
Classification of bone tumours
Simple classification
A i. Primary
ii Secondary- more common
B i. Benign - osteoma
ii. Malignant - sarcoma

Primary Bone tumors are classified
according to the cell of origin
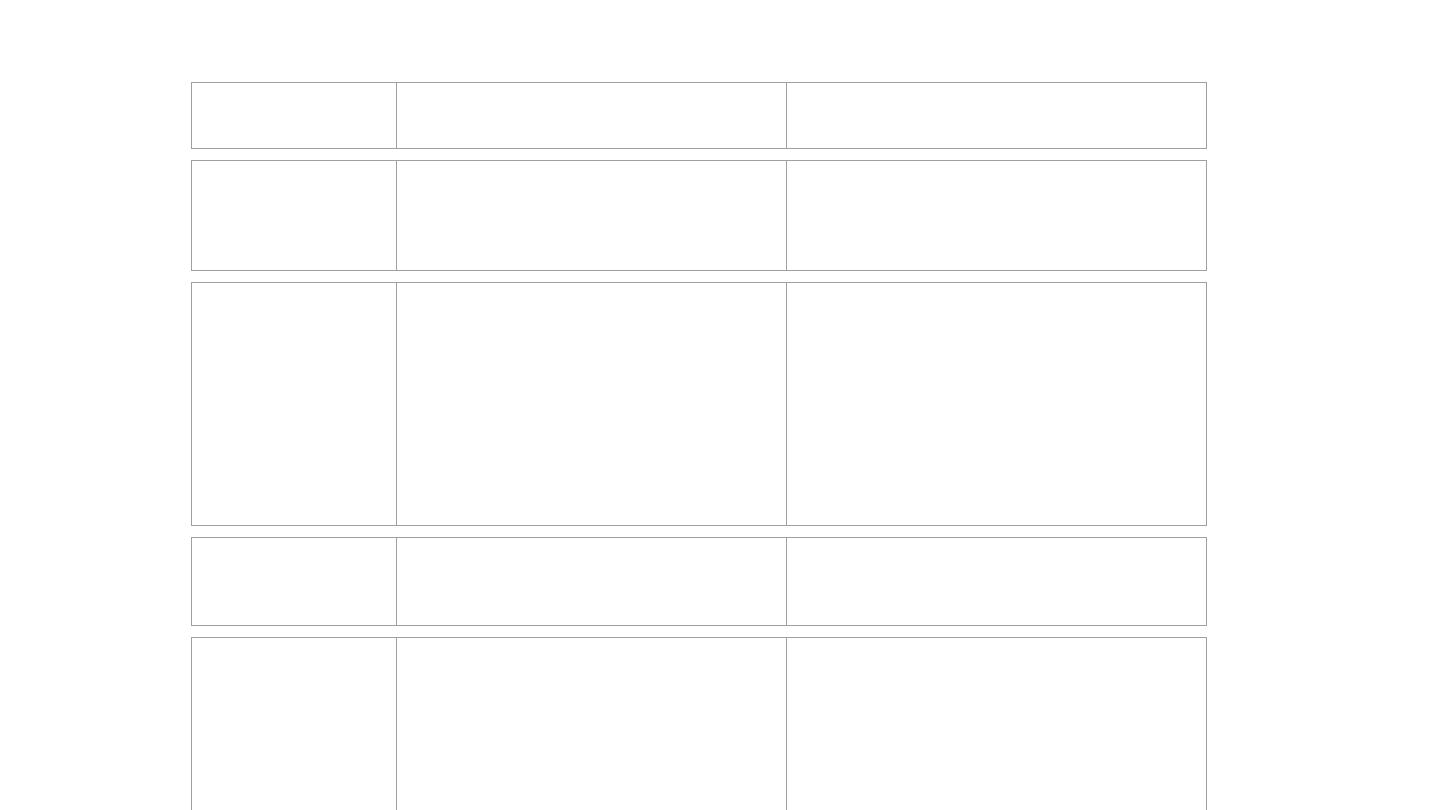
Histologic Type
Benign
Malignant
Hematopoietic (40%)
Myeloma
Malignant lymphoma
Chondrogenic (22%)
Osteochondroma
Chondrosarcoma
Chondroma
Dedifferentiated chondrosarcoma
Chondroblastoma
Mesenchymal chondrosarcoma
Chondromyxoid fibroma
Osteogenic (19%)
Osteoid osteoma
Osteosarcoma
Osteoblastoma
Unknown origin (10%)
Giant cell tumor
Ewing tumor
Giant cell tumor
Adamantinoma
Histiocytic origin
Fibrous histiocytoma
Malignant fibrous histiocytoma
Fibrogenic
Metaphyseal fibrous defect (fibroma)
Desmoplastic fibroma
Fibrosarcoma
Notochordal
Chordoma
Vascular
Hemangioma
Hemangioendothelioma
Hemangiopericytoma
Lipogenic
Lipoma
Liposarcoma
Neurogenic
Neurilemmoma

Diagnosis of Bone Tumours
1. Age of patient
2. Location of tumour
3. Radiological appearance
4. Histological features
AGE
(probably the most important clinical clue).
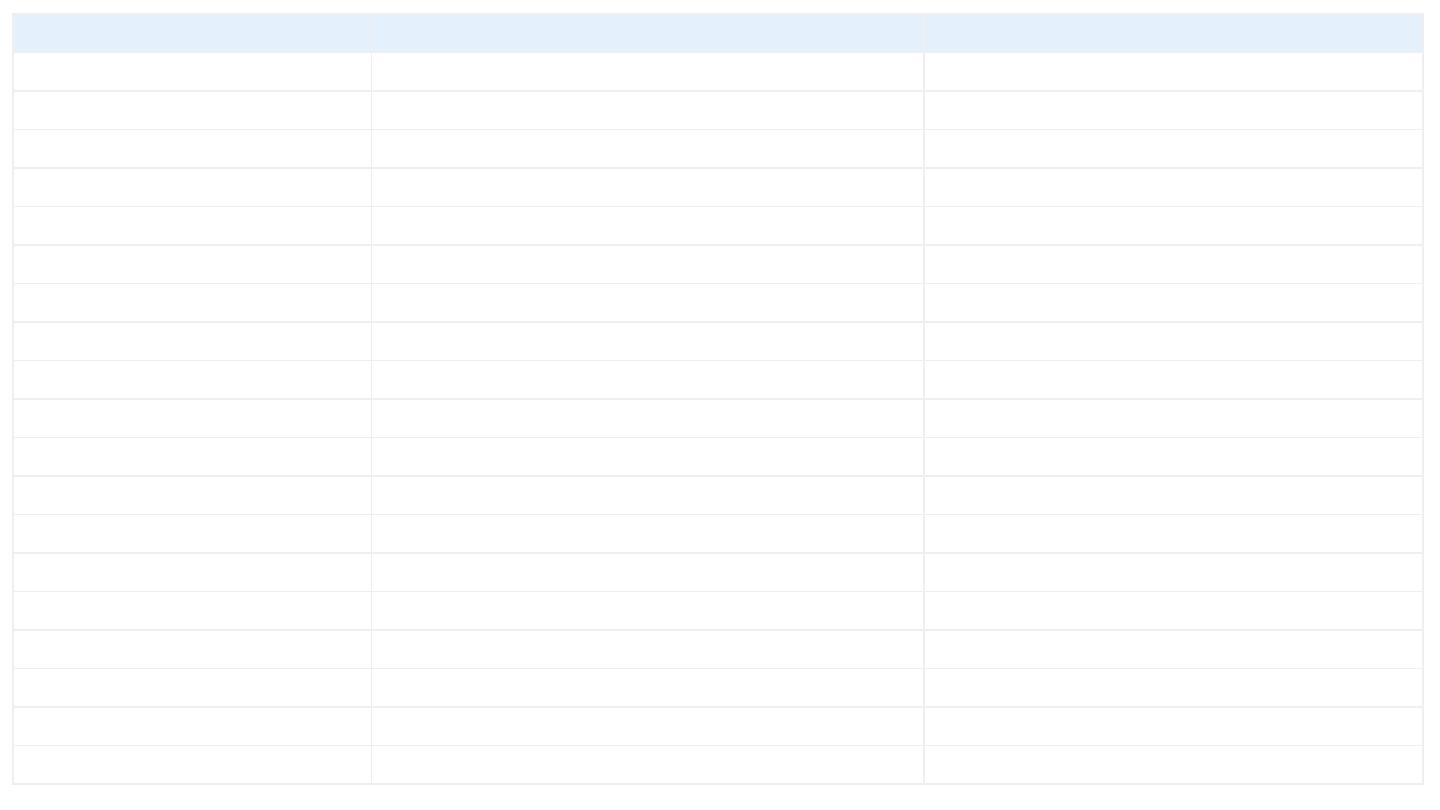
Age group
Most common benign lesions
Most common malignant tumors
0-20
non-ossifying fibroma
fibrous dysplasia
simple bone cyst
aneurysmal bone cyst
osteochondroma (exostosis)
osteoid osteoma
osteoblastoma
chondroblastoma
chondromyxoid fibroma
eosinophilic granuloma
Ewing's sarcoma
leukemic involvement
metastatic neuroblastoma
osteosarcoma,
Ewing's sarcoma,
21 - 40
enchondroma
giant cell tumor
chondrosarcoma
40 & above
osteoma
metastatic tumors
myeloma
leukemic involvement
chondrosarcoma
osteosarcoma (Paget's associated)
MFH
chordoma
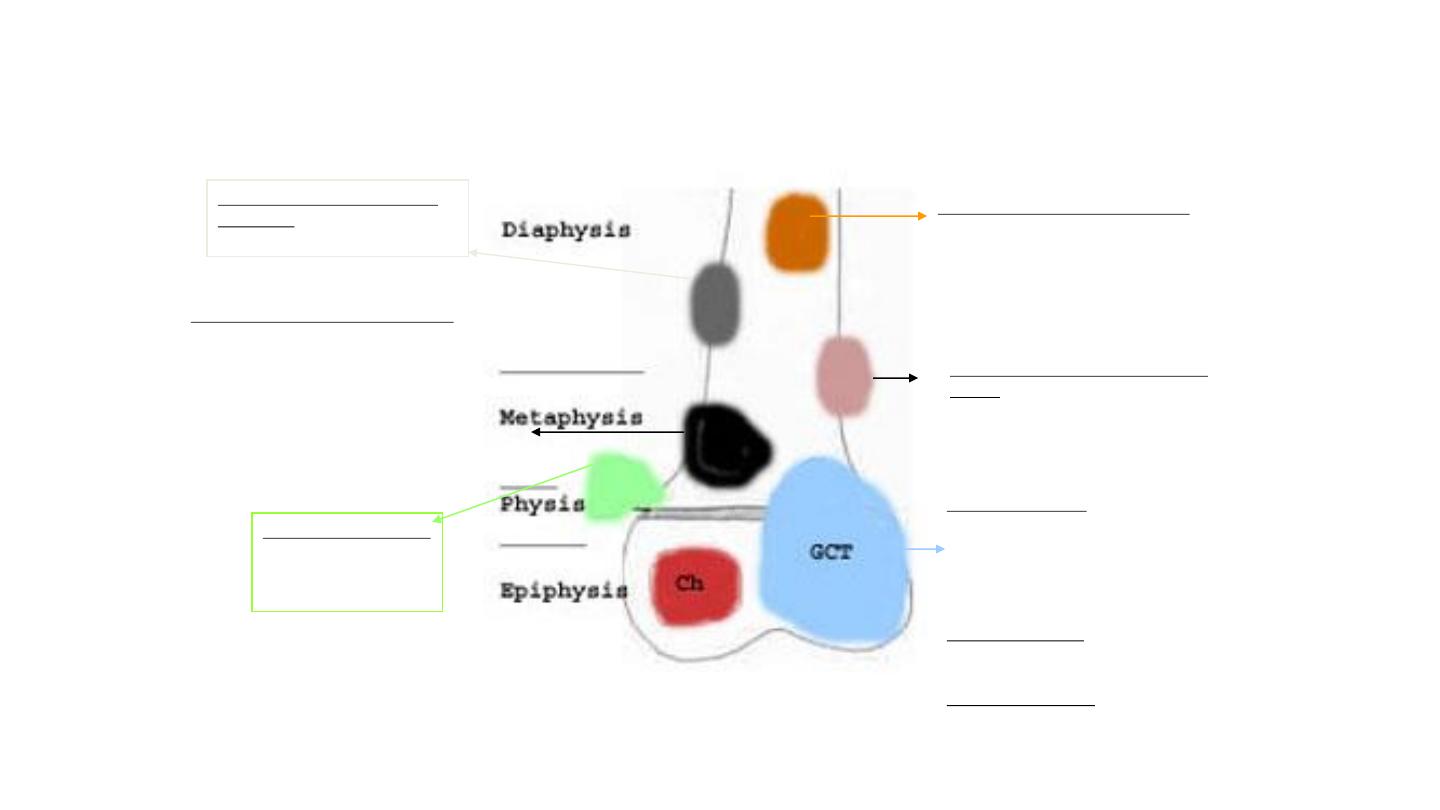
SITE OF LONG BONE INVOLVEMENT
(most primary bone tumors have favored sites within long bones; this may provide a clue to
diagnosis).
Diaphyseal intramedullary lesions:
Ewing's sarcoma, lymphoma, myeloma.
Common for fibrous dysplasia and
enchondroma
Metaphyseal lesions centered in the
cortex:
Classic location for a non-ossifying
fibroma (NOF). Also, a common site for
osteoid osteoma.
Epiphyseal lesions:
Chondroblastoma (Ch) and Giant
Cell Tumor (GCT) are almost
invariably centered in the epiphysis.
Chondroblastoma is a rare tumor
seen in children and adolescents with
open growth plates. GCT is the most
common tumor of epiphyses in
skeletally mature individuals with
closed growth plates. GCT often
shows metaphyseal extension.
Metaphyseal exostosis:
Osteochondroma
Metaphyseal intramedullary lesions:
Osteosarcoma is usually centered in the
metaphysis. Chondrosarcoma and
fibrosarcoma often present as metaphyseal
lesions. Osteoblastoma, enchondroma,
fibrous dysplasia, simple bone cyst, and
aneurysmal bone cyst are common in this
location.
Diaphyseal lesions centered in
the cortex:
Osteoid osteoma
Patients may be completely asymptomatic until the
.
1
ray.
-
is discovered on x
abnormality
Symptoms
•
2)bone pain. progressive and unremitting pain is a provoking
symptom. It may be caused by rapid expansion with stretching
of surrounding tissues, central haemorrhage or degeneration
in the tumour, or an incipient pathological fracture
The pain can be
severe (somewhat like a toothache), may occur at rest or at night and tends to progressively worsen.
• 3)
(pathologic fracture)
fracture with little or no stress
•
4)History of truma
whether the injury initiates a pathological
change or merely draws attention to what is already there
remains unanswered
5)Swelling
, or the appearance of a lump (painless lump), may be
alarming ,some patients seek advice only when a mass
becomes painful or continues to grow
6)Neurological
sign
, (paraesthesiae or numbness) may be caused by pressure upon or stretching of
a peripheral nerve.
Examination
If there is a lump, where does it arise? Is it discrete or ill-
defined? Is it soft or hard, or pulsatile? And is it tender?
Swelling is sometimes diffuse, and the overlying skin warm
and inflamed; it can be difficult to distinguish a tumour from
infection or a haematoma. If the tumour is near a joint there
may be an effusion and/or limitation of movement. Spinal
lesions, whether benign or malignant, often cause muscle
spasm and back stiffness, or a painful scoliosis
Imaging
x-ray
.
Different types of tumors have different characteristics on X-ray. Some B.Tu
cause an osteolytic lesion . Other cause an excessive osteoblast activity leading to
increase bone lay down i.e additional bone formation . Some can have a mixture of
these findings
.
X-ray
•
Clues by Appearance of Lesion
•
Clues by Location of Lesion
•
Clues by Density of Lesion
•
Other Clues
Clues by Appearance of Lesion
• Patterns of Bone Destruction
• Periosteal Reactions
• Tumor Matrix
• Expansile Lesions of Bone
Clues by Appearance of Lesion
• Patterns of Bone Destruction
– Geographic
– Moth-eaten
– Permeative

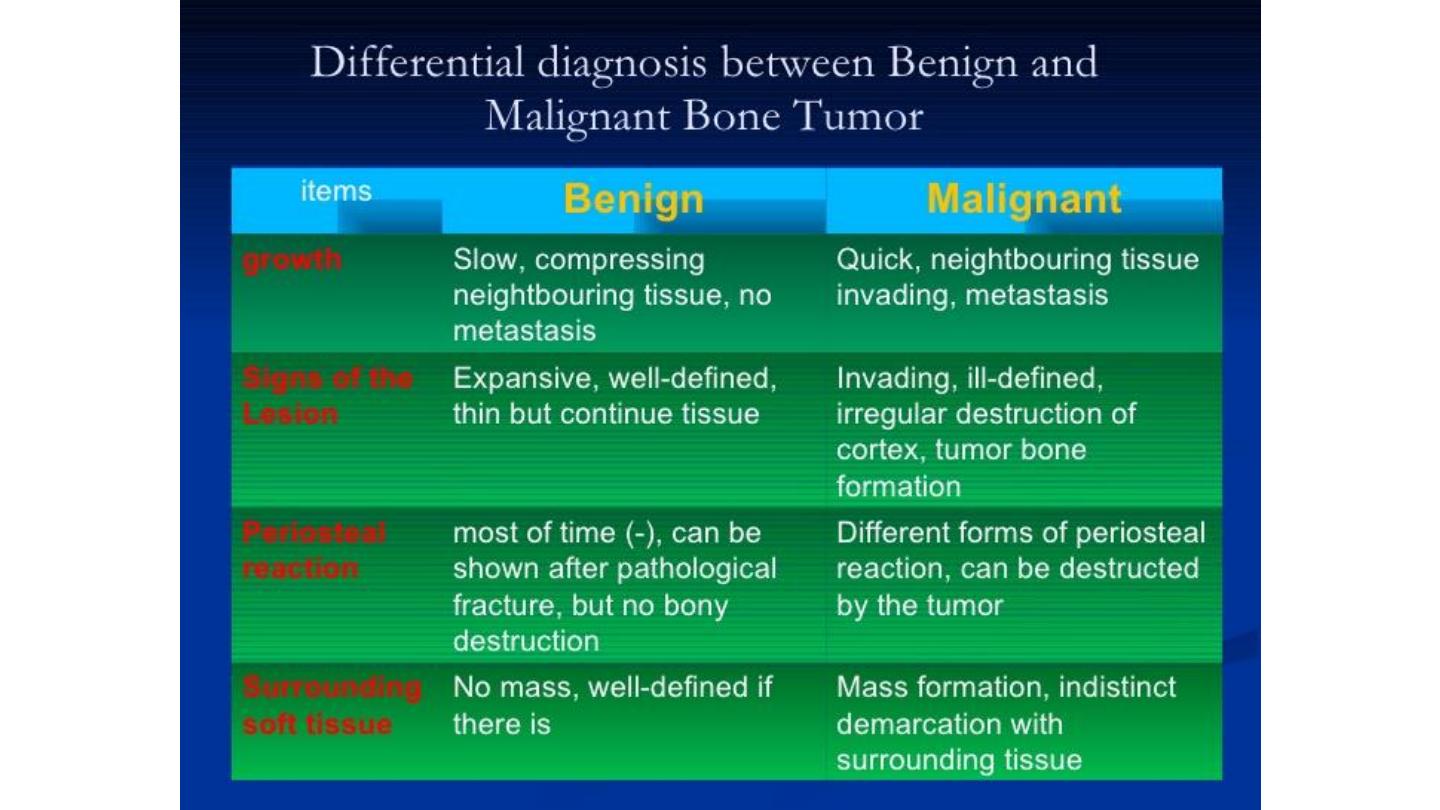
Geographic Bone Destruction
• Destructive lesion with sharply defined border
• Implies a less-aggressive, more slow-growing, benign process
• Narrow transition zone
Non-ossifying
fibroma

Moth-eaten Bone Destruction
• Areas of destruction with ragged borders
• Implies more rapid growth
• Probably a malignancy
Multiple Myeloma

Permeative Bone Destruction
• Ill-defined lesion with multiple “worm-holes”
• Spreads through marrow space
• Wide transition zone
• Implies an aggressive malignancy
• Round-cell lesions
Leukemia
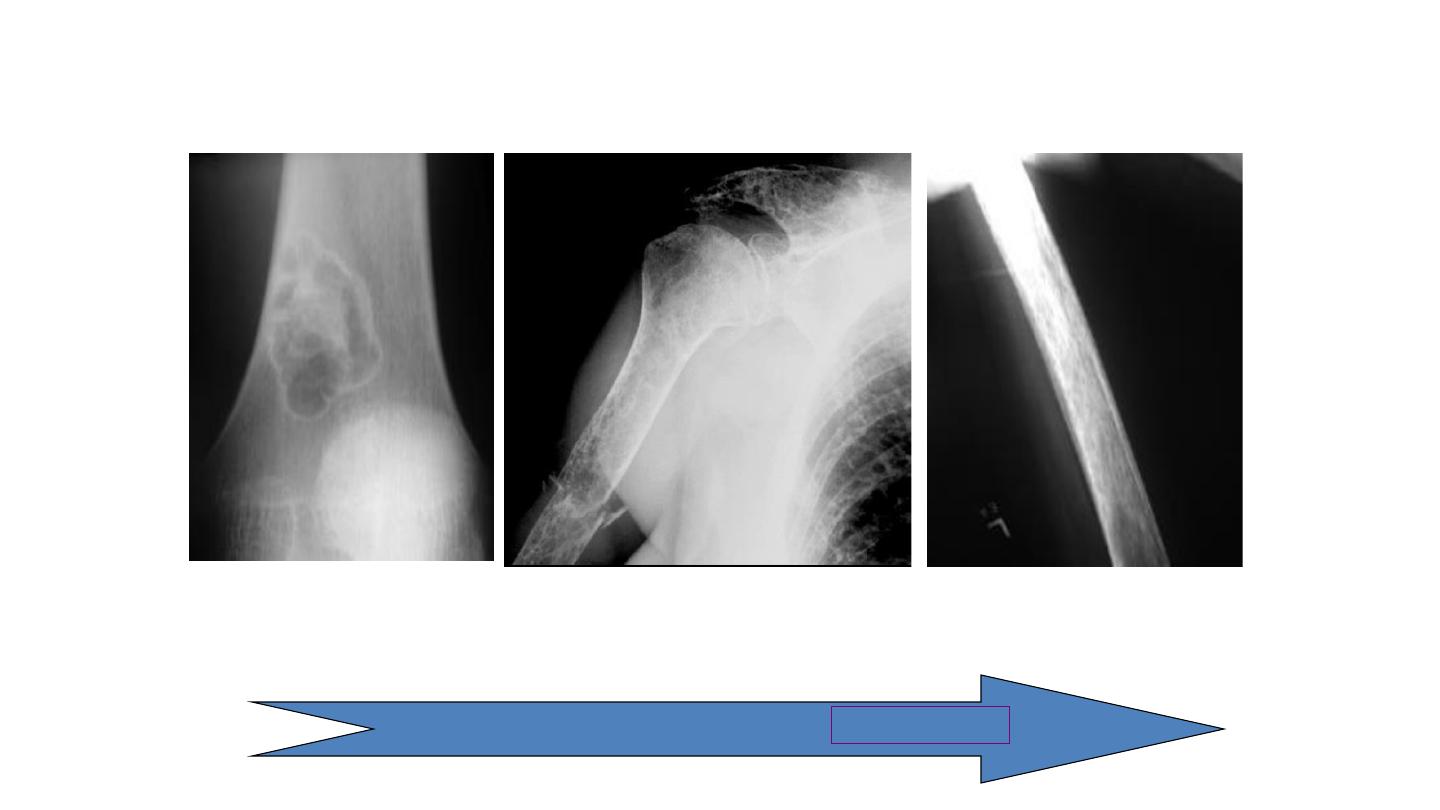
Patterns of Bone Destruction
Geographic
Moth-eaten
Permeative
Less malignant
More malignant
Periosteal Reactions
• Benign
– None
– Solid
• Aggressive/malignant
– onion-peel
– Sunburst
– Codman’s triangle
Non-ossifying fibroma

Periosteal Reactions
• Benign
– None
– Solid
• Aggressive/malignant
– onion-peel
– Sunburst
– Codman’s triangle
Chronic osteomyelitis
Periosteal Reactions
• Benign
– None
– Solid
• Aggressive/malignant
– onion-peel
– Sunburst
– Codman’s triangle
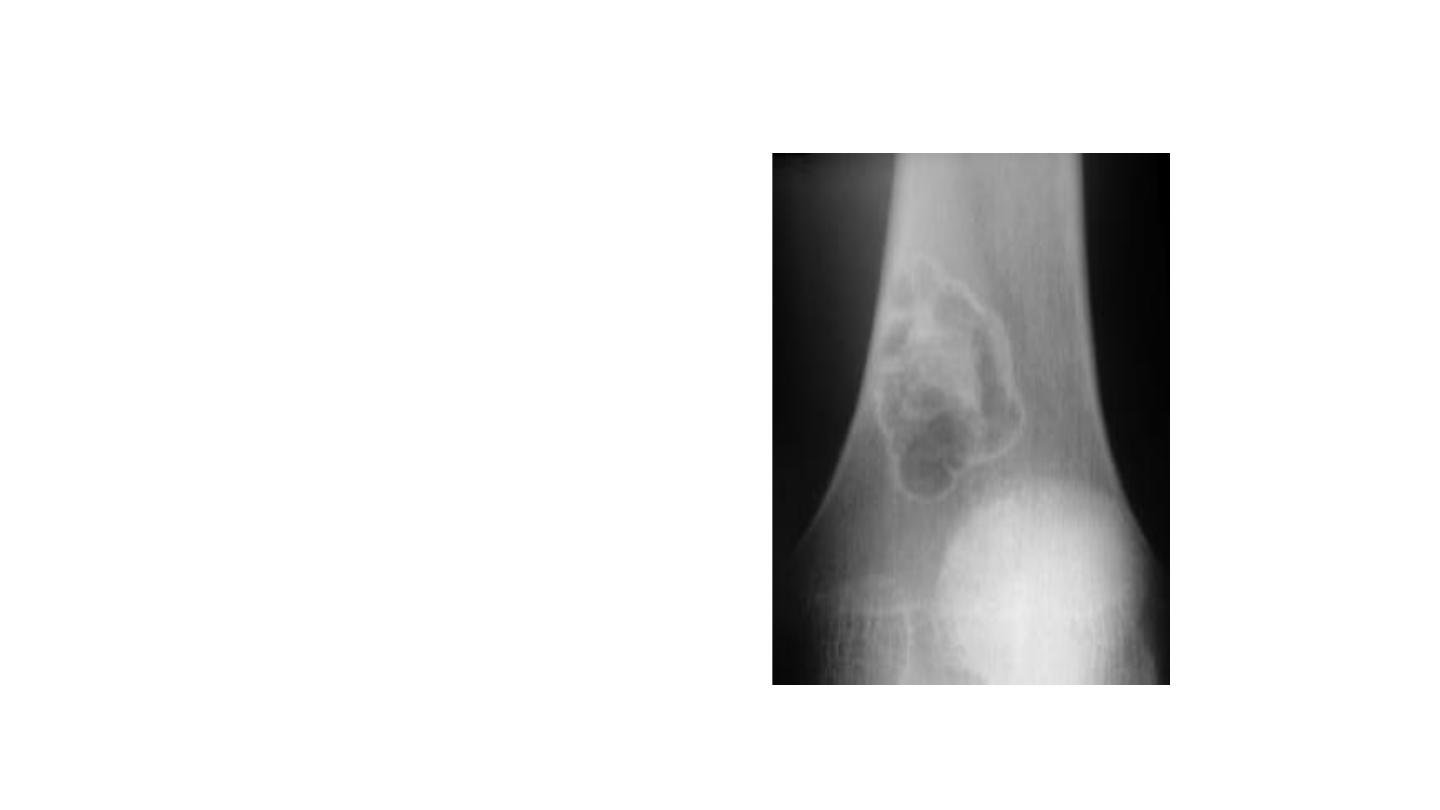
Ewing sarcoma
Periosteal Reactions
• Benign
– None
– Solid
• Aggressive/malignant
– onion-peel
– Sunburst
– Codman’s triangle
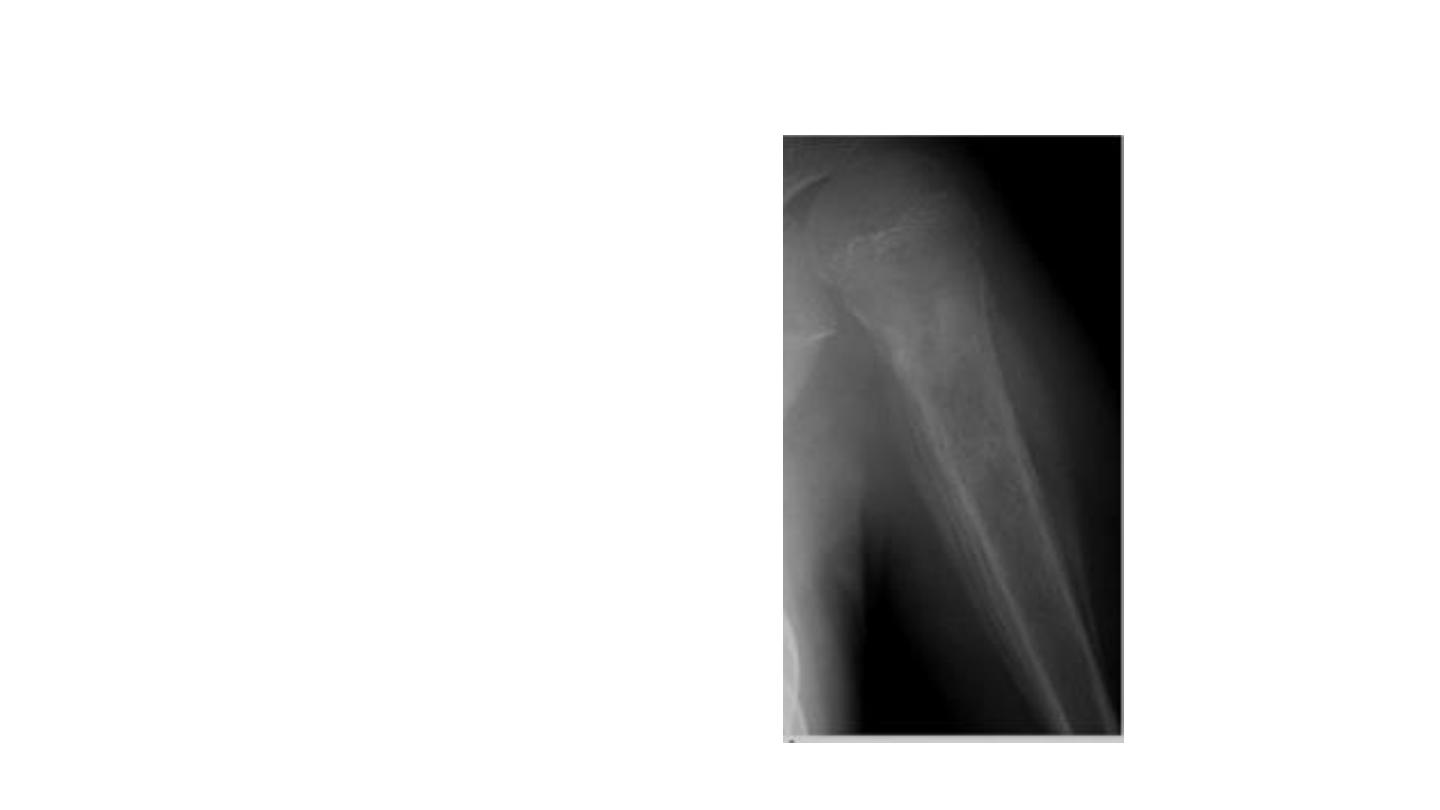
Osteo-sarcoma

Periosteal Reactions
• Benign
– None
– Solid
• Aggressive/malignant
– onion-peel
– Sunburst
– Codman’s triangle
Osteo-sarcoma
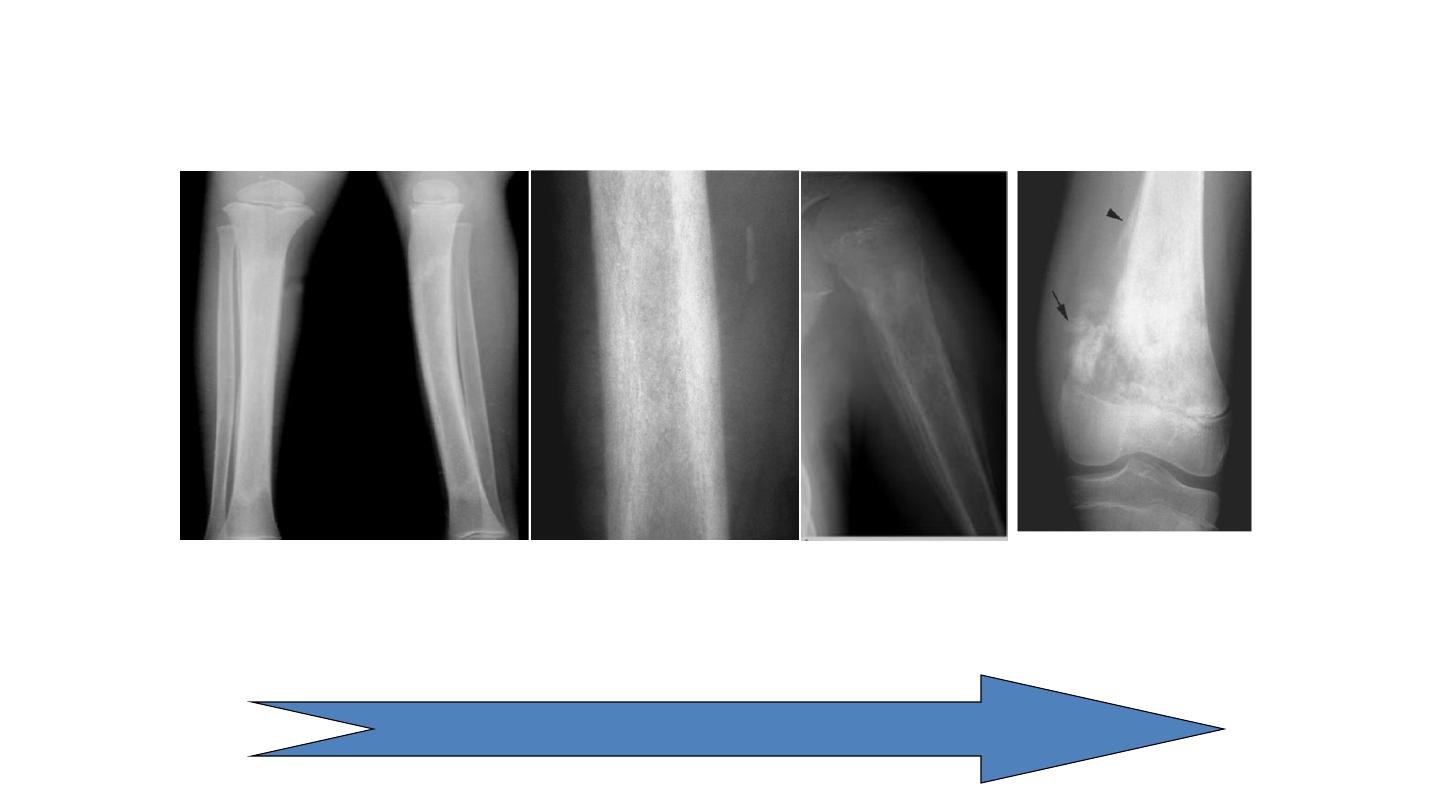
Periosteal Reactions
Solid
onion-peel
Sunburst
Codman’s
triangle
Less malignant
More malignant

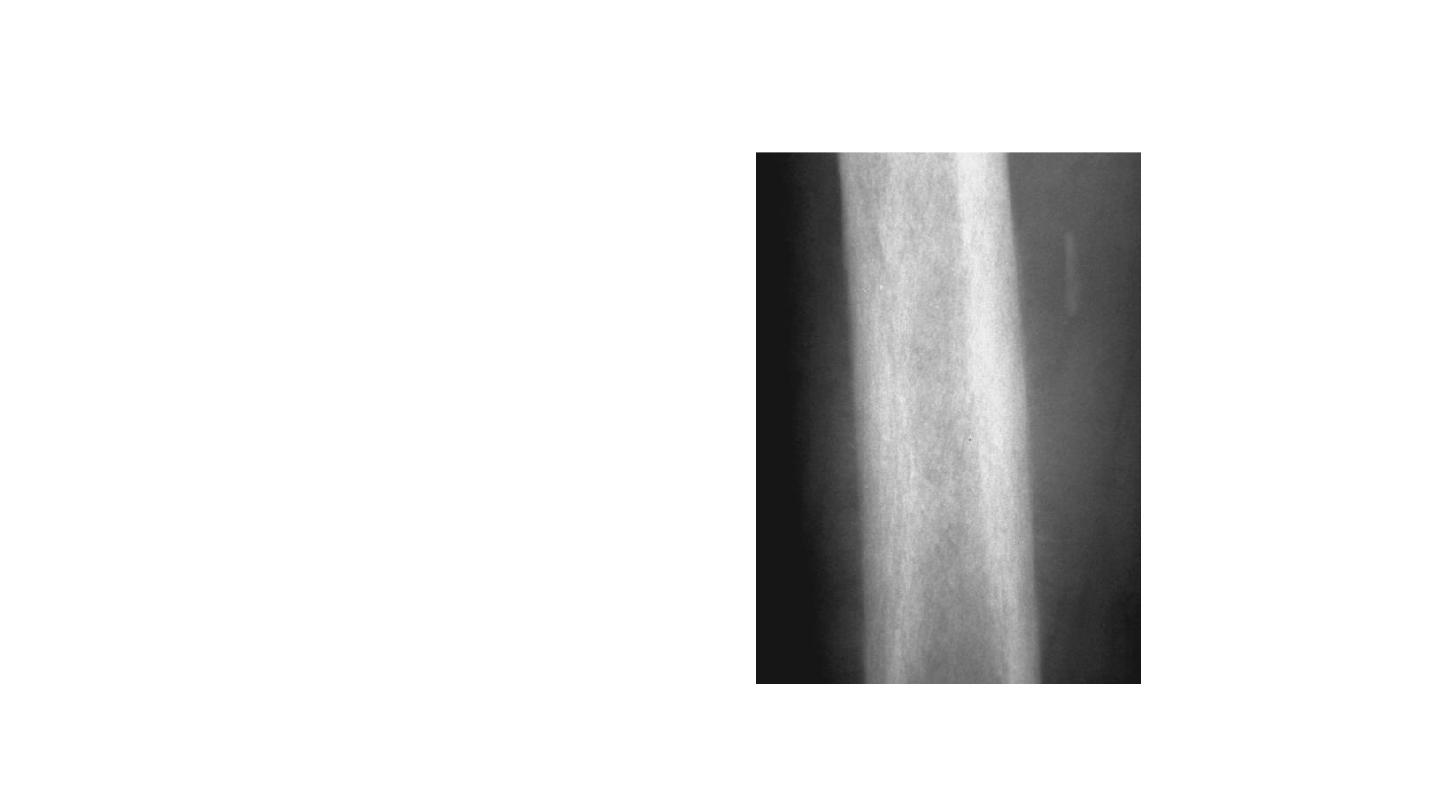
Tumor Matrix
• Osteoblastic
–Fluffy, cotton-like or cloud-like densities
–Osteosarcoma
• Cartilaginous
– Comma-shaped, punctate, annular, popcorn-like
– Enchondroma, chondrosarcoma, chondromyxoid
fibroma

Tumor Matrix
• Osteoblastic
– Fluffy, cotton-like or cloud-like densities
as Osteosarcoma
• Cartilaginous
– Comma-shaped, punctate, annular, popcorn-like
as Enchondroma, chondrosarcoma, chondromyxoid
fibroma
Chondrosarcoma
Clues by Density of Lesion
• Sclerotic Cortical Lesions
• Lytic Lesions in Children
• Lytic Lesions in Adults
• Blastic Lesions in Children
• Blastic Lesions in Adults
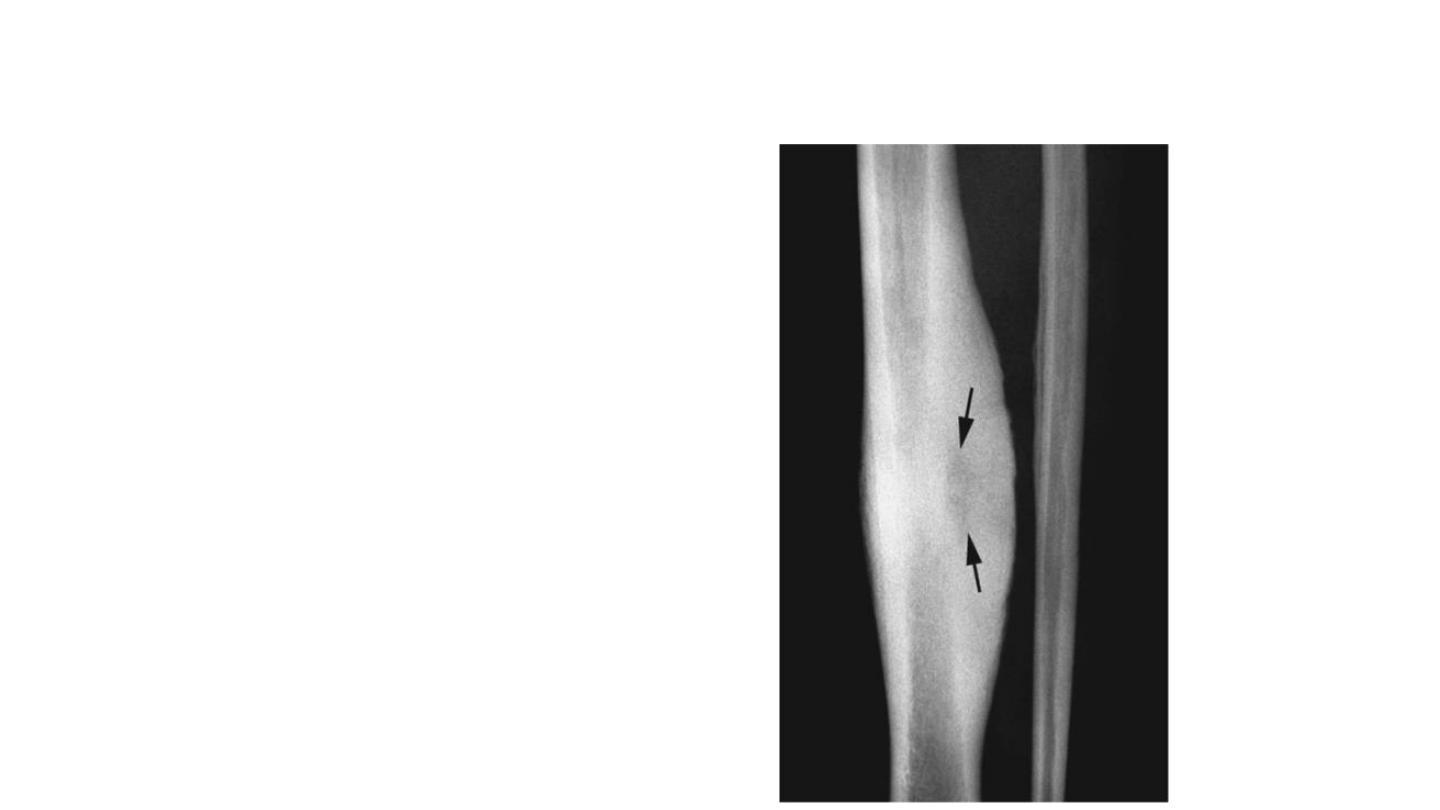
Sclerotic Cortical Lesions
• Osteoid
osteoma
• Brodie’s abscess

Blastic Lesions in Children
• Lymphoma

Blastic Lesions in Adults
• Metastatic disease
• Breast –female
• Prostate –male
Prostatic Ca.
–
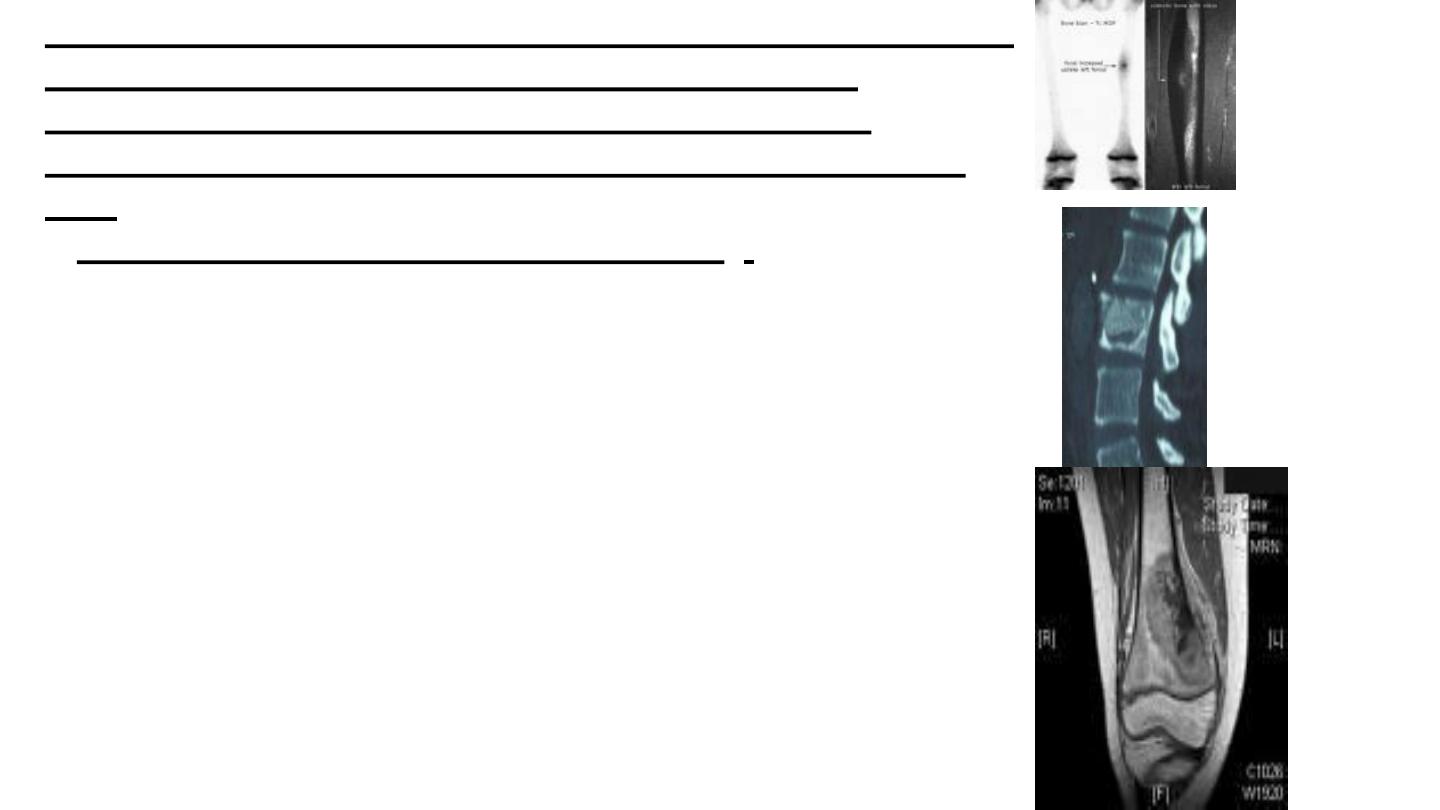
If other forms of imaging are planned (bone scans, CT or
MRI), they should be done before undertaking a
biopsy,which itself may distort the appearances.
Isotopis bone scaninig( TC99)
computed tomography
(CT)
(
magnetic resonance imaging) (MRI)
If an x-ray is not
conclusive, these will often help determine the exact location
and size of the tumor and give additional information as to
the nature of the tumor( bengin or aggressive ) ,,(intra. Or
extra compartmental),with involving of a near by
Neurovascular bundle ,or any skip lesion (2
nd
metastasis ),or
detecting expanding Tu. in (pelvis or spine) which is a
difficult places to reach ,
O
p
e
n
B
i
o
p
s
y

PET Scan
Lab.Tests
Blood
tests
,
Blood tests are often necessary to exclude other
conditions, e.g. infection or metabolic bone disorders, or a ‘brown tumour’
in hyperparathyroidism
. 1) complete blood pic
. Anaemia,
increased ESR and
2)elevated serum alkaline phosphatase
levels seen in pagets dis. Or osteoscrcoma
3
)
Serum protein
electrophoresis
may reveal an abnormal globulin fraction and the
urine may contain Bence Jones protein in patients with myeloma.
4)A raised serum acid phosphatase & PSA test suggests
prostatic carcinoma
5) Eleveted s.calcium in parathyroid tu.
Biopsy
a biopsy is usually necessary to confirm the
diagnosis.
Needle Biopsy
Often it is carried out with the help of
ultrasound or CT guidance. A large bore biopsy needle is
used,, biopsy is carried out in the line of any further surgical
incision so that the tract can be excised at the time of
definitive surgery
Open Biopsy either Excisional or Incisional
Points to be considered
1)
Biopsy taking from the boundries
…why ?.
2)
From the site were the next incision is to be done.
3)
Tourniqea remove. ,good heamostasis,drain
avoided
4)
Several samples
5) Complication
;
infection ,pathalogical
haemorrage.

Staging
•
Staging of malignant bone tumors (Enneking
)
– G (Grade) : G1 %10 > metastasis potency , G2 %20 < metastasis
potency
– T (Compartment) : intracompartmental (T1) or
extracompartmental (T2)
– M (Metastasis): Lymph nodule or far metastasis
IA
G1 T1 M0
IB
G1 T2 M0
IIA
G2 T1 M0
IIB
G2 T2 M0
IIIA G1-G2 T1 M1
IIIB G1-G2 T2 M1

Treatment
•
First of all, LIFE
!!
•
• Extremity preserving surgery
• Usable extremity
• Physical appearance of the body
• Psychological compliance
• Sociocultural compliance
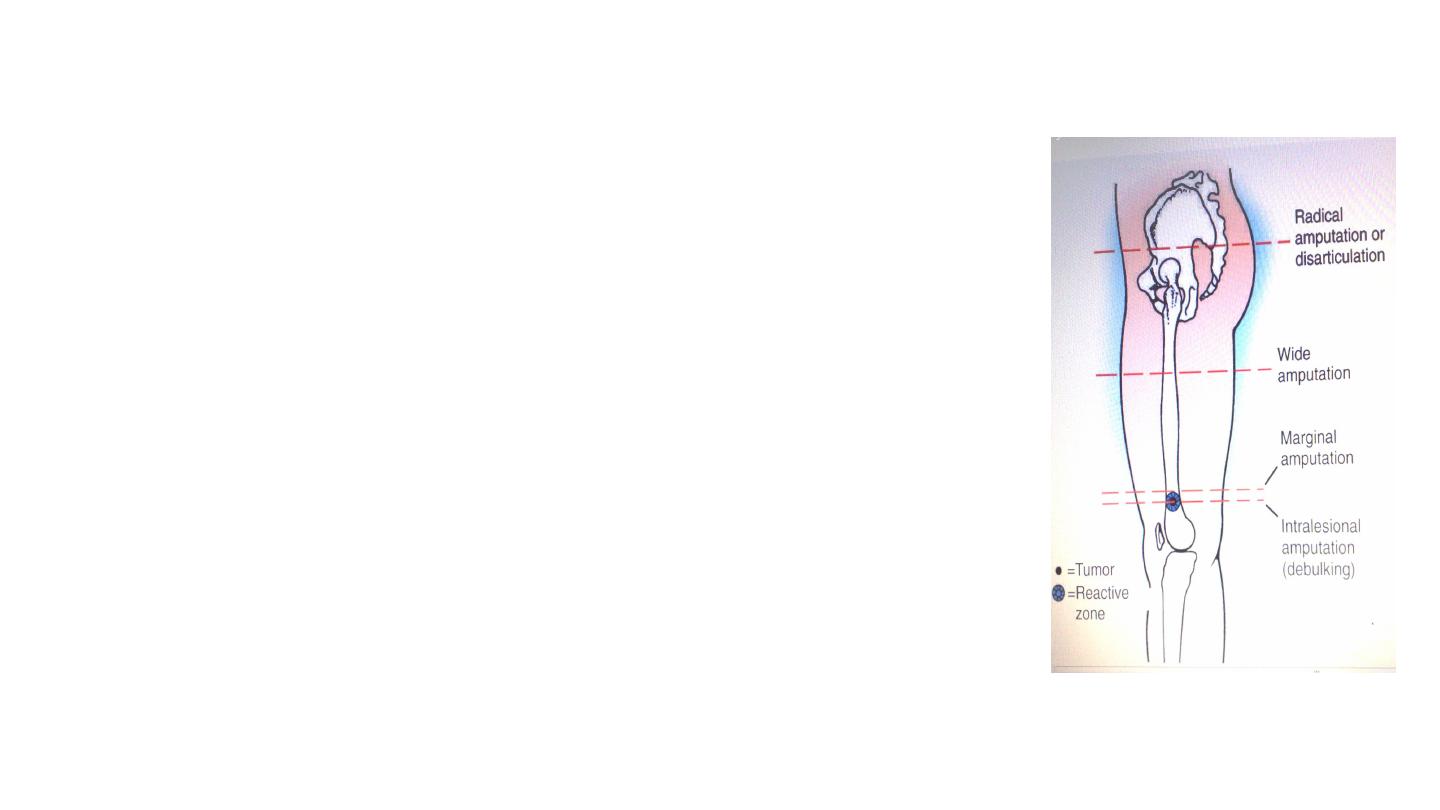
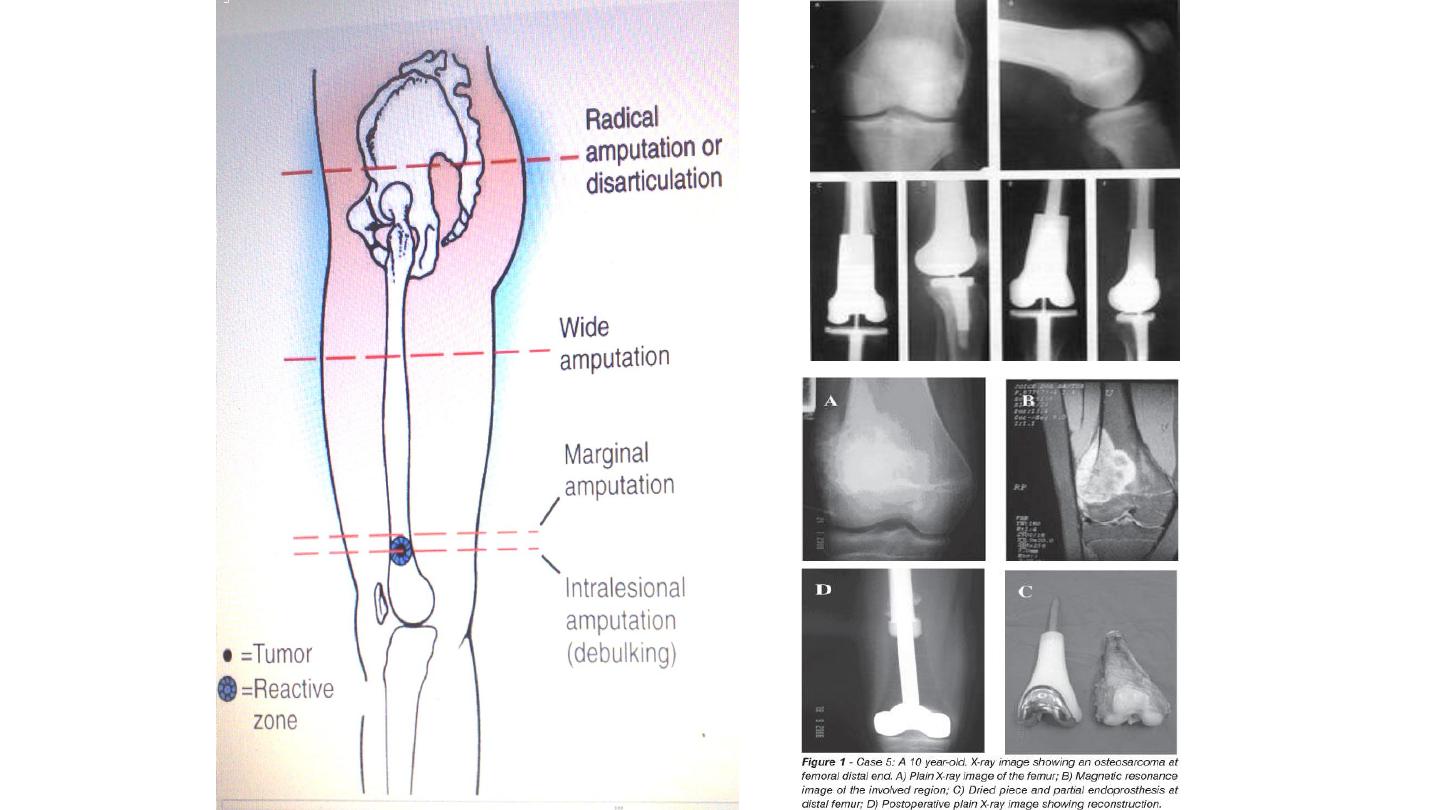
Surgical treatment
1.Intracapsular:
- Benign, latent lesions
2.Marginal excision:
- Excision of the lesion with reactive zone
- Benign, active lesions

Surgical treatment
3.Wide resection:
- Resection of the tumor with surrounding healthy-normal tissues
- Benign, aggressive lesions; malignant low grade lesions (with
adjuvant therapies)
4.Radical resection:
- Resection of the whole, entire compartment
- Malignant high grade lesions
5. Amputation
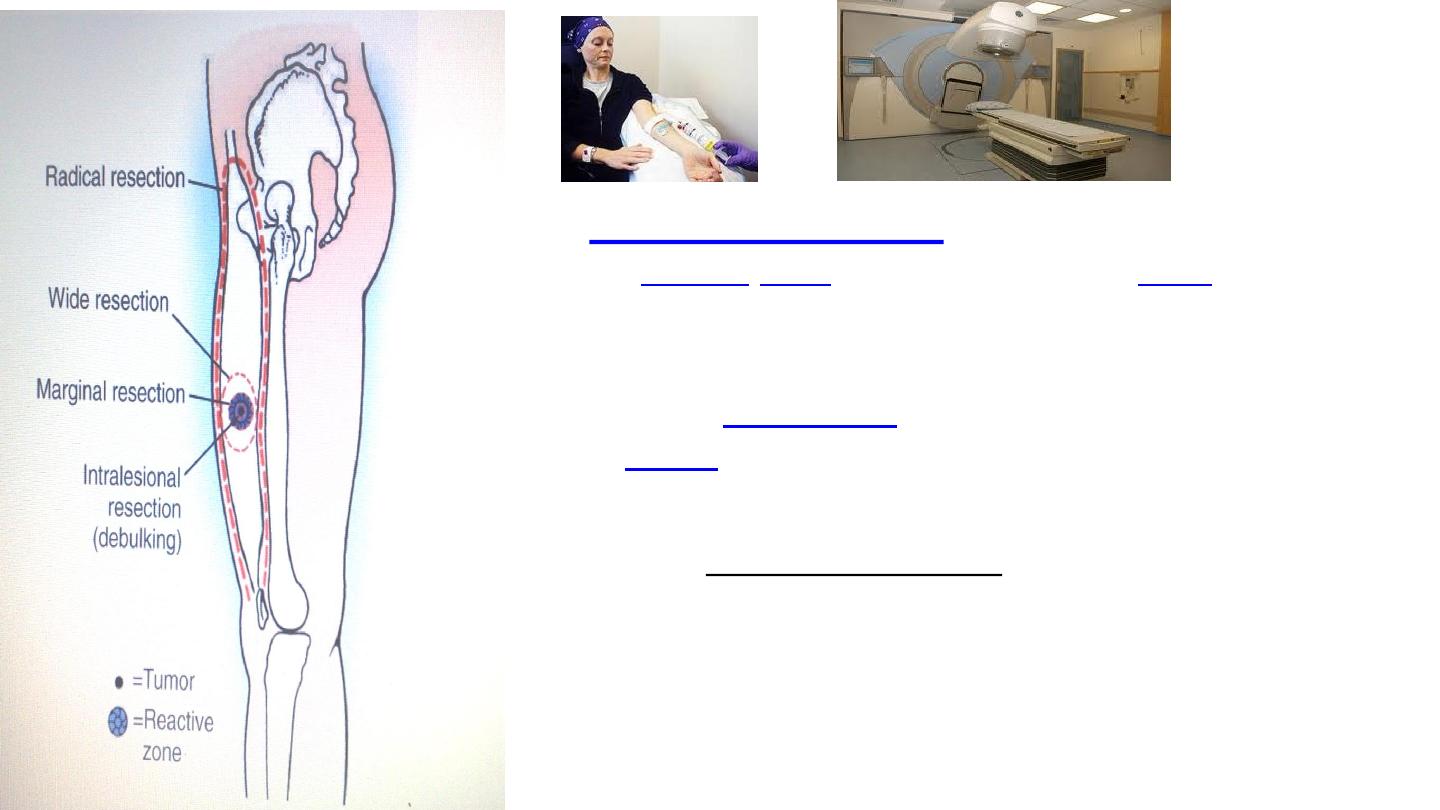
Chemotherapy
usually begins before
any surgery. Decreased tumor size on x-
ray, decreased pain level, and decreased
serum alkaline phosphatase which
indicate some response
,
uses high-energy radiation to
kill
by damaging their
.
…….The radiation used for cancer treatment
may come from a machine outside the body, or it may
come from
material placed in the body
near
