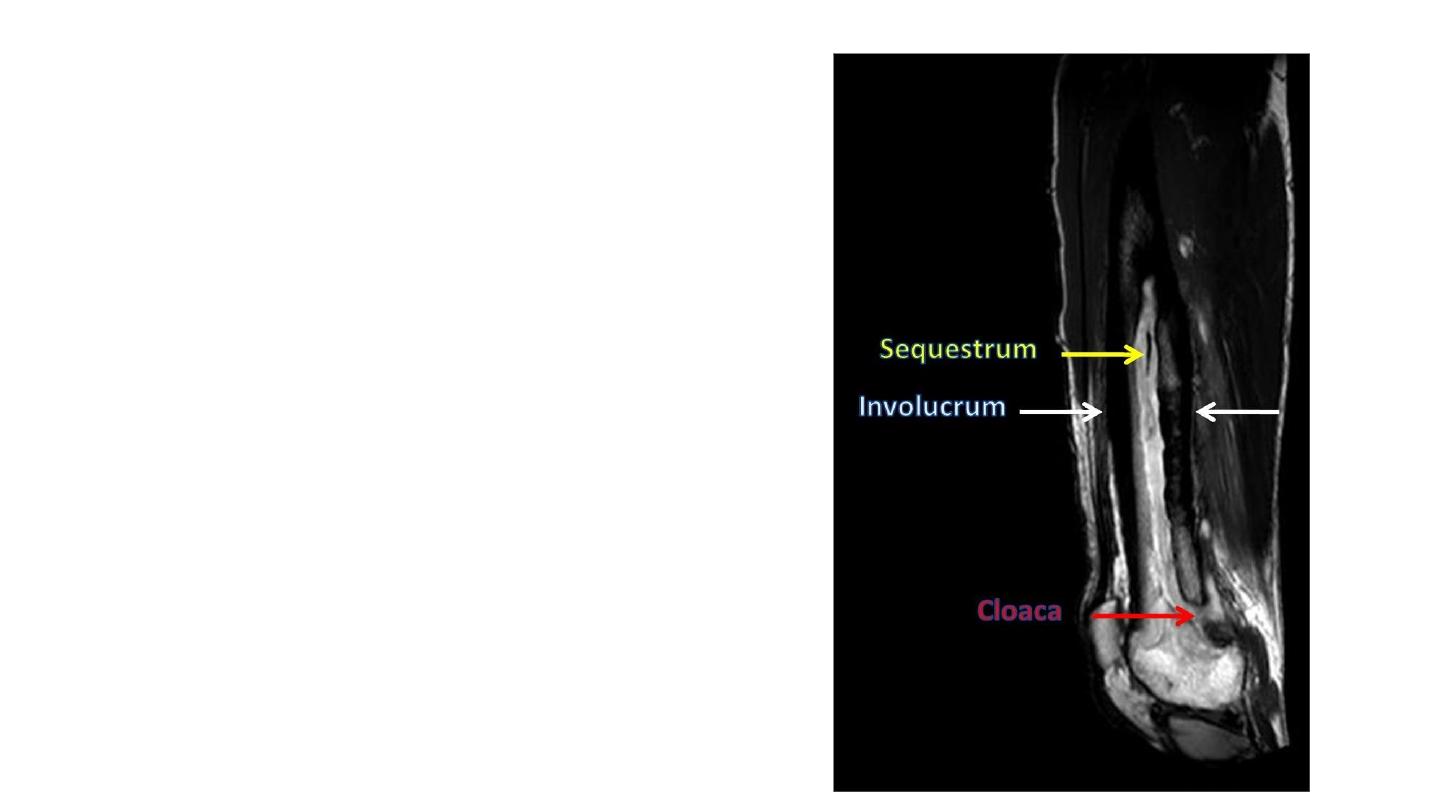
• If infection persists, pus
and tiny sequestrated
spicules
of
bone may
continue to
discharge
through
perforations in
involucrum
(cloacae).

• TREATMENT
• 1. Remove the sequestrum
from Cavity
or
Saucerization
of
cavity
(Leaving the Cavity
open).
• 2. Identify
the organism and control
the infection
(most
important step).
• 3. Fill the gap in
Cavity
with Bone graft/Bone
cement
(Poly Methyl
MethAcrylate).

• 4. Provide
a
good soft tissue coverage—Local closure or
by Myoplasty or Composite graft of Bone, Muscle and skin.
Instillation-suction technique for
the treatment of
chronic
bone infection
is
described in
which
infected
bone is
first exposed
and all
sequestra
removed. Two drainage
tubes are inserted. One tube
is
connected to
a
drip containing antibiotic
solution
and the second
to
a
continuous
suction
pump.
Closed
continuous steady
flow
instillation-suction
is
established to
do
lavage
of
cavity.
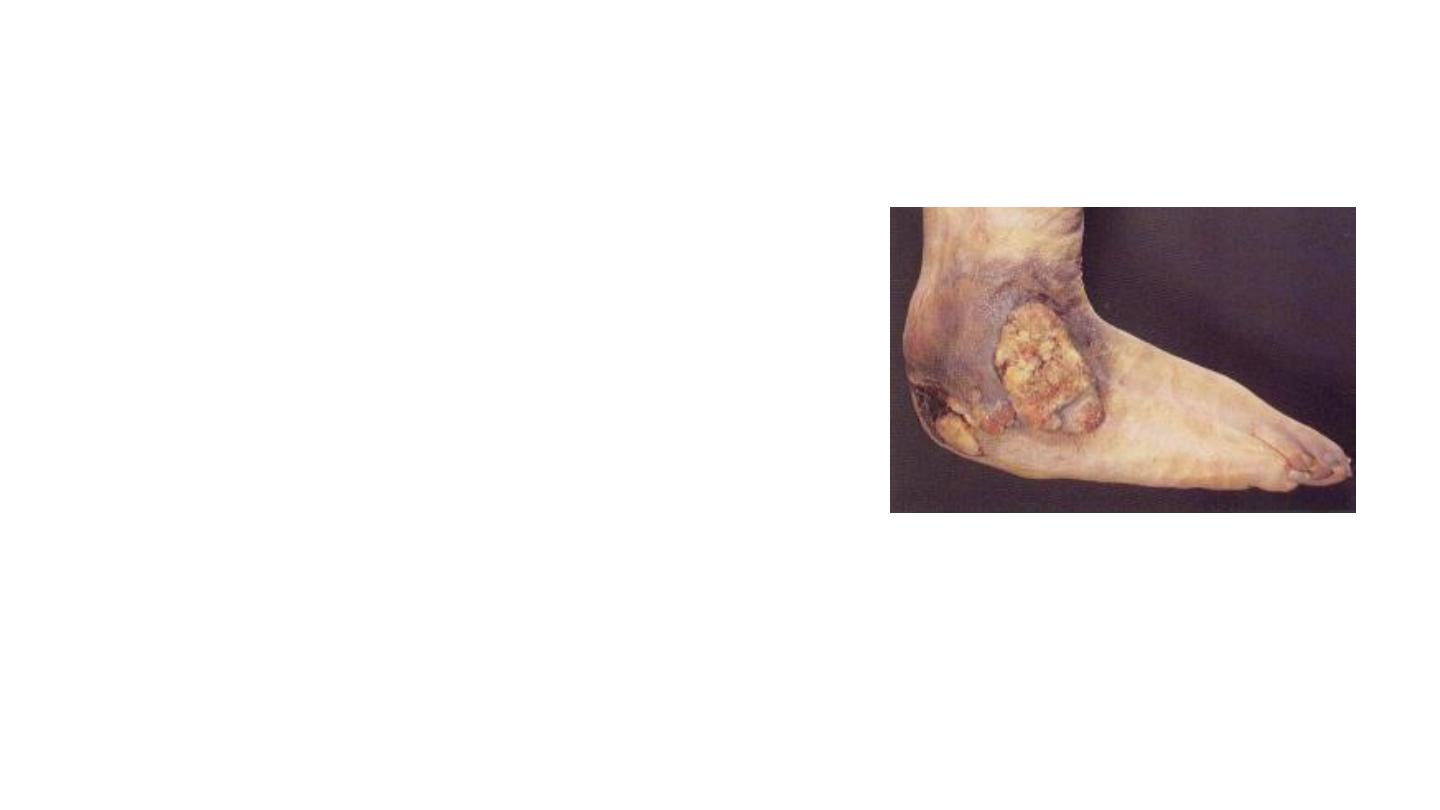
Complications of Chronic Osteomyelitis:
• i. Acute excacerbation
• ii. Growth
abnormalities
due to
damage
to
adjacent
growth
plate
• iii. Pathological fracture
• iv. Joint stiffness
• v. Sinus tract malignancy (very rare):
Squamous cell carcinoma
• vi. Amyloidosis
