NEONATAL SEPSIS:
Definition:
A clinical syndrome of systemic illness accompanied by
bacteremia occurring in the first month of life,
especially
among premature & V.L.B.W. Infants.
- It usually presents
as septicemia, pneumonia, meningitis, arthritis,
osteomyelitis & U.T.I., and
it is the commonest cause of
neonatal mortality.
SOURCE OF INFECTIONS:
- Intra-amniotic infection
(CHORIOAMNIONITIS)
by ascending route is
the commonest source for neonatal sepsis.
The primary sites of infection are the skin,
nasopharynx, oropharynx conjunctiva, &
umbilicus.
- Some infections are transmitted
transplacentally
(CONGENITAL or TORCH INFECTIONS)
.

Neonates are more liable to get infections because
:
1. Immaturity of the immune system.
• 2. They have low level of complements.
• 3. Impaired function of neutrophils,
monocytes, & macrophages.
• 4. K-cells (killer cells) have diminished
cytotoxic effect.
• 5. IgM & IgA do not cross the placenta.
TYPES OF SEPSIS:
1.Early
Onset Sepsis
:
• - Usually occurs in the first wk. of life,
characterized by multisystem, fulminant
illness with prominent respiratory
symptoms caused by group B
Streptococci (G.B.S.), Listeria
monocytogenes, & viruses e.g. CMV.
• - 90% of cases presents in the first 24 hr. as
respiratory distress which proceeds to
respiratory failure.
• -
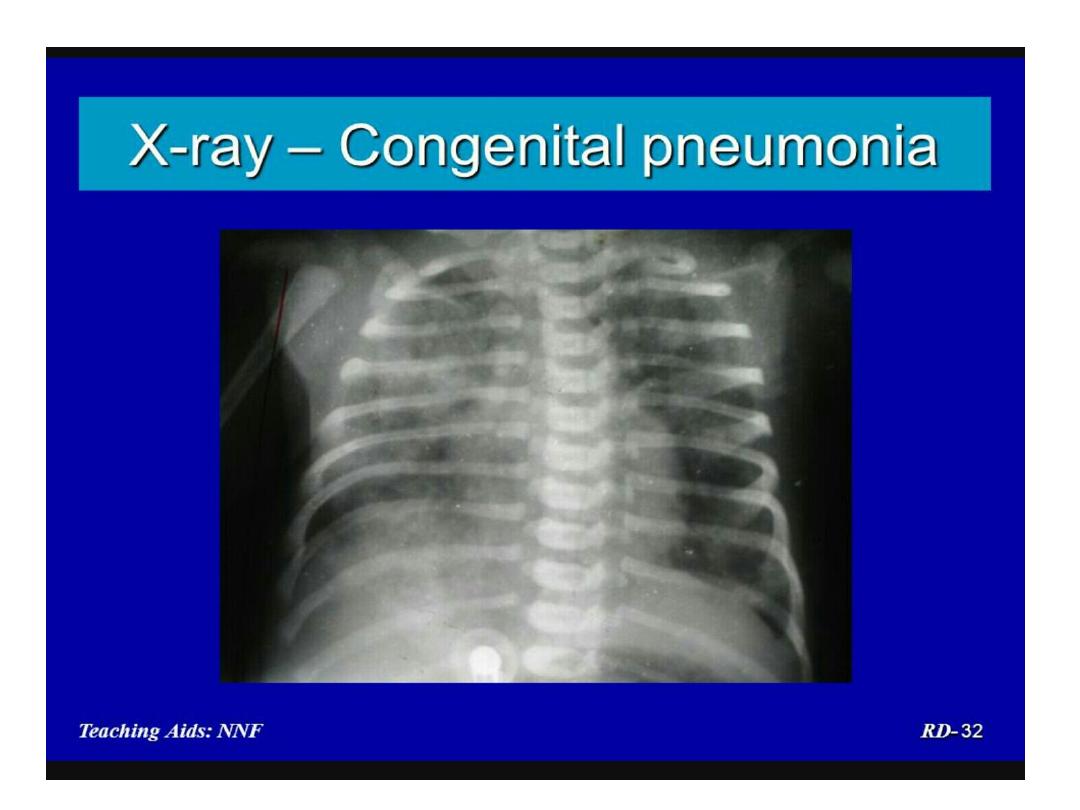
Pneumonia is commonest disease
.
2.Late Onset Sepsis:
• - It usually presents after the first wk.
•
- Commonly presents as meningitis.
• - G.B.S. is the commonest organism
but Listeria monocytogenes
accounts for up to 20%.
3.Nosocomial
Infection
:
• - Usually occurs in the N.I.C.U. & in ill
infants.
• - It depends on N.I.C.U. environment,
invasive monitoring and techniques.
• - Common organisms are staphylococcus
epidermidis, Gram –ve bacteria (e.g.
E.coli, Pseudomonas, Klebsiella, Proteus)
& fungi.
Risk factors for neonatal sepsis:
• 1. Prematurity.
• 2. Prolonged rupture of membranes (>
24 hr.).
3. Maternal fever (> 38c).
• 4. Maternal U.T.I. or genital infection.
• 5. Meconium stained or foul smelling
amniotic fluid.
• 6.
Multiple
gestation
.
CLINICAL PRESENTATION :
• 1. Reluctance to feed.
• 2. Respiratory distress, grunting & apnea.
• 3. Lethargy, decreased or absent
movements & neonatal reflexes.
• 4. Hypo or hyperthermia (only 50% of
infected neonates have high temp.).
• 5. Vomiting, diarrhea, abdominal distension.

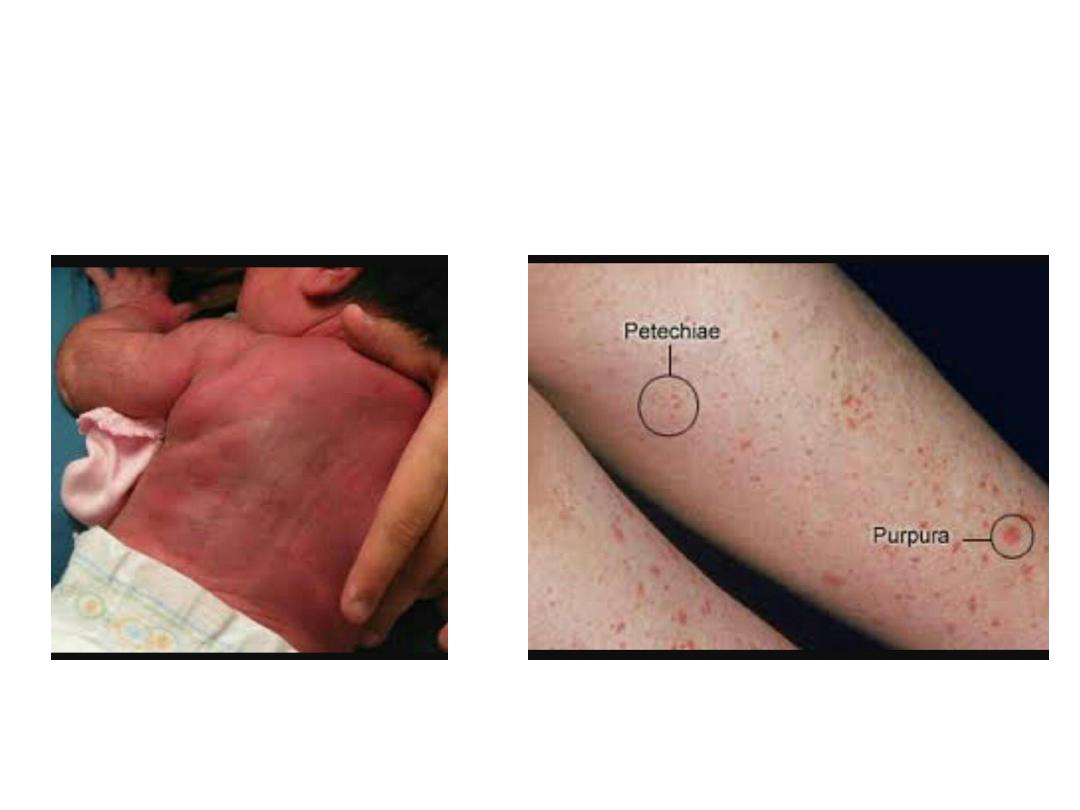
6. Skin rash, petechiae, purpura, skin
mottling (cutis marmorata),
ecthyma gangrenosum (deep ulcers with
ecchymotic margins commonly seen in
mpetigo, cellulitis,
i
infection),
klebsiella
omphalitis.
•
•
• 7. Hypoglycemia.
• 8. Sclerema , Edema.
9. Hepatosplenomegaly, jaundice.
•
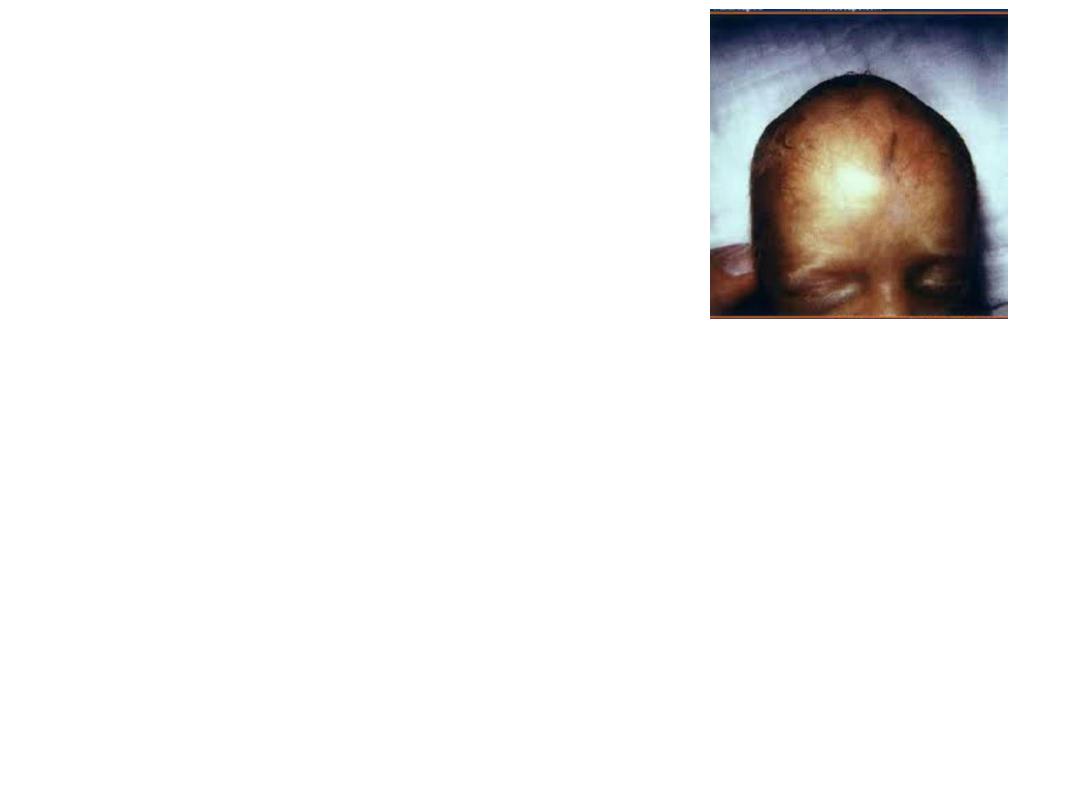
• 10. Convulsions, bulging anterior fontanel.
(Sclerema means hardening of skin &
subcutaneous tissue)
•
Differential Diagnosis:
1. R.D.S.
• 2. Perinatal asphyxia.
• 3. Intracranial hemorrhage.
• 4. Severe congenital heart disease.
• 5. Inborn errors of metabolism.
So a high index of suspicion is the corner
stone for diagnosis of sepsis because
clinical symptoms are non-specific.
LAB STUDIES:
1.Complete Blood Picture:
a) Low platelet count(
<100.000/c.mm).The presence of
large platelets has poor prognosis.
b) Total WBC count is increased or decreased.
Neutropenia(<1500) is common. The immature to total
neutrophil ratio (I:T) is increased > 0.2 (normally it is up to
0.16). 2. Elevated ESR & CRP (C-reactive
protein). 3. Blood Culture ( for aerobic & anaerobic
cultures) is +ve in < 30% of cases. 4. CSF Culture
(because meningitis occurs in 1/3
rd
. of cases).

5. P.C.R.
• 6. Imaging studies ( CXR, ultrasound, CT,
MRI).
• 7.Elevated IgM level (in congenital
infections).
Indications
of
Lumbar
Puncture :
1. Infants with +ve
blood
culture.
2. Clinical & Lab. data suggestive of
bacteremia.
3. No response or deterioration while on
antimicrobial tratment.
TREATMENT:
• - Early treatment is very
important.
- No delay is made waiting for
lab. results.
•

BUT REMEMBER THAT:
• Prolonged empirical Rx (≥5 days) with broad-
spectrum antibiotics for preterm neonates is
associated with higher risks of N.E.C. & death.
So antimicrobial therapy should be discontinued at
48 hours if clinical probability of sepsis is low & CRP
remains normal.
TREATMENT :
• 1. Antibiotics:
should be given by intravenous route.
• Duration of Rx:
Clinical sepsis (based on clinical
suspicion) : 7-10 days.
Pneumonia: 10-14 days.
Meningitis: 2-3 weeks.
Osteomyelitis: 4-6 weeks.

CHOICE OF ANTIBIOTICS:
• - A combination of ampicillin & an aminoglycoside
(e.g. gentamicin) or ampicillin & 3
rd
. generation
cephalosporin (e.g.cephotaxim) is generally used
against Gm+ve, Gm-ve & Listeria.
• -Ceftriaxone is contraindicated in neonates
because it is highly protein bound and may
displace bilirubin, leading to a risk of kernicterus.
-Metronidazole for anaerobic infections (for 7-
10days).

• 2. Supportive care (incubator, O2, i.v.fluid &
electrolytes, dopamine, TPN, IPPV, vit.K,
blood & blood products).
• 3. I.V.Immunoglobulin: which promotes
host defences by multiple mechanisms.
4. Granulocyte transfusion.
•
COMPLICATIONS:
1. Septic emboli.
2. Abscesses.
3.Septic shock.
4.DIC.
5.Mortality is about 50% .
