
Contraception & Sterilization
D

LEARNING OBJECTIVES
• • Understand the mechanism of action of
current contraceptive methods.
• • Describe factors that affect contraceptive
effectiveness.
• • Understand the non-contraceptive benefits
of methods.
• • Remember the use of medical eligibility
criteria for contraception.

The ideal form of contraception would be 100%
effective, completely reversible, totally acceptable
& absolutely free of side effects.
No such method exists.
Assessment of effectiveness by Pearl index: is the
number of unwanted pregnancies which occur in
100 women using that method for a year.

Effectiviness
• Method typical use perfect use
• 1. no method 85 85
• 2.fertility-awareness 24 0.4-0.5
• 3.male condom 18 2
• 4. diaphragm 12 6
• 5. progesterone-only pill 9 0.3
• 6. combined hormonal contraception 9 0.3
• 7.progesterone-only injectable 6 0.2
• 8.copper IUD 0.8 0.6
• 9.LNG-IUS 0.2 0.2
• 10. progesterone –only implant 0.05 0.05
• 11.female sterilization 0.5 0.5
• 12.vasectomy 0.15 0.1

Definition of UKMEC categories
• UKMEC Definition of category
• 1 A condition with no restriction for the use of the
contraceptive method.
• 2 A condition where the advantages of the
contraceptive method generally outweigh the
theoretical or proven risks.
• 3 A condition where the theoretical or proven risks of
the contraceptive method outweigh the advantages.
Expert clinical judgement and/or referral to a specialist
contraceptive provider is recommended.
• 4 A condition which represents an unacceptable
health risk if the contraceptive method is used.

1-Methods not requiring medical consultation:
A-Coitus interrupts:
• Withdrawal of penis at the moment before
ejaculation. It causes psychological symptoms
in both couples. Failure rate is high,.
• Failure rates of about 10 per 100 WY
• Failure occurs from delay in withdrawal or
because the pre-ejaculatory fluid may contain
some spermatozoa

B-Condom:
It has the advantages: that is readily available in
most societies, does not need medical
supervision & provides protection against
sexually transmitted diseases.Occasional
failures occur because the sheath is defective,
or because it is not worn in the earlier phases
of coitus.Recently female condom is
polyurethane sheath inside the vagina,
protect against sexual transmitted disease.

Fertility awareness-based methods (FAB)
C-Safe period (rhythm or calendar method):
The method is based on the assumption that
the ovum is capable of being fertilized for only
24 hours after its release, & that the sperm
can fertilize the ovum for only 72 hours after
they are deposited in the vagina. If ovulation
occurs between days 12-16 of a 28 day cycle;
the fertile period during which coitus should
be avoided between day 9= (12-3) & day 17=
(16+1) of the cycle.

Calendar method; relies on an analysis of the
women’s menstrual data over the preceding 6
months.
• First fertile day = shortest cycle minus 20
• Last fertile day = longest cycle minus 10
This method of contraception is not suitable for
women with very irregular periods.
Temperature method
An attempt may be made to predict the time of
ovulation by recording the basal body temperature
first thing in the morning, coitus is avoided for 72
hours after the rise in temperature has occur (0.2–
0.4C).

Cervical mucus method
• Few women able to determine the changes in her cervical
mucus secretion (increase secretion of clear, slippery &
stretchable cervical mucus can be detected in the vagina on
the days preceding ovulation.
• Cervical palpation
• At midcycle, the cervix rises 1–2 cm and feels softer and
moist.
• Personal fertility monitor
• This hand-held monitor analyses diposable urine dipsticks .
ovulation kits are available for detecting the LH surge in the
urine 36 hours before ovulation. A red light indicates fertile
phase (risk of conception) and green, infertile.
The safe period has a high failure rate; pearl index is 20-40.
D- Spermicides:
• These are chemical substances placed in the vagina
before coitus, which kill the spermatozoa. They are
prepared as pessaries, cream, or foams. When used
alone they give very poor results , but they are
often used in conjunction with a mechanical barrier
such as a diaphragm or condom. The method is
simple, not need medical supervision. It sometime
causes soreness or irritation to one or other
partner.
• Some data have suggested that frequent use of N-9
might increase the risk of HIV transmission.

E-Vaginal tampons:
A disposable sponge impregnated with the
spermicidal as nonoxynol- 9 used in the upper
vagina as a barrier to sperm penetration of
the cervix.

2-Methods requiring medical supervision:
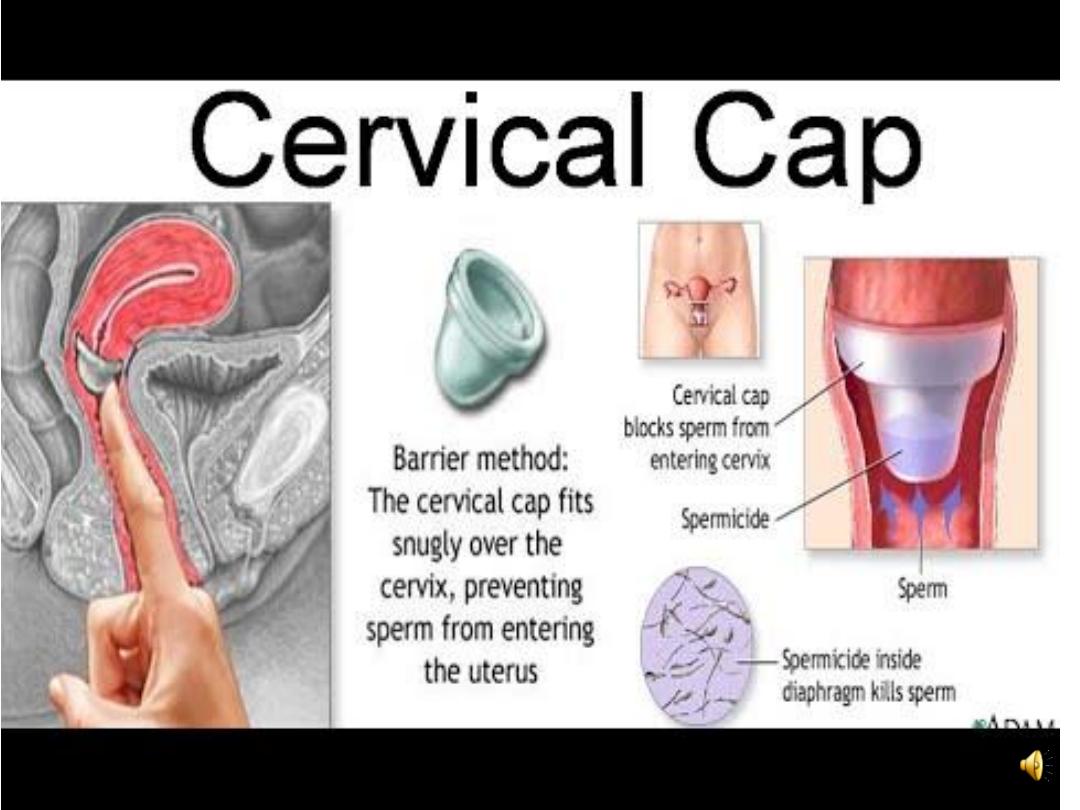
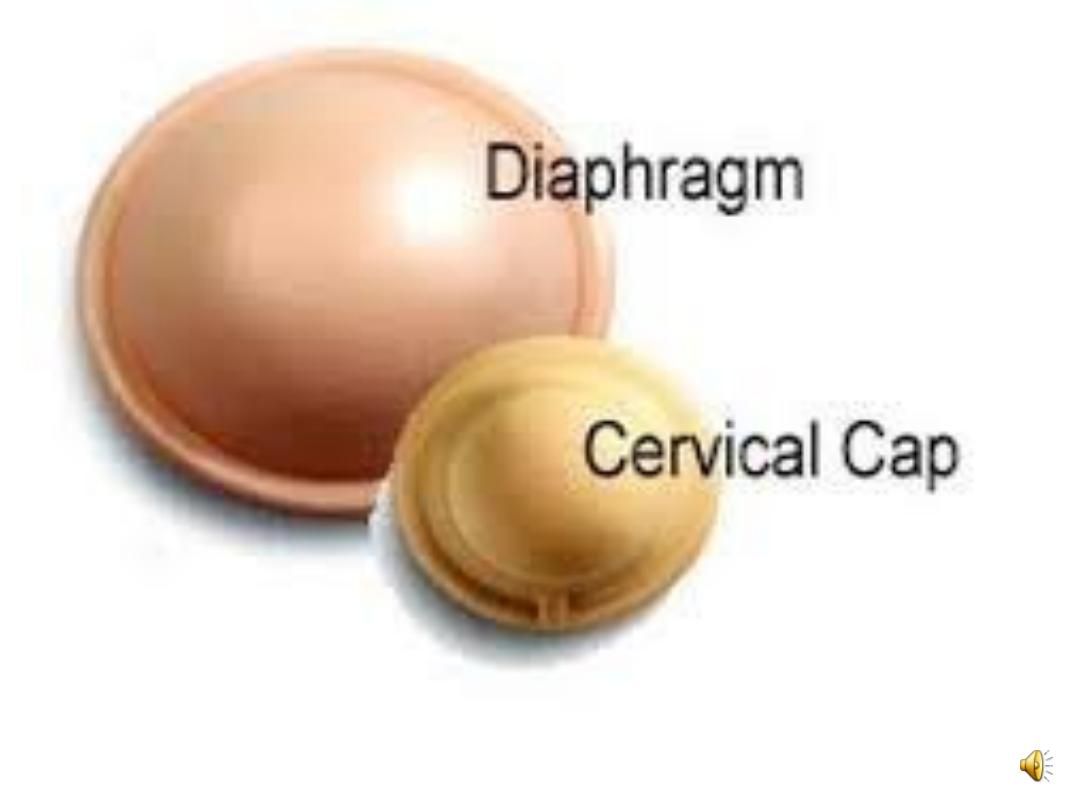
• A-Vaginal diaphragm & cervical cap:
• These are latex or non-latex devices that are inserted
into the vagina to prevent passage of sperm to the
cervix
The vaginal diaphragm is made in various sizes. They are
used in conjunction with spermicide. The diaphragm is
inserted before coitus, & should not be taken out for at
least 6 hours afterwards, so that the spermicide will kill
any spermatozoa before it is removed.
Disadvantages: it is coitally related. The only
contraindication to use of diaphragm is occurrence of
uterine prolapsed.
Cervical caps are not widely used as the diaphragm. It is
cup-shaped rubbed cap which fits over the cervix.

Diaphragm and cap
• Disadvantages
• are that women need to be taught how to insert
and remove the device
• and typical failure rates in the region of 18% are
reported.
• In some women their use may be associated with
increased vaginal discharge and urinary tract
infections.


B- I.U.C.D: 3 types
1-inert devices such as lippes loop.
2-devices with various applications of copper
designed to increase effectiveness & decrease
surface area &so decrease side effects particularly
the menorrhagia & dysmenorrheal e.g. copper T &7
& now Multiload & Nova T.
3-Medicated I.U.C.D releasing low concentrations of
progesterone or norgestrel e.g
• The 52 mg LNG-IUS (Mirena®) . levonorgestril
available in U.K in 1995 release 20 ug levonorgestrel
/day & lasting for 5 years, advantage is menstrual
blood loss is very substantially reduced 90% at 1
year.
• and the 13.5 mg LNGIUS
• (known as Jaydess) is licensed for 3 years for
contraceptive use.
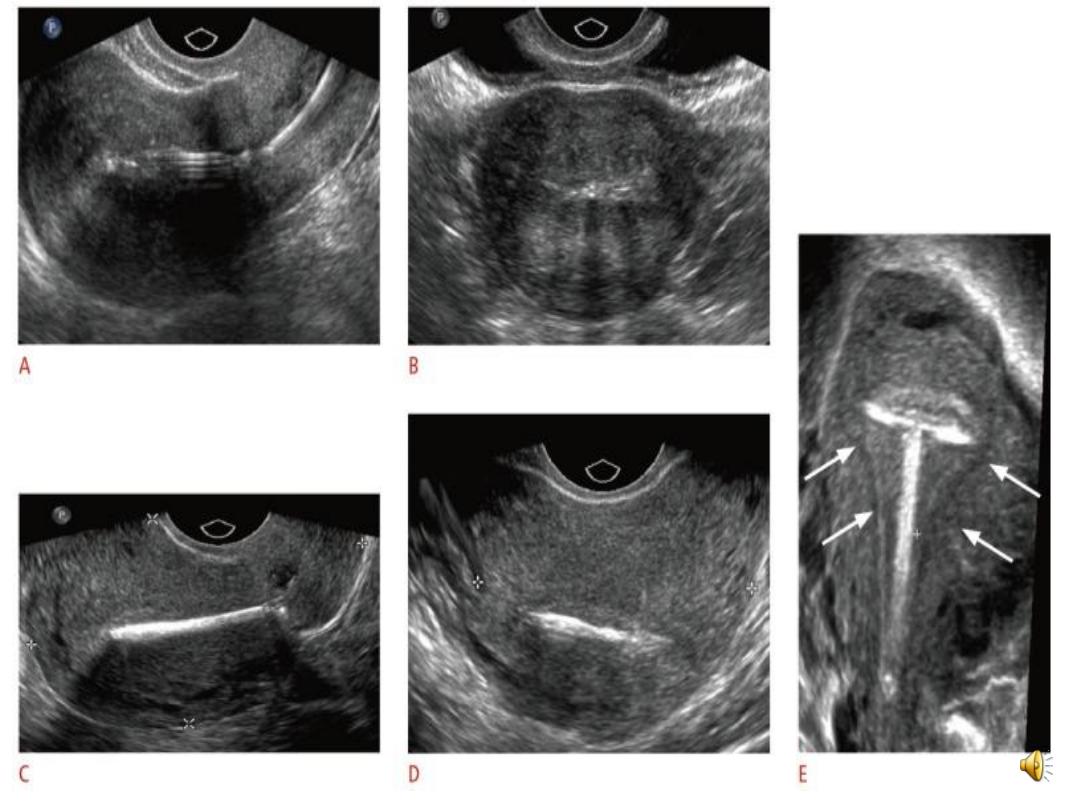

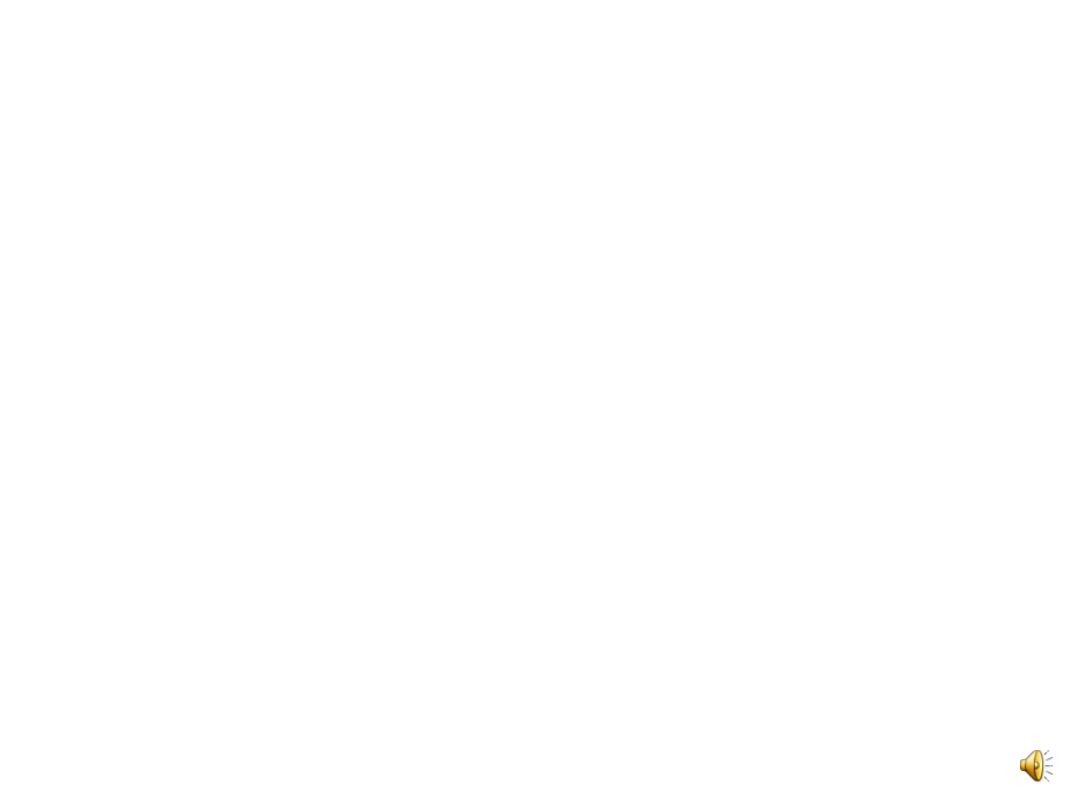
Displaced iucdwith early pregnancy
Perforated iucd

• Mechanism of action:
• IUDs work by inhibiting fertilisation by direct
toxicity . An inflammatory reaction within the
endometrium can also have an anti-implantation
effect. Copper is toxic to the ovum and the sperm
and the copper content of the cervical mucus
inhibits sperm penetration as well
• . LNG-IUS works primarily by its effect on the
endometrium, which prevents endometrial
proliferation and implantation. Its progestogenic
effect on thickening the cervical mucus also
• impedes entry of sperm The LNG-IUS does not
prevent ovulation.

• The Cu-IUD duration of use is between 3 and 10
years, depending on the device used and age of
woman at insertion. If a woman has a Cu-IUD
inserted at 40 years or above, it can be left
in situ
until the
menopause.
• For women who have a 52 mg LNG-IUS inserted at
45 years or over, the device can be left for
contraceptive purposes until the menopause.

Non-contraceptive health benefits of LNG-IUS (52 mg)
• Heavy menstrual bleeding
• Endometriosis
• Adenomyosis
• Dysmenorrhoea
• Endometrial protection
• Simple hyperplasia

Contraindications:
1-pregnancy.
2-multiple fibroids.
3-congenital uterine abnormality.
4-acute or sub acute PID or active vaginal
inflammation.
5-ca. of the cervix or of body of uterus.
6-valvular heart disease (risk of bacterial
endocarditic).

7-abnormal uterine bleeding.
8-known allergy to copper if a copper IUCD
is being chooses.

Insertion:
An IUD can be fitted at any point in the cycle provided
there is no risk of pregnancy.
Postpartum insertion; should be delayed 8 weeks to
decrease the risk of expulsion & perforation
especially in lactating woman.
IUD can be inserted immediately after abortions;
although expulsion rates may be higher in second
trimester abortion.
Efficacy; during first year after insertion between 2-
3% of women will conceive. Levonorgestril is more
effective 0.1.

Side effects:
1-Menstrual disturbances: the effects of IUD on the
endometrial particularly. The local PGs tens to
cause increase menstrual bleeding &
dysmenorrheal. Also IUD may cause irregular
bleeding. In contrast the levonorgestril IUD
decrease the blood loss.

2-Perforation; usually occur at the time of insertion;&
it is often unnoticed . It is about 1:1000 & most
frequently is through the uterine fundus. It should
be suspected when at the routine follow up (6
weeks later) there e is absence of the thread (other
2 possibilities is either expulsion of the device or it
is rotated within uterine cavity). Pelvic u/s or x-ray
will help to localize the device. Intraperitoneal
devices can be recovered through laparoscope or
sometime laprotomy.

3-expulsion; rate vary from 1-20 women, most
commonly in the first 3 months of use.
• 4-ectopic pregnancy; women using IUD has 80%
decrease in the risk of ectopic pregnancy compared
with women not using contraception.but if
pregnancy occur with IUCD more likely it is ectopic
pregnancy.
• The ectopic pregnancy rate for Cu-IUD users is 0.02
per 100 WY (0.3–0.5 per 100 WY for those not using
contraception)
5-pelvic infection; infection is most likely to occur
during the 20 days following insertion
Actinomycosis occur more with IUCD.

-pregnancy with IUCD in place; increase risk of
about 3 x & removal of IUCD will decrease the
risk of abortion. If the IUCD left in place there
is slight risk of intrauterine infection, preterm
labour,second trimester miscarriage &APH,
but most pregnancies are uncomplicated &
the device is delivered with the placenta.
