
بسم هللا الرحمن الرحيم
Respiratory Medicine
05 /02/2020
Dr.Majeed Mohan Alhamami

Objectives
• Defintion
• Epidemiology
• Clinical presentation in emergency and
outpatient.
• Diagnosis
• Treatment of the emergency and chronic
condition.
• Complication
• prognosis
Asthma
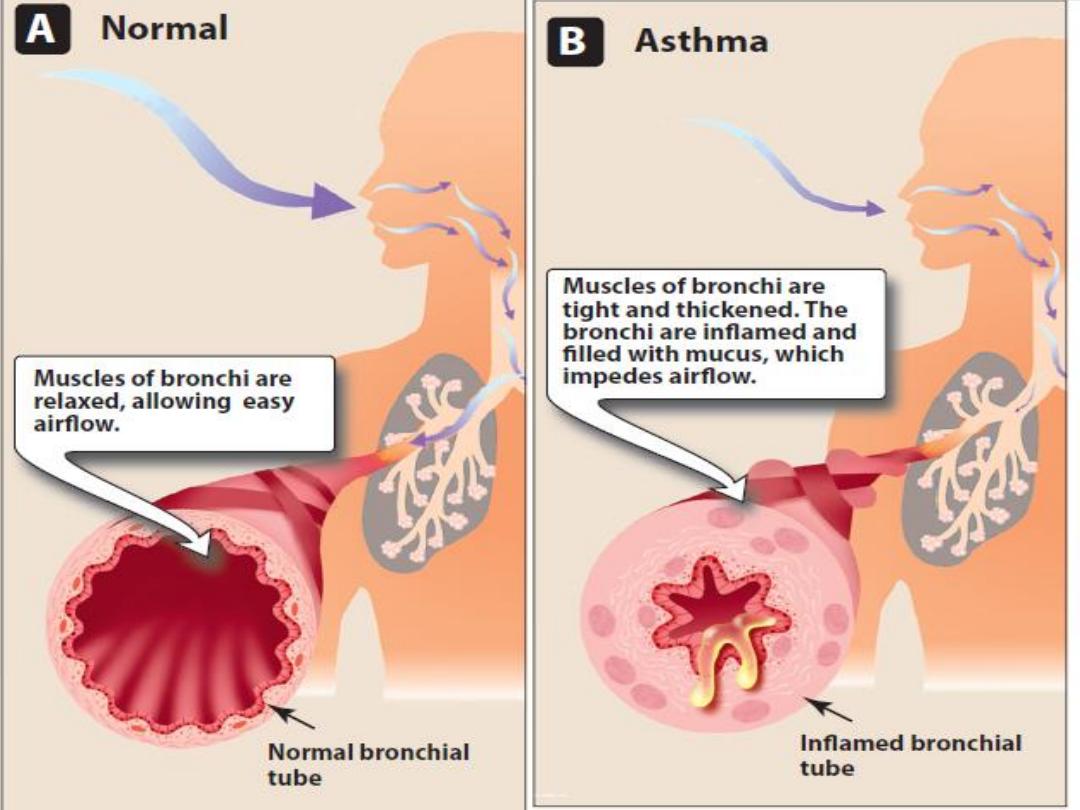
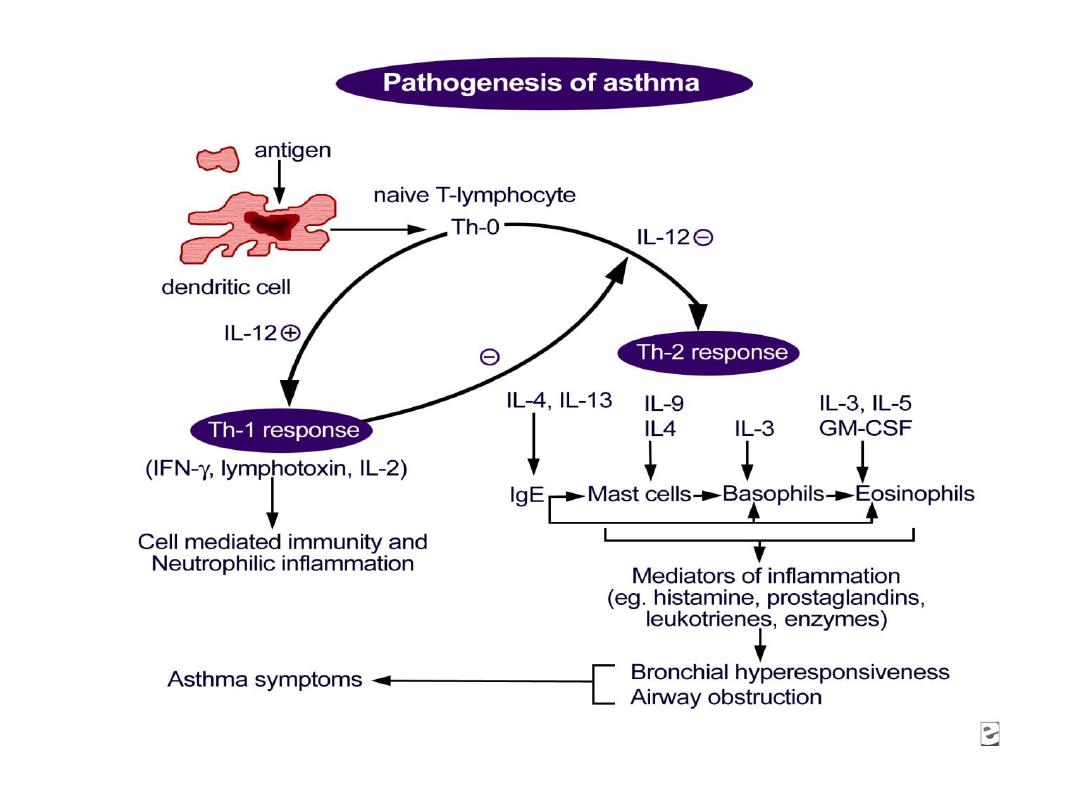
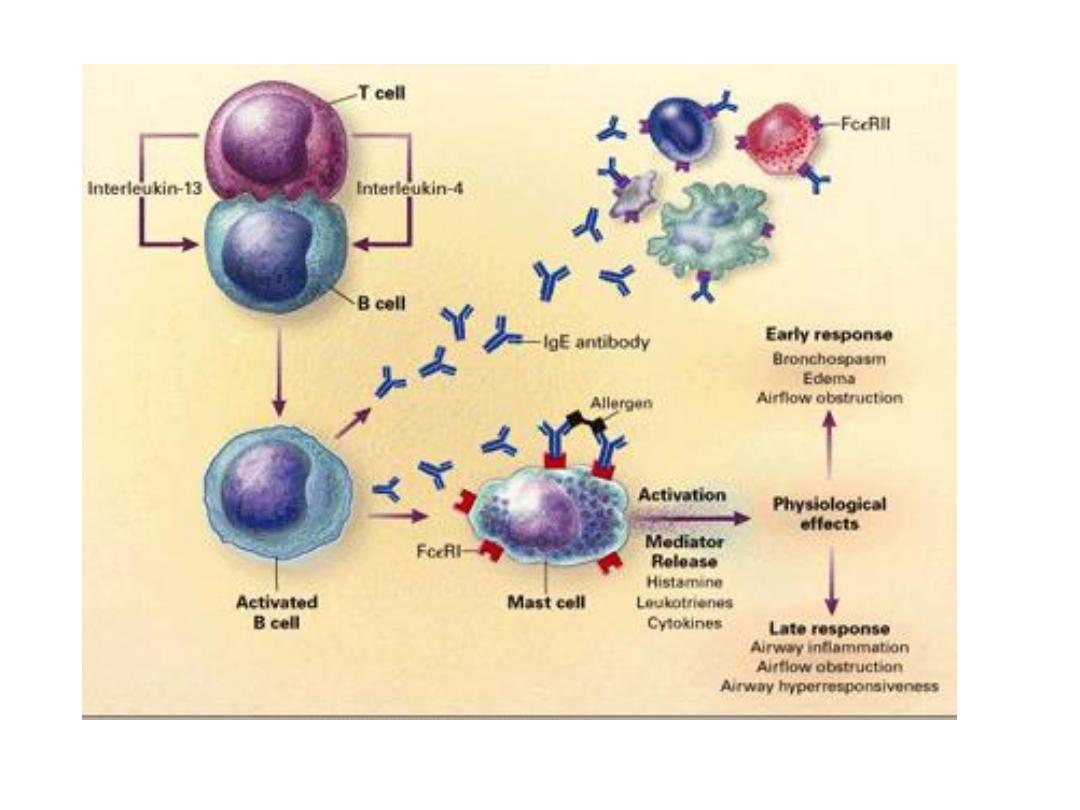
• Asthma is a common chronic inflammatory
condition of the lung airways whose cause is
still incompletely understood.
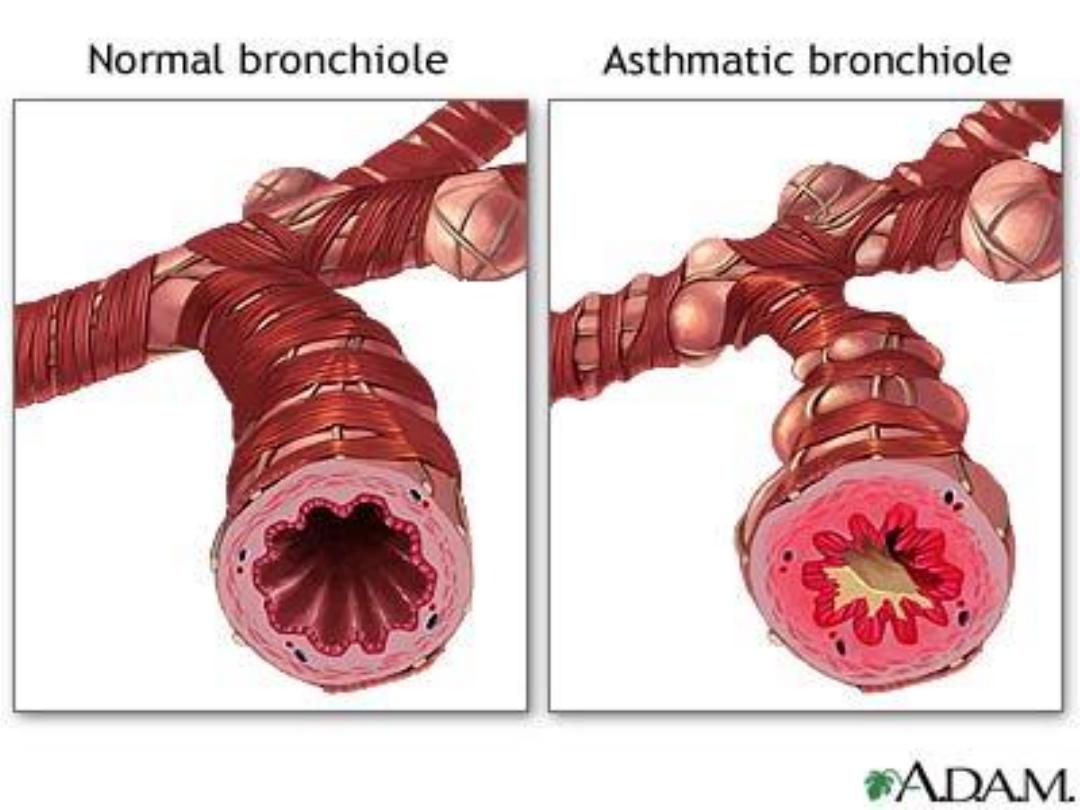
Asthma has three characteristics:
• Airflow limitation which is usually reversible
spontaneously or with treatment .
• Airway hyperresponsiveness to a wide range
of stimuli .
• Inflammation of the bronchi with
eosinophils, T lymphocytes and mast cells
with associated plasma exudation, oedema,
marked smooth muscle hypertrophy, mucus
plugging and epithelial damage.

Typical symptoms include
• wheeze,
• cough,
• chest tightness
• dyspnoea

Epidemiology
• The prevalence of asthma increased steadily.
• that asthma affects 300 million people world-
wide
• an additional 100 million persons will be
diagnosed by 2025.
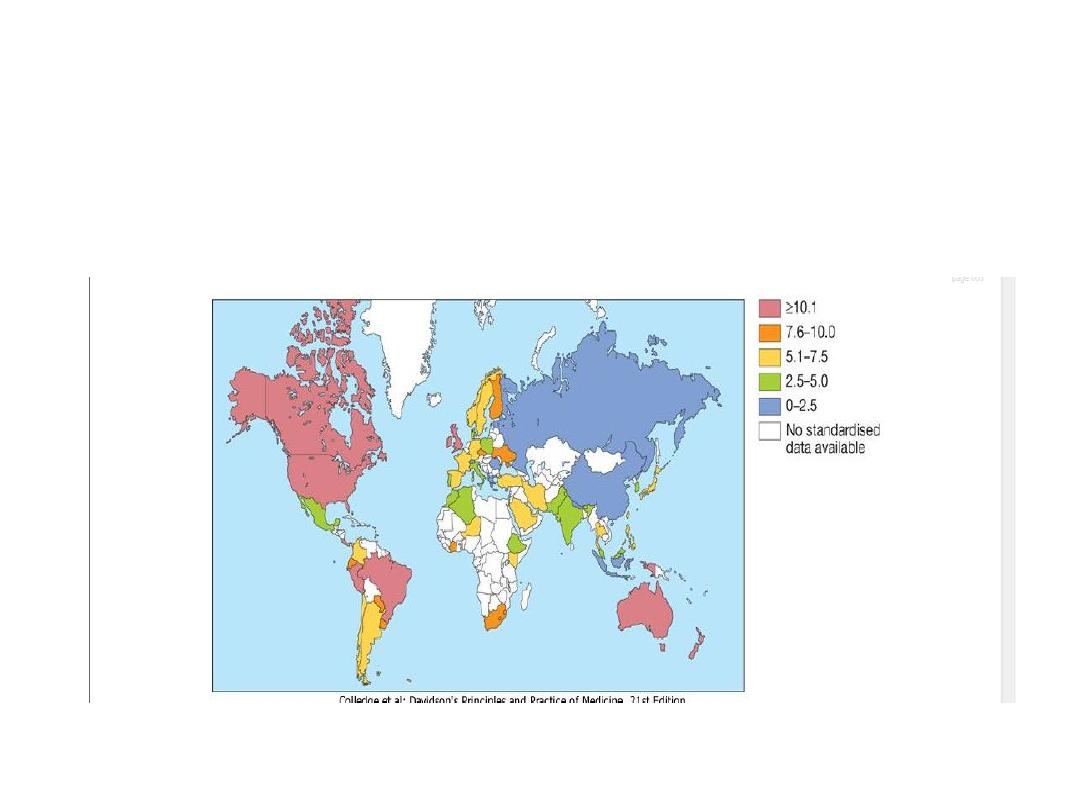
World map showing the prevalence of clinical asthma
(proportion of population (%)). Data drawn from the
European Community Respiratory Health Study (ECRHS) and
the International Study of Asthma and Allergies in Childhood
(ISAAC).

Classification
• Asthma can be divided into:
• extrinsic - implying a definite external cause
• intrinsic or cryptogenic - when no causative
agent can be identified.

Extrinsic asthma
• Most frequently in atopic individuals.
• Atopy or positive skin-prick tests to inhalant
allergens are shown in 90% of children and
50% of adults with persistent asthma.
• Childhood asthma is often accompanied by
eczema .

Intrinsic asthma
• often starts in middle age ('late onset').
• Non-atopic
• from extrinsic causes such as sensitization to
occupational agents
• aspirin intolerance
• β-adrenoceptor-blocking agents.

• Extrinsic causes must be considered in all
cases of asthma and, where possible,
avoided.
• Aspirin-sensitive asthma .
• In exercise-induced asthma,

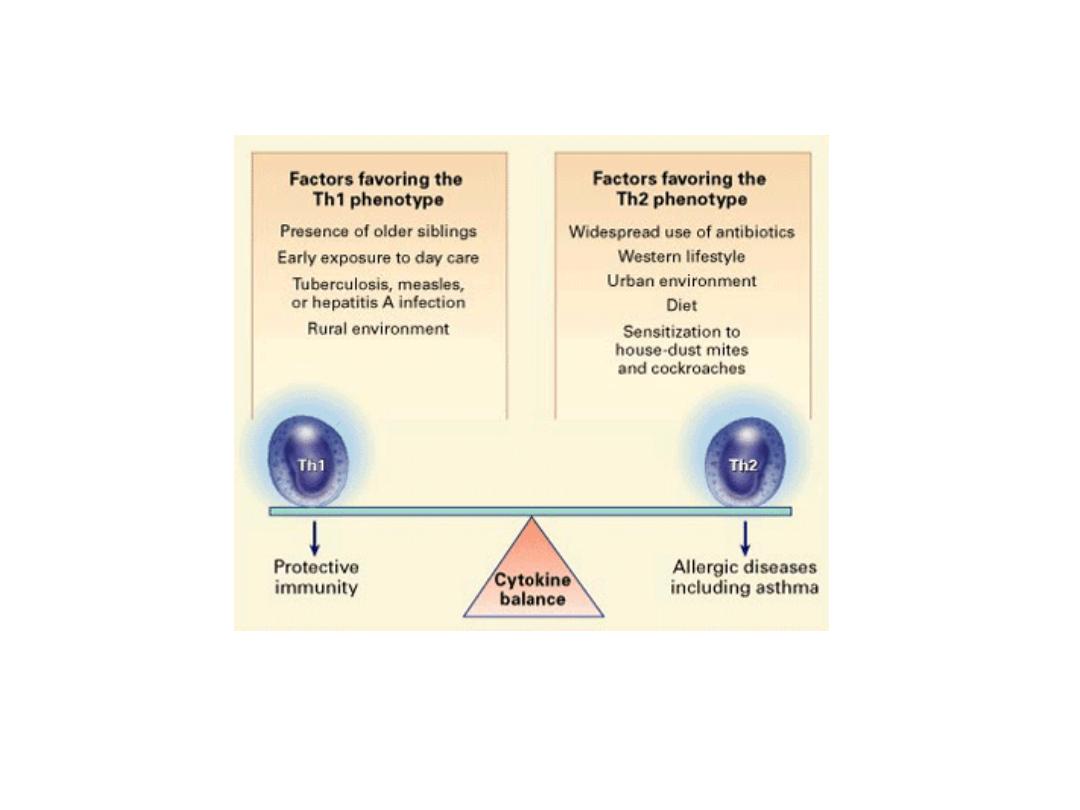
Factors implicated in the development of, or
protection from, asthma.
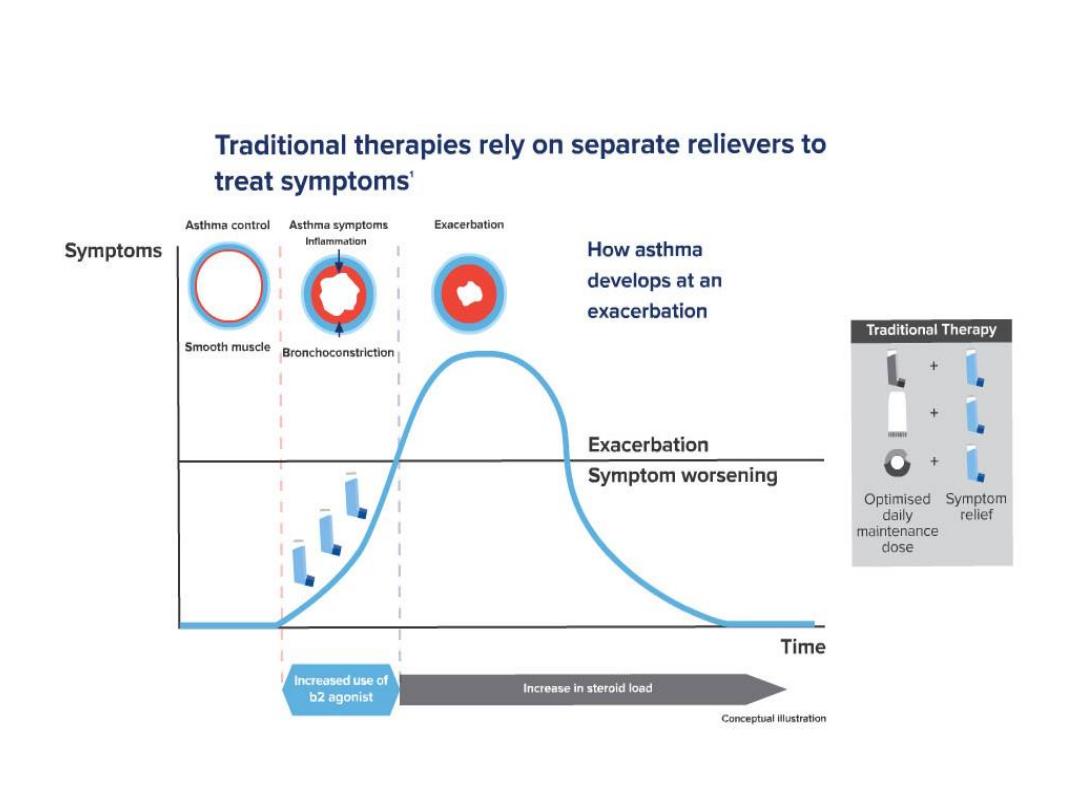
Asthma Traditional Therapy
Approach
.1
Tattersfield AE, et al. Am J Respir Care Med 1999; 160:594-9
.2
2. FitzGerald JM, et al. Can Respir J 2003; 10(8):427
.3
Bateman et al .J Allergy Clin Immunol 2010; 125: 600-8

•
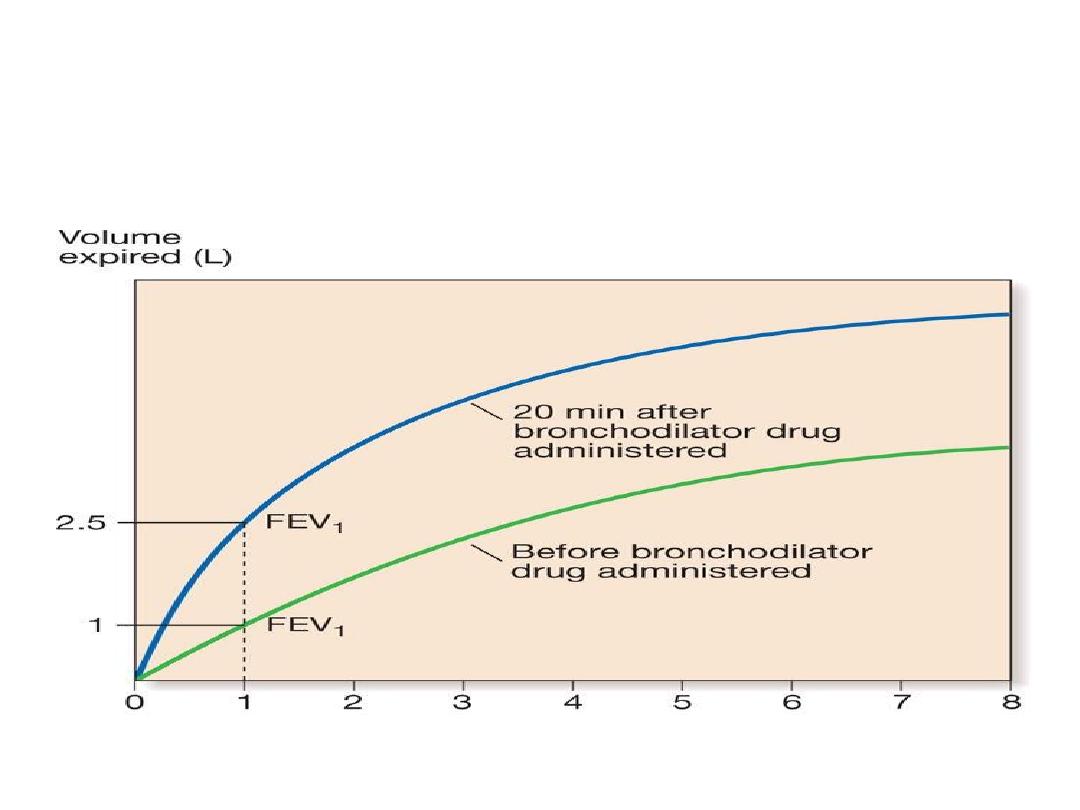
Reversibility test. Forced expiratory before and 20
minutes after inhalation of a
β
2
-adrenoceptor
agonist. Note the
increase in FEV
1
from 1.0
to
2.5 L
Airway hyper-reactivity in asthma.
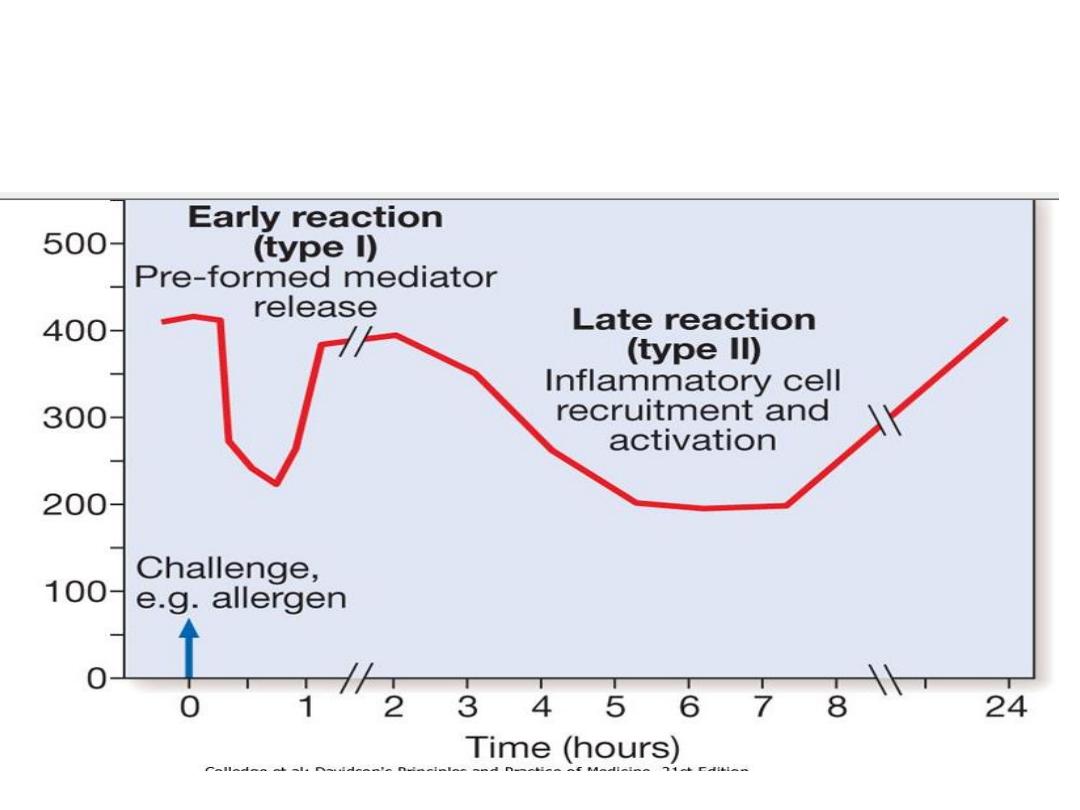
Changes in peak flow following allergen challenge. A similar biphasic
response is observed following a variety of different challenges.
Occasionally an individual will develop an isolated late response with
no early reaction

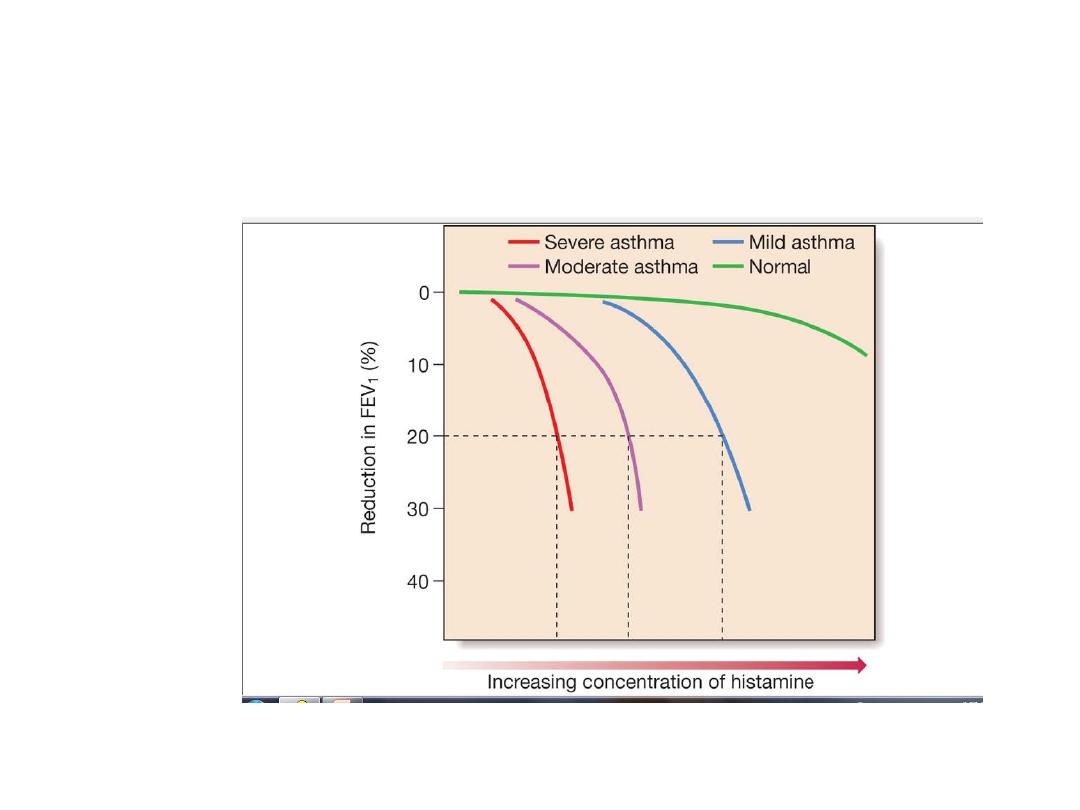
• Airway hyper-reactivity in asthma. This is
demonstrated by bronchial challenge tests by the
administration of sequentially increasing
concentrations of either histamine, methacholine or
mannitol. The reactivity of the airways is expressed
as the concentration or dose of either chemical
required to produce a certain decrease (usually 20%)
in the FEV
1
(PC
20
or PD
20
respectively).
.

Diurnal pattern
Asthma characteristically displays a diurnal
pattern,
with symptoms and lung function being worse in
the
early morning. Particularly when poorly
controlled,
symptoms such
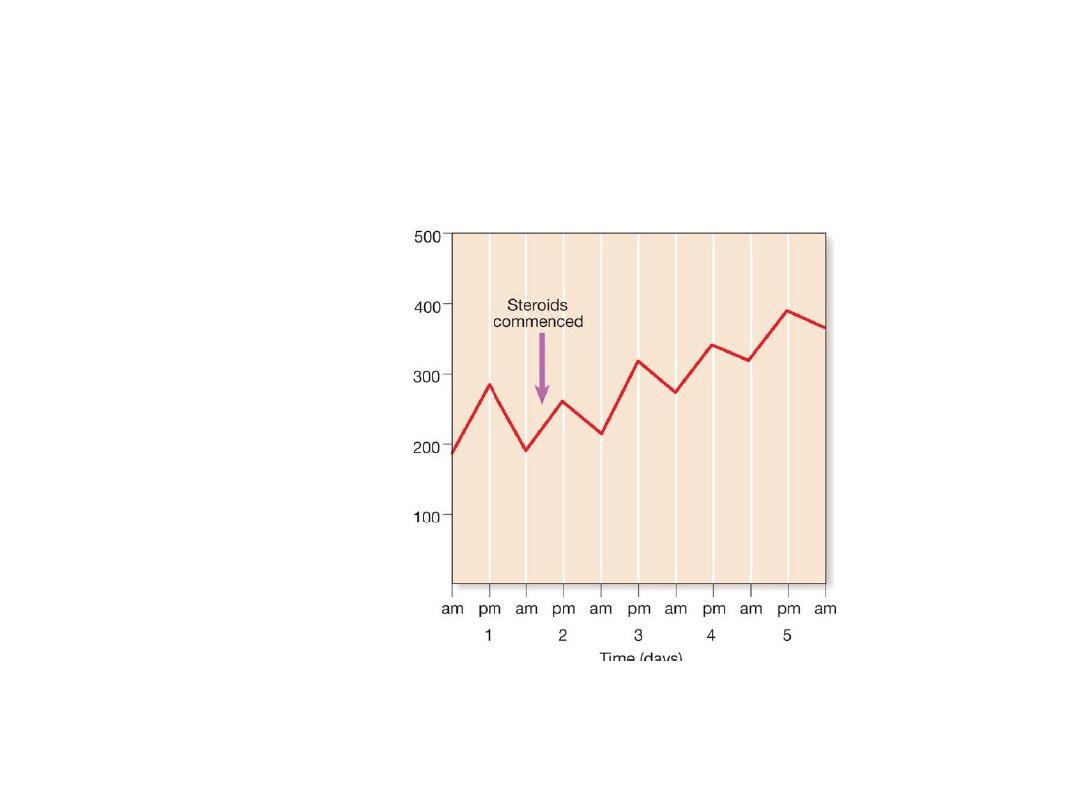
Serial recordings of peak expiratory flow (PEF) in a patient with
asthma. Note the sharp overnight fall (morning dip) and
subsequent rise during the day. In this example corticosteroids
have been commenced, followed by a subsequent improvement
in PEF rate and loss of morning dipping.
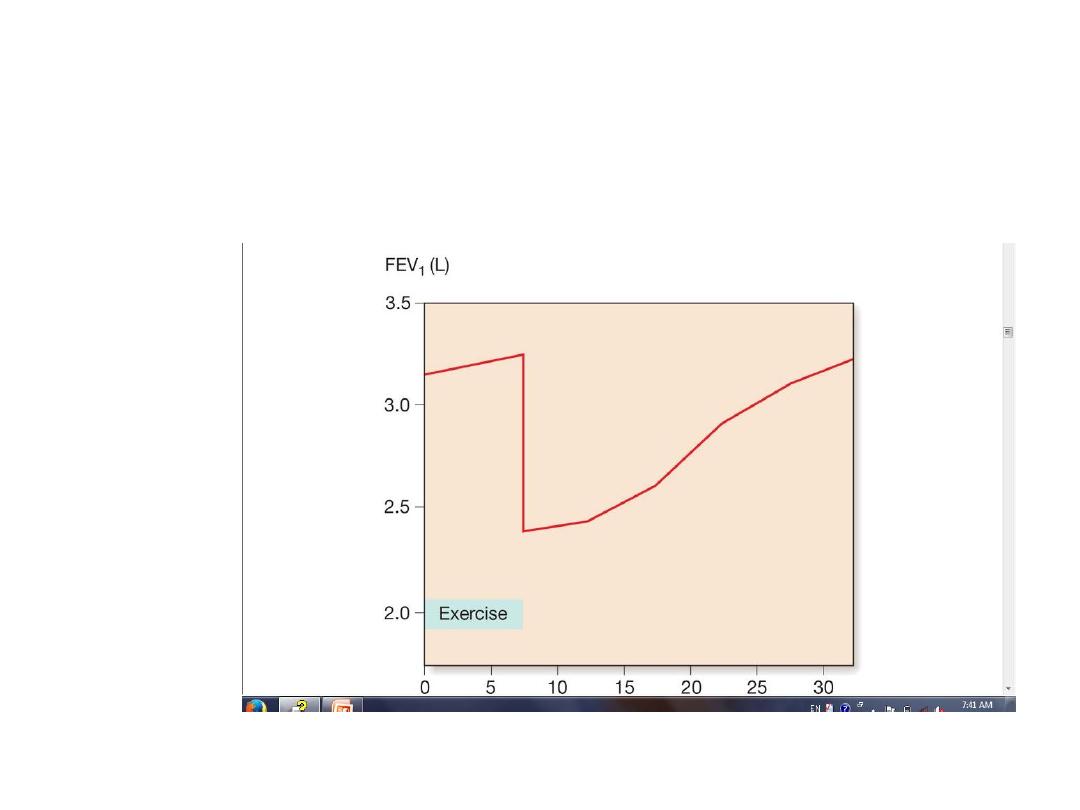
Exercise-induced asthma. Serial recordings of FEV
1
in a patient with
bronchial asthma before and after 6 minutes of strenuous exercise.
Note initial slight rise on completion of exercise, followed by sudden
fall and gradual recovery. Adequate warm-up exercise or pre-
treatment with a β
2
-adrenoceptor agonist, nedocromil sodium or a
leukotriene antagonist (e.g. montelukast sodium) can protect against
time in minute
)
exercise-induced symptoms.

Making a diagnosis of asthma
• Compatible clinical history plus either/or: FEV
1
≥ 15%* (and 200 mL) increase following
administration of a bronchodilator/trial of
corticosteroids
• > 20% diurnal variation on ≥ 3 days in a week
for 2 weeks on PEF diary
• FEV
1
≥ 15% decrease after 6 mins of exercise

Signs
• Depend on severity
• Conscious level normal-………. coma
• Respiratory rate normal-tachypnoea-…….apnoea
• Blood pressure hypertension(vasculitis) paradox
• Pulse rate
• Position
• Chest examination normal in mild type
hyperinflation in chronic one
Prolonged expiration exp,inspiratory
rhonchi
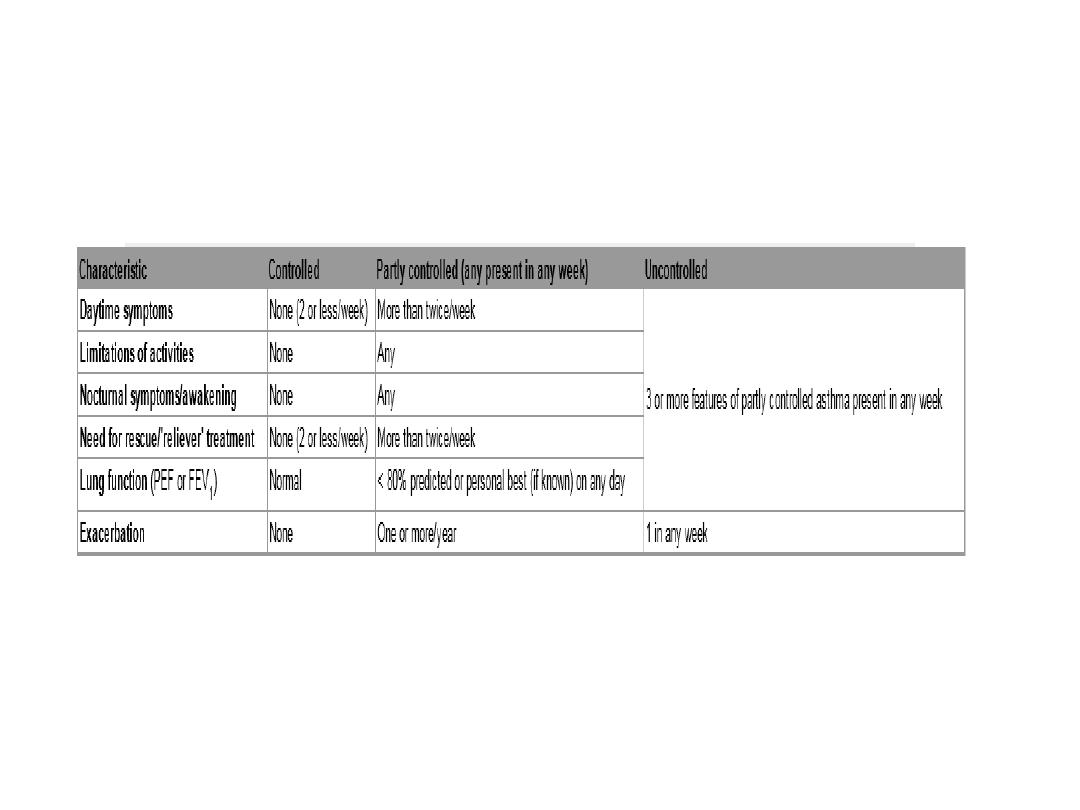
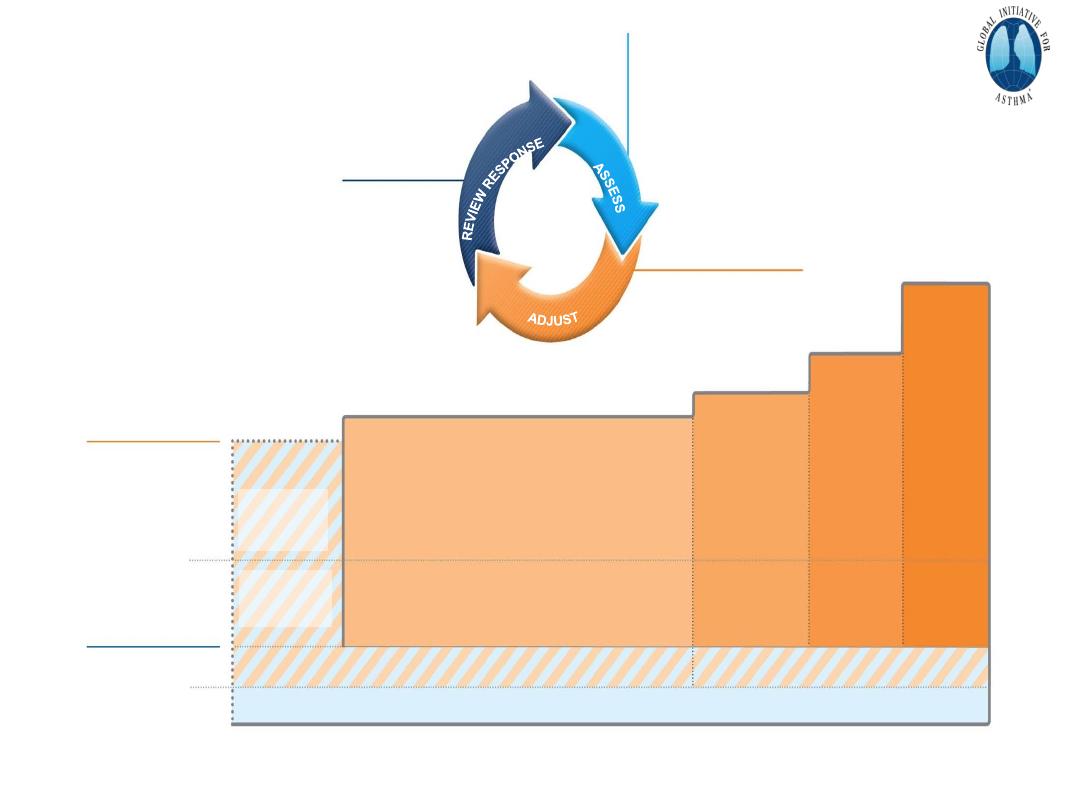
Level of asthma control
© Global Initiative for Asthma, www.ginasthma.org
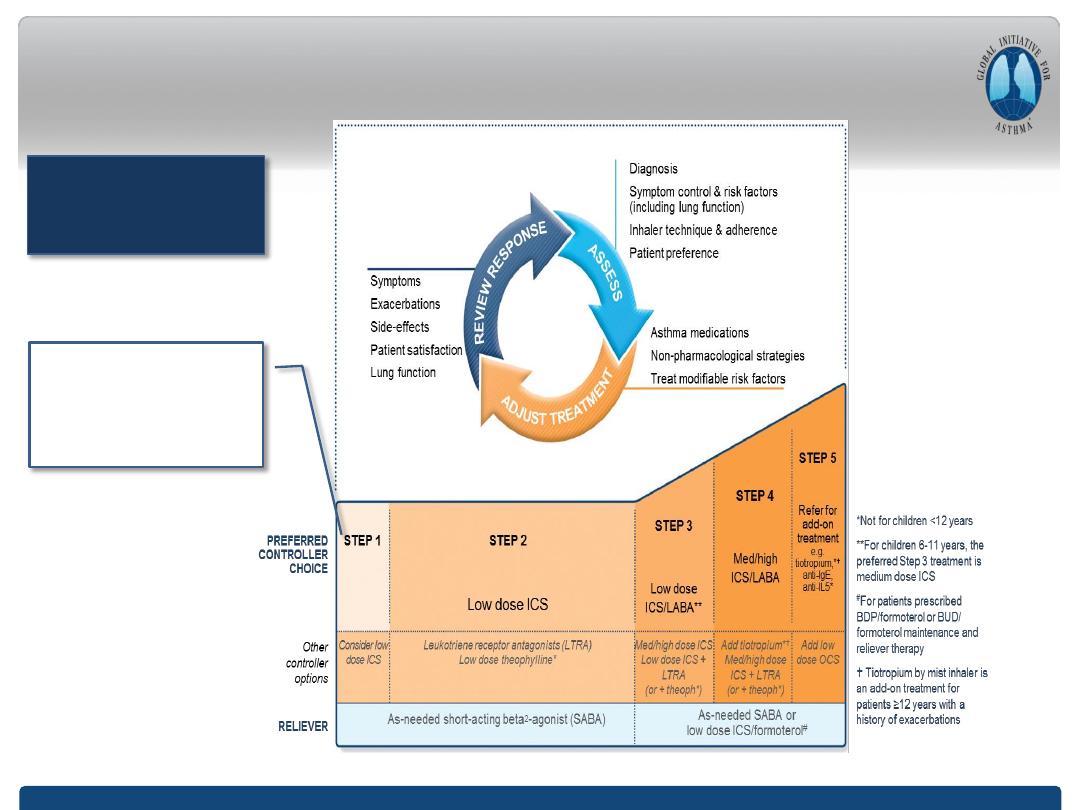
GINA 2018
– main treatment figure
GINA 2018, Box 3-5 (2/8) (upper part)
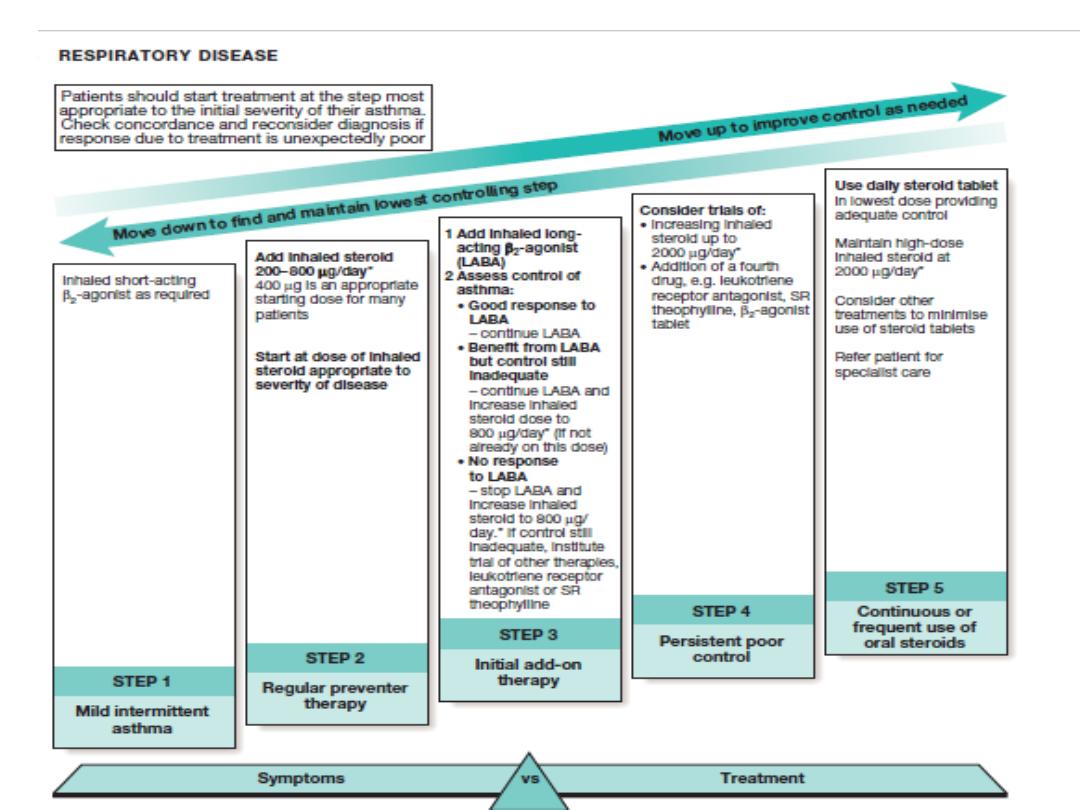
Previously, no controller was
recommended for
Step 1, i.e. SABA-only
treatment was ‘preferred’
Step 1 treatment is for
patients with symptoms
<twice/month and no risk
factors for exacerbations
*
Off-label; data only with budesonide-formoterol (bud-form)
†
Off-label; separate or combination ICS and SABA inhalers
PREFERRED
CONTROLLER
to prevent exacerbations
and control symptoms
Other
controller options
Other
reliever option
PREFERRED
RELIEVER
STEP 2
Daily low dose inhaled corticosteroid (ICS),
or as-needed low dose ICS-formoterol *
STEP 3
Low dose
ICS-LABA
STEP 4
Medium dose
ICS-LABA
Leukotriene receptor antagonist (LTRA), or
low dose ICS taken whenever SABA taken
†
As-needed low dose ICS-formoterol *
As-needed short-acting
β
2
-agonist (SABA)
Medium dose
ICS, or low dose
ICS+LTRA #
High dose
ICS, add-on
tiotropium, or
add-on LTRA #
Add low dose
OCS, but
consider
side-effects
As-needed low dose ICS-formoterol
‡
Box 3-5A
Adults & adolescents 12+ years
Personalized asthma management:
Assess, Adjust, Review response
Asthma medication options:
Adjust treatment up and down for
individual patient needs
STEP 5
High dose
ICS-LABA
Refer for
phenotypic
assessment
± add-on
therapy,
e.g.tiotropium,
anti-IgE,
anti-IL5/5R,
anti-IL4R
Symptoms
Exacerbations
Side-effects
Lung function
Patient satisfaction
Confirmation of diagnosis if necessary
Symptom control & modifiable
risk factors (including lung function)
Comorbidities
Inhaler technique & adherence
Patient goals
Treatment of modifiable risk
factors & comorbidities
Non-pharmacological strategies
Education & skills training
Asthma medications
1
© Global Initiative for Asthma, www.ginasthma.org
STEP 1
As-needed
low dose
ICS-formoterol
*
Low dose ICS
taken whenever
SABA is taken
†
‡ Low-dose ICS-form is the reliever for patients prescribed
bud-form or BDP-form maintenance and reliever therapy
#
Consider adding HDM SLIT for sensitized patients with
allergic rhinitis and FEV >70% predicted
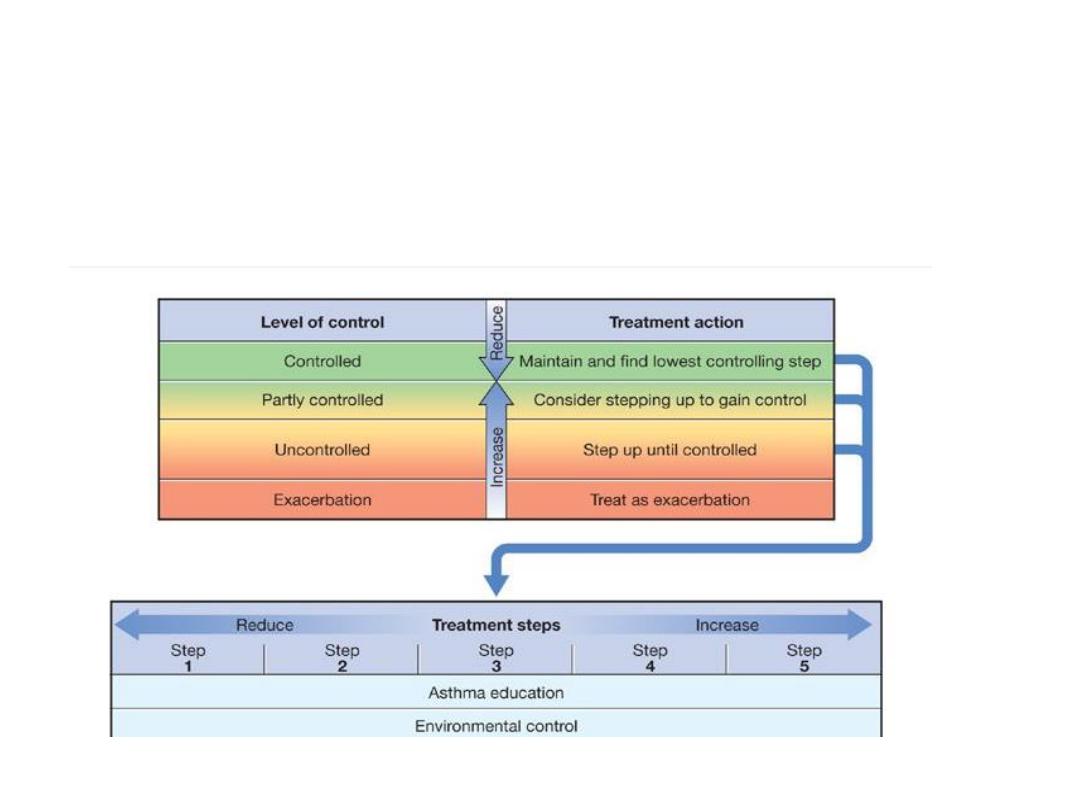
Management approach based on asthma control. For
children older than 5 years, adolescents and adults. (ICS =
inhaled corticosteroid) *Receptor antagonist or synthesis
inhibitors

How to use a metered-dose inhaler.

Step 3: assess inhaler
technique
Step 4: assess patient adherence to treatment
Step 5: exclude alternative or
overlapping diagnosis as primary
conditions
Step 7-
Environmental Factors:
Action - Advice on allergens avoidance
Animals outside the home (cats, dogs, hamsters)
Dust Mites: Allergy Waterproof Cases
Damp cloth and vacuum
Home Humidity <50%
No carpets in the bedroom
Washing with hot water weekly
Pollens: Close windows in time of pollination
Snuff: Avoid smoking and passive exposure
Fungi: Remove mildew stains on the walls
Avoid wood stoves, smoke, air fresheners, etc..

Classification of severity of asthma
exacerbations.
Symptoms
Speech
•
Mild Breathlessness With activity Sentences
• Moderate With talking Phrases
• Severe At rest Words
•
Impending Respiratory Failure At rest Mute
•

Mild Moderate Severe Impending Respiratory Failure
Signs
Body position
Able to recline Prefers sitting Unable to recline Unable to recline
Respiratory rate
Increased Increased
Often > 30/min > 30/min
Use of accessory respiratory muscles
Usually not Commonly Usually Paradoxical thoracoabdominal
movement

Pulsus paradoxus (mm Hg) Mental status
Mild < 10 May beagitated
Moderate 10–25 Usually agitated
Sever often > 25 Usually agitate
Impending Often absent Confused or drowsy

Mild Moderate Severe Impending Respiratory Failure
•
Breath sounds Heart rate
(beats/min)
Moderate wheezing at mid- to end-expiration < 100
Loud wheezes throughout expiration 100-120
Loud inspiratory and expiratory wheezes > 120
Little air movement without wheezes Relativebradycardia

Mild Moderate Severe Impending Respiratory Failure
• Functional assessment
•
PEF (% predicted or personal best)
> 80 50–80 < 50 or response to therapy lasts < 2 hours < 50
• SaO
2
(%, room air)
> 95 91–95 < 91 < 91
•
Pa O
2
(mm Hg, room air)
Normal > 60 < 60 < 60
• Pa CO
2
(mm Hg)
< 42 < 42 42 42
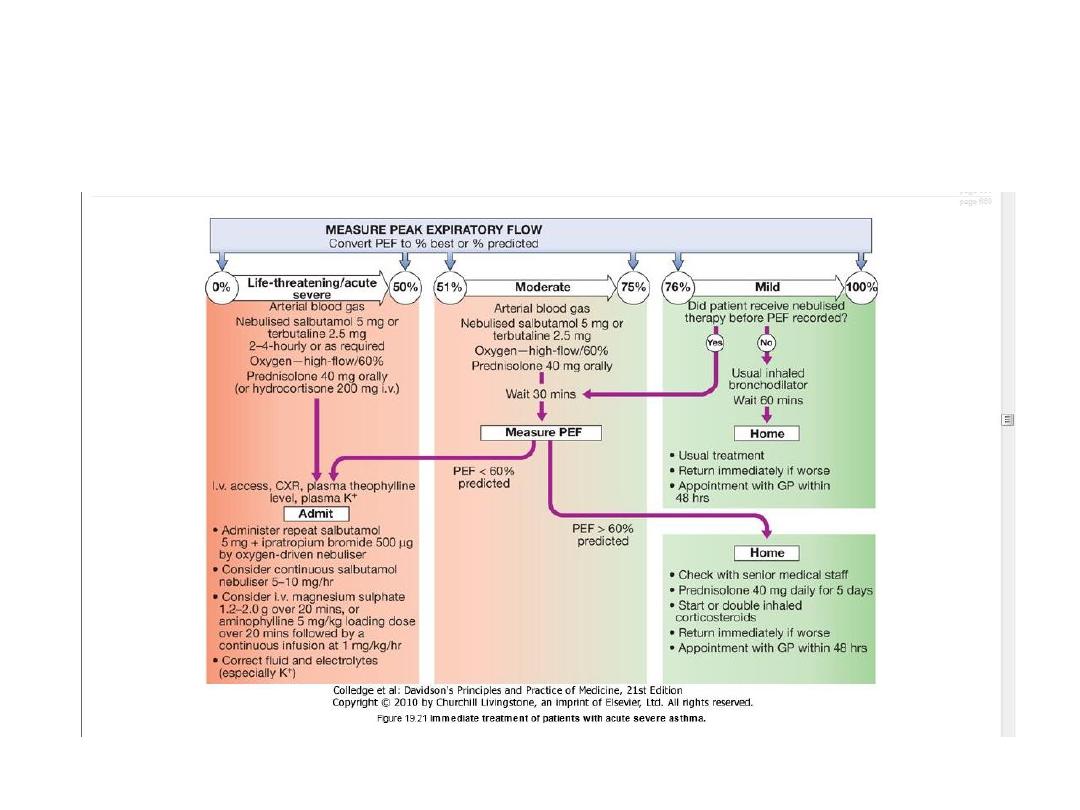
Immediate treatment of patients with acute severe asthma.
Indications for assisted ventilation in
acute severe asthma
• Coma
• Respiratory arrest
• Deterioration of arterial blood gas tensions
despite optimal therapy
– PaO
2
< 8 kPa (60 mmHg) and falling
– PaCO
2
> 6 kPa (45 mmHg) and rising
– pH low and falling (H
+
high and rising)
• Exhaustion, confusion, drowsiness
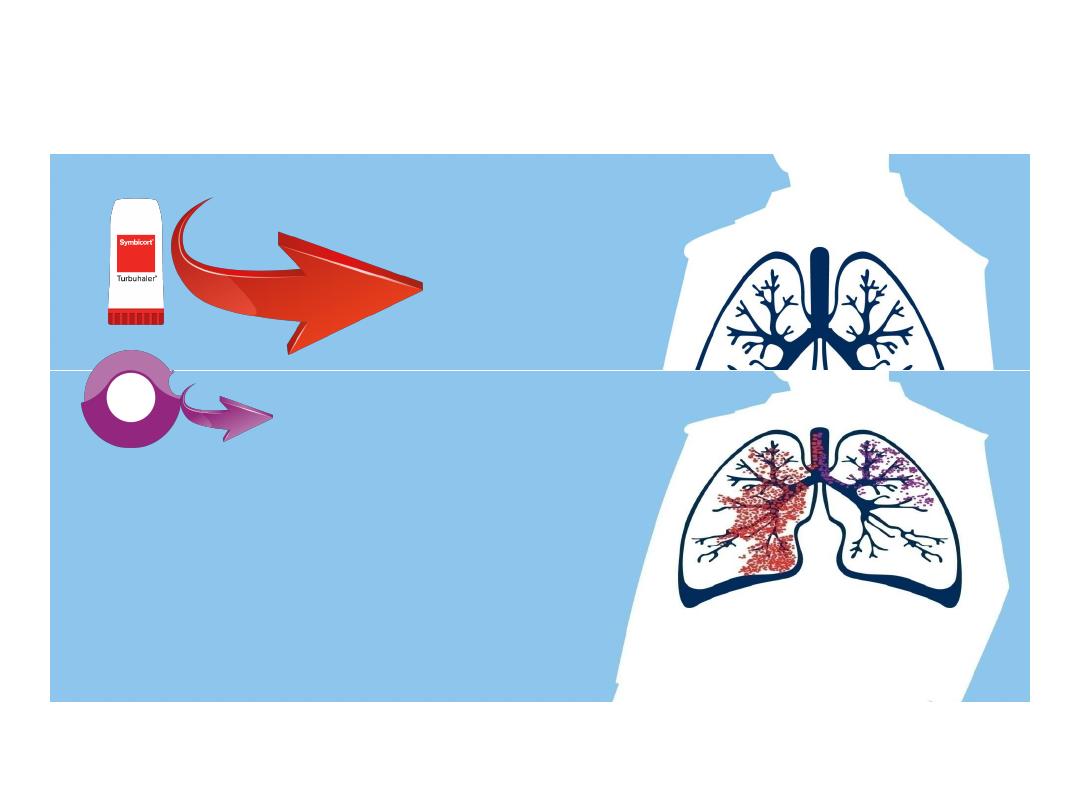
Symbicort® efficacy enhanced by Turbuhaler
Device
36%
Diskus 12%
•
Fine particles lead to higher lung
deposition that leads to higher
improvement in lung function
1-5
1. Borgstrom L et al., Int J Clin Pract, 2005, 59, 12, 1488-1495 2. Thorsson L et al., Int Journal of Pharmaceutics 168 (1998) 119-127
3. Usmani O, AM J Resp and Critical Care Medicine, vol 172 2005; 1497-1504 4. Selroos et al., Treat Resp Med 2006; 5 (suppl 48): 584S.
5. Selroos et al., Treat Resp Med 2006; 5 (5): 305-315
Device Comparison for lung deposition
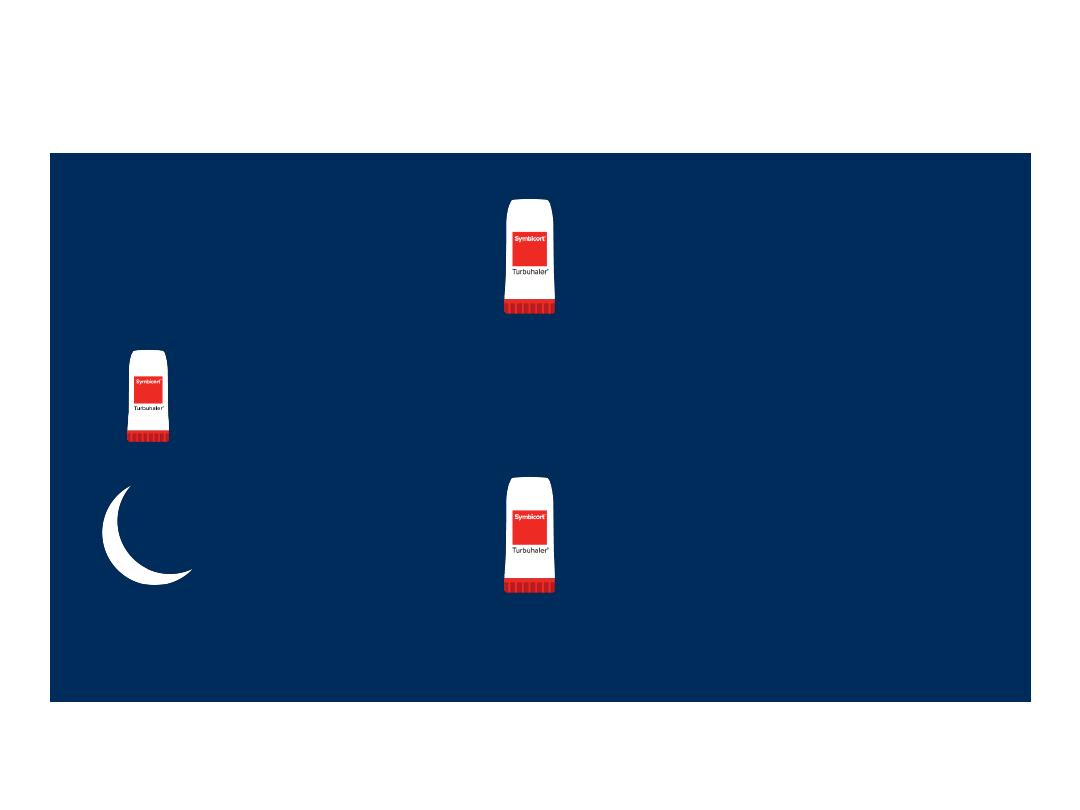
Symbicort®… The only combination
treatment offering flexibility in
prescription
1
1 inhalation
every morning
Extra doses
when needed
1 inhalation
every evening
1.
Symbicort Turbuhaler 160/4.5 mg/dose SX Leaflet text

Complication
• 1-Pnemothorax.
• 2-exacerbation.
• 3-bronchiectasis.
• 4-Respiratory failure.
• 5-Druge side effects.
Prognosis
Control can achieved as a chronic disease ,death
is uncommon.

Discussion and questions

Many thanks
50
