Male factor infertility
• Male factor infertility implies a lack of sufficient
numbers of competent sperms, resulting in failure
to fertilize the normal ovum.
• It is directly responsible for 30% of cases of
infertility
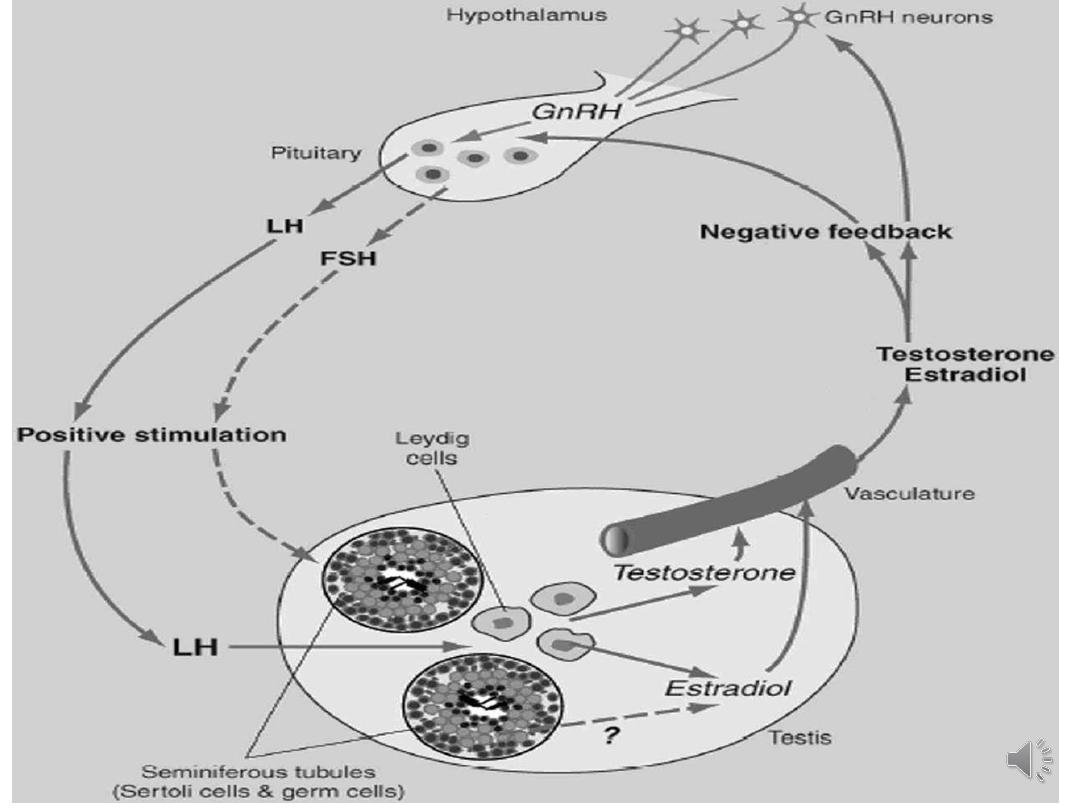
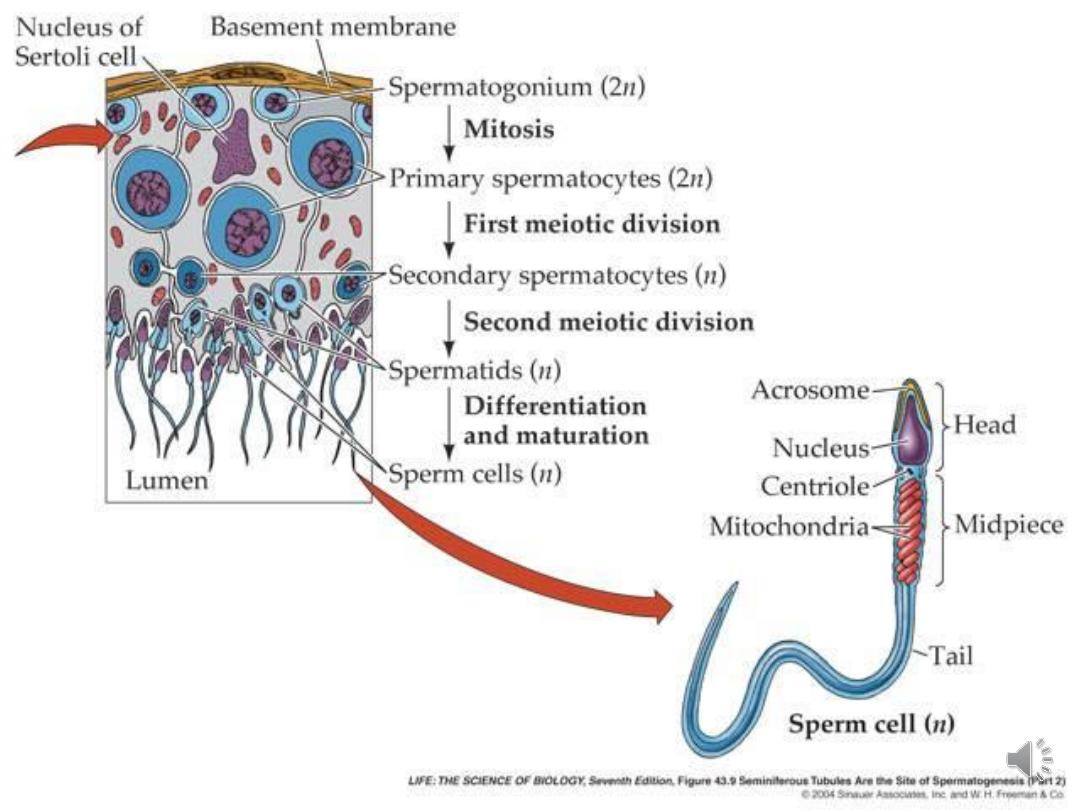
• Spermatogenesis requires testicular growth &
differentiation & it is under endocrine control by
FSH & paracrine control by androgens produced by
LH-stimulated Leydig cells.
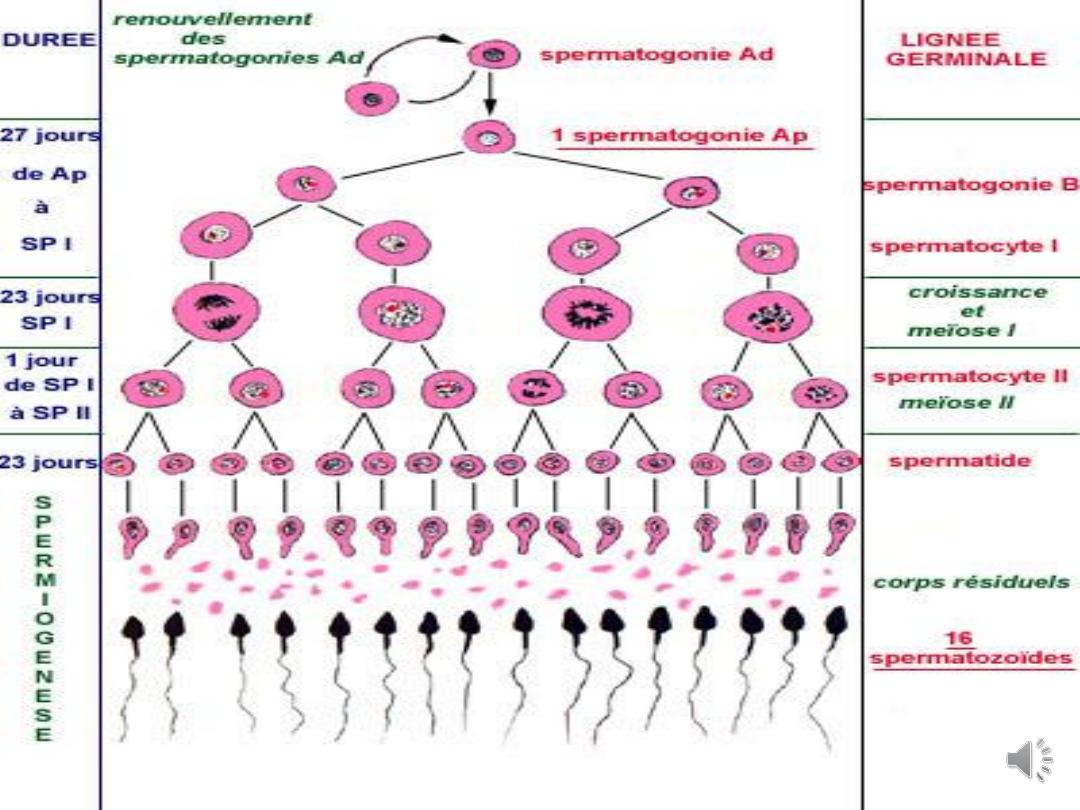
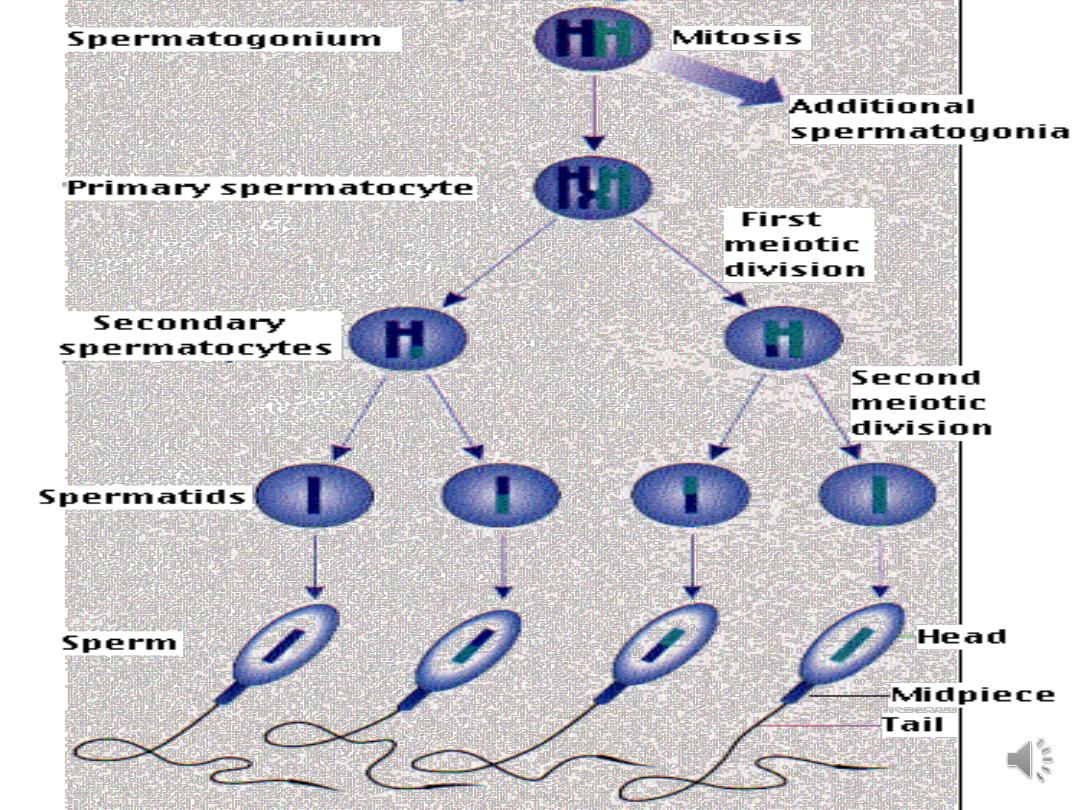
• Spermatogenesis comprises the mitotic division of
spermatogonia & meiotic division of spermatocytes.
• These will develop into spermatids which then
transform into mature spermatozoa in a process
called spermiogenesis.
• The process takes 72 days to complete

Causes of male infertility:
• Disorders of spermatogenesis:
• Increased scrotal temperature
• Orchitis causing damage to sperms
• Genetic causes: aneuploidy of sex chromosomes
(Klinefelter XXY) or structural abnormalities of the
autosomes. Microdeletions of the azoospermic factor
(AZF) regions of the Y chromosome are associated with
low sperm counts and motility
• Drugs
• Impaired Sperm transport:
• Epidydimal malformation
• Inflammation
• Congenital Bilateral Absence of the Vas.
• Ejaculatory dysfunction:
• Anejacualation
• Premature ejaculation
• Retrograde ejaculation
• Impotence
• Other causes:
Immunological factors such as antisperrn
antibodies (IgG or IgA) and general infections
may affect sperm function and lead to
infertility

Assessment of male partner
History
• Duration of infertility
• Fertility in previous relationships
• Previous fertility investigations and
treatment
Medical
• Sexually transmitted infection
• Epididymitis
• Mumps orchitis
• Testicular maldescent
• Chronic disease
• Drug/alcohol abuse
• Recent febrile illness
• Recurrent urinary tract infection
• Herniorrhaphy
• Testicular injury
• Torsion
• Orchidopexy
• Vasectomy and/or
reversal
• Toxic substance exposure
including chemicals,
radiation
• Onset of puberty
• Coital habits
• Premature ejaculation
• Libido/impotence

Examination:
• General, Height, weight, body mass index
• Fat and hair distribution
• Evidence of hypoandrogenism or gynaecomastia
• Groin Exclude inguinal hernia (patient in upright
position)
• Check for inguinal mass, e.g. ectopic testicle
• Examination of genitalia
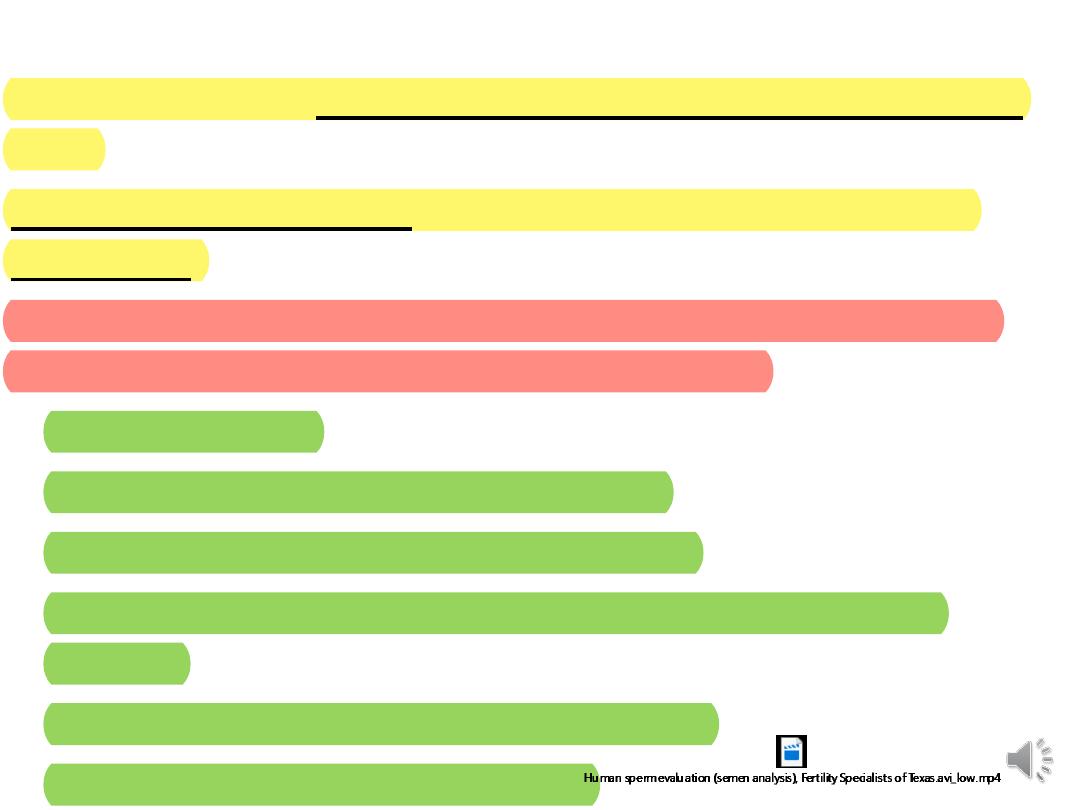
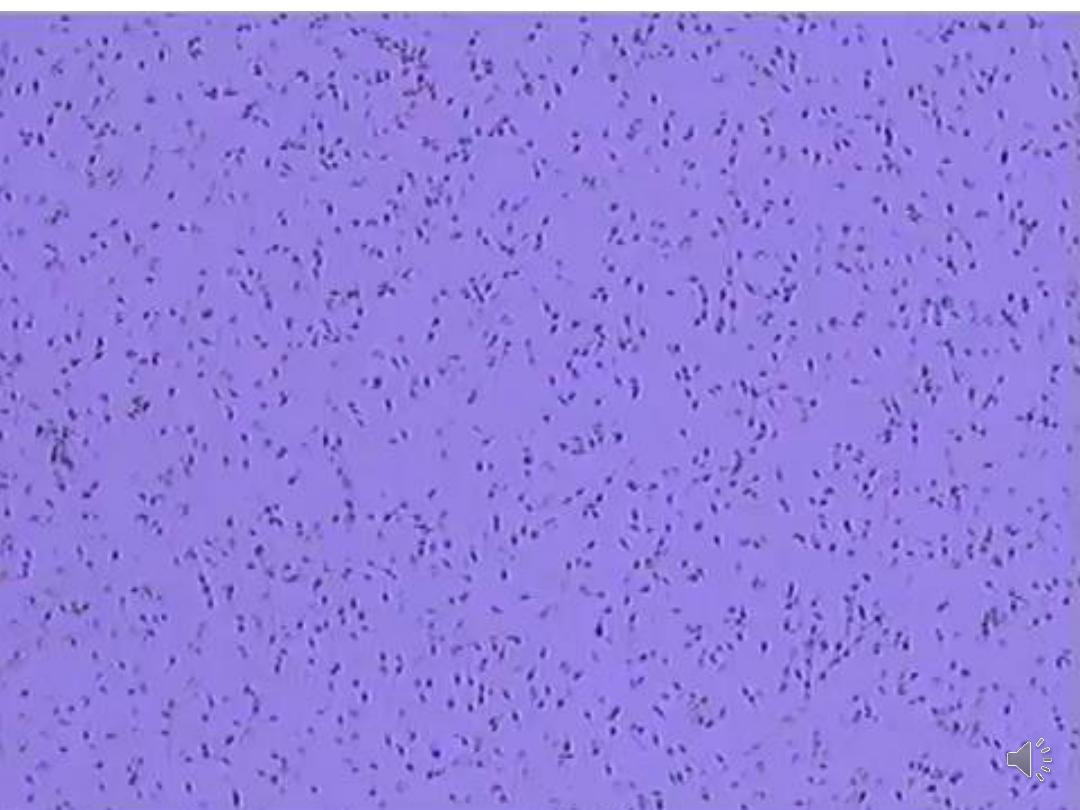
Seminal Fluid Analysis:
the patients have abstained from sexual intercourse for 3–4
days.
Two abnormal test results are required to diagnose male
subfertility.
The World Health Organization (WHO) 2010 has proposed a
set of criteria for normal semen parameters:
• Volume: 1.5 mL
• Liquifaction time: within 30 minutes
• Sperm concentration: ≥ 15 million/mL
• Sperm motility: >32% progressive motility, 40% total
motility
• Sperm morphology: >4% normal forms
• White blood cells: <1million/mL

• Repeat confirmatory tests should ideally be
undertaken 3 months after the initial analysis to
allow time for the cycle of spermatozoa formation
to be completed.
• However, if a gross spermatozoa deficiency
(azoospermia or severe oligozoospermia) has been
detected the repeat test should be undertaken as
soon as possible.

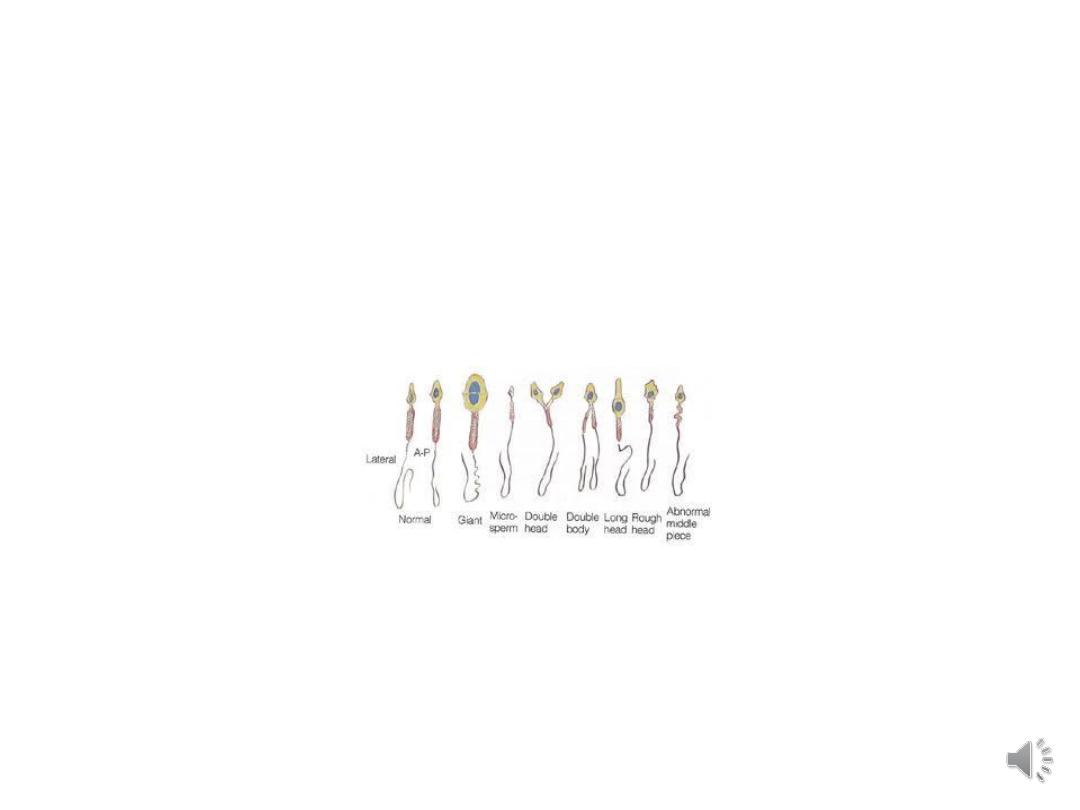
Nomenclature for some semen variables:
• Oligozoospermia: Sperm concentration less than
the reference value
• Asthenozoospermia: less than the reference value
for motility
• Teratozoospermia: less than the reference value for
morphology
• Azoospermia: no spermatozoa in the ejaculate:
o Obstructive
o Non- obstructive
• Aspermia: no ejaculate

Further investigations of male infertility:
• Endocrine tests:
For men with a very low sperm count or
azoospermia, it is important to check their testosterone
levels (low levels suggest a production impairment) and
FSH, LH, Prolactin to differentiate obstructive from non-
obstructive azoospermia, testicular failure may be
associated with symptomatic low testosterone.
• Chromosomal & genetic studies: DNA
fragmentation index & test for cystic fibrosis gene
may be done in certain cases
• Microbiology of semen
• Imaging of male genital tract
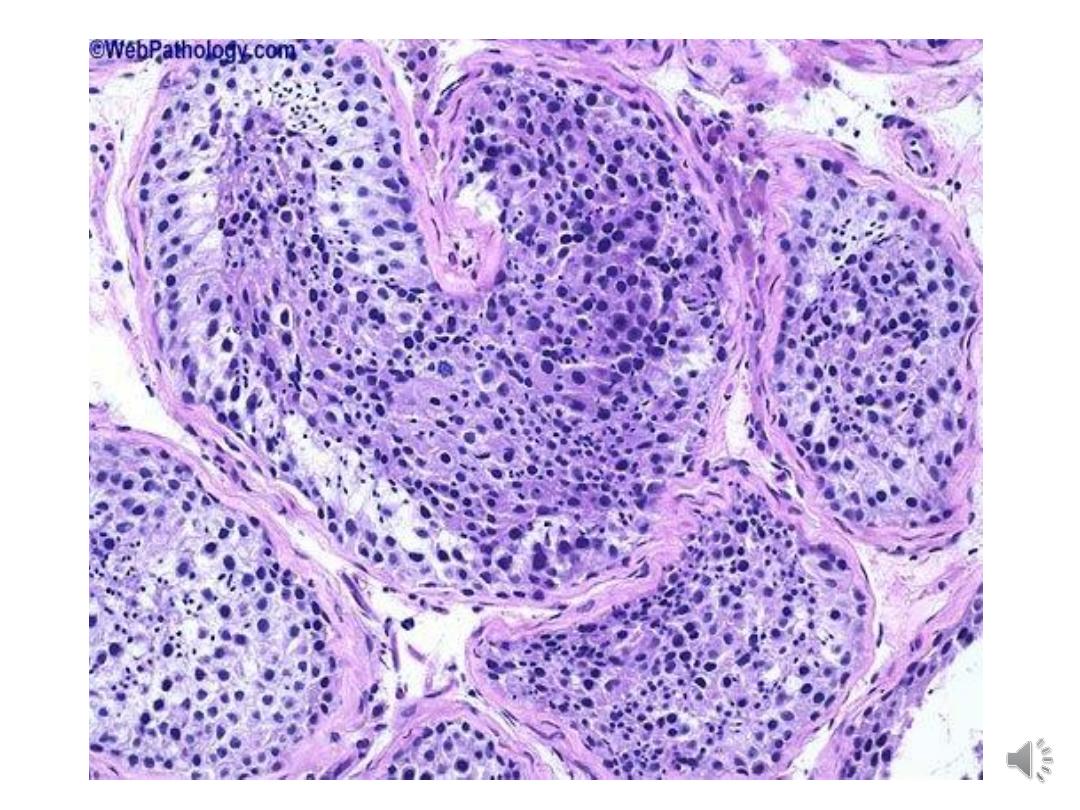
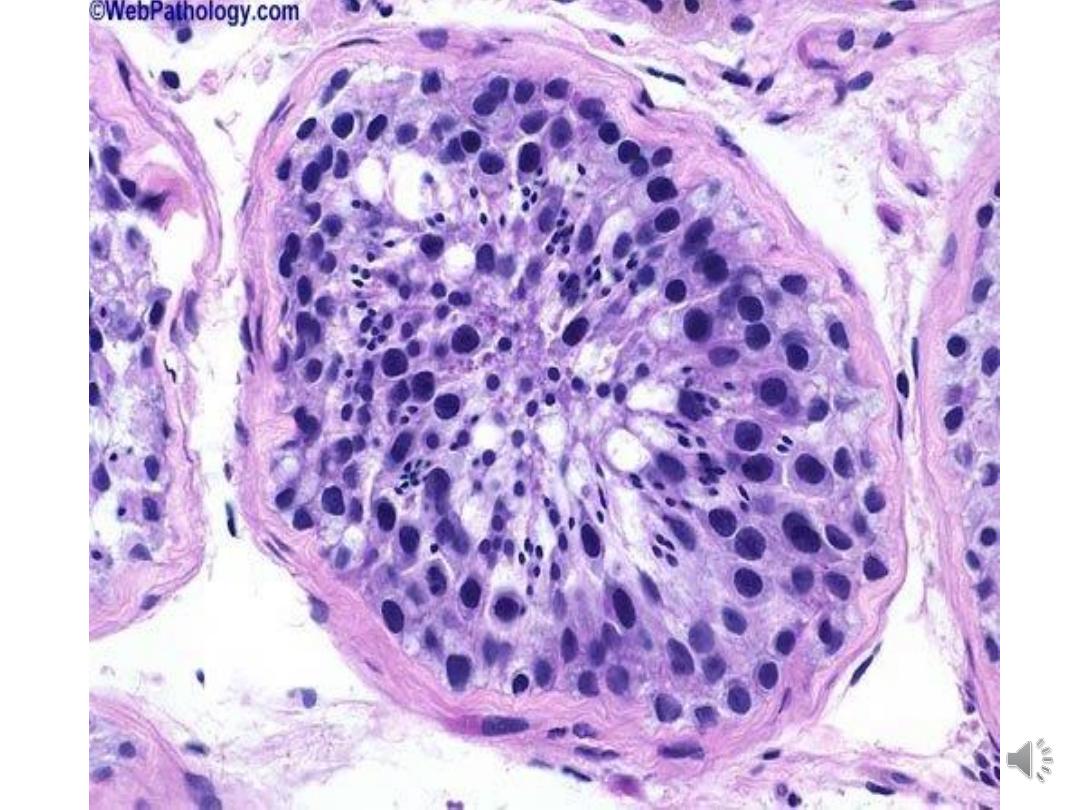
• Testicular biopsy

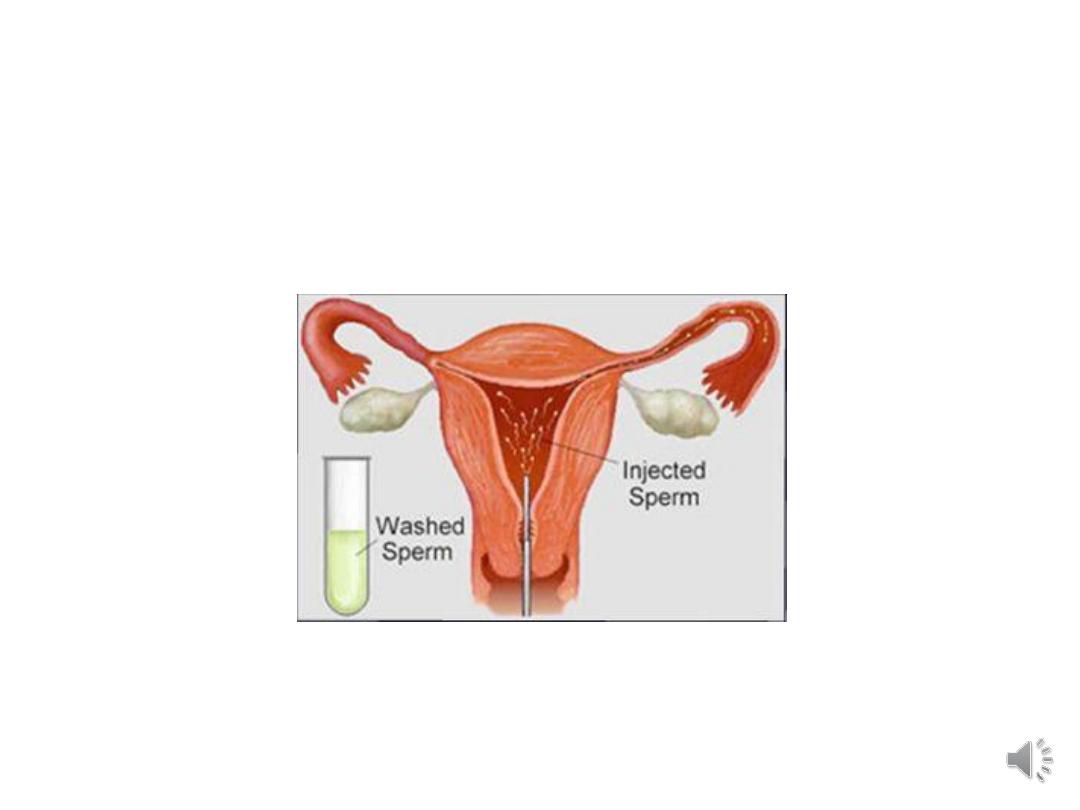
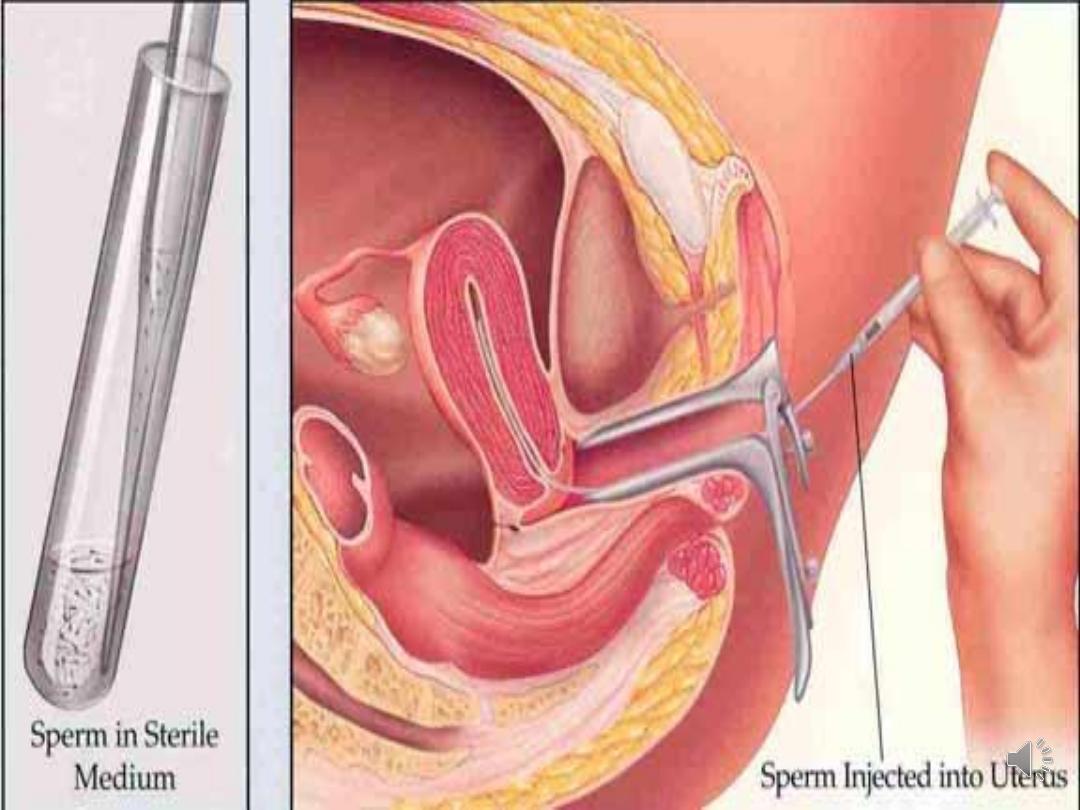
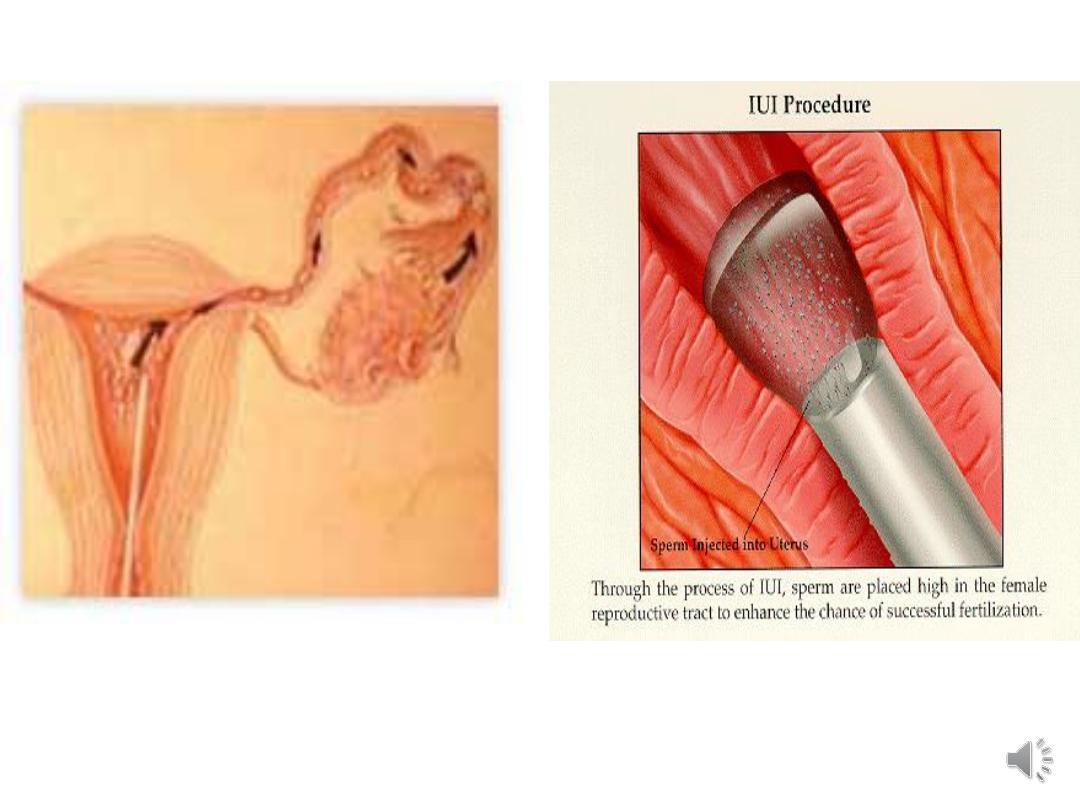
• Intrauterine insemination (IUI):): using washed
sperm with or without controlled ovarian
stimulation considered in cases where semen
parameters show mild or moderate abnormalities.
• In Vitro Fertilization/ Intracytoplasmic Sperm
Injection IVF/ICSI: Where semen parameters are
poor, it may be appropriate to consider IVF
treatment straightaway
Management of male factor infertility


Conventional treatment for male infertility:
• GONADOTROPHINS: Hypogonadotrophic
hypogonadism responds to gonadotrophin
treatment. Administration of FSH and hCG is
effective in achieving an acceptable sperm count in
80% of men
• SURGICAL TREATMENT: in case of varicocele or
hydrocele
• EJACULATORY FAILURE:
Sildenafil: erectile dysfunction
Alpha-agonists and anticholinergic drugs:
retrograde ejaculation
