4
th
Stage/2020
1
University of Mosul
College of Dentistry
Oral & Maxillofacial Surgery
Department
4
th
Stage/2020
Osteomyelitis
Osteomyelitis is an inflammatory condition of the bone, which begins as an infection of the
medullary cavity, rapidly involves the haversian systems, and extends to involve the periosteum
of the affected area.
Classification
The general categories of osteomyelitis of the jaws include:
1. Suppurative.
2. Primary.
3. Chronic sclerosing.
4. Osteomyelitis with proliferative periostitis (Garre osteomyelitis).
The vast majority of osteomyelitis cases are caused by bacterial infections and result in an
expanding lytic destruction of the involved bone, with suppuration and sequestra formation.
This condition is more appropriately termed suppurative osteomyelitis, bacterial
osteomyelitis, or secondary osteomyelitis. Traditionally, Staphylococcus species were the
predominant bacteria involved as in the other bones of the body, although it is known now that
several other organisms may contribute to the disease process. The microbiologic profile most
often present in cases of osteomyelitis of the mandible includes Streptococci spp., as well as
anaerobic bacteria, such as Bacteroides or Peptostreptococcus.
Primary chronic osteomyelitis, by contrast, does not respond consistently to antibacterial
medications and typically demonstrate ultimate sclerosis of bone without suppuration or
sequestra formation.
4
th
Stage/2020
2
University of Mosul
College of Dentistry
Oral & Maxillofacial Surgery
Department
4
th
Stage/2020
Predisposing factors:
Though the marrow of the maxilla and mandible are often exposed to periapical pathogens,
osteomyelitis is rare. This is because host defenses usually localize the infection to a periapical
abscess and limit the progression. However, some conditions increase the incidence of the
occurance such as;
• Chronic systemic diseases.
• Immunocompromised status.
• Disorders associated with hypovascularized bone (e.g., osteopetrosis, dysosteosclerosis,
late Paget disease, end-stage cementoosseous dysplasia).
• Tobacco use, alcohol abuse, IV drug abuse.
• Diabetes mellitus.
• Malaria.
• Sickle cell anemia.
• Malnutrition.
• Malignancy.
• Collagen vascular diseases.
• AIDS.
• Radiation
Note
Osteomyelitis is more common in the mandible than the maxilla; this
is due to the fact that the blood supply to the maxilla is multifocal
and robust, which is in contrast with the mandible that primarily
obtains its blood supply from the inferior alveolar artery and
periosteum. In contrast, the periosteal blood supply to the maxilla
penetrates its cortex to perfuse the underlying porous bone much
easier than that of the much thicker cortex of the mandible.
4
th
Stage/2020
3
University of Mosul
College of Dentistry
Oral & Maxillofacial Surgery
Department
4
th
Stage/2020
1. Suppurative osteomyelitis (Secondary Osteomyelitis)
A. Acute suppurative osteomyelitis exists when an acute inflammatory process spreads
through the medullary spaces of the bone and the patients have signs and symptoms for less
than 1 month in duration.
Clinical features:
Symptoms are pain, tenderness and swelling in the affected area similar to an acute dental
infection . The mandible is affected more frequently than the maxilla. Where the body or lower
ramus of the mandible is affected, an important symptom is a developing numbness over the
chin as a result of inferior alveolar nerve involvement. On occasion, paresthesia of the lower lip,
drainage, or exfoliation of fragments of necrotic bone may be discovered. A fragment of
necrotic bone that has separated from the adjacent vital bone is termed a sequestrum. On
occasion, fragments of necrotic bone may become surrounded by new vital bone, and the dead
bone in this situation is known as an involucrum.
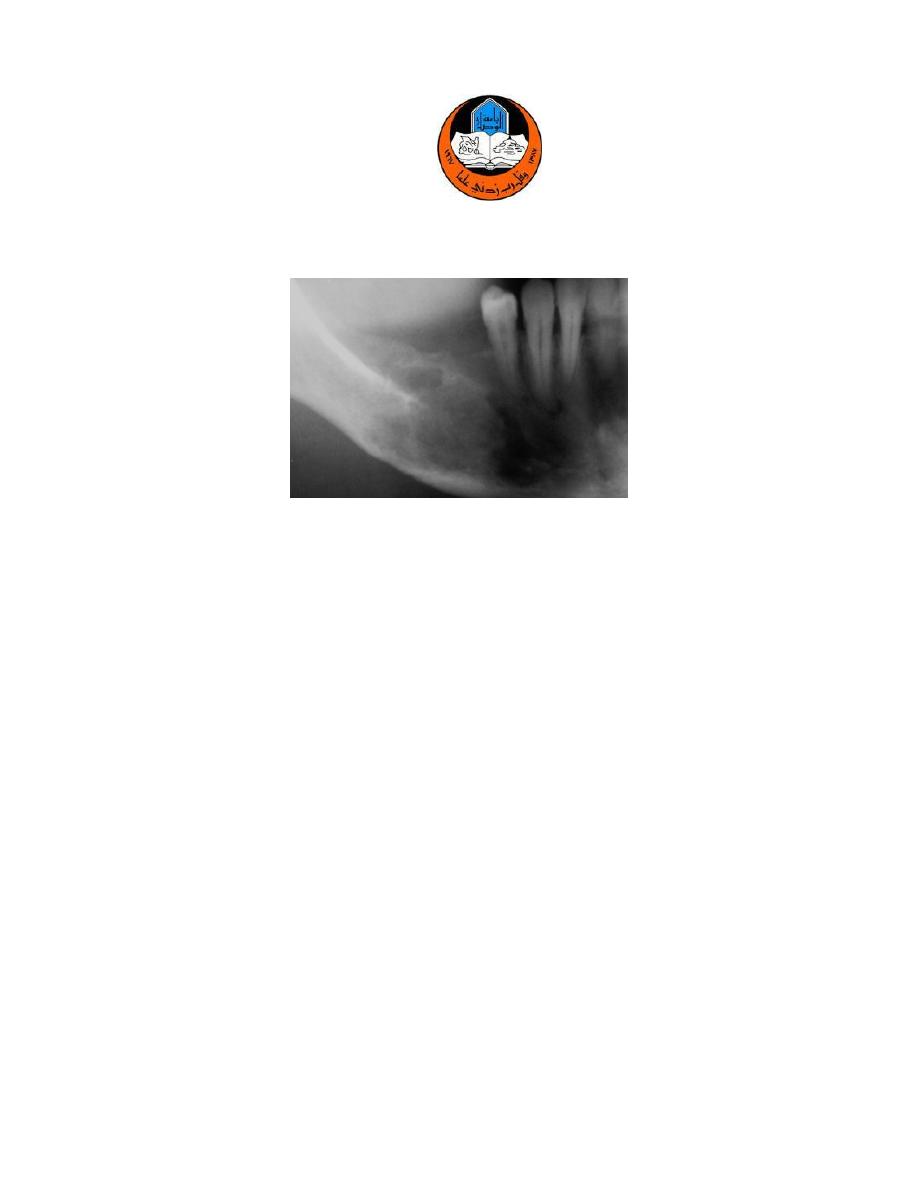
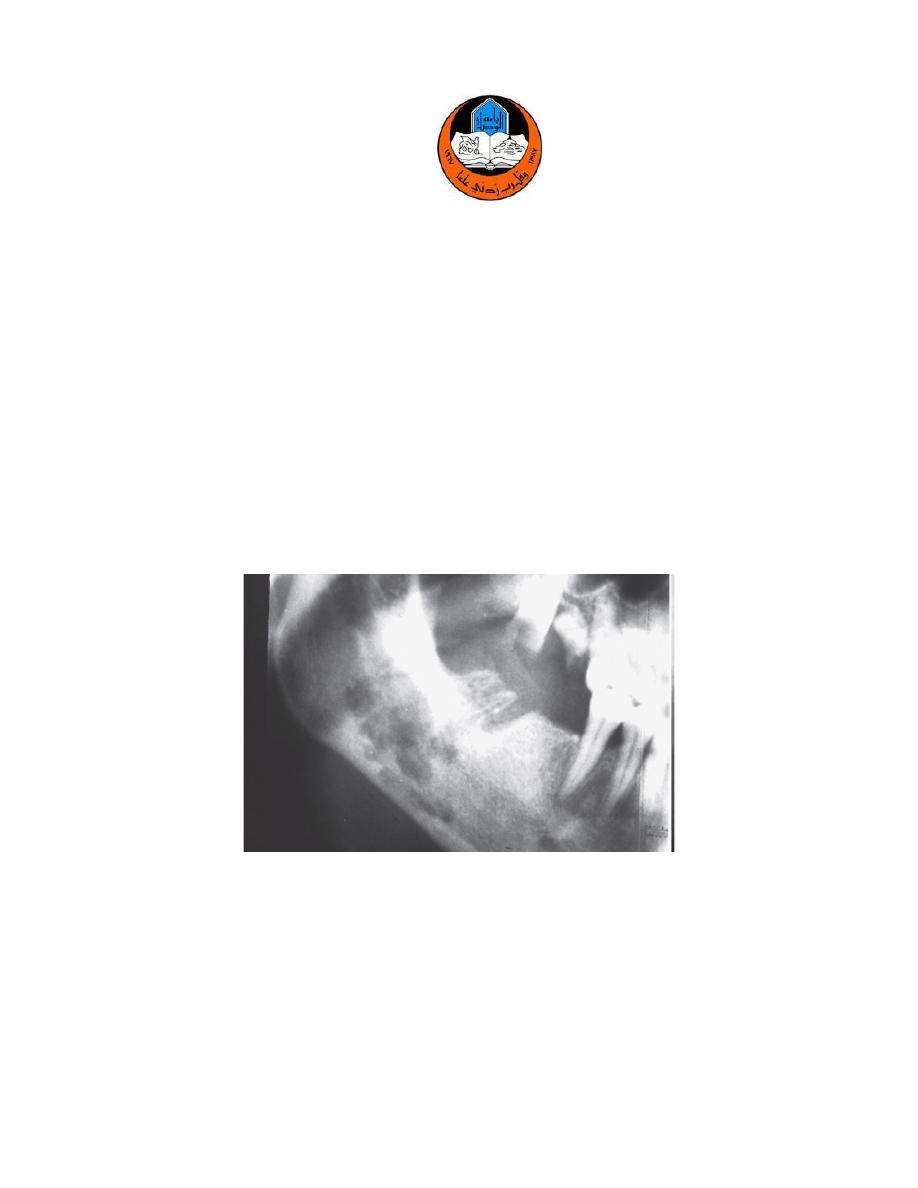
Radiographical findings
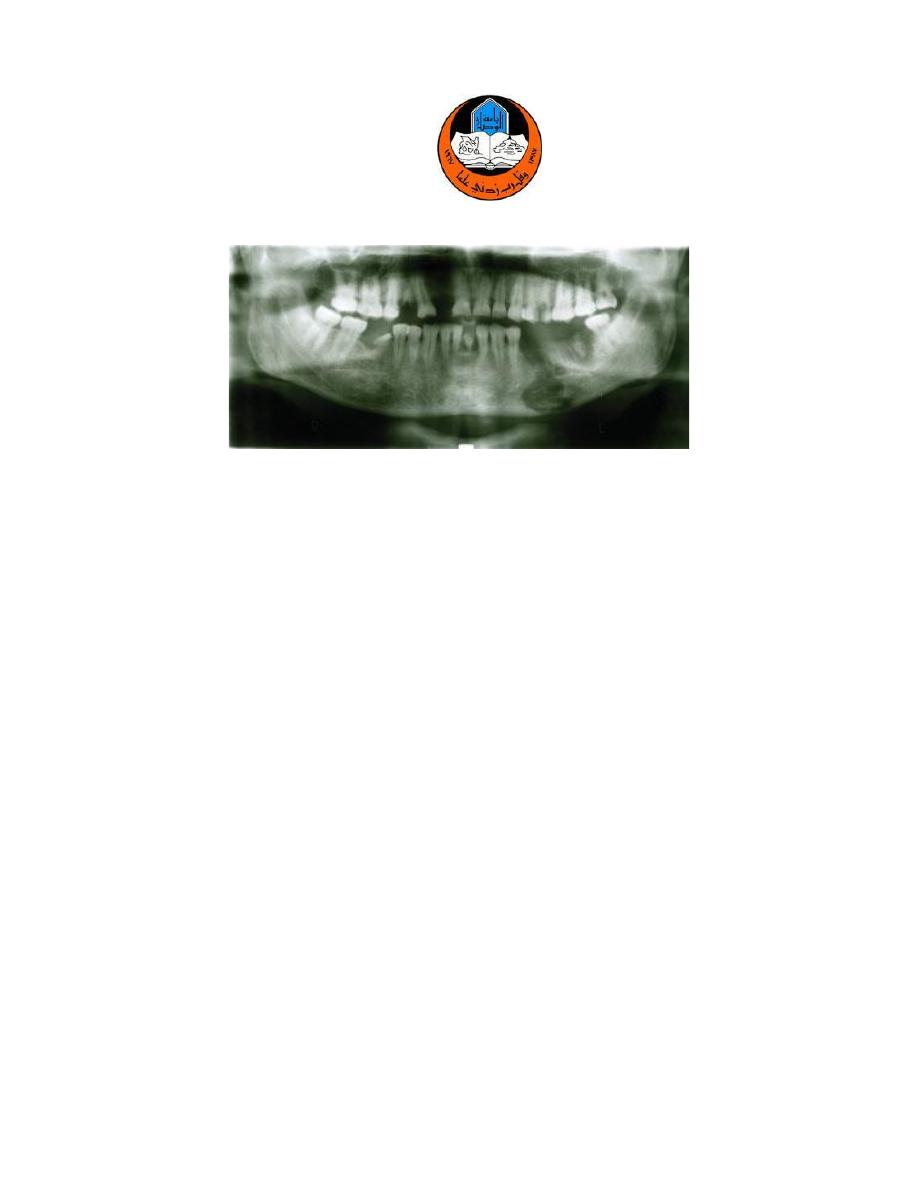
Plain dental or panoramic radiographs may demonstrate an ill-defined radiolucency (Fig.1),
occasionally combined with widening of the periodontal ligament, loss of lamina dura, or loss of
circumscription of the inferior alveolar canal or mental foramen. Periosteal new bone formation
also may be seen in response to subperiosteal spread of the infection. Cone-beam CT
represents another excellent alterative with shorter scanning times and lower doses of
radiation when compared to conventional CT.
4
th
Stage/2020
4
University of Mosul
College of Dentistry
Oral & Maxillofacial Surgery
Department
4
th
Stage/2020
Fig. 1- Acute Osteomyelitis. Ill-defined area of radiolucency of the right body of the mandible
Histopathologic Features
Acute osteomyelitis the biopsy consists predominantly of necrotic bone. The bone shows a loss
of the osteocytes from their lacunae, peripheral resorption, and bacterial colonization (Fig.
3-46). The periphery of the bone and the haversian canals contain necrotic debris and an acute
inflammatory infiltrate consisting of polymorphonuclear leukocytes.
Treatment and Prognosis
Therapy centers around surgical intervention to 1) resolve the source of infection, 2) establish
drainage, 3) removal of obviously infected bone, and 4) obtain bacteriologic samples for culture
and antibiotic sensitivity testing. While waiting on the bacteriologic evaluation, antibiotics are
administered empirically, usually penicillin with metronidazole or clindamycin. Antibiotics
should be continued for at least 2 weeks after control of the acute infection.
4
th
Stage/2020
5
University of Mosul
College of Dentistry
Oral & Maxillofacial Surgery
Department
4
th
Stage/2020
Summary of management of acute osteomyelitis
➢ Essential measures
• Bacterial sampling and culture
• Vigorous (empirical) antibiotic treatment
• Drainage
• Analgesics
• Give specific antibiotics once culture and sensitivities
• Debridement
• Remove source of infection, if possible
➢ Adjunctive treatment
• Sequestrectomy
• Decortication if necessary
• Resection and reconstruction for extensive bone destruction
B. Chronic suppurative osteomyelitis
If acute osteomyelitis is not resolved expeditiously, the entrenchment of chronic osteomyelitis
occurs; or the process may arise primarily without a previous acute episode. Chronic
osteomyelitis exists when the defensive response leads to the production of granulation tissue,
which subsequently forms dense scar tissue in an attempt to wall off the infected area. The
encircled dead space acts as a reservoir for bacteria, and antibiotic medications have great
difficulty reaching the site. This pattern begins to evolve about 1 month after the spread of the
initial acute infection and results in a smoldering process that is difficult to manage unless the
problem is approached aggressively.
4
th
Stage/2020
6
University of Mosul
College of Dentistry
Oral & Maxillofacial Surgery
Department
4
th
Stage/2020
Clinical features
Swelling, pain, sinus formation, purulent discharge, sequestrum formation, tooth loss, or
pathologic fracture may occur. Patients may experience acute exacerbations or periods of
decreased pain associated with chronic smoldering progression.
Radiographical findings
Radiographs reveal a patchy, ragged, and ill-defined radiolucency that may contain central
radiopaque sequestra and be intermixed with zones of radiodensity (Fig.2).
Fig.2- Chronic Osteomyelitis. Ill-defined area of radiolucency of the right body of the mandible adjacent to a
recent extraction site.
4
th
Stage/2020
7
University of Mosul
College of Dentistry
Oral & Maxillofacial Surgery
Department
4
th
Stage/2020
Histopathologic Features
Biopsy material from patients with chronic osteomyelitis demonstrates a significant soft tissue
component that consists of chronically or subacutely inflamed fibrous connective tissue filling
the intertrabecular areas of the bone (Fig. 3-47). Scattered sequestra and pockets of abscess
formation are common.
Treatment and Prognosis
Chronic osteomyelitis is difficult to manage medically, presumably because pockets of dead
bone and organisms are protected from antibiotic drugs by the surrounding wall of fibrous
connective tissue.
1. The antibiotic medications are similar to those used in the acute form but must be given
intravenously in high doses.
2. Surgical intervention is mandatory. The extent of the surgical intervention depends on
the spread of the process; removal of all infected material down to good bleeding bone
is mandatory in all cases.
➢ For small lesions, curettage, removal of necrotic bone, and saucerization are sufficient.
➢ For extensive osteomyelitis, decortication or saucerization often is combined with
transplantation of cancellous bone chips.
➢ For persisting osteomyelitis, resection of the diseased bone followed by immediate
reconstruction with an autologous graft is required. Weakened jawbones must be
immobilized. Scintigraphic techniques with technetium-99m (99mTc)-labeled
phosphorus compounds can be used to evaluate the therapeutic response and progress
of treatment. Hyperbaric oxygen is recommended primarily for the rare patient who
4
th
Stage/2020
8
University of Mosul
College of Dentistry
Oral & Maxillofacial Surgery
Department
4
th
Stage/2020
does not respond to standard therapy or for disease arising in hypovascularized bone (e.g.,
osteoradionecrosis, osteopetrosis, Paget disease, and cemento-osseous dysplasia).
2. Primary Chronic Osteomyelitis
Affected patients have recurrent episodes of pain, swelling, local induration, and limited mouth
opening that is not associated with any obvious dental infection. During periods of disease
activity, regional lymphadenopathy and reduced sensation in the distribution of the inferior
alveolar nerve may be present. Absence of fever, purulence, sequestration, and sinus formation
are characteristic. The lack of an obvious association with an odontogenic infection and the
nonsuppurative presentation clearly separate this condition from chronic suppurative
osteomyelitis. one of the proposed causes is an alteration of immune response to an organism
of low virulence. The predominant radiographic alteration of primary chronic osteomyelitis is
medullary sclerosis.
Treatment
Even with significant surgical and medical intervention, the disease course is characterized by
flares separated by partial remissions. Most treatments directed toward elimination of
infection have been proven ineffective. Long-term antibiotic treatment with or without
hyperbaric oxygen therapy has not produced consistent long-term success. Surgical
decortication has decreased the intensity and frequency of symptoms but has failed to resolve
the process totally. Because of inconsistent results from surgical intervention, extensive surgery
is contraindicated, especially in young, growing patients. Corticosteroid medications, NSAIDs,
calcitonin, and tumor necrosis factor-α antagonists have been reported to relieve symptoms
but usually are associated with incomplete resolution. In a number of publications, IV
4
th
Stage/2020
9
University of Mosul
College of Dentistry
Oral & Maxillofacial Surgery
Department
4
th
Stage/2020
administration of bisphosphonates has shown significant therapeutic benefits with reduction of
symptoms and radiographic resolution of bony abnormalities
3. Chronic Sclerosing Osteomyelitis
This rare form of osteomyelitis is an intramedullary bone infection with one of the Actinomyces
species as well as Eikenella corrodens as the offending organisms. The combination of these
two organisms produces a sclerosis and fibrosis of the medullary space. The pathognomonic
clinical sign is intense pain. This pain may fluctuate along with acute exacerbations of
mandibular expansion and soft tissue edema. Usually a chronic dull pain is always present. In
general, there is no purulence of drainage present. Symptoms may persist for up to 5 years
before recognition and establishment of a diagnosis. Radiographically, there is an increased
trabecular bone density is present in the alveolar and basal bone of the mandible.
Treatment
Although antibiotic therapy, combined with or without hyperbaric oxygen therapy, may
mitigate the progression of the disease, surgical resection of the diseased bone is often
required.
4. Osteomyelitis with Proliferative Periostitis (Garre Osteomyelitis)
It is a chronic disease that usually affects children due to their increased vascularity and
regenerative capabilities. The most notable radiographic finding is paracortical bone formation
(“onion-skinning”) due to repetitive irritation of the periosteum usually associated with a
periapical infection of the mandibular tooth (Fig. 17.25). Clinically there is expansion of the
mandible with pain, but no purulence, drainage, or erythema. Removal of the infectious source
is of paramount importance, and biopsy is considered when a source of infection is not
4
th
Stage/2020
10
University of Mosul
College of Dentistry
Oral & Maxillofacial Surgery
Department
4
th
Stage/2020
identified because malignancy may have similar radiographic findings.
Radiographical findings
Extracortical bone formation in the form of woven bone in layers parallel to the cortex
connected by bridges of bone perpendicular to the cortex is seen.
Treatment
Removal of the offending infectious source a short course of antibiotic therapy (penicillin,
tetracycline, or clindamycin) until the bone inflammation resolves spontaneously.
Alveolar osteitis (dry socket ; fibrinolytic alveolitis)
Alveolar osteitis (dry socket) is the most frequent painful complication of extractions. It is not
really an infection but leads to superficial bacterial contamination of exposed bone and can
progress to osteomyelitis. Osteitis simply means inflamed bone, not infection. The prevalence is
between 1% and 3% of all extractions, but it increases to 25% to 30% for impacted mandibular
third molars.
The cause is early loss of clot from the extraction socket due to excessive local fibrinolytic
activity. The alveolar bone and gingiva have a high content of fibrinolysin activators (plasmin),
that are released when the bone is traumatised, degrading the clot and leaving the socket
empty. Once the clot has been destroyed, bacterial colonisation from the mouth is inevitable,
and bacterial enzymes contribute to clot lysis.
4
th
Stage/2020
11
University of Mosul
College of Dentistry
Oral & Maxillofacial Surgery
Department
4
th
Stage/2020
➢ Predisposing factors for alveolar osteitis
• Difficult disimpactions of third molars or traumatic extractions.
• Lower molar region, where the bone is denser and less vascular than elsewhere.
• Limited local blood supply.
• Gingival infection such as acute ulcerative gingivitis, pericoronitis or abscess.
• Local anaesthesia with vasoconstrictor.
• Smoking.
• Oral contraceptives. The oestrogen component of oral contraceptives enhances serum
fibrinolytic activity and interferes with clotting, and its use is associated with a higher incidence
of alveolar osteitis.
• Osteosclerotic disease: Paget’s disease, cementoosseous dysplasia.
• Radiotherapy.
• History of previous dry socket.
➢ Clinical features
Patients aged 20–40 years are most at risk, and women are more frequently affected if oral
contraceptive use is taken into account.
Typically, pain usually starts a few days after the extraction, but sometimes may be delayed for
a week or more. It is deep-seated, severe and aching or throbbing. On occasion, the pain
radiates from the socket to the ipsilateral ear, temporal region, or eye.
other symptoms include foul odour, and (less frequently) swelling and lymphadenopathy
develop 3 to 4 days after extraction of the tooth. Rarely, trismus also may be noted. The signs
and symptoms may last from 10 to 40 days.
The mucosa around the socket is red and tender. There is no clot in the socket, which contains,
4
th
Stage/2020
12
University of Mosul
College of Dentistry
Oral & Maxillofacial Surgery
Department
4
th
Stage/2020
instead, saliva and often decomposing food debris. When debris is washed away, whitish, dead
bone may be seen or may be felt as a rough area with a probe and probing is painful. The
appearance of an empty socket and exposed bone is diagnostic. Sometimes the socket becomes
concealed by granulations growing in from the gingival margins, narrowing the opening and
trapping food debris. Pain often continues for a week or two, or occasionally longer.
Sequestration of the socket wall may sometimes be seen radiographically (Fig. 8.3), but a
radiograph performs no useful purpose except to exclude retention of a root fragment.
➢ Prevention of dry socket
• Preoperative infection control
• Scaling teeth before extraction
• Chlorhexidine rinsing preoperatively and for 3 days postoperatively
• Atraumatic extraction
•Immediately after the extraction the socket edges should be squeezed firmly together and
held for a few minutes until the clot has formed.
• For norma patients, the value of prophylactic antibiotics is unproven, and there is no
indication for using antibiotics for routine dental extractions.
• Patients who have had irradiation for oral cancer or have sclerotic bone disease,
postoperative antibiotic cover should be given and the tooth removed surgically to cause as
little damage as possible to surrounding bone. Antibiotics are given primarily to prevent
osteomyelitis rather than dry socket.
• Adherence to postoperative instructions
• No rinsing or forceful spitting
• No hot fluids
• No smoking
4
th
Stage/2020
13
University of Mosul
College of Dentistry
Oral & Maxillofacial Surgery
Department
4
th
Stage/2020
• Postoperative antibiotics only for those at particular risk.
• It is important to explain to patients that they may have a week or more of discomfort. It is
also important to explain that the pain is not due, as patients usually think, to a broken root.
➢ Treatment
The aim of treatment is to control symptoms, keep the open socket clean and to protect
exposed bone from excessive bacterial contamination until healing is complete, usually after
approximately 10 days.
➢ Cleaning: The socket should be irrigated with mild warm antiseptic or saline to remove
all food debris. Curettage of the socket is not recommended, because this typically
increases the associated pain.
➢ Dressing: It is then traditional to place a dressing into the socket to deliver analgesia and
close the opening so that further food debris cannot enter the socket. Many socket
dressings have been formulated and should be antiseptic, obtundent, adhere to the
socket wall, and be absorbable. Whatever is used, the minimum dressing to close the
socket opening is used because dressing packed hard into the socket will delay healing.
Non-absorbable dressings must be removed as soon as possible to allow the socket to
heal. A dressing may only last 1–2 days, and the whole process needs repeating until
pain subsides, normally after one or two dressings. Frequent hot saline mouthwashes
also help keep the socket free from debris.
➢ Analgesic prescription.
4
th
Stage/2020
14
University of Mosul
College of Dentistry
Oral & Maxillofacial Surgery
Department
4
th
Stage/2020
Case scenario
Please, read the following senario then explain your management (diagnosis & treatment) of
this case based on the clinical and radiographical presentation
A 48-year-old man reported to the Department of Oral and Maxillofacial Surgery, with an
extraorally draining sinus in the left anteroinferior border of mandible and a foul odor from the
oral cavity for 4.5 months. The patient also complained of paresthesia of the left lower lip for
the previous 1.5 months. The patient reported having pain in the lower left back of the jaw 4.5
months previously.The patient visited a local dentist who extracted the left mandibular second
premolar and first and second molars; following the extractions, pain decreased but the
draining sinus and dull continuous pain persisted. As the condition did not improve, the patient
presented to Oral and Maxillofacial Surgery department for definitive treatment. A panoramic
radiograph was taken, which revealed bifocal radiolucent areas extending between left
mandibular first premolar and third molar.
Note
The colonisation of the socket and sequestra by oral bacteria
probably contributes to pain and slow healing. Anaerobes are
thought to be significant and can produce fibrinolytic enzymes.
However, antibiotics including metronidazole have not been
shown to either prevent dry socket or speed healing reliably. Only
chlorhexidine rinsing preoperatively has been shown to reduce
incidence.
4
th
Stage/2020
15
University of Mosul
College of Dentistry
Oral & Maxillofacial Surgery
Department
4
th
Stage/2020
