ASSISTED CONCEPTION
TECHNIQUES
Dr.Nadia Mudher Al-Hilli
FICOG
Department of Obs&Gyn
College of Medicine
University of babylon

Objectives
• Know the indications of IVF
• Understand the steps of IVF
• Learn about ovarian hyperstimulation
syndrome & its management

•
In vitro
fertilization and embryo transfer
(IVF-ET) involves the fertilization of
gametes in the laboratory and transfer of
embryos to the uterus.

• There are a number of related techniques that are
carried out to overcome barriers to enhance
fertilization:
• Intracytoplasmic sperm injection (ICSI)
• Testicular biopsy
• Percutaneous epidydimal sperm aspiration (PESA)
• Donor Insemination (DI)

Indications of IVF include:
• Tubal damage
• Unexplained infertility
• Severe endometriosis
• PCOS
• Moderate & severe male factor:
non-obstructive azoospermia
obstructive azoospermia
• Unsuccessful IUI

The success rate of IVF per cycle is about 30 per cent
in women under 35 years of age.
Typical IVF-ET cycle:
I. Initial consultation and tests:
Assess the cause of infertility, explain the procedure,
side effects, complications and success rates.
An assessment of ovarian reserve by antimullarian
hormone AMH, FSH, estradiole & ultrasound measure
of antral follicle count.

II. Pituitary down regulation : To prevent the
risk of spontaneous LH surge necessitating
unplanned oocyte collection. Using GnRH
analogues, different protocols are available
using agonist or antagonist drugs according to
patient characteristics.
III. Ovarian stimulation: FSH (either recombinant
or urinary) or human menopausal gonadotrophins
injections :
try to get about 8-10 eggs (18 mm)
IV. Ovulation trigger with hCG : 5000-10000 IU
V. Oocyte collection is carried out 34-36 hours after
hCG administration
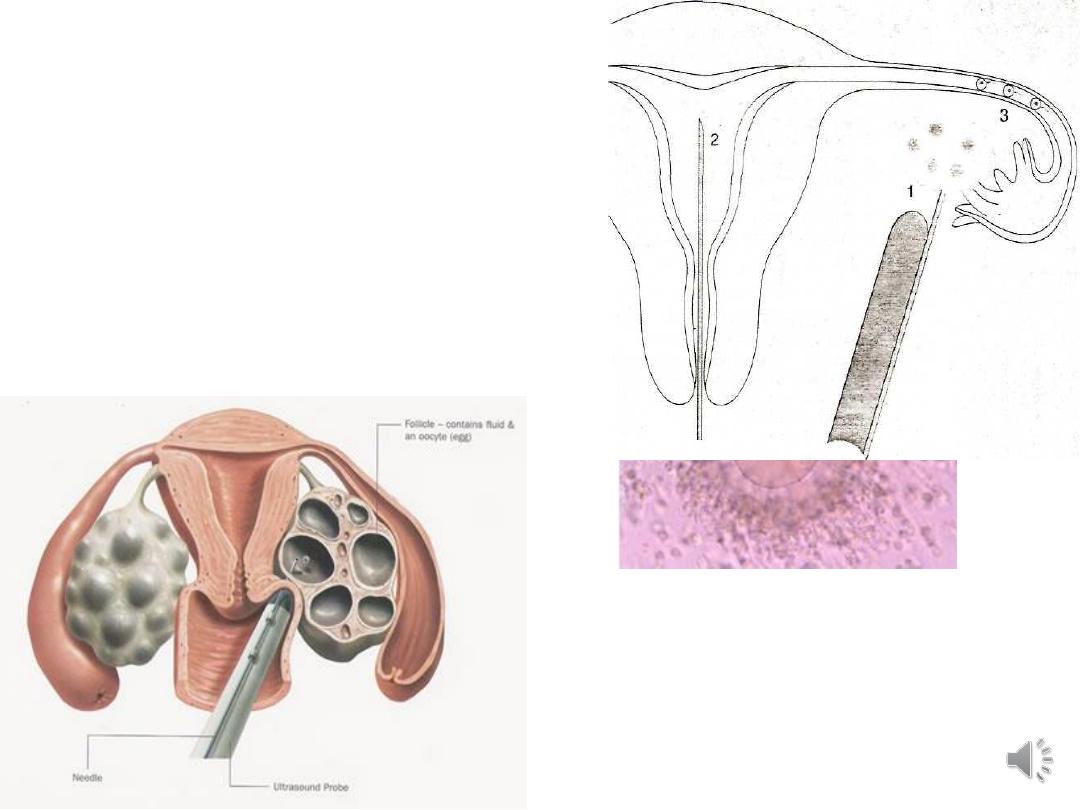
Oocyte collection:
the eggs are collected
using q an ultrasound
guided procedure via
a very fine needle.
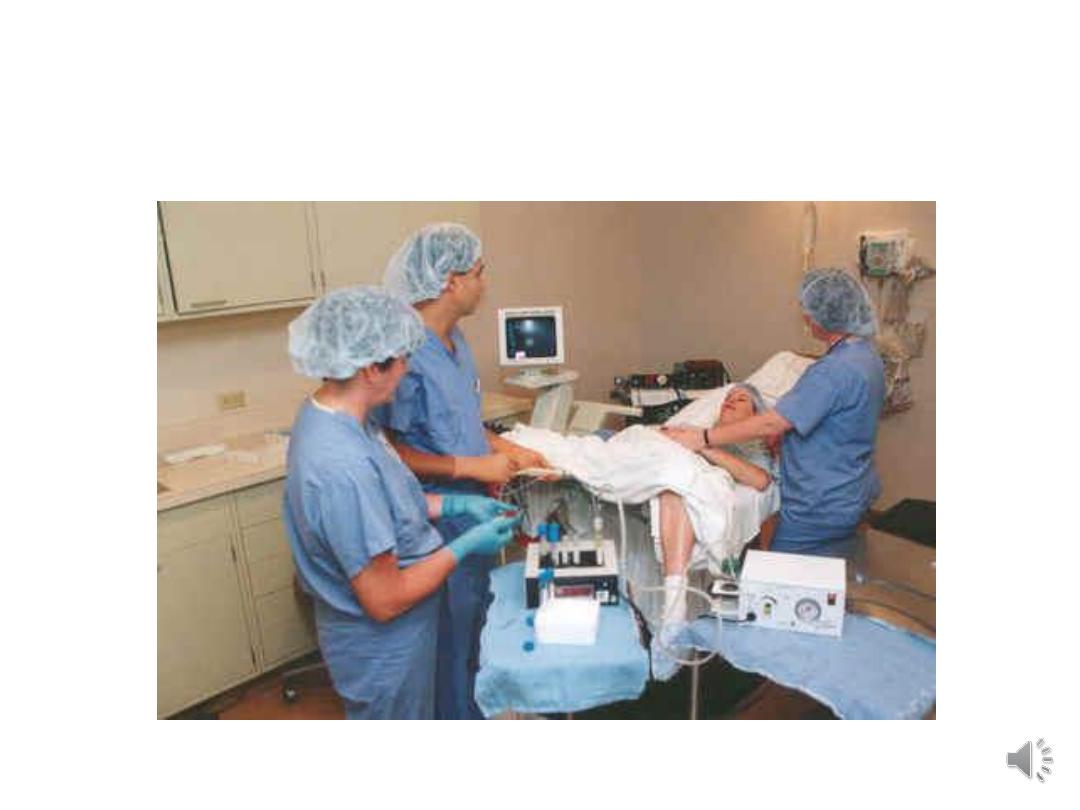
Egg retrieval
VI. Semen preparation
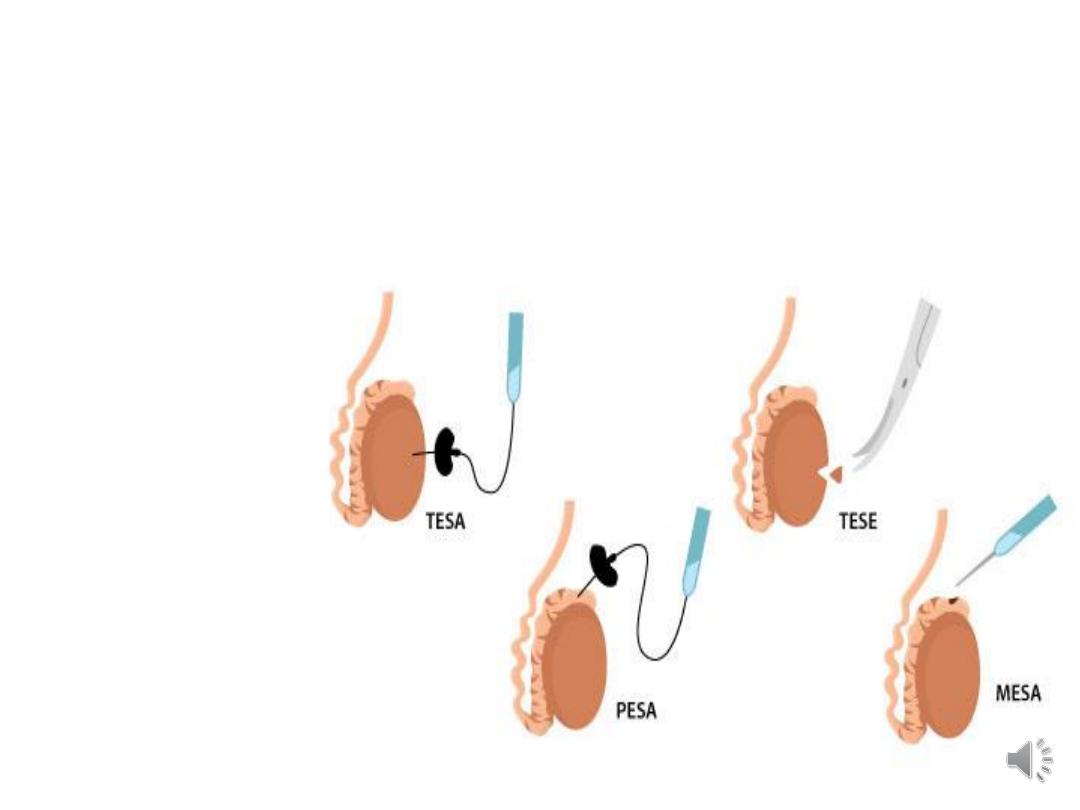
Sperm aspiration techniques :
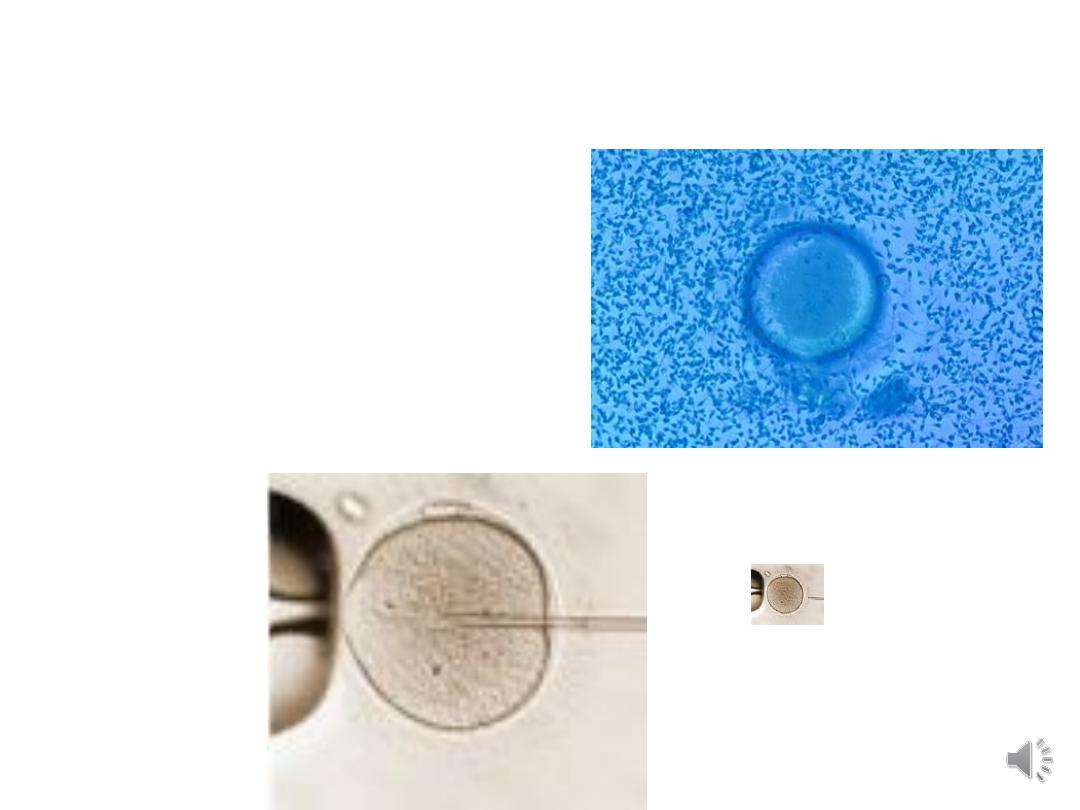
VII. Insemination :
Conventional IVF or
ICSI

VIII. Fertilization and
embryo cleavage:
. Embryos
are graded microscopically from I to
IV, with I being excellent and IV
being poor.
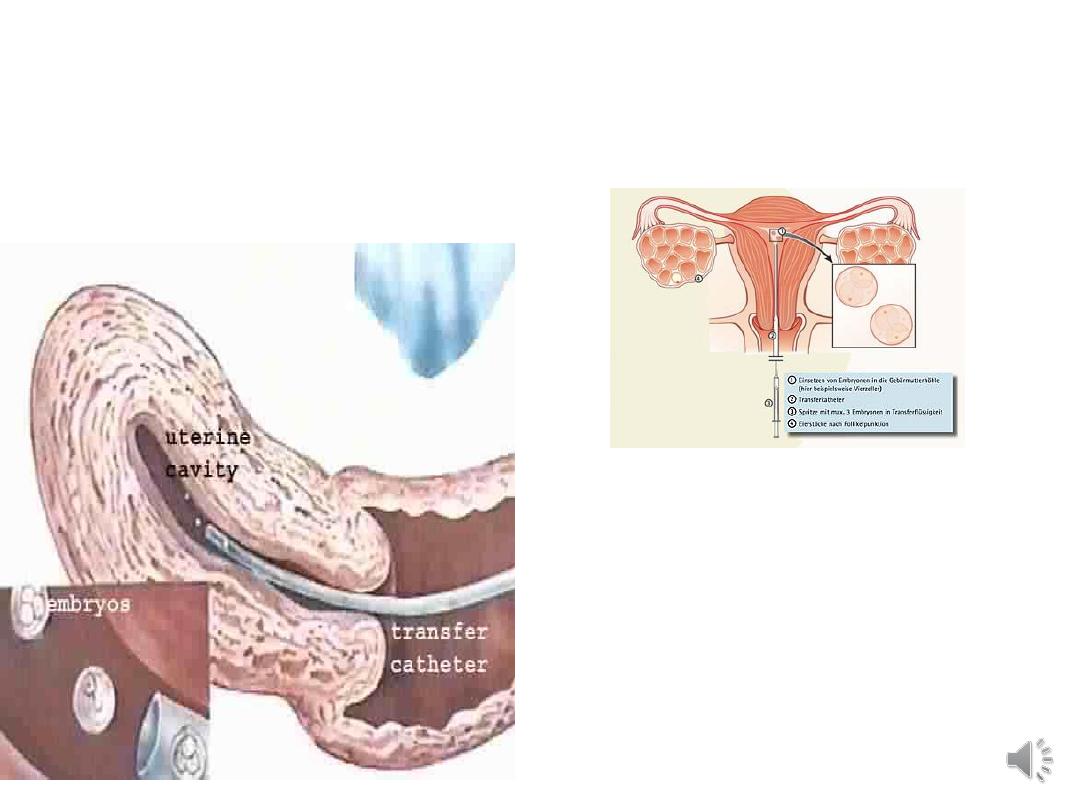
IX. Embryo transfer:
Embryos are normally
transferred to the uterus 2-5 days after oocyte collection.

Embryo cryopreservation

X. Luteal support and establishment of
pregnancy:
supported by progesterone
transvaginal.with or without im injections
• A blood test for hCG is performed 14 days
after embryo transfer.
Complications of IVF treatment
• Ovarian hyperstimulation syndrome
• multiple pregnancy
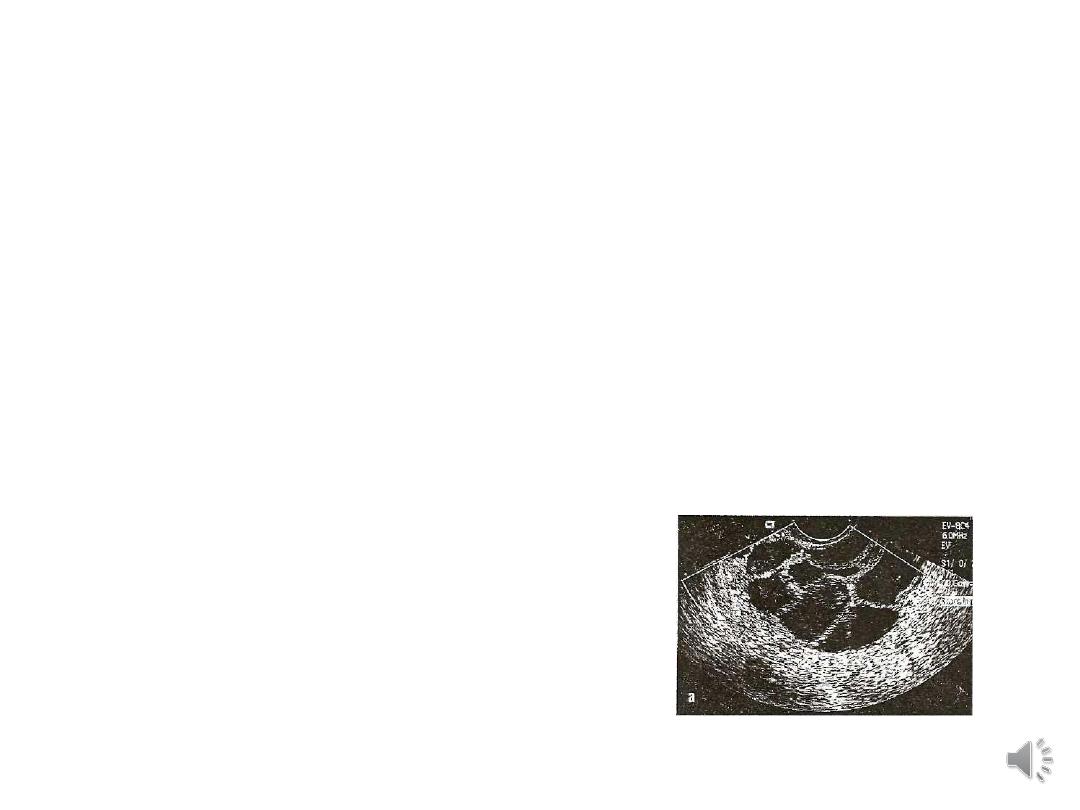
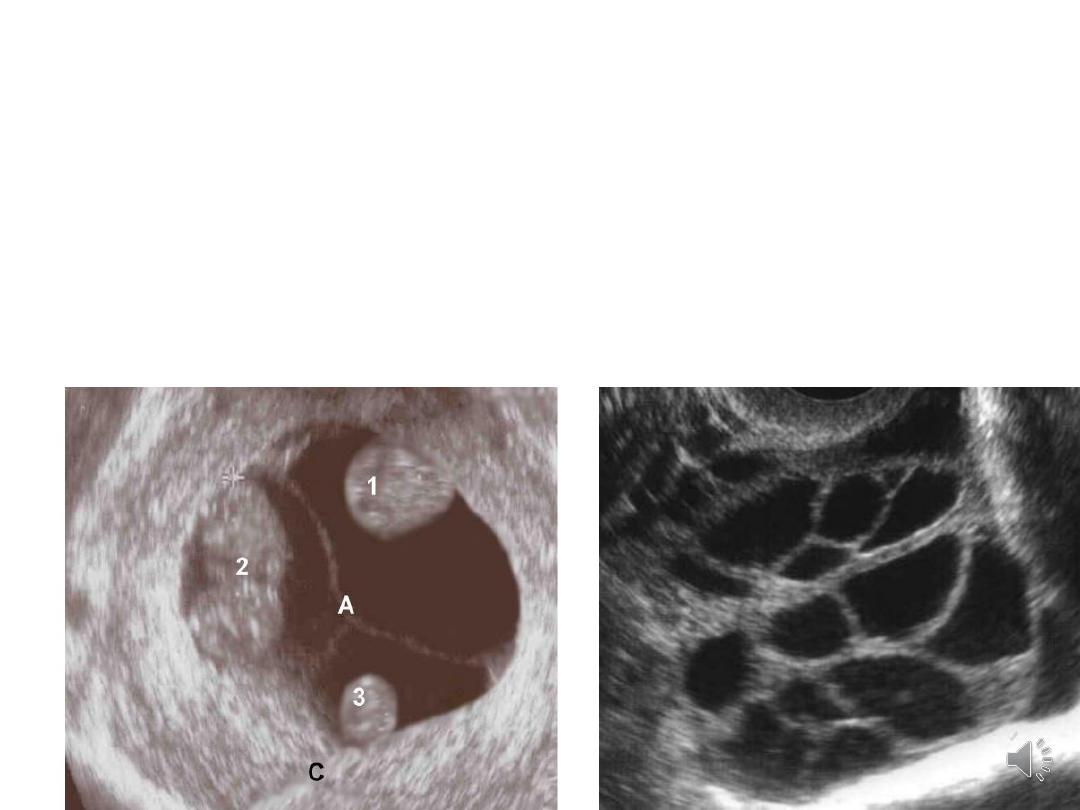
Ovarian hyperstimulation syndrome
• This syndrome is characterized by ovarian
enlargement due to multiple
and
an acute fluid shift into the extravascular
space.
• Complications of OHSS include ascites,
hemoconcentration, hypovolemia, and
electrolyte imbalances.

• OHSS is a systemic disease resulting from
vasoactive products released by
hyperstimulated ovaries
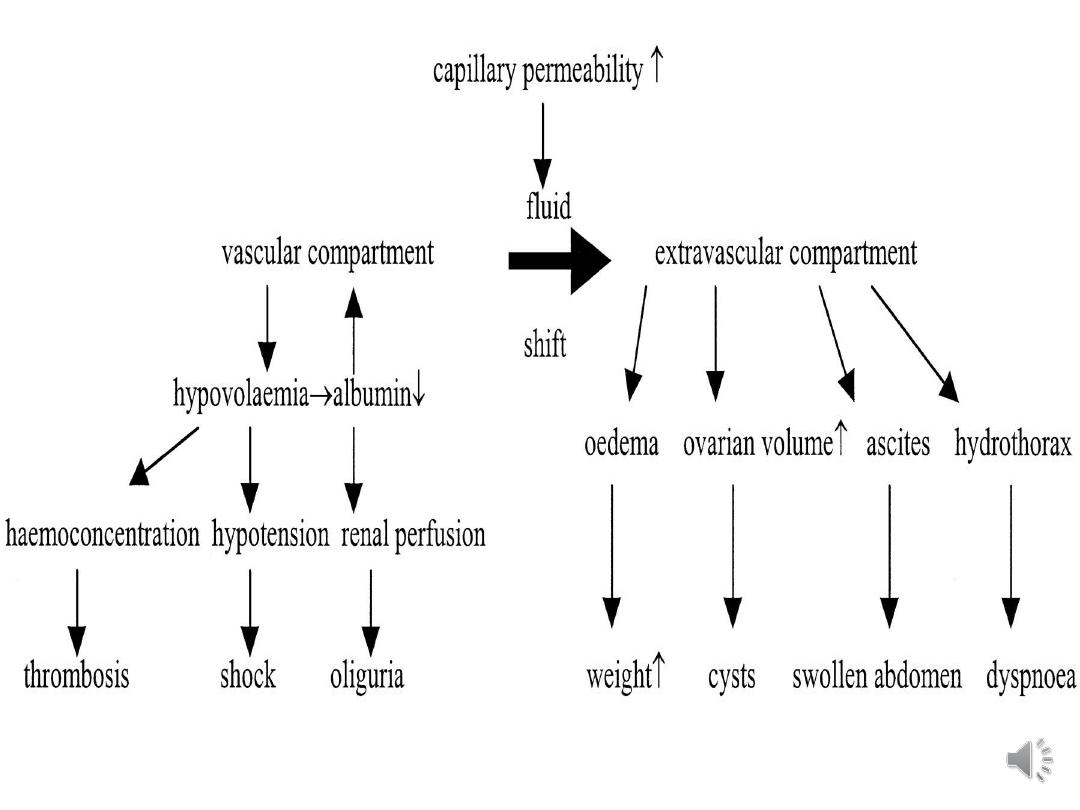
The pathophysiology:
• increased capillary permeability,
• leakage of fluid from the vascular
compartment
• third space fluid accumulation
• intravascular dehydration

• Incidence:
• mild forms of OHSS affect up to 33% of in vitro
fertilisation (IVF) cycles
• moderate or severe OHSS affect 3–8% of IVF
cycles
Diagnosis of OHSS
• history of ovarian stimulation, mostly by
gonadotrophins, followed by the typical symptoms
of abdominal distension, abdominal pain, nausea
and vomiting.
Differential diagnoses:
• complication of an ovarian cyst (torsion,
haemorrhage)
• pelvic infection
• intra-abdominal haemorrhage
• ectopic pregnancy
• appendicitis

Assessing severity and reporting
adverse outcomes
• Women with OHSS should have the severity of
their condition assessed and documented as an aid
to management.
• Mild OHSS:
• Abdominal bloating
• Mild abdominal pain
• Ovarian size usually <8 cm3
• Moderate OHSS:
• Moderate abdominal pain
• Nausea ± vomiting
• Ultrasound evidence of ascites
• Ovarian size usually 8–12 cm*

• Severe OHSS:
• Clinical ascites (occasionally hydrothorax)
• Oliguria
• Haemoconcentration, haematocrit >45%
• Hypoproteinaemia
• Ovarian size usually >12 cm
3
• Critical OHSS:
• Tense ascites or large hydrothorax
• Haematocrit >55%
• White cell count >25 000/ml
• Oligo/anuria
• Thromboembolism
• Acute respiratory distress syndrome

• OHSS classified into ‘early’and ‘late’,depending
on the time of onset, determine the prognosis.
• OHSS presenting within 9 days after the
ovulatory dose of hCG is likely to reflect excessive
ovarian response and the precipitating effect of
exogenous hCG.
• OHSS presenting after this period reflects
endogenous hCG stimulation from an early
pregnancy. Late OHSS is more likely to be severe
and to last longer than early OHSS.

Treatment
• mild & moderate OHSS: can be managed on an
outpatient basis.
• Analgesia: paracetamol or codeine . Nonsteroidal
anti-inflammatory drugs should not be used.
• Women encouraged to drink to thirst, rather than
to excess.
• Strenuous exercise and sexual intercourse should
be avoided for fear of injury or torsion of
hyperstimulated ovaries.
• continue progesterone luteal support but hCG
luteal support is inappropriate.

• Severe OHSS: Hospital admission should be
recommended & observation until resolution of the
condition.
• Critical OHSS should prompt consideration of the
need for intensive care.

• Strict fluid balance: Allowing women to drink
according to their thirst
• Paracentesis : if distress due to abdominal
distension or if oliguria persists despite adequate
volume replacement.
• Intravenous colloid replacement if large volumes of
ascitic fluid drained.
• Thromboprophylaxis should be provided for all
women admitted to hospital with OHSS.
• Pelvic surgery should be restricted to cases with
adnexal torsion
