بسم هللا الرحمن الرحيم
18/02/2020
كلية الطب جامعة ذي قار
هيرصانلا راق يذ

Pneumonia
Dr. Majeed Mohan Alhamami
Dep. Of medicine

Objectives
To know the the following
• Etiology
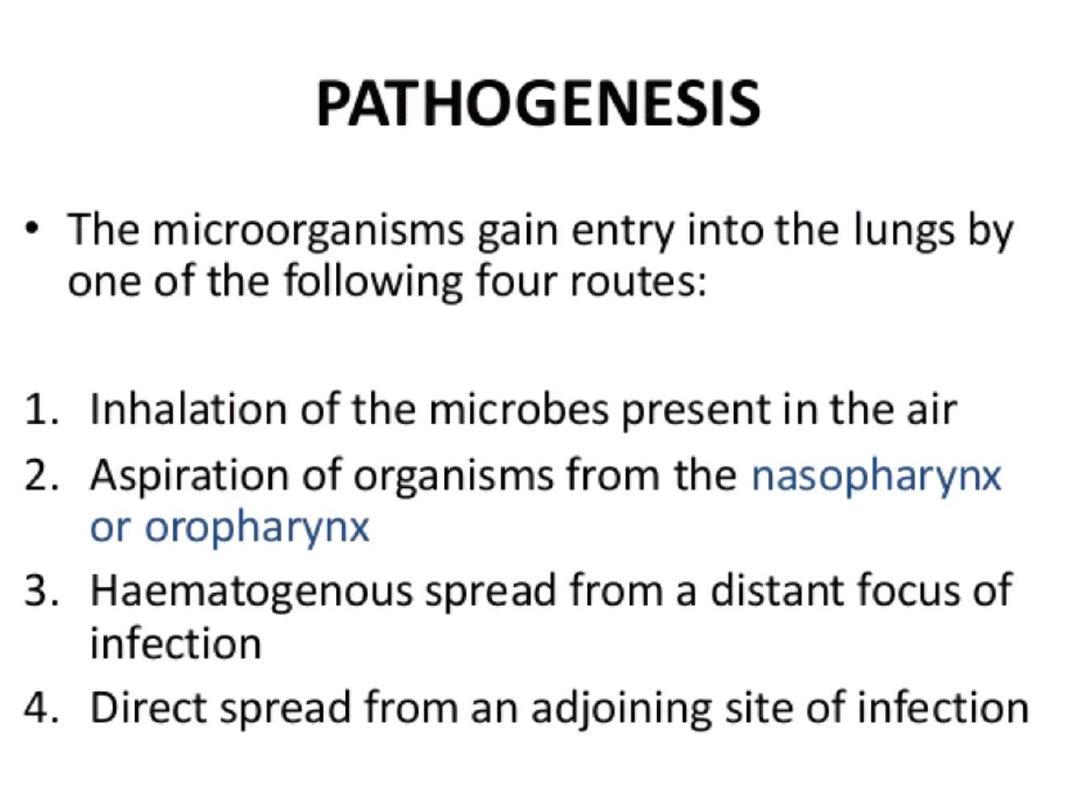
• Pathogenesis
• Clinical presentation
• Complication
• Investigation
• Treatment
• Prognosis

Community-acquired pneumonia
(CAP)
•
the sixth leading cause of death in the
United States,
•
responsible for 4 to 10 million
respiratory infections each year..
•
5-12% of all lower respiratory tract
infections.
•
The incidence varies with age, being
much higher in the very young and very
old, in
•
whom the mortality rates are also much
higher
.
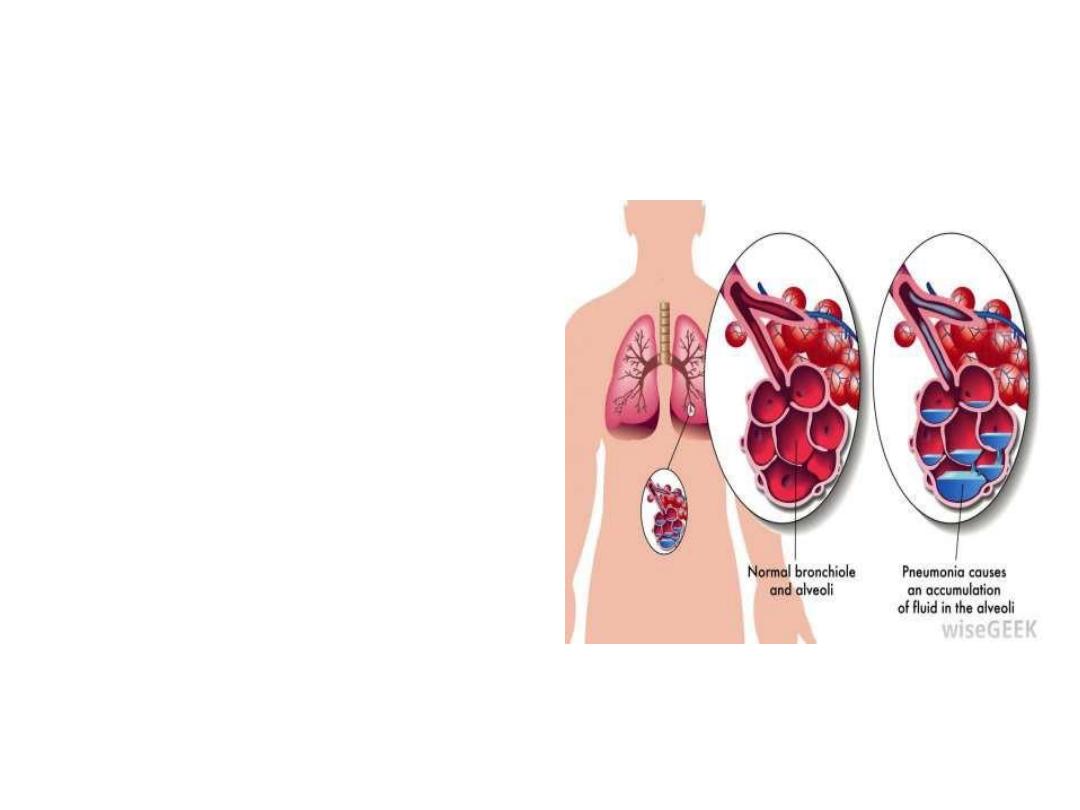
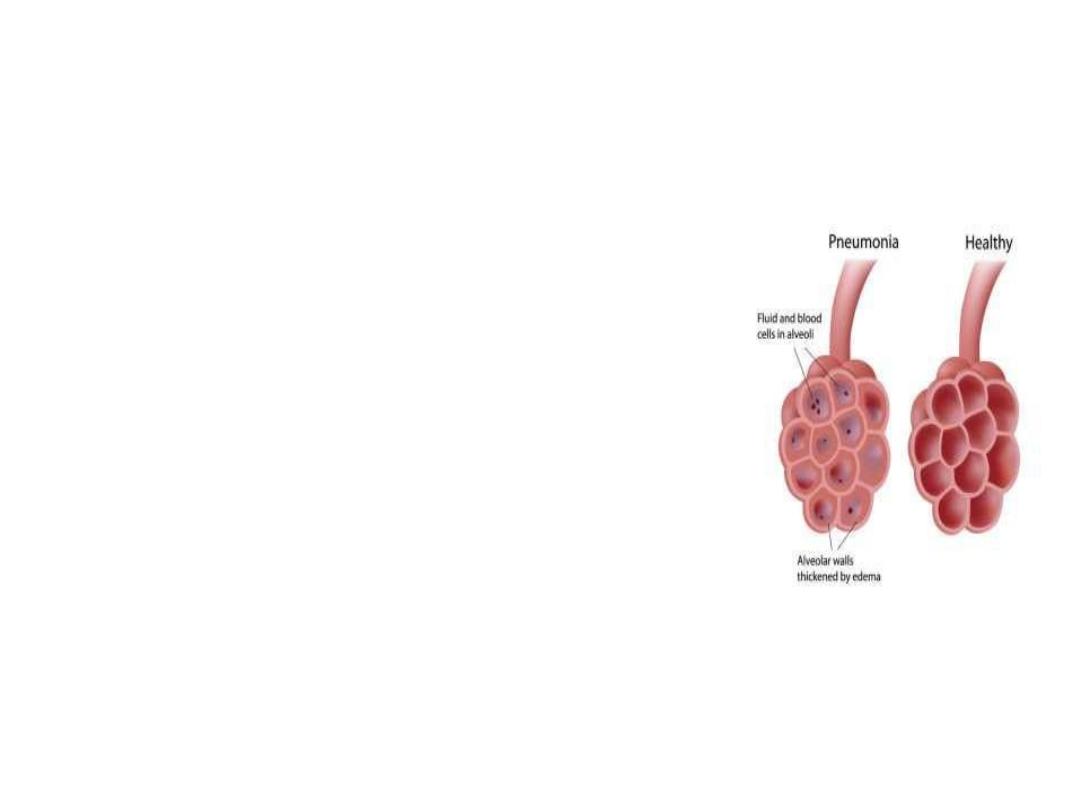
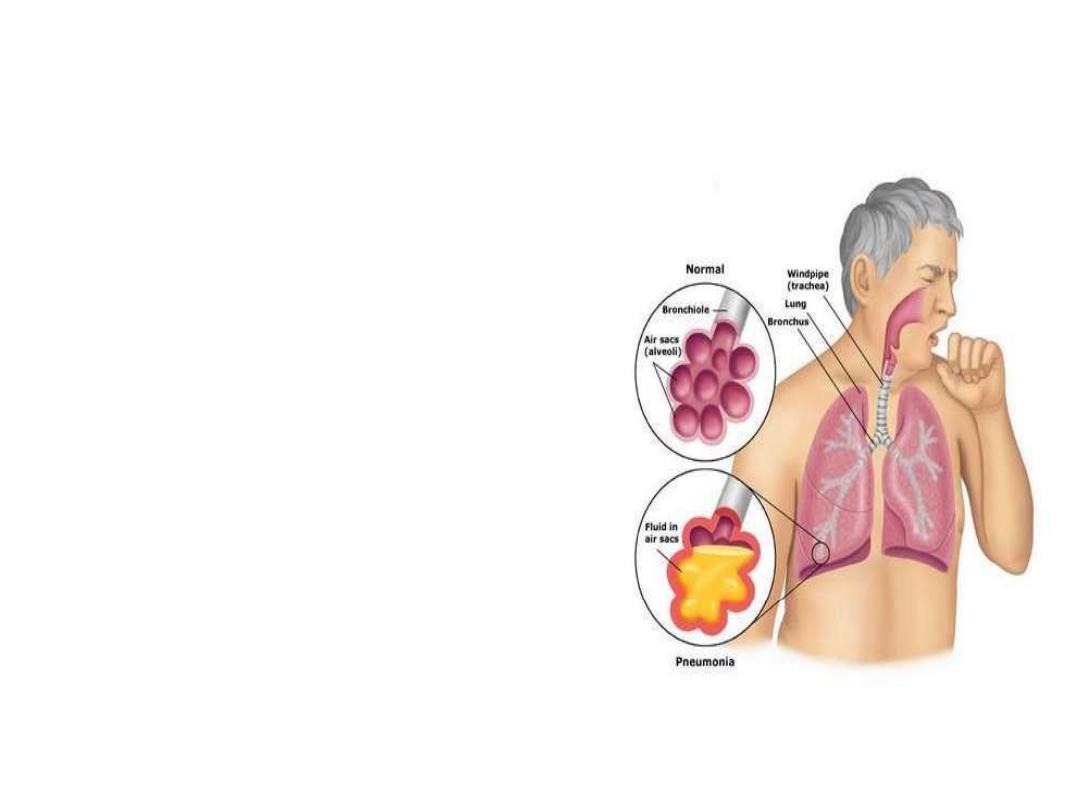
Pneumonia
Pneumonia is an infection
in one or both lungs.
Pneumonia causes
inflammation in the
alveoli.
The alveoli are filled with
fluid or pus, making it
difficult to breathe.
DEFINITION
It is as an acute respiratory illness
associated with recently developed
Pneumonia is as an acute respiratory
illness associated
with recently developed radiological
pulmonary
shadowing, which may be segmental,
lobar or multilobar.
pulmonary
shadowing, which may be
segmental, lobar or multil
COSOLIDATION =
‘Inflammatory
induration of a normally aerated lung
due to the presence of
’
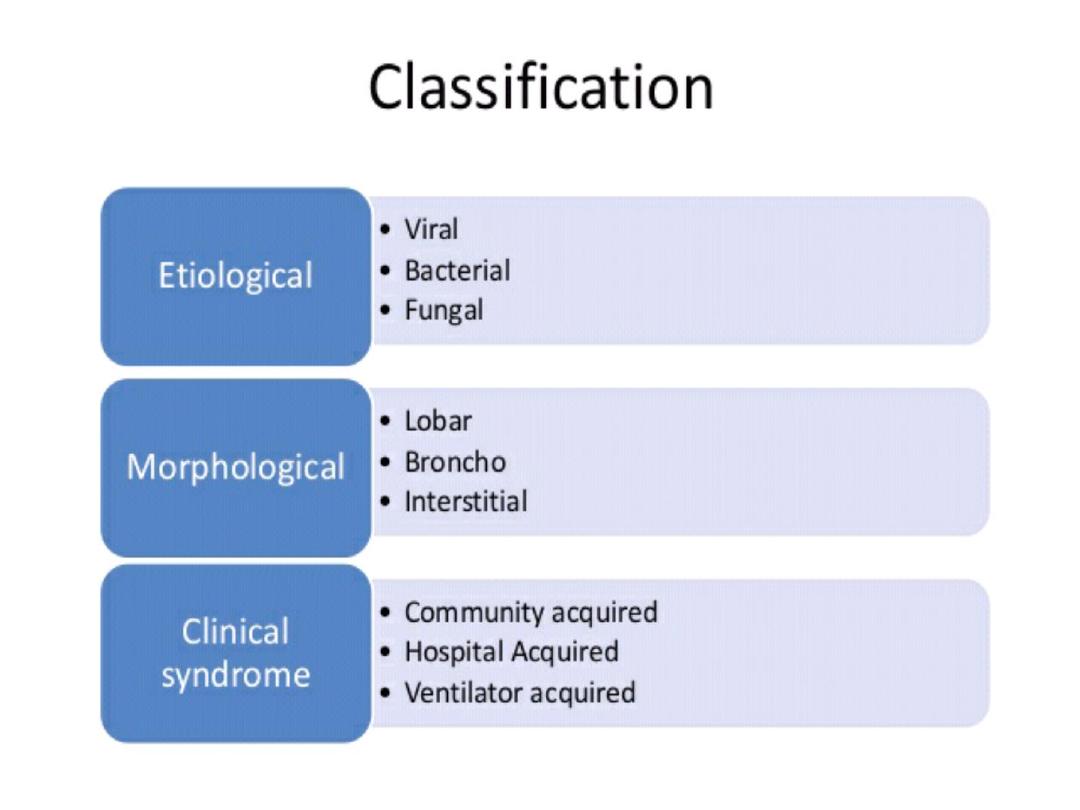

pneumonias are usually classified
Clinical
community-acquired
hospital-acquired, HCAP VAP
immunocompromised hosts. ‘
Morphological
Lobar pneumonia’ .‘
Bronchopneumonia’.
Interstitial pneumonia.
Etiological acausative organism:
bacerial,
viral ,
fungal.

Lobar and bronchopneumonia
Lobar pneumonia’ is a radiological and
pathological term referring to homogeneous
consolidation of one or more lung lobes,
often with associated pleural inflammation.
Bronchopneumonia’ refers to more patchy
alveolar consolidation associated with
bronchial and bronchiolar inflammation, often
affecting both lower lobes.

The inflammatory response in lobar
pneumonia
Evolves through stages of
Congestion,
Red hepatisation
Grey hepatisation,
finally resolution.
.
Congestion
•
Presence of a
proteinaceous
exudate
—
and often of bacteria
—
in the alveoli
RED HEPATIZATION
•
Presence of
erythrocytes
in the
cellular intraalveolar exudate
•
Neutrophils are also present
•
Bacteria are occasionally seen in
cultures of alveolar specimens
collected
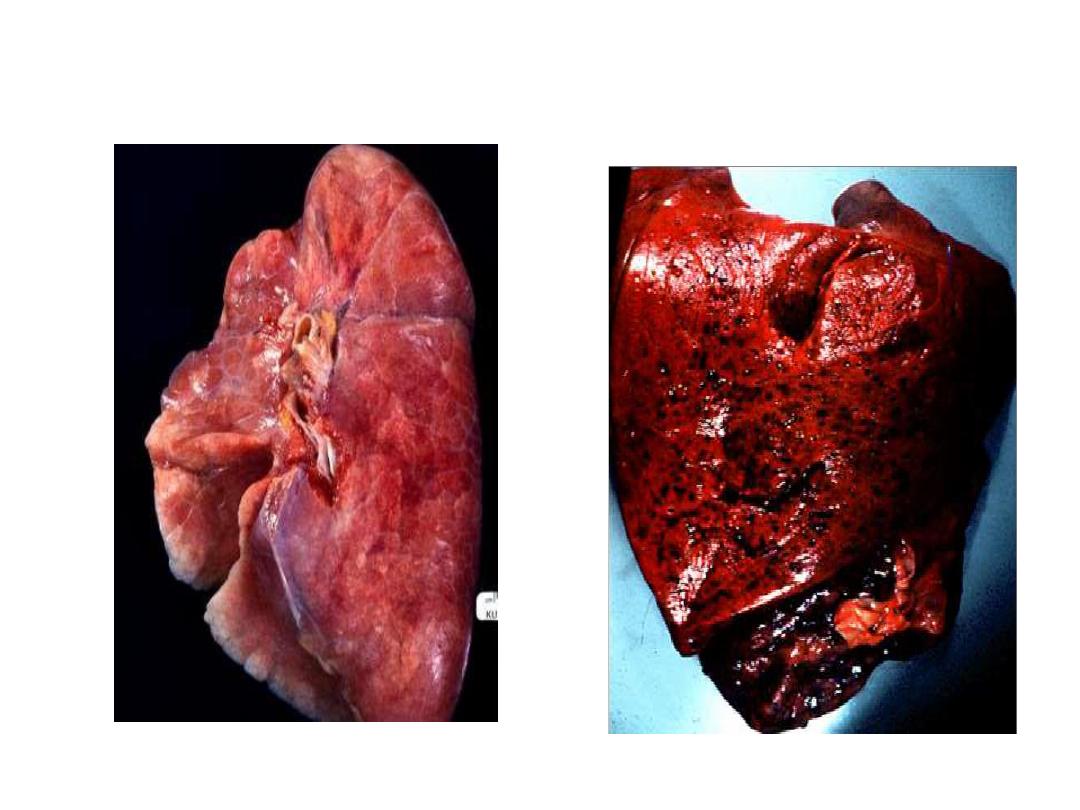
Normal Lung
Red Hepatization

GRAY HEPATIZATION
•
No new erythrocytes are extravasating, and those
already present have been lysed and degraded
•
Neutrophil is the predominant cell
•
Fibrin deposition is abundant
•
Bacteria have disappeared
•
Corresponds with successful containment of the
infection and improvement in gas exchange
Factors that predispose to Pneumonia
Cigarette smoking
• Upper respiratory tract infections
• Alcohol
• Corticosteroid therapy
• Old age
• Recent influenza infection
• Pre-existing lung disease
• HIV
• Indoor air pollution

Organisms causing community-acquired pneumonia
Bacteria
• Streptococcus pneumoniae
• Mycoplasma pneumoniae
• Legionella pneumophila
• Chlamydia pneumoniae
• Haemophilus influenzae
• Staphylococcus aureus
Chlamydia psittaci
• Coxiella burnetii (Q fever,
‘querry’ fever)
• Klebsiella pneumoniae
(Freidlنnder’s bacillus)
• Actinomyces israelii

Organisms causing community-acquired pneumonia
Viruses
• Influenza, parainfluenza
• Measles
• Herpes simplex
• Varicella
• Adenoviruse
Cytomegalovirus (CMV)
(
• Coronavirus (Urbani ARS-associated
coronavirusus

Clinical features
• Pneumonia, particularly lobar pneumonia, usually
presents as an acute illness.
Systemic features such as
• fever,
• rigors, shivering
• malaise
• delirium .
• Decrease appetite .
• headache.

Clinical features
• Pulmonary symptoms
• cough, which at first is short, painful and dry,
but later accompanied by the expectoration of
mucopurulent sputum.
• Rust-coloured sputum may be seen in patients
with Strep. pneumoniae,
• may report haemoptysis.
• Pleuritic chest pain.
• Upper abdominal tenderness .

On examination
• the respiratory and pulse rate may be raised
• the blood pressure low,
• delirium.
• Temperature may be normal
• Oxygen saturation on air may be low, and the
patient cyanosed and distressed.
• Herpes labialis-----Streptococcal pneumonia
• poor dental hygiene ----Klebsiella or Actinomyces
israelii

Chest signs
depending on the phase of the inflammatory
response.
• When consolidated, the lung is
• typically dull to percussion ,
• bronchial breathing and whispering
pectoriloquy; crackles areheard throughout.
However, in many patients, signs are more
subtle with reduced air entry only, but
crackles are usually present.


Prevention
smokers should be advised to stop.
Influenza and pneumococcal vaccination should be considered in
selected patients .
Legionella pneumophila requires notification to the appropriate
health authority.
In developing countries, tackling
malnourishment and indoor air pollution, and encouraging
immunisation against measles, pertussis and Haemophilus
influenzae type b are particularly important in
children.

Differential diagnosis of pneumonia
• Pulmonary infarction
• • Pulmonary/pleural TB
• • Pulmonary oedema (can be unilateral)
• • Pulmonary eosinophilia .
• • Malignancy: bronchoalveolar cell carcinoma
• • Rare disorders: cryptogenic organising
pneumonia/
bronchiolitis obliterans organising pneumonia
(COP/BOOP

Investigations in CAP
Blood
•
Full blood count
• Very high (> 20 × 109/L) or low (< 4 × 109/L) white cell
count: marker of severity
• Neutrophil leucocytosis > 15 × 109/L: suggests bacterial
aetiology
• Haemolytic anaemia: occasional complication of Mycoplasma
•
Urea and electrolytes
• Urea > 7 mmol/L (~20 mg/dL): marker of severity
• Hyponatraemia: marker of severity
•
Liver function tests
• Abnormal if basal pneumonia inflames liver
• Hypoalbuminaemia: marker of severity
•
Erythrocyte sedimentation rate/C-reactive protein
• Non-specifically elevated

Investigations in CAP
Blood
• Blood culture
• Bacteraemia: marker of severity
• Serology
• Acute and convalescent titres for Mycoplasma, Chlamydia,
Legionella and viral infections
• Cold agglutinins
• Positive in 50% of patients with Mycoplasma
• Arterial blood gases
• Measure when SaO2 < 93% or when severe clinical features
to assess ventilatory failure or acidosis

Investigations in CAP
Sputum
• Sputum samples
• Gram stain culture and antimicrobial sensitivity
testing
• Oropharynx swab
• PCR for Mycoplasma pneumoniae and other
atypical
pathogens
• Urine
• Pneumococcal and/or Legionella antigen

Investigations in CAP
Chest X-ray and Ultrasound
Lobar pneumonia
• Patchy opacification ,consolidation.
• Air bronchogram (air-filled bronchi appear lucent against
consolidated lung tissue)
Bronchopneumonia
• Typically patchy and segmental shadowing
Complications
Staph. aureus
• multilobar shadowing, cavitation, pneumatocoeles and abscesses.
Pleural fluid
• • Always aspirate and culture.
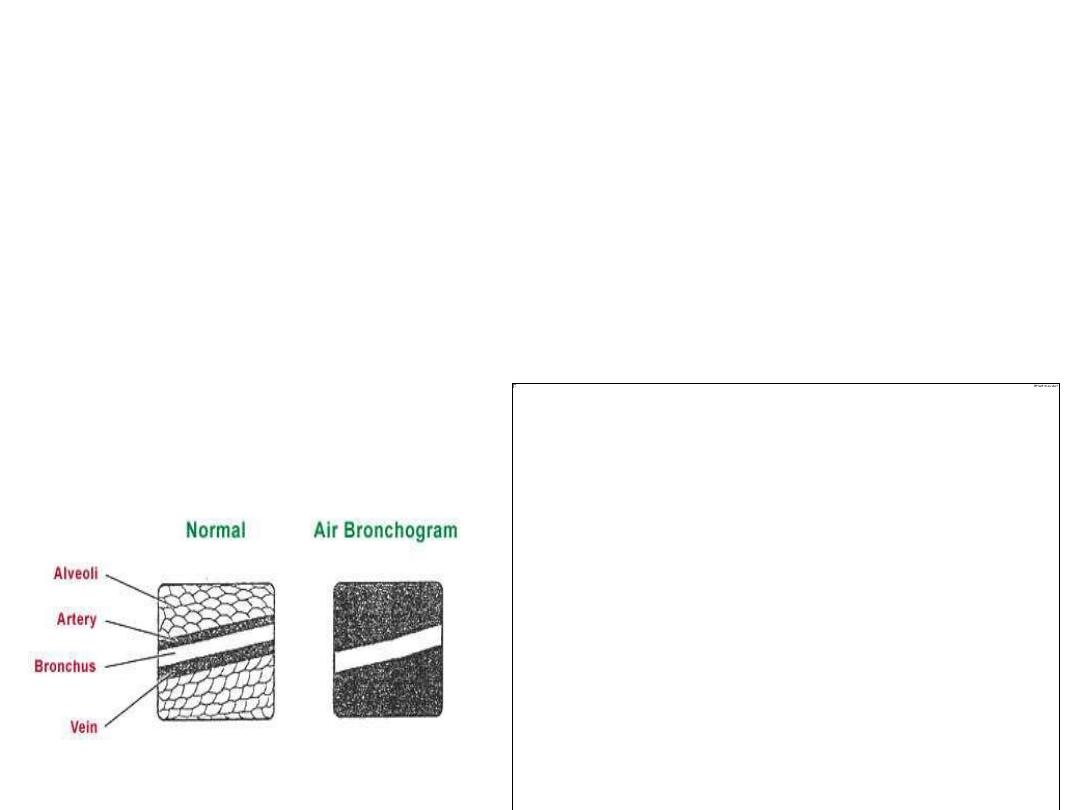
X Ray
Homogenous opacity with
air
bronchogram
LOBAR PNEUMONIA
•
Peripheral airspace consolidation pneumonia
•
Without prominent involvement of the bronchial tree
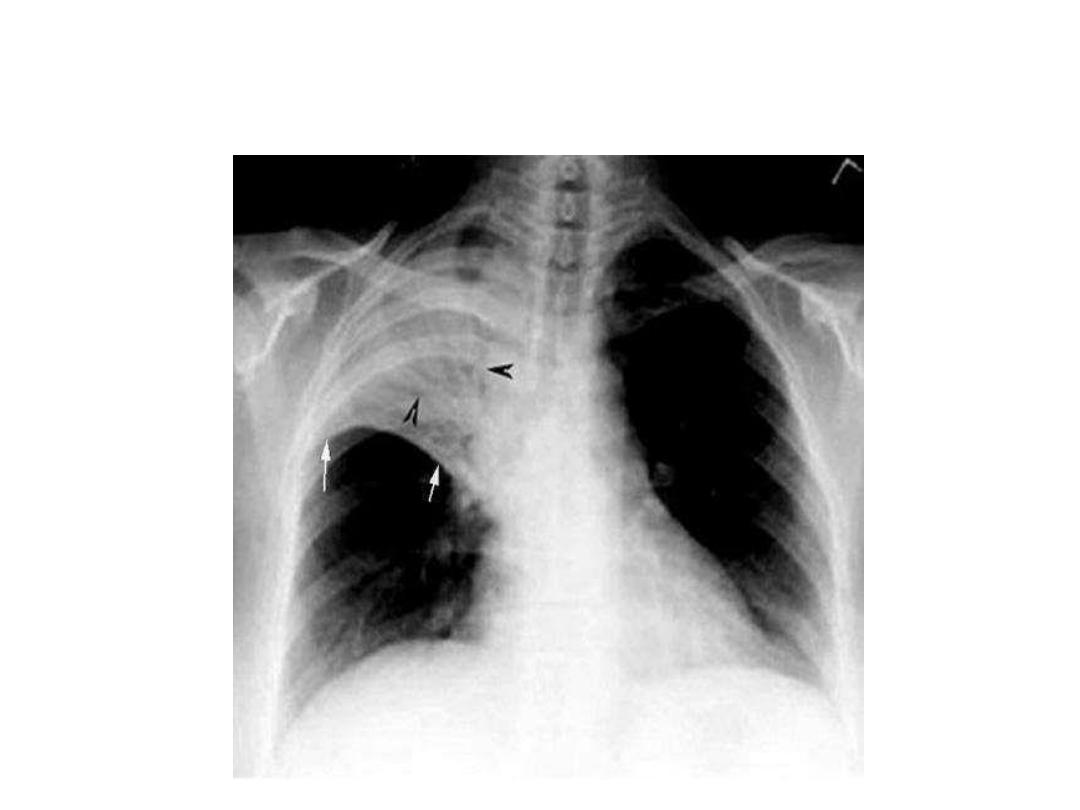
RUL Consolidation
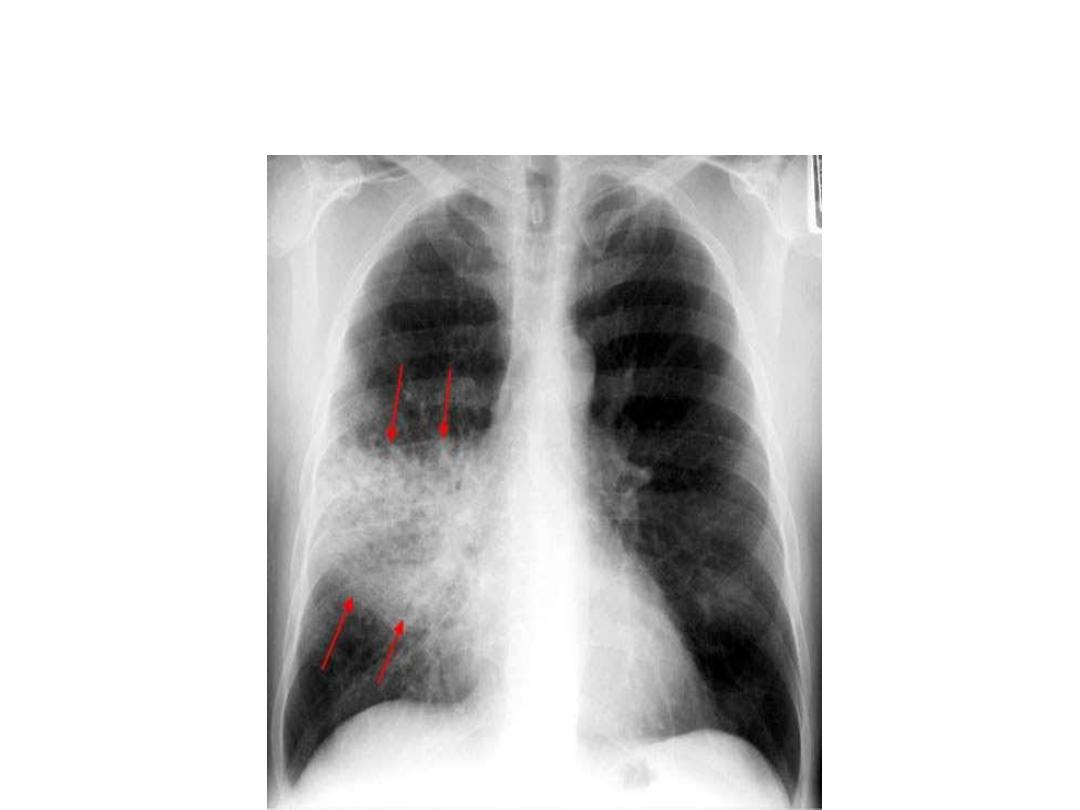
RML Consolidation
RLL Consolidation
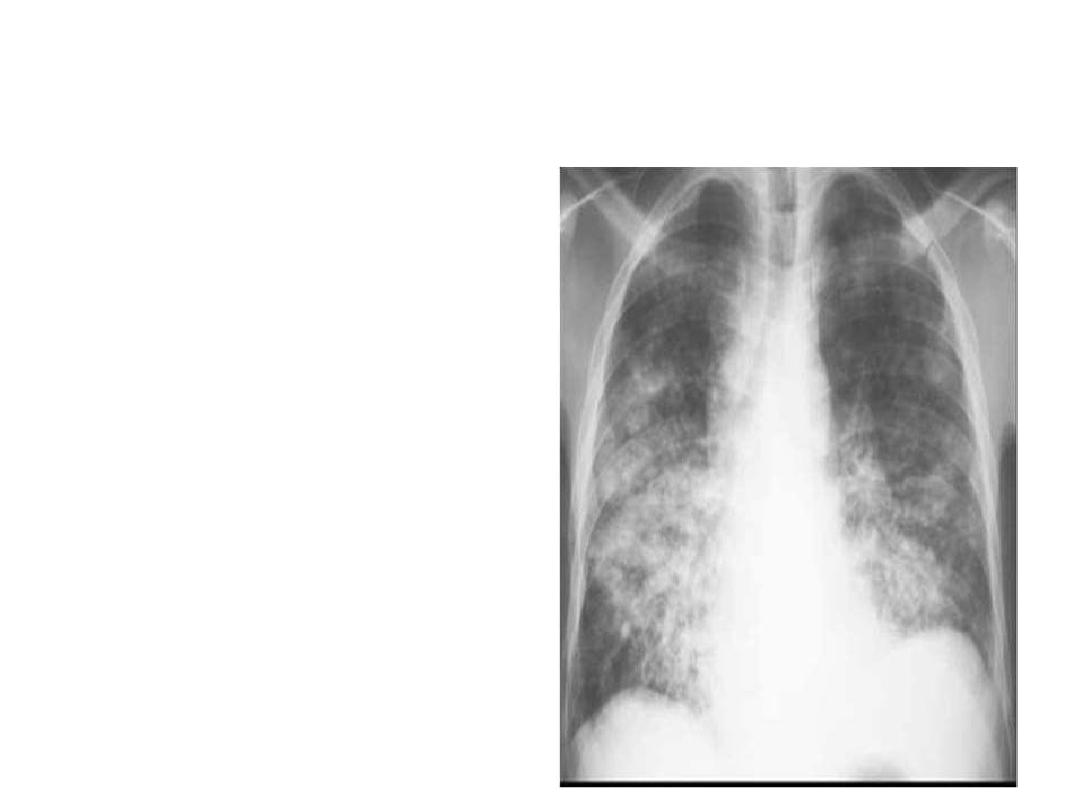
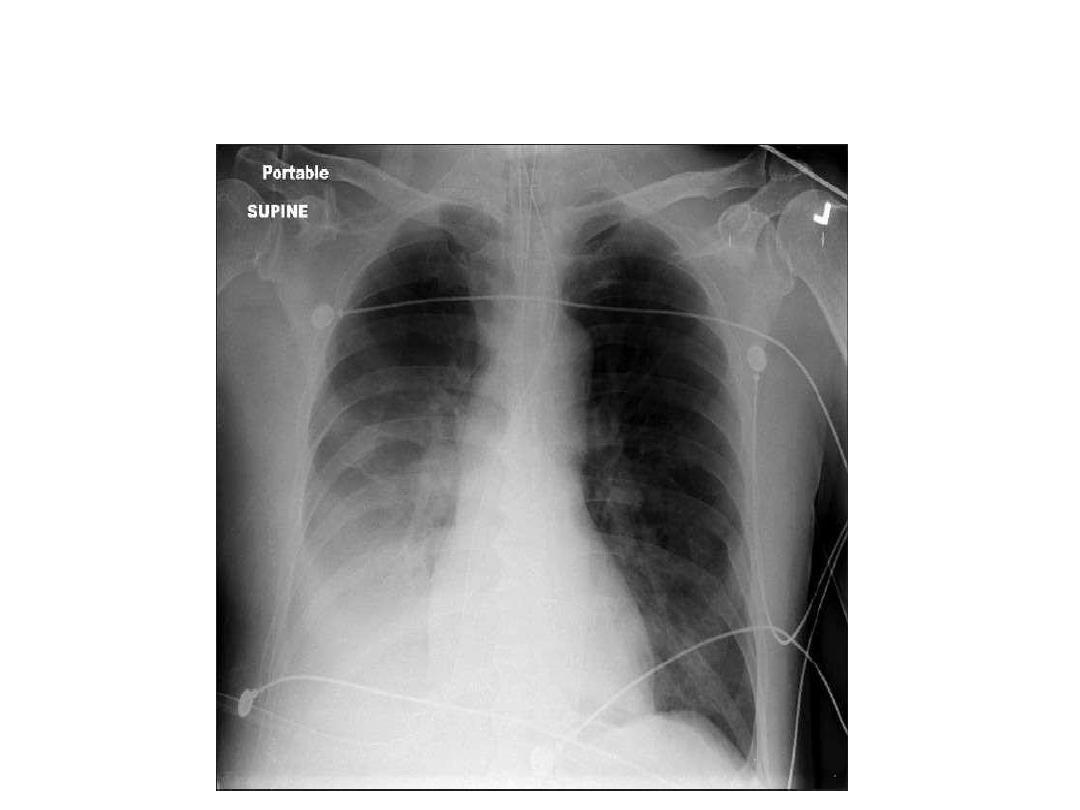
BRONCHOPNEUMONIA
•
Centrilobular and
Peribronchiolar opacity
pneumonia
•
T
ends to be
multifocal
•
Patchy
in distribution
rather than localized to any
one lung region
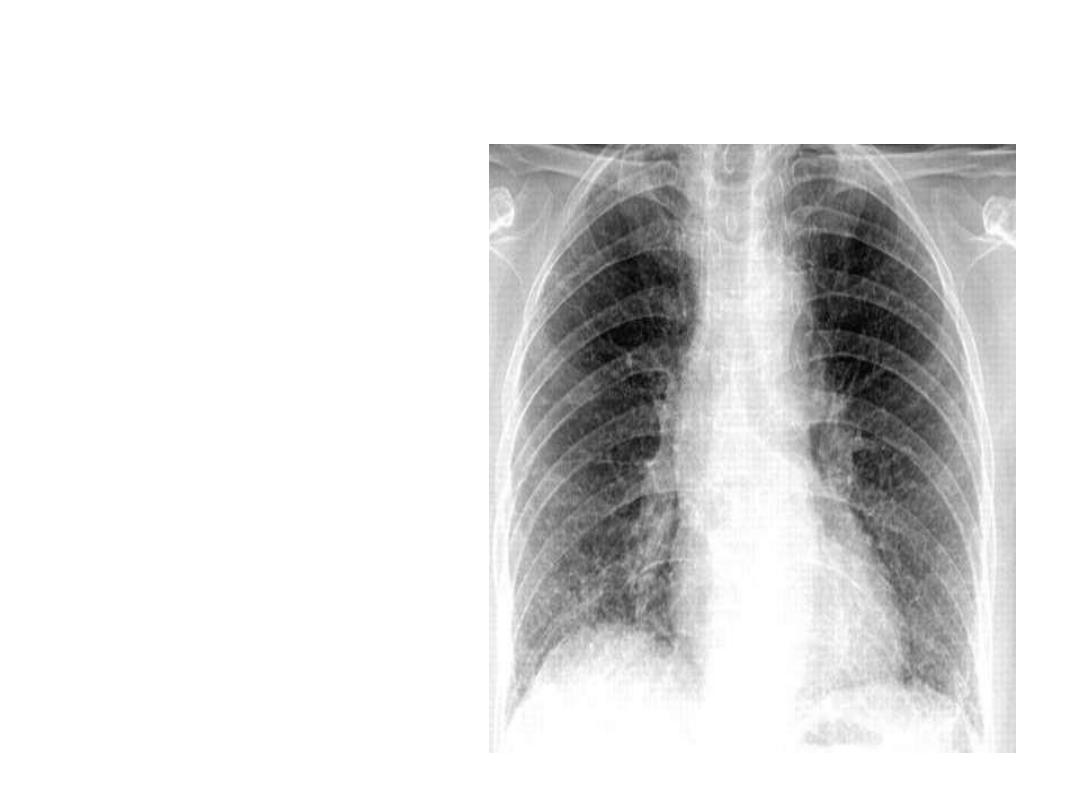
INTERSTITIAL PNEUMONIA
•
Peribronchovascular
Infiltrate
•
Mycoplasma , viral
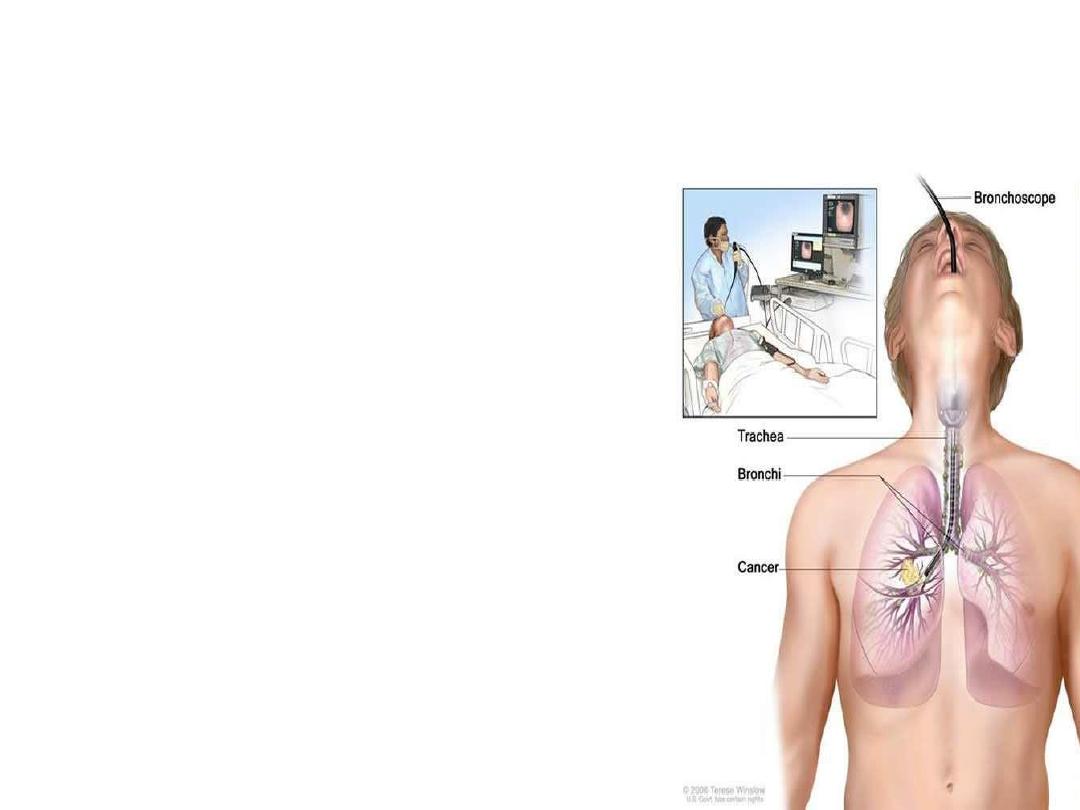
INVASIVE
•
Bronchoscopy
•
Thoracoscopy
•
Percutaneous aspiration/biopsy
•
Open lung biopsy
•
Pleural aspiration
Hospital CURB-65.
*
Defined as a Mental Test Score of 8 or less, or new disorientation in person,
place or time. ( Urea of 7 mmol/L ≅20 mg/dl

Indications for referral to ITU
CURB score of 4–5, failing to respond rapidly to
initial
management
• Persisting hypoxia (PaO2 < 8 kPa (60 mmHg)),
despite high concentrations of oxygen
• Progressive hypercapnia
• Severe acidosis
• Circulatory shock
• Reduced conscious level

Complications of pneumonia
• Para-pneumonic effusion – common
• Empyema .
• lobar collapse
• Deep vein thrombosis and pulmonary embolism
• Pneumothorax, particularly with Staph. aureus
• Suppurative pneumonia/lung abscess
• ARDS, renal failure, multi-organ failure .
• Ectopic abscess formation (Staph. aureus)
• Hepatitis, pericarditis, myocarditis, meningoencephalitis
• Pyrexia due to drug hypersensitivity
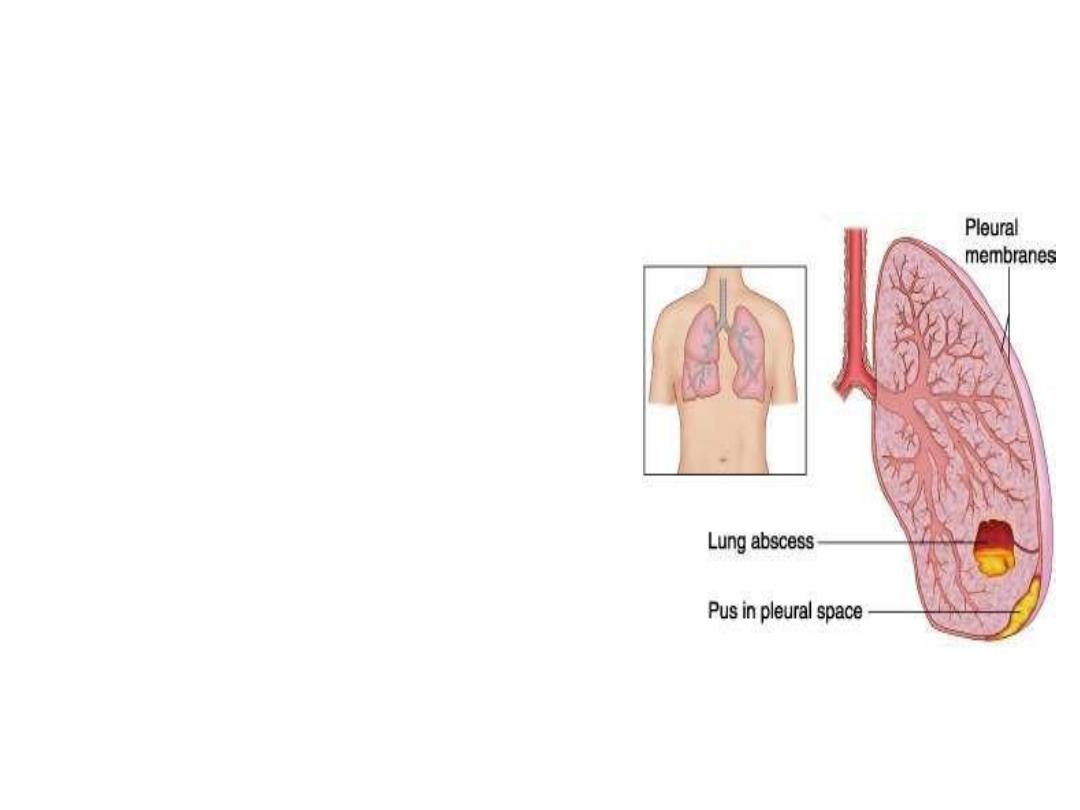
COMPLICATIONS
•
Lung abscess
•
Para-pneumonic effusions
•
Empyema
•
Sepsis
•
Metastatic infections
(meningitis,endocarditis,arthritis)
•
ARDS , Respiratory failure
•
Circulatory failure
•
Renal failure
•
Multi-organ failure
Management
The most important aspects of management are
Oxygenation,
Fluid balance
Antibiotic therapy.
Nutritional support in severe or prolonged
illness,

Oxygen
tachypnoea,
hypoxaemia,
hypotension
acidosis,
The aim of maintaining the PaO2 at or above 8 kPa
(60 mmHg) or the SaO2 at or above 92%.
High concentrations (35% or more), preferably humidified, should be
used in all patients who do not have hypercapnia associated
with COPD.
Continuous positive airway pressure (CPAP) for hypoxic despite this,
managed in a high-dependency or intensive care environment,

Intravenous fluids
o severeillness,
o older patients
o vomiting.
o Otherwise, an adequate oral intake of fluid
should
o be encouraged.
o Inotropic support may be required in patients
with shock

Antibiotic treatment for CAP
Antibiotics improves the outcome.
The initial choice of antibiotic is guided by
clinical context,
severity assessment,
local knowledge of antibiotic resistance
patterns
any available epidemiological information.

Antibiotic treatment for CAP
Uncomplicated CAP
• Amoxicillin 500 mg 3 times daily orally
If patient is allergic to penicillin
• Clarithromycin 500 mg twice daily orally or Erythromycin
500 mg 4 times daily orally
If Staphylococcus is cultured or suspected
• Flucloxacillin 1–2 g 4 times daily IV plus
• Clarithromycin 500 mg twice daily IV
If Mycoplasma or Legionella is suspected
• Clarithromycin 500 mg twice daily orally or IV or
Erythromycin 500 mg 4 times daily orally IV plus
• Rifampicin 600 mg twice daily IV in severe cases

Antibiotic treatment for CAP
Severe CAP
•
Clarithromycin 500 mg twice daily IV or Erythromycin 500 mg
4 times daily IV plus
• Co-amoxiclav 1.2 g 3 times daily IV or Ceftriaxone 1–2 g
daily IV or Cefuroxime 1.5 g 3 times daily IV or
• Amoxicillin 1 g 4 times daily IV plus flucloxacillin 2 g 4
timesdaily IV

Discharge and follow-up
The decision to discharge patients depends on
their home circumstances and the likelihood
of complications.
Clinical review should be arranged around 6
weeks later and a chest X-ray obtained if there
are persistent symptoms,physical signs or
reasons to suspect underlying malignancy.

Thank you

Q
• QUIZE
