
Septic Arthritis
• It occurs most commonly during the first 2 yr of life and
adolescence.
• Half of all cases occur by 2 yr and three fourths occur by 5 yr .
• Joints of the lower extremity constitute three fourth of all cases.
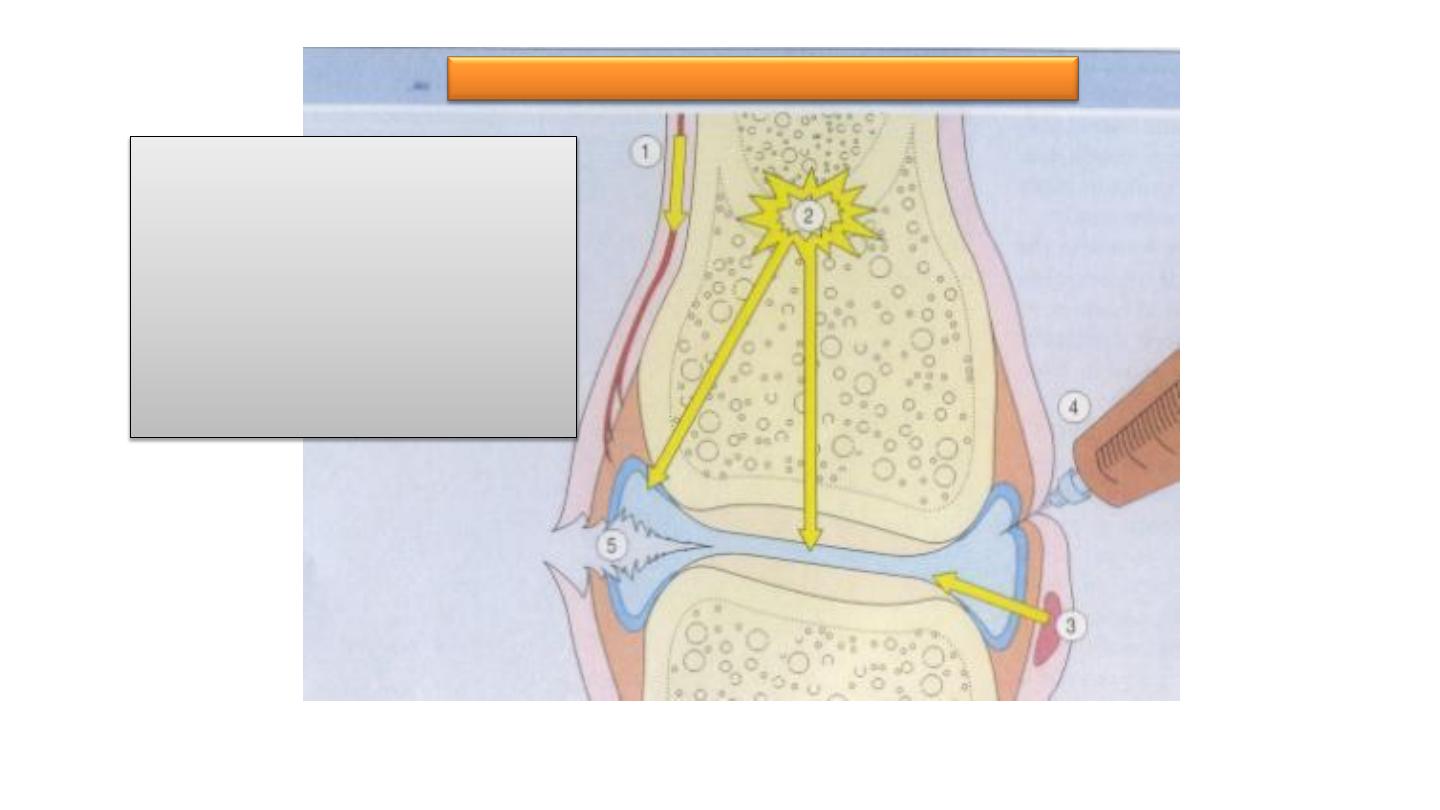
1.
Hematogenous
2.
Contiguous spread from
osteomyelitis
3.
Contiguous spread from
a soft tissue abscess
4.
Iatrogenic
5.
Traumatic
Routes of infection:

etiology
• S.aureus is the most common agent.
• H.influ type b is the most common factor in 3 month to -4 yr .
• Streptococci , pneumococci, meningococci that may occure in
the absence of sepsis or meningitis.
• Gonococcal arthritis most common cause of polyartheritis and
monoarticular artheritis in adolecent.

Clinical manifestation( con)
• Often difficult to assess septic arthritis of the hip and may cause
referred pain the knee .
• The hip for minimize pain from pressure ,The limb may be
positioned in external rotation and flexion .
• The knee and elbow joints usually are in flexion .

•
Infectious arthritis must be rapidly diagnosed and treated
promptly to prevent irreversible and permanent joint damage.
•

• Plain radiographs typically add little information to the physical
findings.
• Radiographs may show swelling
of the joint capsule, a widened joint space, and displacement
of adjacent normal fat lines.

• MRI is useful in distinguishing joint infections from cellulitis or
deep abscesses.

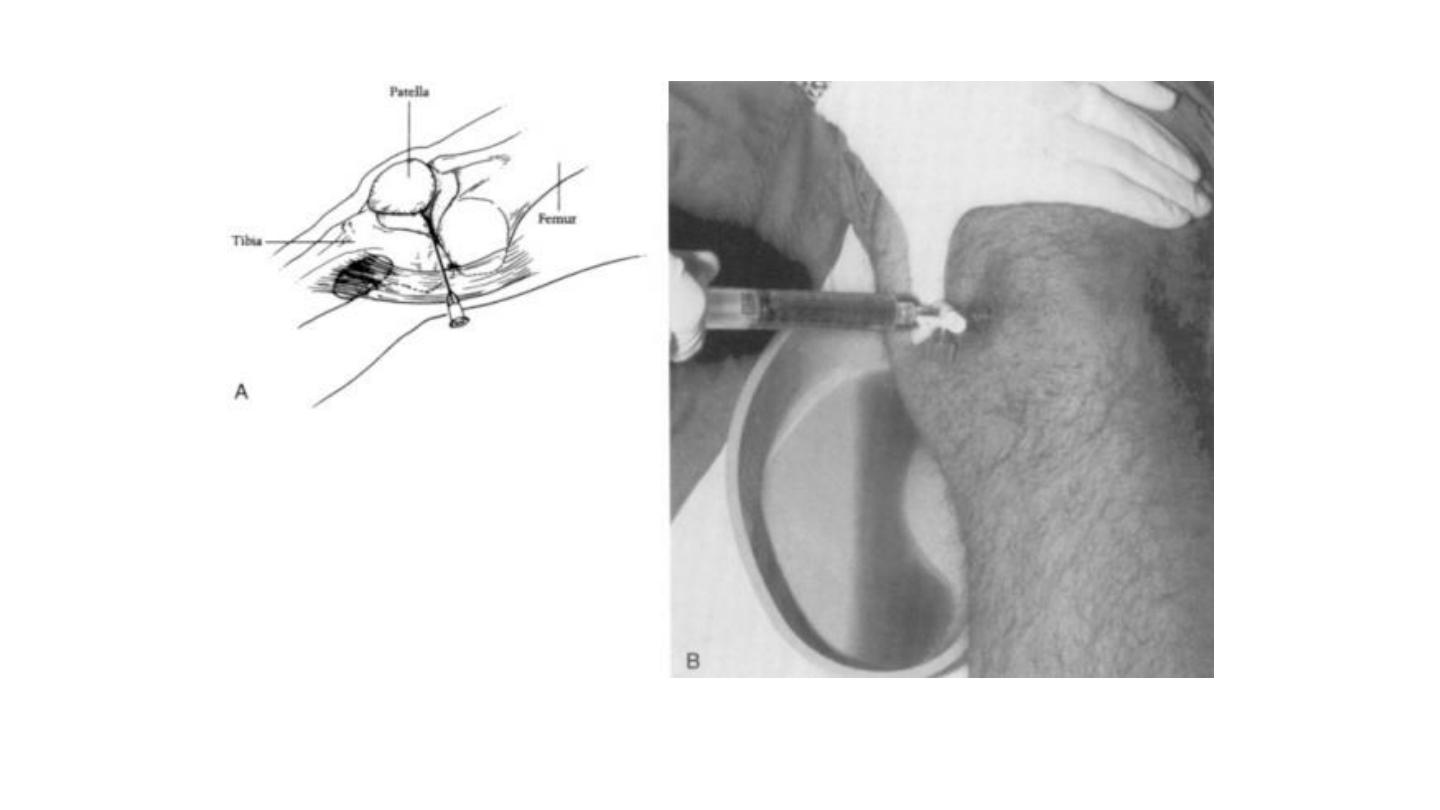
diagnosis
(Synovial fluid analysis)
• Synovial fluid analysis for
cell count, diff ,protein and glucose has
limited usefulness .
• Noninfection inflammatory disease can also increased cells and
protein and decreased glucose
(rheumatic fever , and rheumatoid arthritis)

diagnosis
• In up to 30% of patients who have never received antibiotic
may not reveal bacterial pathogens .
• In chronic arthritis synovial biopsy may distinguish between an
septic and a non infection process.
• Radiography or bone scans of adjacent bone .

Differential diagnosis
• Reactive arthritis is immune-mediated synovial inflammation thar follows a bacrerial
or viral infection
• Non infectious
(Rheumatoid arthritis , SLE,serum sickness , IBD)
• Henoch –schonlein purpura, leukemia ,metabolic diseases ,
foreign bodies , traumatic arthritis
• viral infections may cause arthritis

• Suppurative arthritis must be distinguished from
Lyme disease, osteomyelitis, suppurative bursitis,
fasciitis, myositis, cellulitis, and soft tissue
abscesses.
• Psoas muscle abscess often presents with fever and
pain on hip flexion and rotation

Complication
• Septic arthritis can lead to ankylosis and even fatal septicemia.
• However, prompt antibiotic therapy and joint aspiration or
drainage cures most patients.

Tuberculous osteomyelitis
Incidence
• First cases evident in 5,000-year-old Egyptian mummies
• Spinal TB described by Percival Pott in 1779
• Spinal involvement in < 1% of patients with TB
• Spinal TB accounts for 50% of skeletal TB
• Thoracolumbar junction most common site
• Neurologic complications occur in 10–43%

Tuberculous osteomyelitis
Routes of entry;
1. Usually blood borne and originate from a focus of active
visceral disease.
2. Direct extension (e.g. from a pulmonary focus into a rib or
from tracheobronchial nodes into adjacent vertebrae) or
spread via draining lymphatics.
Tuberculous osteomyelitis
• The most common sites of skeletal involvement are:
– thoracic and lumber vertebrae followed by the knees and
hips
• Pott’s disease is the involvement of spine
In patients with AIDS frequently multifocal
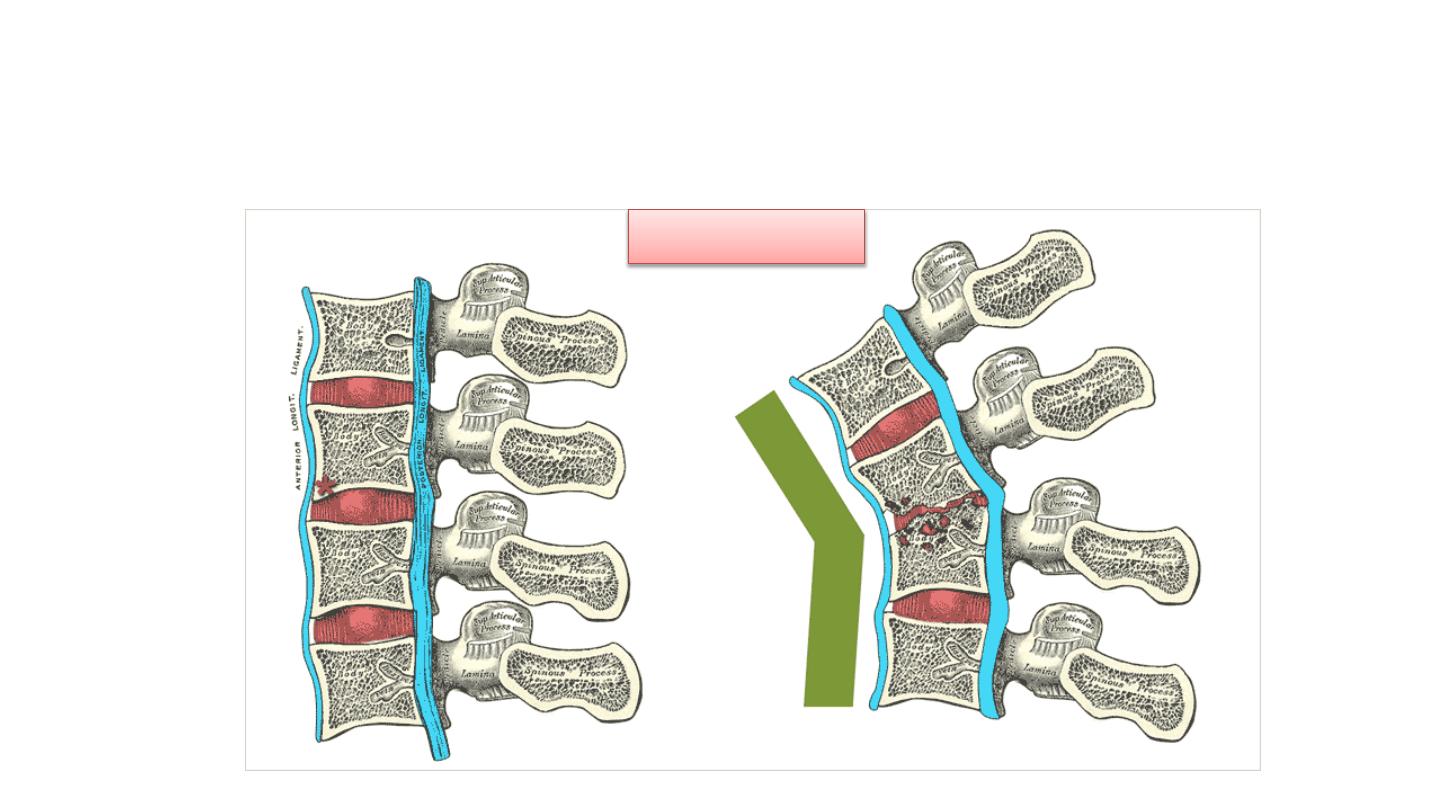
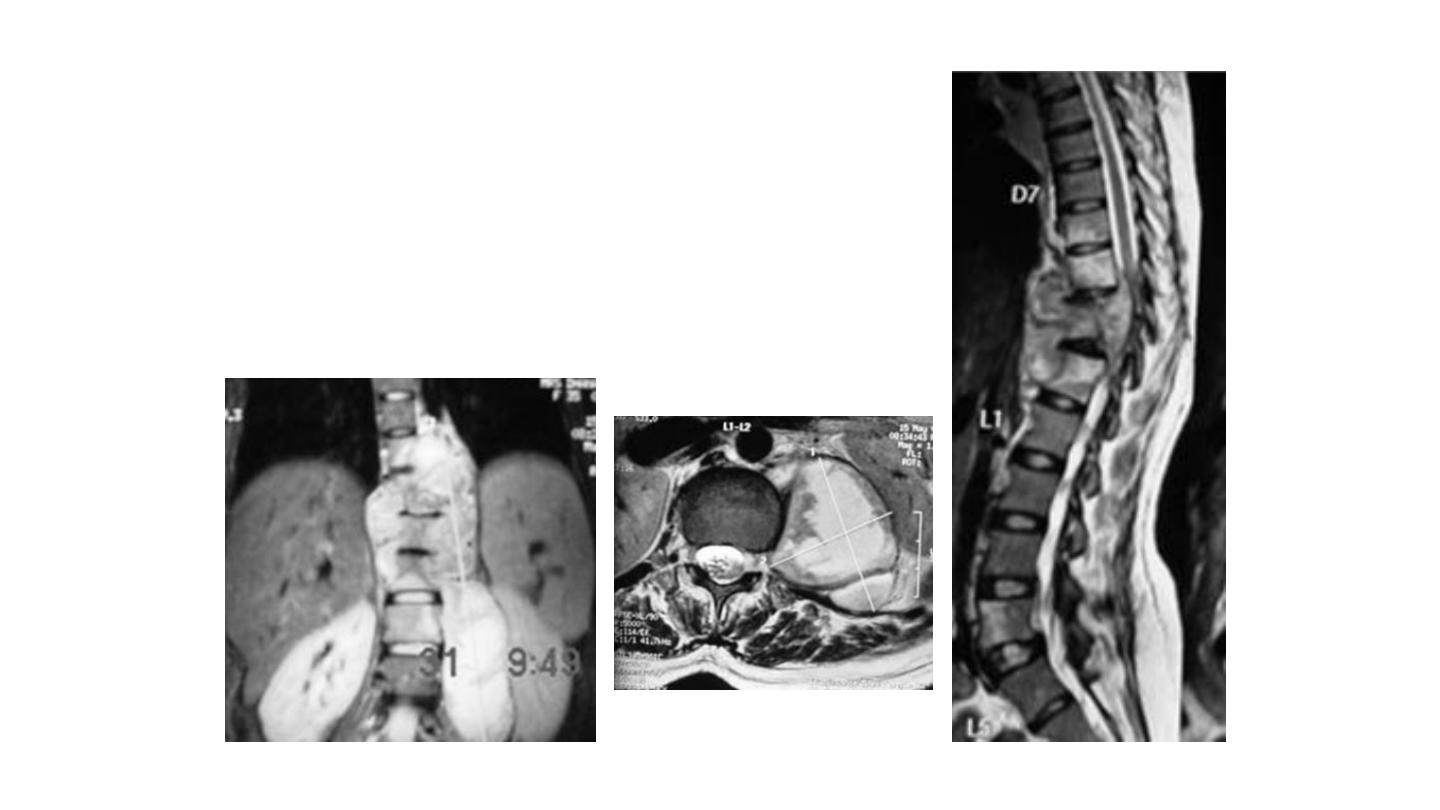
• The infection breaks through the
intervertebral discs and extends into the
soft tissues forming abscesses.
Pott’s disease
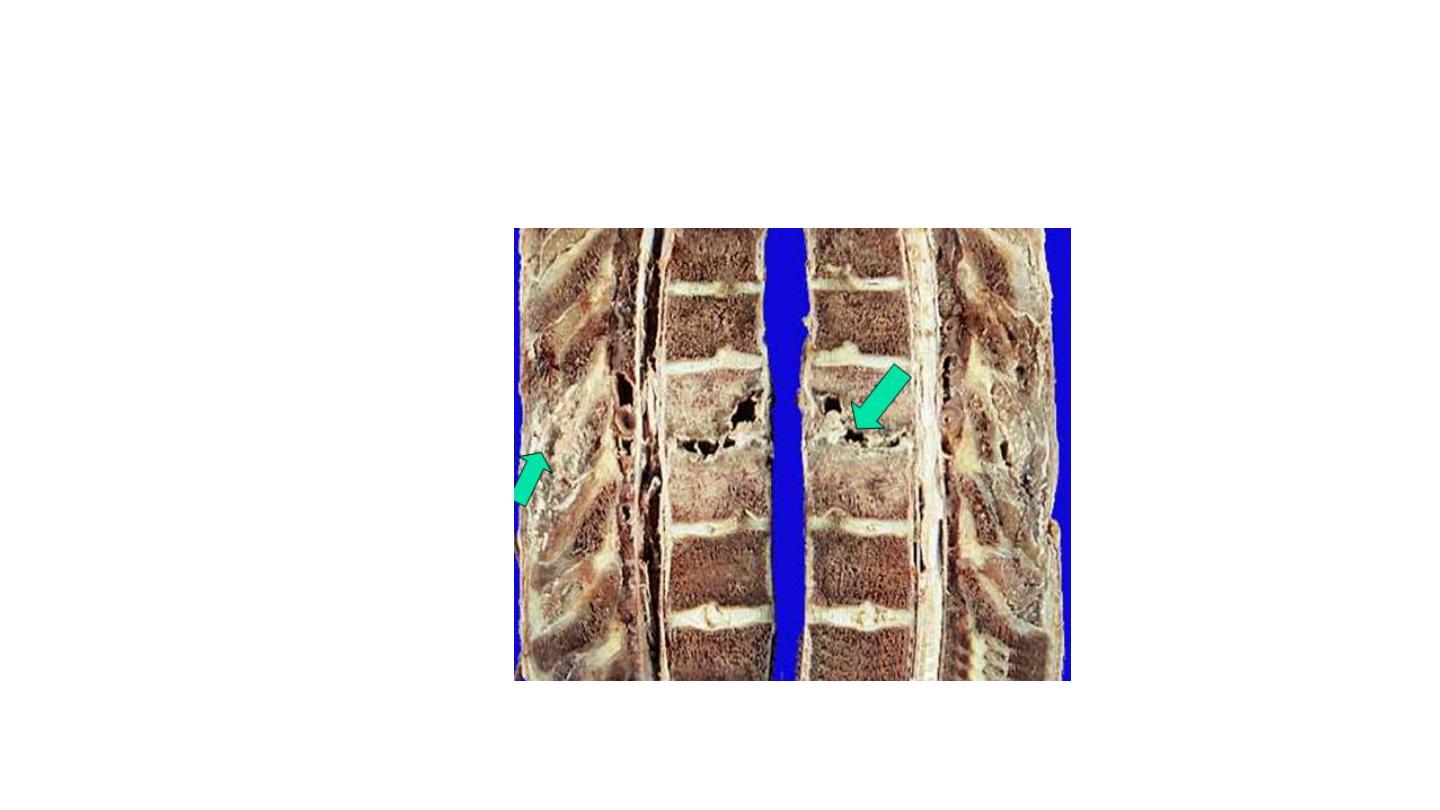
Tuberculous osteomyelitis
Pott’s disease
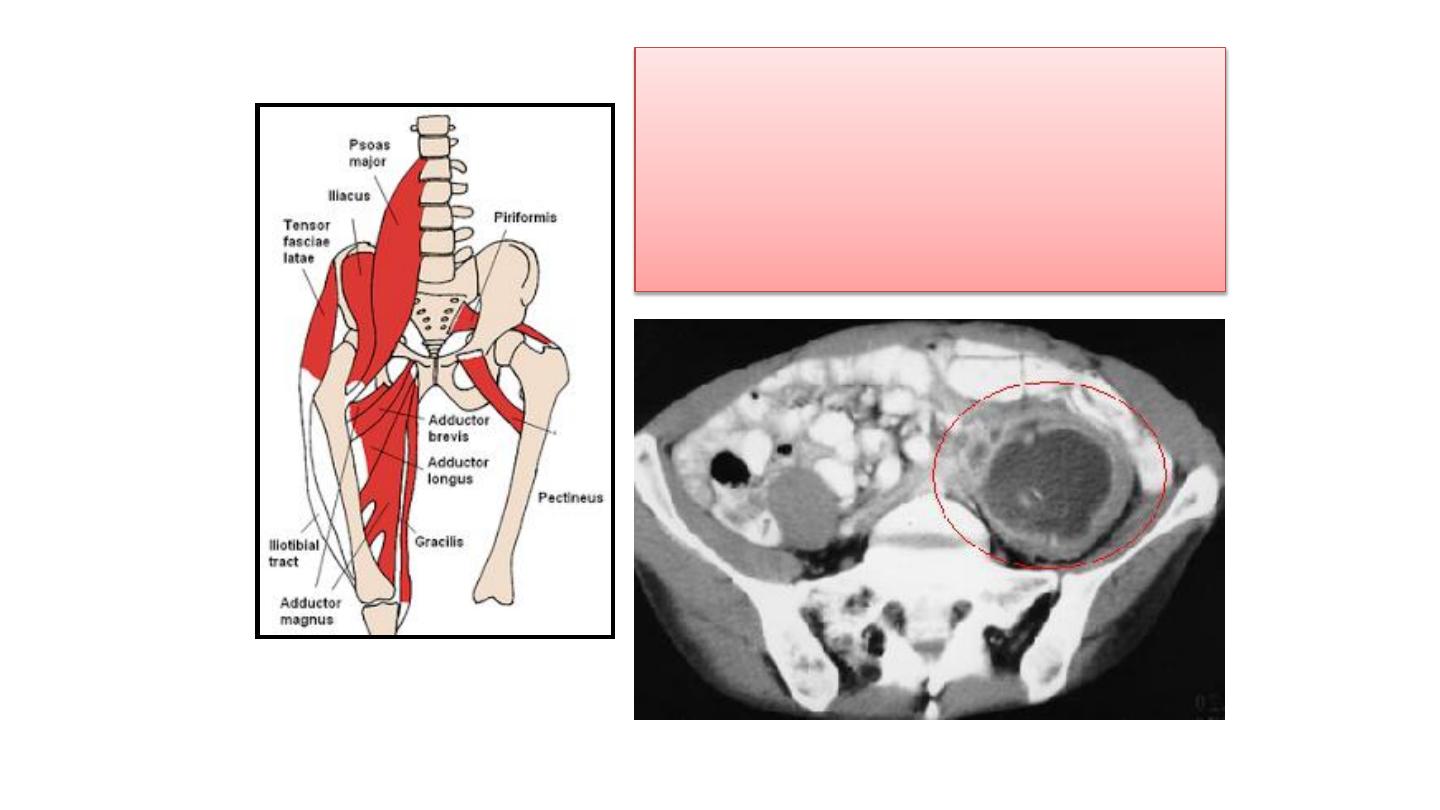
In Pott’s disease, the infection may
breaks through the intervertebral
discs and extends into the muscle
forming
Psoas abscesses
Tuberculous osteomyelitis
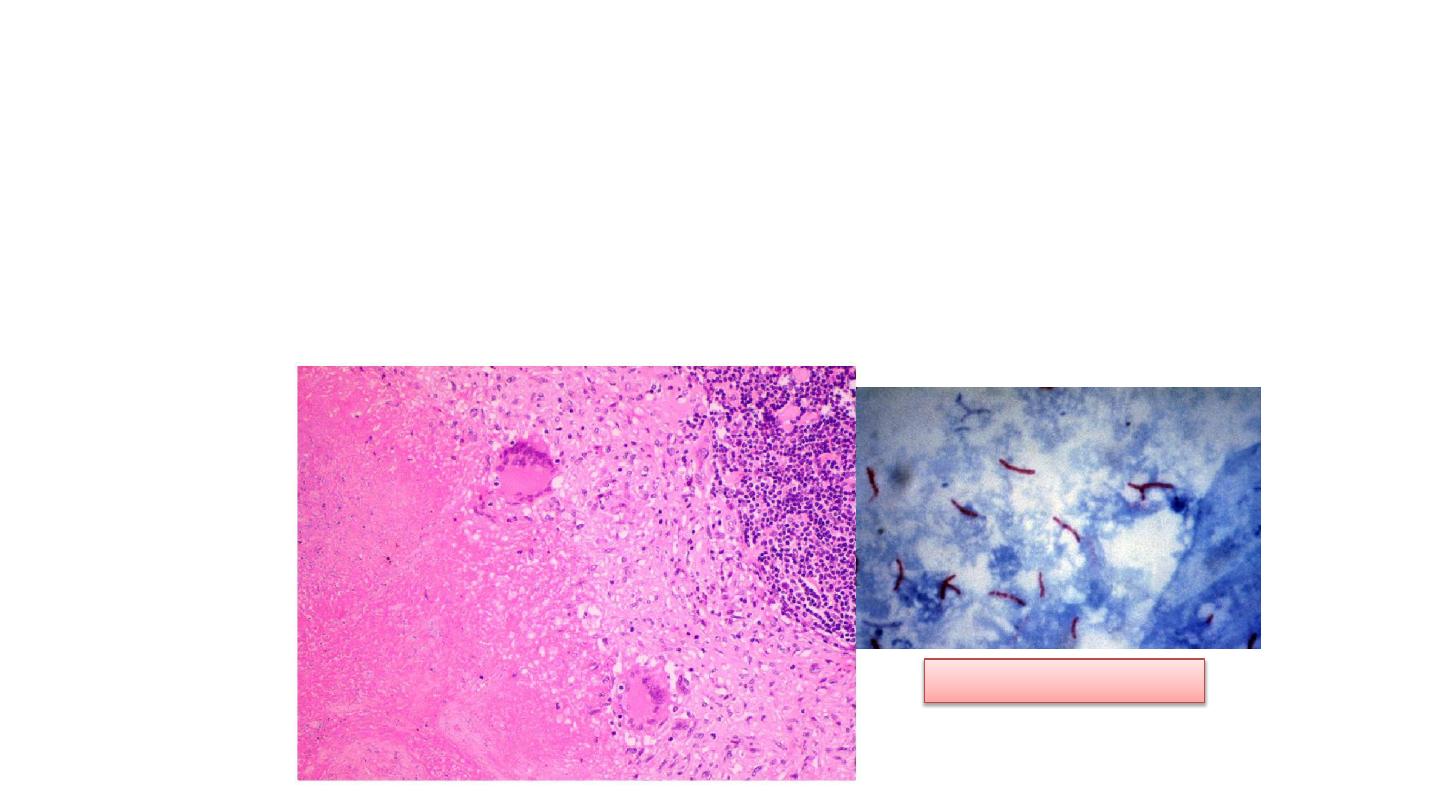
• Histopathology: collections of epithelioid histiocytes and
lymphocytes with caseation necrosis
Ziehl Neelsen stain
Tuberculous osteomyelitis
Clinical features :
• Pain especially at night
• Fever
• Weight loss
• May form an inguinal mass “ psoas abscess”.
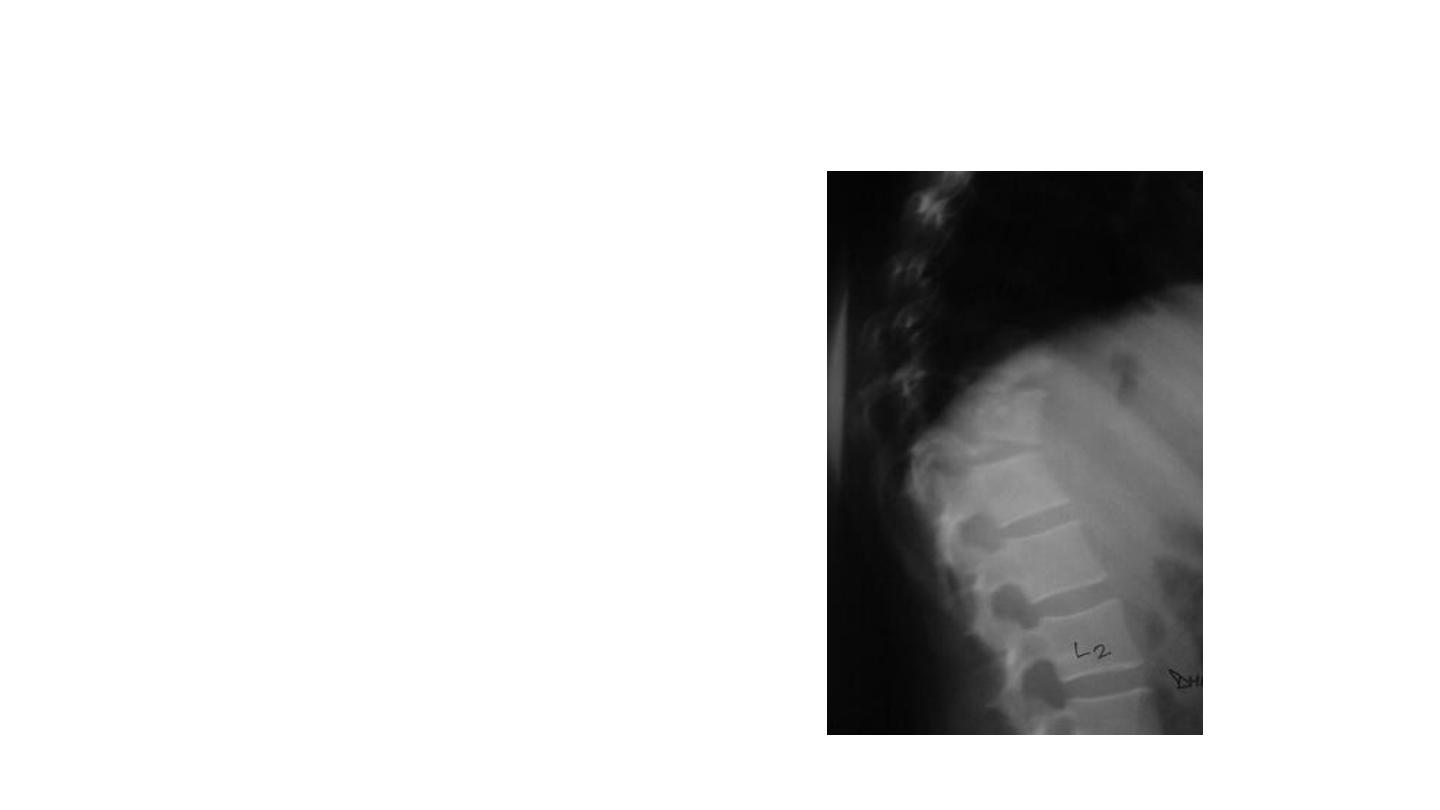
Radiographic assessment
Radiographic assessment
MRI – Investigation of choice
– Reveals the extent of vertebral involvement
as well as soft tissue and abscess formation

Treatment
• Medical management of spinal TB remains the mainstay of
treatment, either in isolation or as an adjunct to surgical treatment
• Combination treatment with;
– Rifampicin
– Isoniazid
– Ethambutol
– Pyrazinamide
• Generally all 4 of these drugs for 2 months, then rifampicin and
isoniazid for a total of 6–18 months
• Where surgery is undertaken, the duration of chemotherapy is
usually limited to 6–9 months

Treatment
• ESR and CRP are reliable parameters to assess response to
treatment
• Medical therapy usually undertaken in conjunction with bracing of
the affected spinal region
• Surgical intervention indicated for
• 1. neurologic involvement,
• 2. instability
• 3.to correct deformity
• 4.Surgery also indicated to obtain adequate tissue samples if
percutaneous biopsy fails to reveal the causative organism
Tuberculous osteomyelitis
Complications
• Bone destruction
• Tuberculous arthritis
• Sinus tract formation
• Amyloidosis

The End
