
بسم هللا الرحمن الرحيم
Respiratory medicine
3ed lecture

RESPIRATORY FAILURE
Objectives
• Familiar with R F
• Causes of R F.
• Clinical presentation of R F.
• Management of R F.
• To know the epidemiology ,etiology,
pathogenesis ,clinical presentation, investigation
,diagnosis ,treatment ,complication ,prognosis

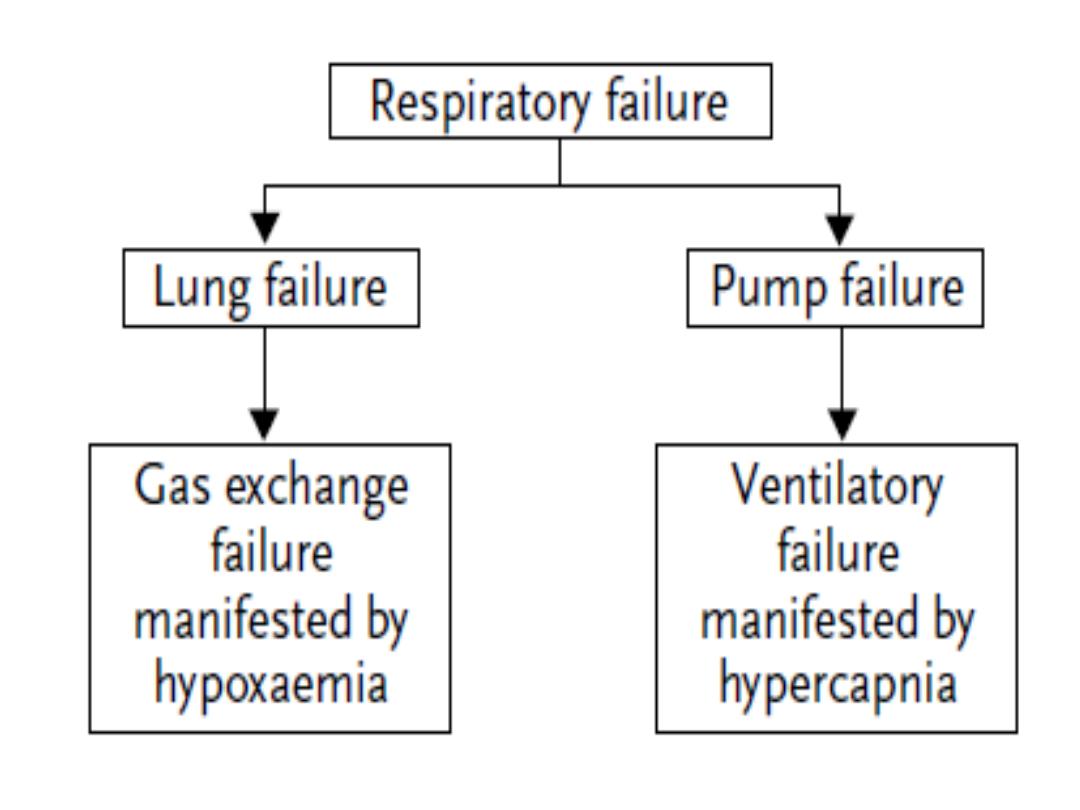
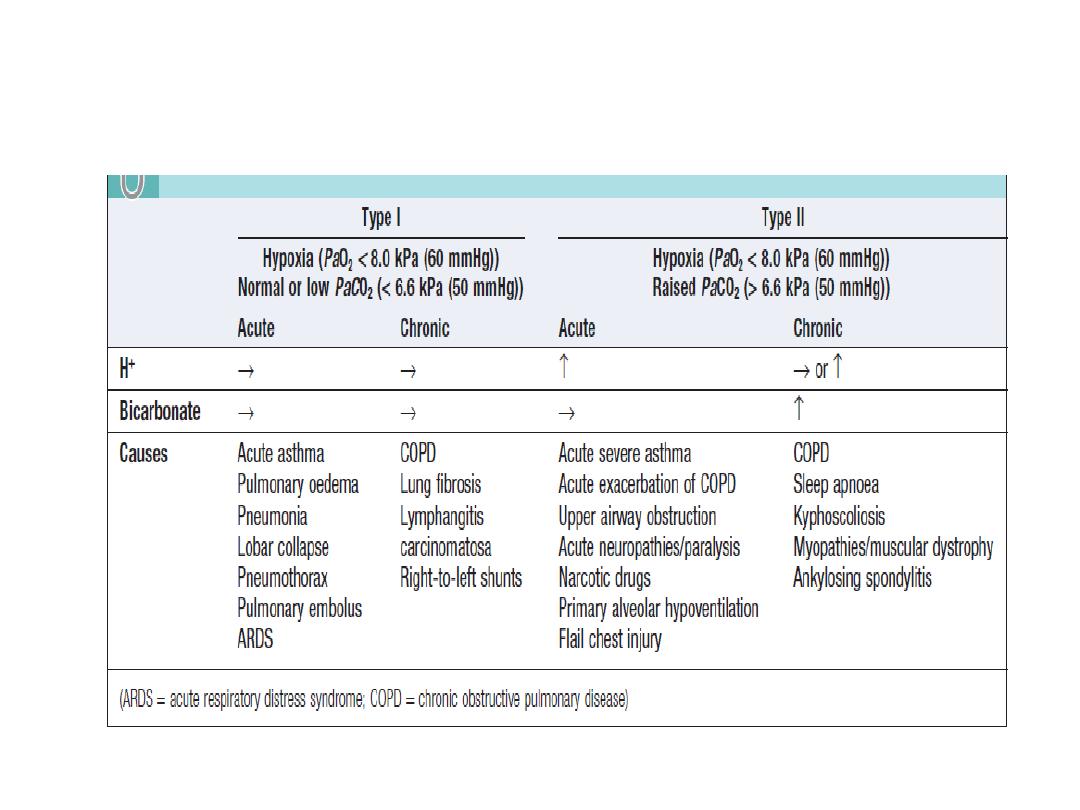
Respiratory failure
• The term respiratory failure is used when
pulmonary gas exchange fails to maintain
normal arterial oxygen and carbon dioxide
levels.
• Its classification into types I and II relates to
the absence or presence of hypercapnia
(raised PaCO
2
).

1. Hypoxemic Respiratory Failure
• The hallmark of this type of respiratory failure is the inability to
adequately oxygenate the blood.
• The main pathophysiologic mechanisms involved are
1.
V/Q mismatch (response to 100 % O2)
2.
intrapulmonary shunting (no significant improvement with 100 % O2).
PRESENTATION :
The rapid shallow breathing pattern
a low or normal PaCO2.
This form of respiratory failure is commonly the result
1.
diffuse acute lung injury with high-permeability
2.
pulmonary edema (ARDS),
3.
severe pneumonic infiltrates,
4.
cardiogenic pulmonary edema
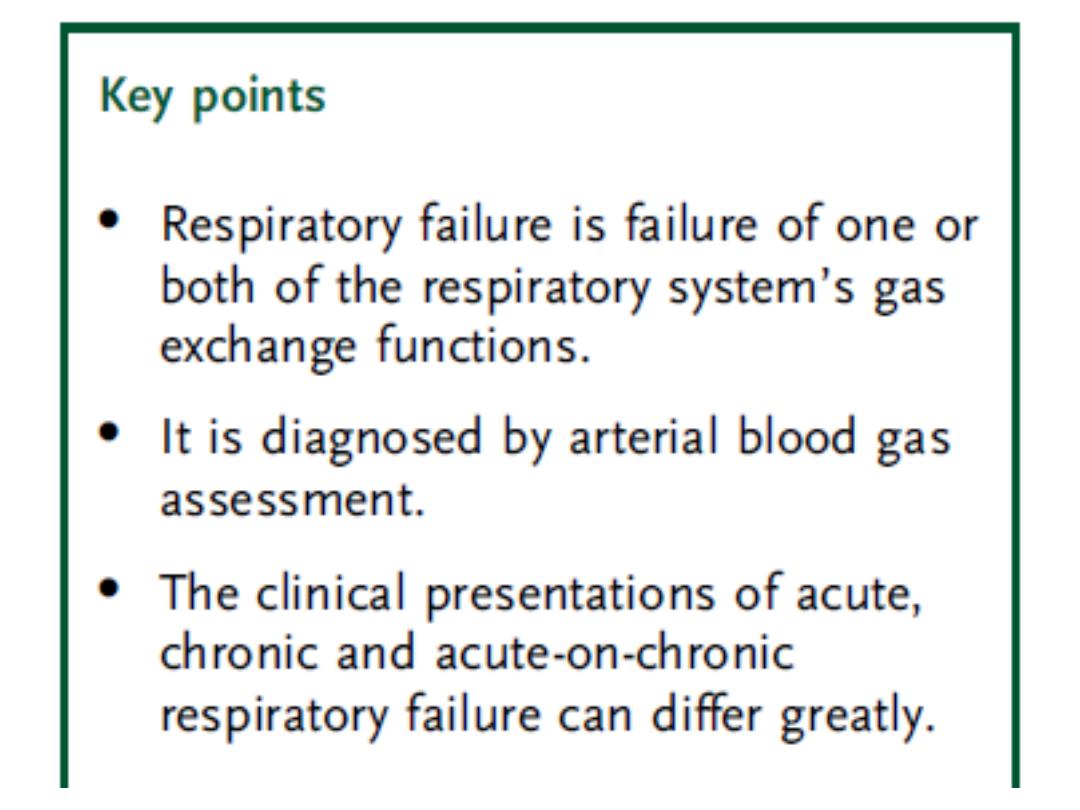
Normal values for arterial blood gases
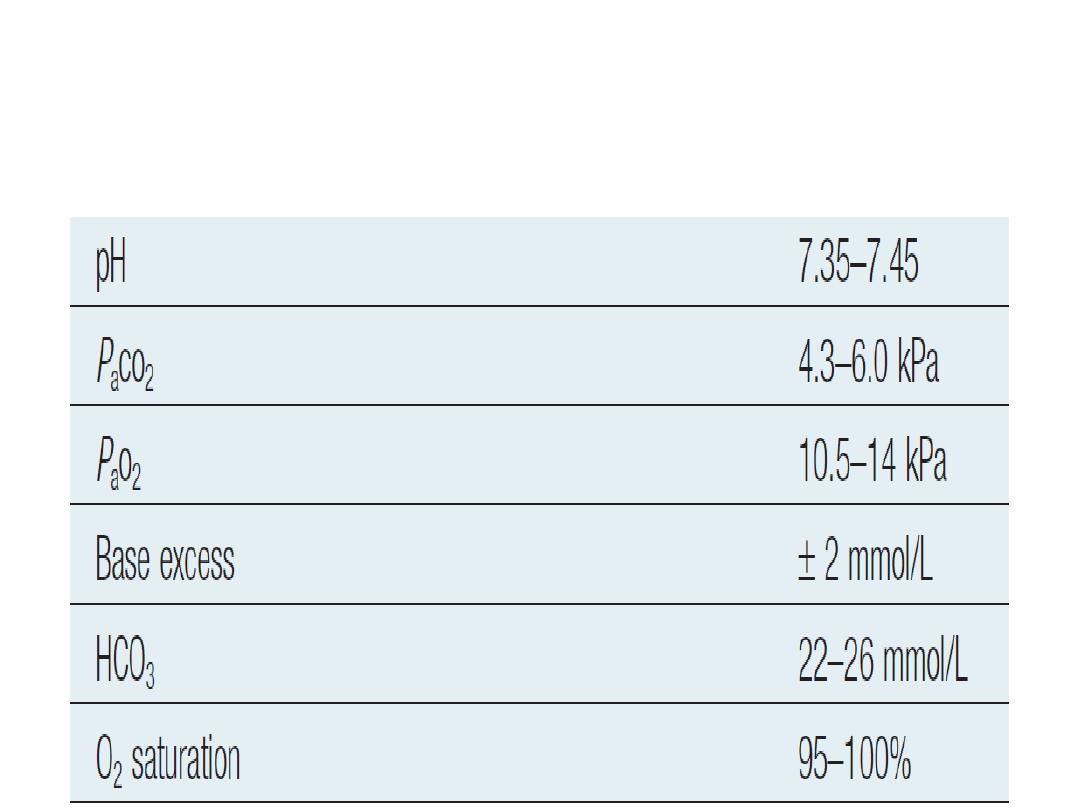
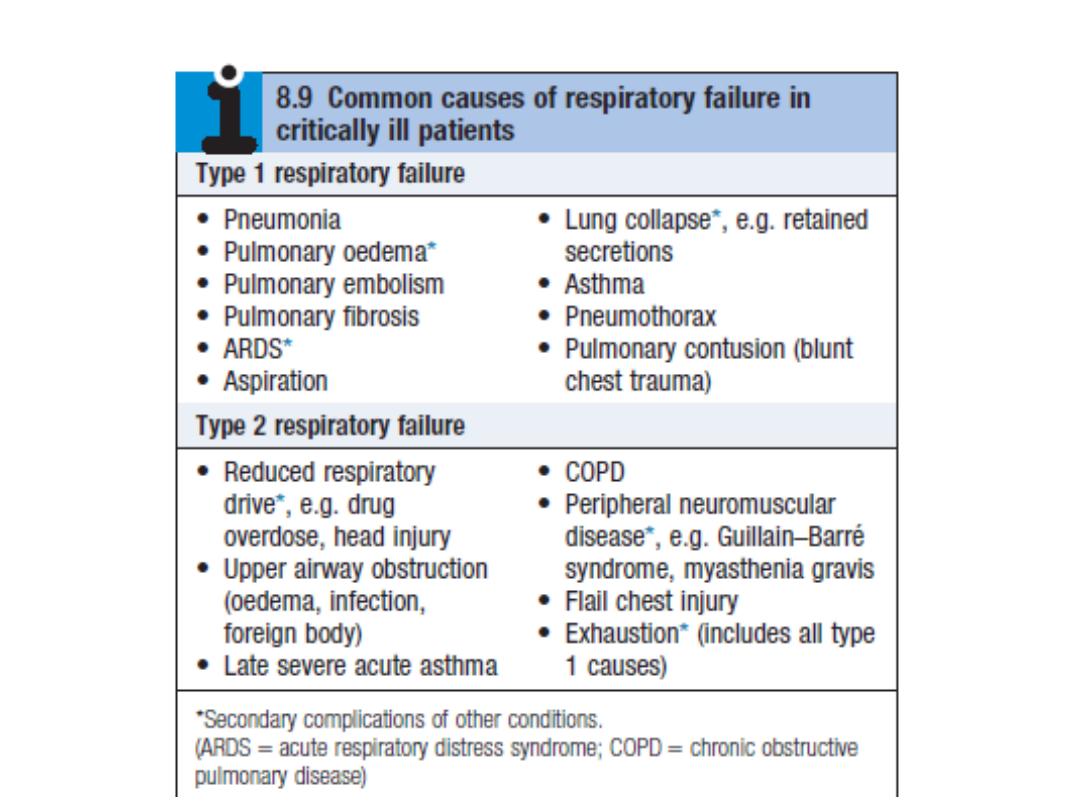
Types , features , causes of respiratory failure
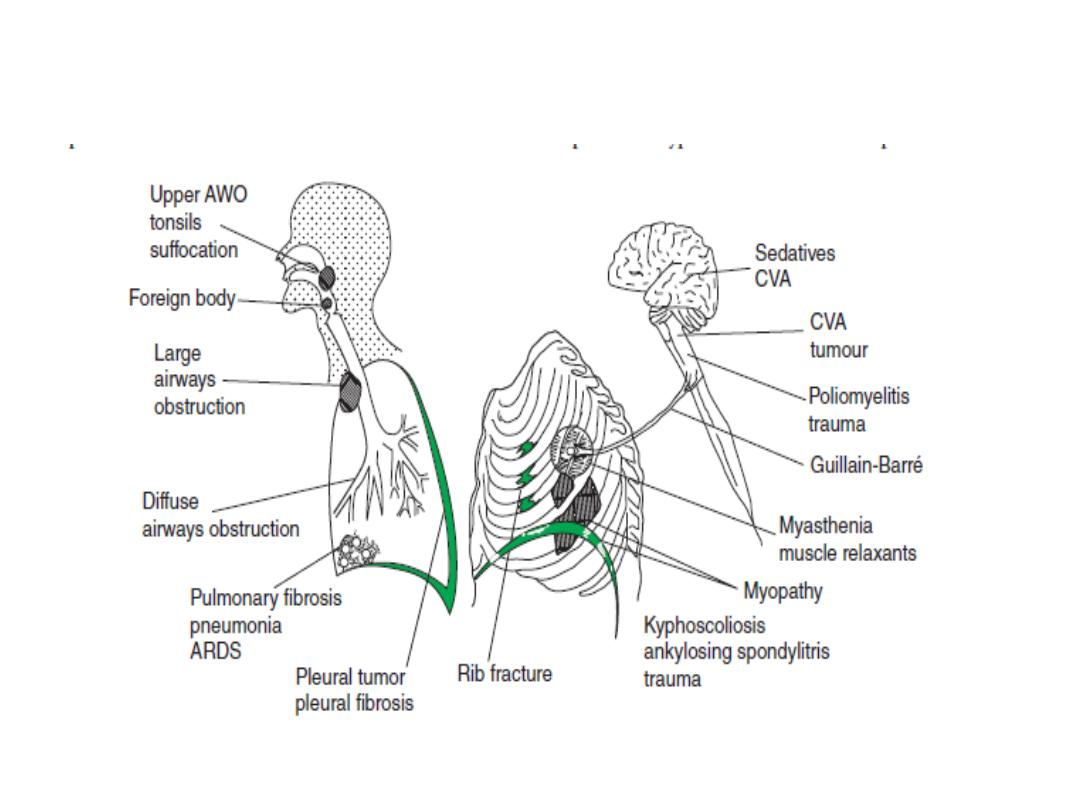
Ventilatory failure (type 2 respiratory failure).

Pathophysiology
• 'type I respiratory failure' disease impairs
ventilation of part of a lung (e.g. in asthma or
pneumonia
•
type II respiratory failure Diseases causing
this abnormality include any that impair
ventilation locally, with sparing of other
regions. Arterial hypoxia with hypercapnia .

Pathophysiology
Type I Respiratory failure
Diseases causing this include all those that impair ventilation
locally with sparing of other regions
Disease impairs ventilation of part of a lung (e.g. in asthma or
pneumonia), perfusion of that region results in hypoxic
and CO2-laden blood entering the pulmonary veins.
Increased ventilation of neighbouring regions of normal lung
can increase CO2 excretion, correcting arterial CO2 to
normal, but cannot augment oxygen uptake because the
haemoglobin flowing through these regions is already fully
saturated.
Admixture of blood from the underventilated and normal
regions thus results in hypoxia with normocapnia,
.

Type II respiratory
failure
Arterial hypoxia with hypercapnia.
is seen in conditions that cause generalised,
severe ventilation–perfusion mismatch,
leaving insufficient normal lung to correct
PaCO2, a disease that reduces total
ventilation.
The latter includes not just diseases of the lung
but also disorders affecting any part of the
neuromuscular mechanism of ventilation

Management of acute respiratory
failure
• Prompt diagnosis and management of the
underlying cause

In type I respiratory failure,
• high concentrations of oxygen (40-60% by
mask).
• mechanical ventilation may be needed.
• Patients who need high concentrations of
oxygen for more than a few hours should
receive humidified oxygen.

Acute type II respiratory failure
• an emergency, requires immediate
intervention.
• distinguish between patients with
1- high ventilatory drive (rapid respiratory rate
and accessory muscle recruitment)
2- reduced or inadequate respiratory effort.

1- high ventilatory drive (rapid respiratory rate
and accessory muscle recruitment)
A-Upper airway obstruction
inspiratory stridor is present acute upper airway
obstruction from
Causes
1. foreign body inhalation
( treated by Heimlich
maneuver )
2. laryngeal obstruction (angioedema, carcinoma
or vocal cord paralysis)
immediate intubation or emergency tracheostomy
may be life-saving.

B-Lung disease
1- severe generalised bronchial obstruction from
COPD, asthma.
2-ARDS .
3-Tension pneumothorax.
Treatment
1- high-concentration (e.g. 60%) oxygen.
2-non-invasive ventilation (NIV).

indications to supported ventilation
1. Failure to respond to initial treatment,
2. declining conscious level .
3. worsening respiratory acidosis .

2- reduced or inadequate respiratory
effort:
Reduced drive or conscious level may be
suffering from
1) sedative poisoning.
2) CO
2
narcosis .
3) a primary failure of neurological drive (e.g.
following intracerebral haemorrhage or head
injury).

Chronic and 'acute on chronic' type II
respiratory failure
The most common cause is severe COPD.
CO
2
may be persistently raised.
no persisting acidaemia.

Hypoxic drive
• A small percentage of patients with severe
chronic COPD and type II respiratory failure
develop abnormal tolerance to raised PaCO
2
and may become dependent on hypoxic drive
to breathe.
• lower concentrations of oxygen (24-28% by
Venturi mask).
• In all cases, regular monitoring of arterial
blood gases is important to assess progress.

Assessment and management of
'acute on chronic' type II respiratory
failure

Initial assessment
• Patient may not appear distressed despite being critically ill
• Conscious level (response to commands, ability to cough)
• CO
2
retention (warm periphery, bounding pulses, flapping
tremor)
• Airways obstruction (wheeze, prolonged expiration,
hyperinflation, intercostal indrawing, pursed lips)
• Cor pulmonale (peripheral oedema, raised JVP,
hepatomegaly, ascites)
• Background functional status and quality of life
• Signs of precipitating cause .

Investigations
• Pulse oximeter(O2 saturation)
• Arterial blood gases (severity of hypoxaemia,
hypercapnia, acidaemia, bicarbonate)
• Chest X-ray

Treatment
• Maintenance of airway
• Treat specific precipitating cause
• Frequent physiotherapy ± pharyngeal suction
• Nebulised bronchodilators
• Controlled oxygen therapy
– Start with 24% Venturi mask
– Aim for a normal PaO
2
• Antibiotics
• Diuretics
severe hypoxaemia
lead to potentially fatal arrhythmias or severe
cerebral complications

•
Doxapram
• is a respiratory stimulant

Non-invasive respiratory support
• Non-invasive respiratory support includes
techniques that do not require sedation or
an endotracheal or tracheostomy tube.

Non-invasive respiratory
Types of
• Continuous positive airway pressure (CPAP)
alone (non-invasive ventilation, or NIV).
•
BIPAP plus additional support, in the form
of pressure applied to the breathing circuit
during inspiration
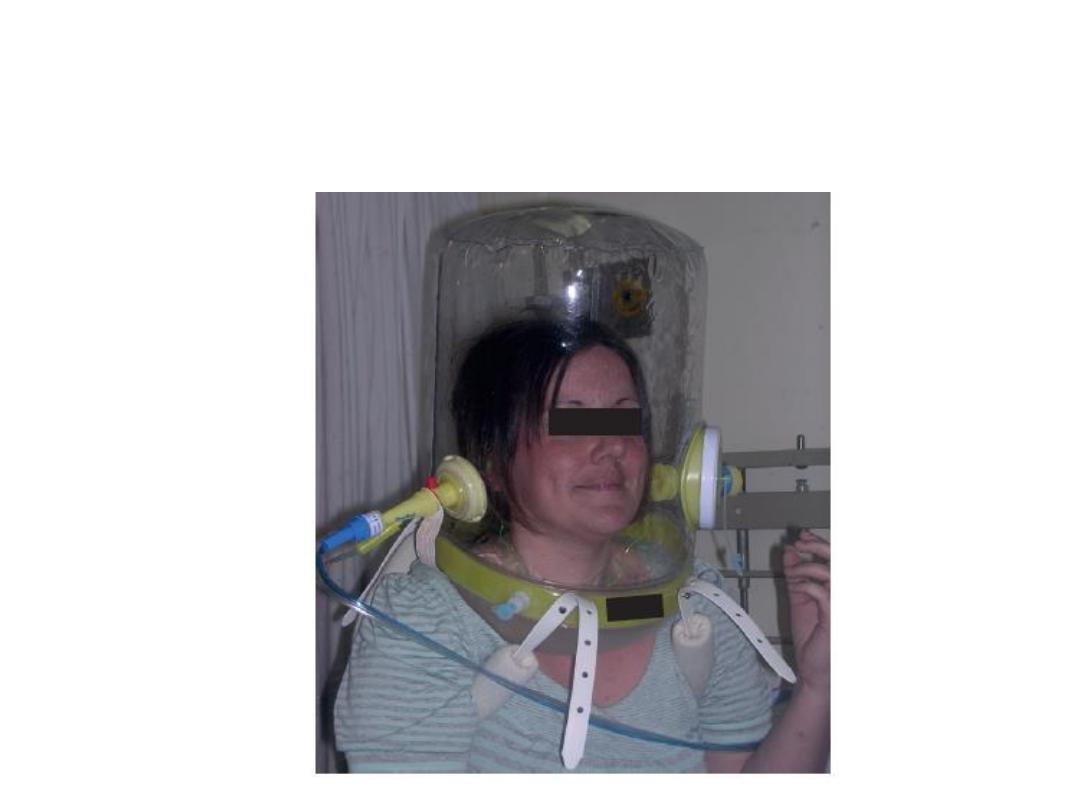
CPAP delivery with a Castar hood.

Lung transplantation
•
Indications for lung transplantation
Parenchymal lung diseas
• Cystic fibrosis
• Emphysema
• Pulmonary fibrosis.

Pulmonary vascular disease
• Primary pulmonary hypertension
• Thromboembolic pulmonary hypertension

•
Types of transplants
• Single-lung transplantation
• bilateral lung transplantation .
• Combined heart-lung transplantation.
The prognosis
• following lung transplantation is improving
steadily with modern immunosuppressive
drugs

Thank you

A 65-year-old man is found collapsed in the ward. On
examination there is no evidence of stridor, respiratory rate
is 4 breaths/min and oxygen saturations are 82% on air.
His pulse is 120 beats/min and regular, blood pressure (BP)
90/60 mmHg, Glasgow Coma Scale is 3/15 and he has
bilateral pupillary constriction and no focal neurological
defi cit.
What is the most likely diagnosis?
a. Anaphylaxis
b. Myocardial infarction
c. Opiate toxicity
d. Pulmonary embolus
e. Raised intracranial pressure

A 57-year-old woman has just undergone fi breoptic
bronchoscopy. Monitoring shows her oxygen saturations
to have fallen to 86% on 2 L/min oxygen. On examination
her pulse is 88 beats/min, BP 146/84 mmHg, respiratory
rate 5 breaths/min. Chest examination reveals trachea –
midline, expansion right = left, percussion right = left,
breath sounds vesicular, nil added.
Which of the following is the most likely complication
that has occurred following bronchoscopy?
a. Bleeding
b. Bronchospasm
c. Infection
d. Oversedation
e. Pneumothorax

Q
•QUIZE
