Rheumatoid disease & Neurologic disorders
DENTALMANAGEMENTOF THE MEDICALLYCOMPROMISED PATIENTMosul university- College of dentistry-oral & maxillofacial surgery department
Dr.Ziad H. Delemi
B.D.S, F.I.B.M.S (M.F.)
Mosul university- College of dentistry-oral & maxillofacial surgery department
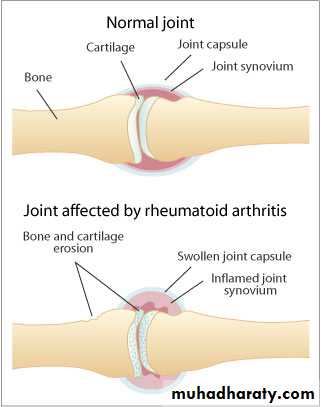
Chronic systemic inflammatory disease affecting synovial membranes & articular structures of multiple joints, Female:Male ratio is 3:1, Age of onset usually between 25 & 50 years.Rheumatoid arthritis (RA)
Pathophysiology & Complications
Autoimmune response
Inflammation & hyperplasia of synovium
CD4 cells activate macrophages & B cells
Osteoclasts & chondroclasts are activated
Mosul university- College of dentistry-oral & maxillofacial surgery department
Mosul university- College of dentistry-oral & maxillofacial surgery department
Rheumatoid arthritis
Mosul university- College of dentistry-oral & maxillofacial surgery departmentDIAGNOSIS OF RHEUMATOID ARTHRITIS
Morning stiffness of > 1 hour
Arthritis involving 3 or more joints
Arthritis of hand joints
Symmetric arthritis
Subcutaneous nodules
Positive test for rheumatoid factor (RF)
Radiographic evidence of RA
Mosul university- College of dentistry-oral & maxillofacial surgery department
LABORATORY DIAGNOSIS OF RHEUMATOID ARTHRITISComplete blood count (CBC)
Rheumatoid factor (latex agglutination test)
Rheumatoid factor
IgM, IgG and IgA
Cyclic citrullinated peptide (CCP) antibody
C-reactive protein (CRP)
Erythrocyte sedimentation rate (ESR)
Anti-nuclear antibody (ANA)
Mosul university- College of dentistry-oral & maxillofacial surgery department
ERYTHROCYTE SEDIMENTATION RATE (ESR)
Non-specific measure of inflammation
Fibrinogen causes RBC’s to stick together
Distance (mm) erythrocyte layer moves in 1 hour
Reference range (Westergren method)< 15 mm/hr (Males < 50)
< 20 mm/hr (Females < 50)
Less sensitive than CRP
Elevation within 5 to 7 daysSimple and inexpensive
Mosul university- College of dentistry-oral & maxillofacial surgery department
TREATMENT OF RHEUMATOID ARTHRITISNonsteroidal anti-inflammatory drugs (NSAIDs)
Aspirin, ibuprofen , naproxen , celecoxib....
Analgesic drugs
AcetaminophenDisease Modifying Anti-rheumatic Drugs (DMARDs)
Methotrexate, hydroxychloroquine (Plaquenil), azathioprine (Imuran)
Biological Response Modifiers
Etanercept (Enbrel), infliximab (Remicade), adalimumab (Humira)1- Short appointments
2- Insurance of physical comfort- Frequent position changes
- Comfortable chair position
-Physical supports as needed (pillows, towels, etc.)
3-Drug considerations
-Aspirin & NSAIDs—bleeding may be increased but is not clinically significant
-Gold salts, penicillamine, antimalarials, immunosuppressive-get complete blood cell count with differential, bleeding time; treat stomatitis symptomatically
-Corticosteroids—adrenal suppression possible
Dental Management of the Patient With Rheumatoid Arthritis
Mosul university- College of dentistry-oral & maxillofacial surgery department
Mosul university- College of dentistry-oral & maxillofacial surgery department
4-Joint prosthesis—prophylactic antibiotics are suggested (cephalosporin or clindamycin)5-Technical treatment modification dictated by patient's disabilities
6-TMJ pain/dysfunction-sudden occlusal changes possible:
-Decrease jaw function
-Soft, nonchallenging diet
-Moist heat or ice to face/jaw .
-Medication as directed by physician
-Occlusal appliance to decrease joint loading
-Consider surgery for persistent pain or dysfunction
Dental Management of the Patient With Rheumatoid Arthritis
Mosul university- College of dentistry-oral & maxillofacial surgery department
OSTEOARTHRITIS (OA)
Degenerative joint disease, is the most common form of arthritis. Almost everyone older than 60 years of age develops OA to some degree, OA is the leading cause of disability among the elderlyOA, which is considered a regional disease, usually affects often used joints such as hips, knees, feet, spine, and hands. The TMJ also is affected. Women are afflicted twice as often as men. It is generally a disease of middle to older age, first appearing after the age of 40.
Mosul university- College of dentistry-oral & maxillofacial surgery department
The articular cartilage becomes thicker than normal, & water content increased, This reflects a repair by the chondrocytes & may last for several years. the joint surface becomes thin leading to softening of the cartilage. Progressive splitting & abrasion of cartilage down to the subchondral bone occur. The exposed bone becomes polished & sclerotic, resembling ivory. Some resurfacing with cartilage may occur if the disorder is arrested or stabilized. New bone forms at the margin of the articular cartilage in the non–weight-bearing part of the joint, creating osteophytes (or spurs).Pathophysiology & Complications
Mosul university- College of dentistry-oral & maxillofacial surgery department
In contrast to RA, OA has a more favorable prognosis & less serious complications, depending on the joint or joints involved. The two most important complications associated with OA are pain & disability.Although RA is a more serious disease, Conservative treatment often can retard the progress of the disease; however, surgery may be required to restore function & reduce pain.
Pathophysiology & Complications
Mosul university- College of dentistry-oral & maxillofacial surgery department
osteoarthritis
Dental Management of the Patient With OsteoarthritisSame as Rheumatoid arthritis
Mosul university- College of dentistry-oral & maxillofacial surgery department
LUPUS ERYTHEMATOSUSIs a connective tissue disorder & has two forms:
1-discoid, (DLE): affects the skin & characterized by chronic, erythematous, scaly plaques on the face, scalp, or ears. Most patients do not have systemic manifestations, & the course tends to be benign.
2-systemic,(SLE): affects multiple organ systems & is the more serious form.
Mosul university- College of dentistry-oral & maxillofacial surgery department
Pathophysiology & Complications
Antibodies are formed in response to some antigenic stimulus, & the reaction between antigen & circulating antibodies forms Ag/Ab complexes, which are deposited in the tissues & organs, including the kidney, skin, blood vessels, muscles & joints, heart, lung, brain, GIT, lymphatics, & eye. The complications includes acute vascular neurologic events, renal failure, & cardiovascular or pulmonary involvement.
Mosul university- College of dentistry-oral & maxillofacial surgery department
-classic picture of SLE is that of a young woman with Polyarthritis & a butterfly-shaped rash across the nose & cheeks-Serious renal abnormalities
-Neuropsychiatric symptoms
-Pulmonary & Cardiac manifestations
Signs & Symptoms
Mosul university- College of dentistry-oral & maxillofacial surgery department
butterfly rash
Finger turns blue
Signs & SymptomsMosul university- College of dentistry-oral & maxillofacial surgery department
1-Consultation with physician
-Extent of systemic manifestations (i.e., kidney, heart)
-Hematologic profile [CBC] with differential, [PT], [PTT], [BT]
-Drug profile
2-Infective endocarditis is a potential problem—AB prophylaxis is not recommended by the AHA.
Dental Management of Patient With SLE
Mosul university- College of dentistry-oral & maxillofacial surgery department
3-Drug considerations- Aspirin& (NSAIDs)-bleeding may be ↑↑ but is not usually clinically significant; if patient is concurrently taking corticosteroids, bleeding is more likely—suggest obtaining pretreatment bleeding time (<20 minutes)
-Gold salts, antimalarials, penicillamine,& cytotoxic drugs may cause leukopenia & thrombocytopenia; also, severe stomatitis—treat symptomatically
- Corticosteroids may cause adrenal suppression
Dental Management of Patient With SLE
Mosul university- College of dentistry-oral & maxillofacial surgery department
4- Hematologic considerations-Leukopenia with corticosteroids or cytotoxic drugs may predispose patient to infection; use of postoperative antibiotics can be considered with surgical procedures
-Platelet count <50,000/mm may result in severe bleeding—consultation with physician
-Elevated PTT associated with lupus anticoagulant usually does not cause increased bleeding—surgery can be performed
Dental Management of Patient With SLE
Mosul university- College of dentistry-oral & maxillofacial surgery department
Five of the more common and significant neurologic diseases:
1- Epilepsy
2- Stroke
3- Parkinson's disease
4- Alzheimer's disease
5- Multiple sclerosis
NEUROLOGIC DISORDERS
Mosul university- College of dentistry-oral & maxillofacial surgery department
EPILEPSYis a term that refers to a group of disorders characterized by chronic recurrent, paroxysmal changes in neurologic function (seizures), altered consciousness, or involuntary movements caused by abnormal & spontaneous electrical activity in the brain. Seizures may be convulsive (i.e., accompanied by motor manifestations) or may occur with other changes in neurologic function (i.e., sensory, cognitive, and emotional).
Mosul university- College of dentistry-oral & maxillofacial surgery department
Classification of Epileptic SeizuresI.PARTIAL (FOCAL, LOCAL)
II. GENERALIZED (CONVULSIVE OR NONCONVULSIVE) Absence seizures (petit mal)
Myoclonic seizuresTonic-clonic seizures (grand mal)
Tonic seizures
Atonic seizures
III .UNCLASSIFIED EPILEPTIC SEIZURES
EPILEPSY
Mosul university- College of dentistry-oral & maxillofacial surgery department
An excessive focal neuronal discharge that spreads to thalamic & brainstem nuclei. The cause is unknown, but may be due to altered sodium channel function, altered neuronal membrane potentials, altered synaptic transmission, diminution of inhibitory neurons, increased neuronal excitability, and decreased electrical threshold for epileptic activity. During the seizure, blood becomes hypoxic, & lactic acidosis occurs.
Pathophysiology & Complications
Mosul university- College of dentistry-oral & maxillofacial surgery department
Complications includes trauma (as a result of falls) to the head, neck, & mouth & aspiration pneumonia. Also, frequent & severe seizures are associated with altered mental function, dullness, confusion, & increased risk of sudden deathPathophysiology & Complications
Mosul university- College of dentistry-oral & maxillofacial surgery department
A serious acute complication of epilepsy (especially tonic-clonic) is the occurrence of repeated seizures over a short time without a recovery period, occurs due to abrupt withdrawal of anticonvulsant medication or an abused substance but may be triggered by infection, neoplasm, or trauma. It constitutes a medical emergency. Patients may become seriously hypoxic & acidotic during this event & suffer permanent brain damage or death.Status Epilepticus
Mosul university- College of dentistry-oral & maxillofacial surgery department
An aura (a momentary sensory alteration that produces an unusual smell or visual disturbance). Irritability. After the aura warning, the patient emits a sudden “epileptic cry” and immediately loses consciousness. The tonic phase consists of generalized muscle rigidity, pupil dilation, eyes rolling upward or to the side. Breathing may stop because of spasm of respiratory muscles. This is followed by clonic activity.Signs & Symptoms
Mosul university- College of dentistry-oral & maxillofacial surgery department
Clonic activity that consists of uncoordinated beating movements of the limbs & head, forcible jaw closing, & head rocking. Urinary incontinence is common, The seizure lasts 90 seconds; then, movement ceases, muscles relax, & a gradual return to consciousness occurs, which is accompanied by stupor, headache, confusion, & mental dulling. Several hours of rest or sleep may be needed for the patient to fully regain cognitive & physical abilities.Signs & Symptoms
Mosul university- College of dentistry-oral & maxillofacial surgery department
Signs & Symptoms
Mosul university- College of dentistry-oral & maxillofacial surgery departmentMEDICAL MANAGEMENT
Anticonvulsants Used in the Management of Generalized Tonic-Clonic :
Phenytoin (Dilantin)
Carbamazepine (Tegretol)
Valproic acid (Depakene)
ALTERNATIVES
Clonazepam (Klonopin)
Ethosuximide (Zarontin)
Phenobarbital (Luminal)
Mosul university- College of dentistry-oral & maxillofacial surgery department
1- Identification of patient by historyType of seizure
Age at time of onset
Cause of seizures (if known)
Medications
Frequency of physician visits (name and phone number)
Degree of seizure control
Frequency of seizures
Date of last seizure
Known precipitating factors
History of seizure-related injuries
Dental Management of the Epileptic Patient
Mosul university- College of dentistry-oral & maxillofacial surgery department
Dental Management of the Epileptic Patient
2-Provision of normal care: Well-controlled seizures pose no management problems
3-If questionable history or poorly controlled seizures, consultation with physician before dental treatment
4-Attention to adverse effects of anticonvulsants.
5-Possibility of bleeding tendency in patients taking (Depakene) or (Tegretol) as the result of platelet interference
Mosul university- College of dentistry-oral & maxillofacial surgery department
6-Management of grand mal seizurePossible placement of a ligated mouth prop at the beginning of the procedure
Chair back in supported supine position
7-Management of the seizure
Clear the area
Turn the patient to the side (to avoid aspiration)
Do not attempt to use a padded tongue blade
Passively restrain
8-After the seizure
Examine for traumatic injuries
Discontinue treatment, arrange for patient transport
Dental Management of the Epileptic Patient
Mosul university- College of dentistry-oral & maxillofacial surgery department
Stroke is a generic term that is used to refer to a cerebrovascular accident—a serious & often fatal neurologic event caused by sudden interruption of oxygenated blood to the brain. This in turn results in focal necrosis of brain tissue & possibly death. Even if a stroke is not fatal, the survivor often is to some degree debilitated in motor function, speech, or mentation.
STROKE (CVA)
Mosul university- College of dentistry-oral & maxillofacial surgery department
1- Identify risk factors.Hypertension
Congestive heart failure
Diabetes mellitus
TIA or previous stroke
Increasing age 75 years
Elevated blood cholesterol or lipid levels
Coronary atherosclerosis
Cigarette smoking
Dental Management of the Patient With Stroke
Mosul university- College of dentistry-oral & maxillofacial surgery department
Dental Management of the Patient With Stroke2-History
Provide only urgent dental care during first 6 months after a stroke, TIA, Avoid elective care
Determine risk for bleeding problems in patients taking anticoagulant drugs, & minimize perioperative bleeding.
Heparin (IV)—Use palliative emergency dental care only, or 6 to 12 hours before surgery, discontinue heparin & start another anticoagulant (e.g., coumadin) with physician's approval.
Mosul university- College of dentistry-oral & maxillofacial surgery department
Use measures that minimize hemorrhage (atraumatic surgery, pressure, gelfoam, suturing), as needed.Have available nonadrenergic haemostatic agents & devices (stents, electrocautery).
3-stress-free, midmorning appointments.
4- Monitor blood pressure and oxygen saturation5- Use minimum amount of anesthetic containing vasoconstrictor.
6- Avoid epinephrine in retraction cord.
Dental Management of the Patient With Stroke
Mosul university- College of dentistry-oral & maxillofacial surgery department
is a progressive neurodegenerative disorder of neurons that produce dopamine. Loss of these neurons results in characteristic motor disturbances (resting tremor, muscular rigidity, bradykinesia, postural instability). Dopaminergic neurons are found in the nigrostriatal pathway of the brain. This disease is chronic & progressive.PARKINSON’S DISEASE
Mosul university- College of dentistry-oral & maxillofacial surgery department
Hydrocephalus is an increasing accumulation of CSF within the cerebral ventricles. It is often requires placement of a shunt within cerebral ventricles & peripheral cavities to reduce increased CSF pressure. (Vetriculoperitoneal, Ventriculoatrial, Lumboperitoneal) are the most common types of shunts. With respect to dentistry, the most significant concern is the risk of CSF shunt infection. CSF shunt infections usually occur within 2 months after implantation.The AHA has issued a statement indicating that antibiotic prophylaxis is not recommended for patients with CSF shunts who are undergoing dental procedures.
CEREBROSPINAL FLUID SHUNTS