1
L1
D. Faez
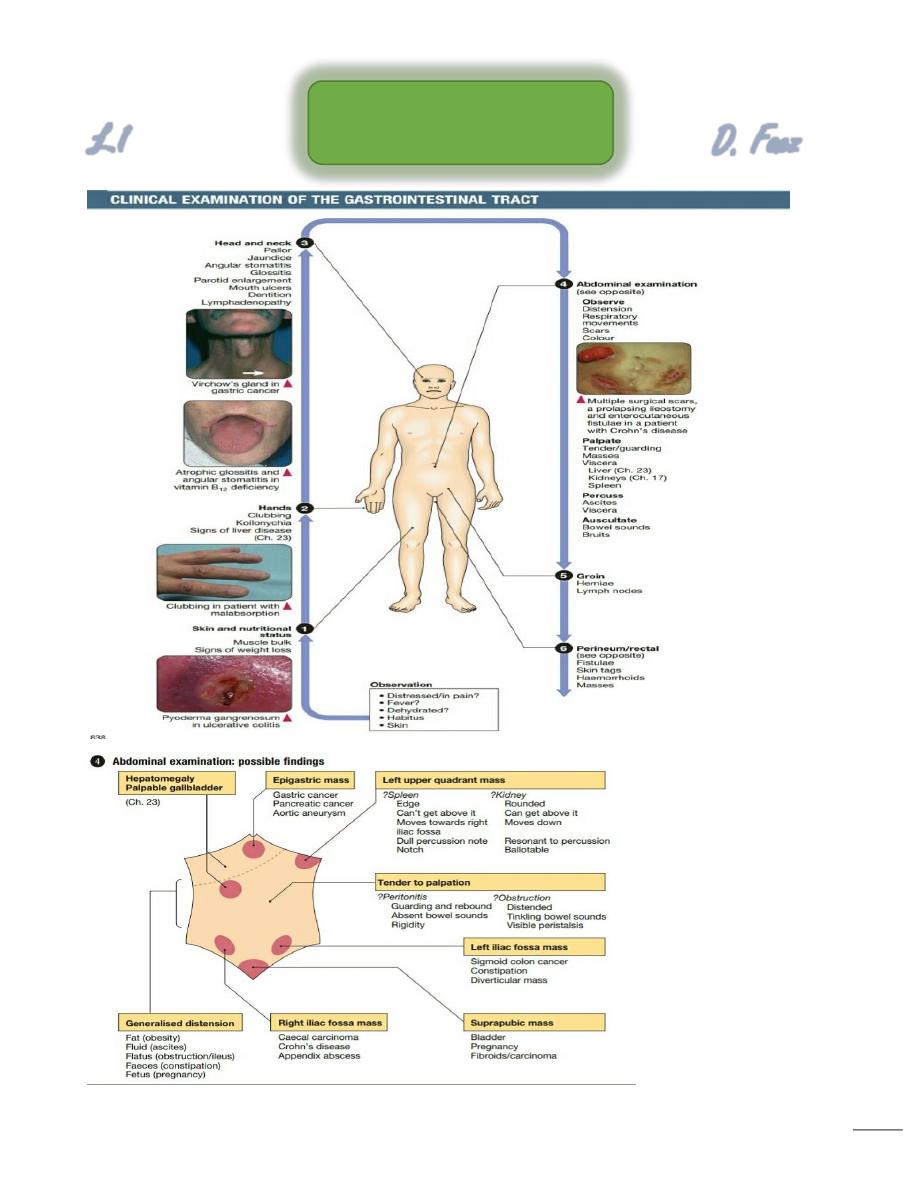
GIT Introduction
2
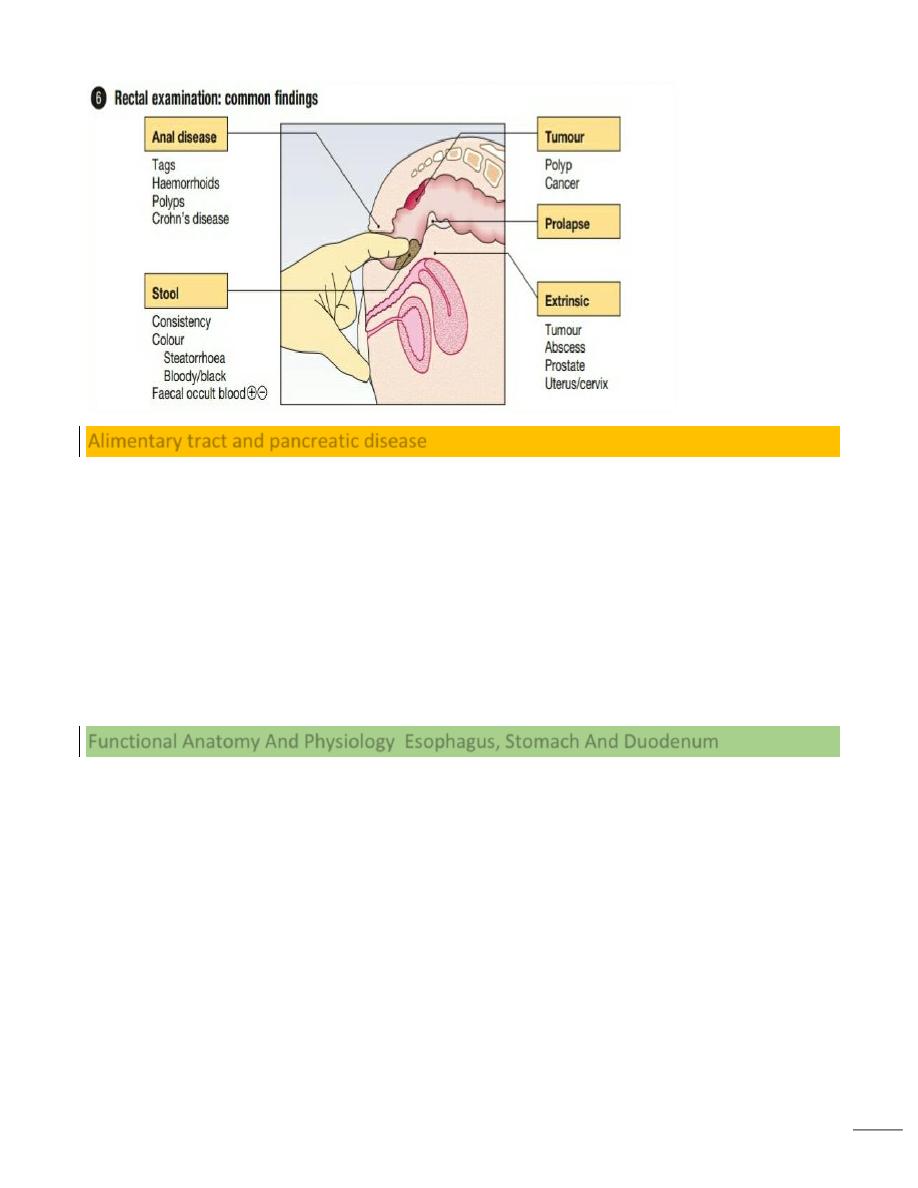
Alimentary tract and pancreatic disease
Diseases of the gastrointestinal tract are a major cause of morbidity and mortality.
Infective diarrhoea and malabsorption are responsible for much ill health and many
deaths in the developing world.
The gastrointestinal tract is the most common site for cancer development. Colorectal
cancer is the second most common cancer in men.
Functional bowel disorders affect up to 10–15% of the population .
The inflammatory bowel diseases, Crohn’s disease and ulcerative colitis, together affect
1 in 250 people in the Western world, with substantial associated morbidity.
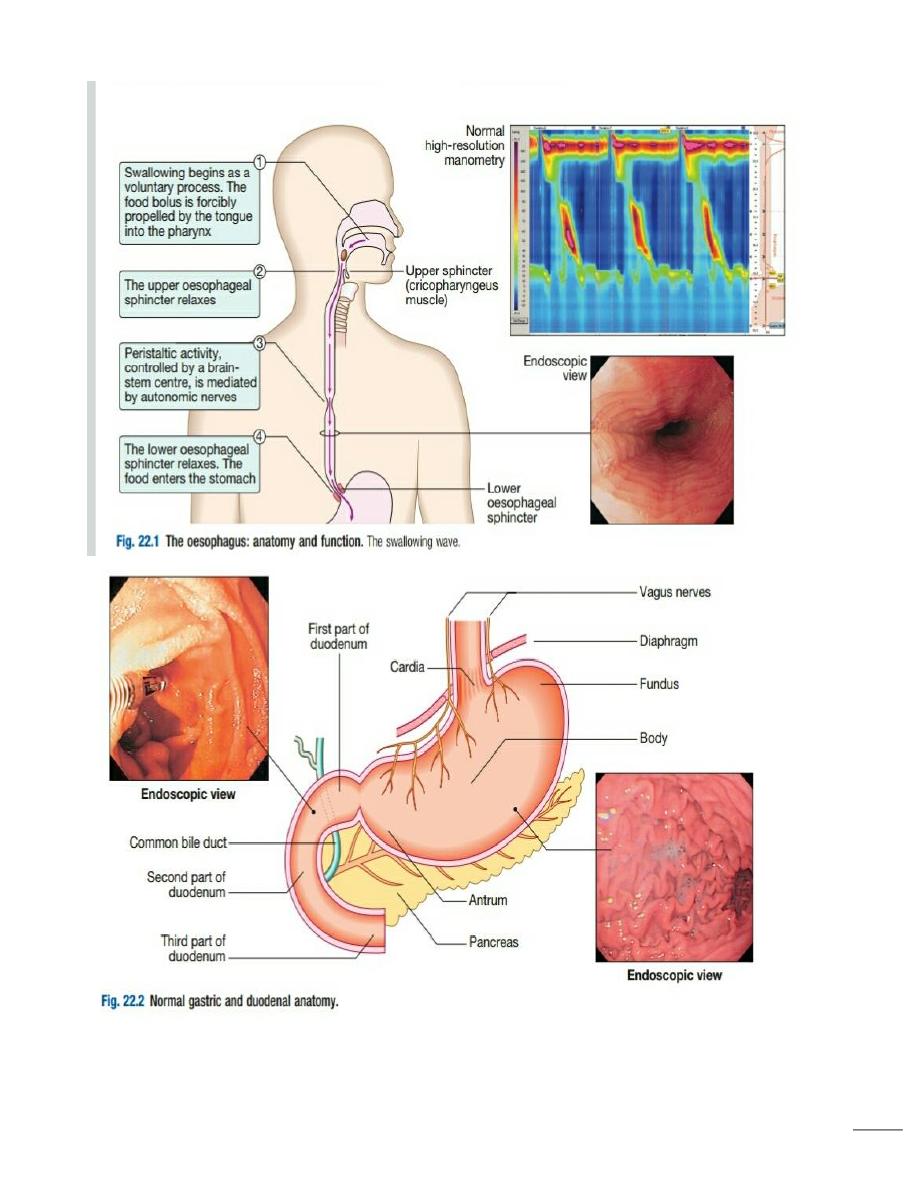
Functional Anatomy And Physiology Esophagus, Stomach And Duodenum
This muscular tube extends 25 cm from the cricoid cartilage to the cardiac orifice of the
stomach.
It has an upper and a lower sphincter.
A peristaltic swallowing wave propels the food bolus into the stomach
The stomach acts as a ‘hopper’, retaining and grinding food, then actively propelling it
into the upper small bowel
3
4
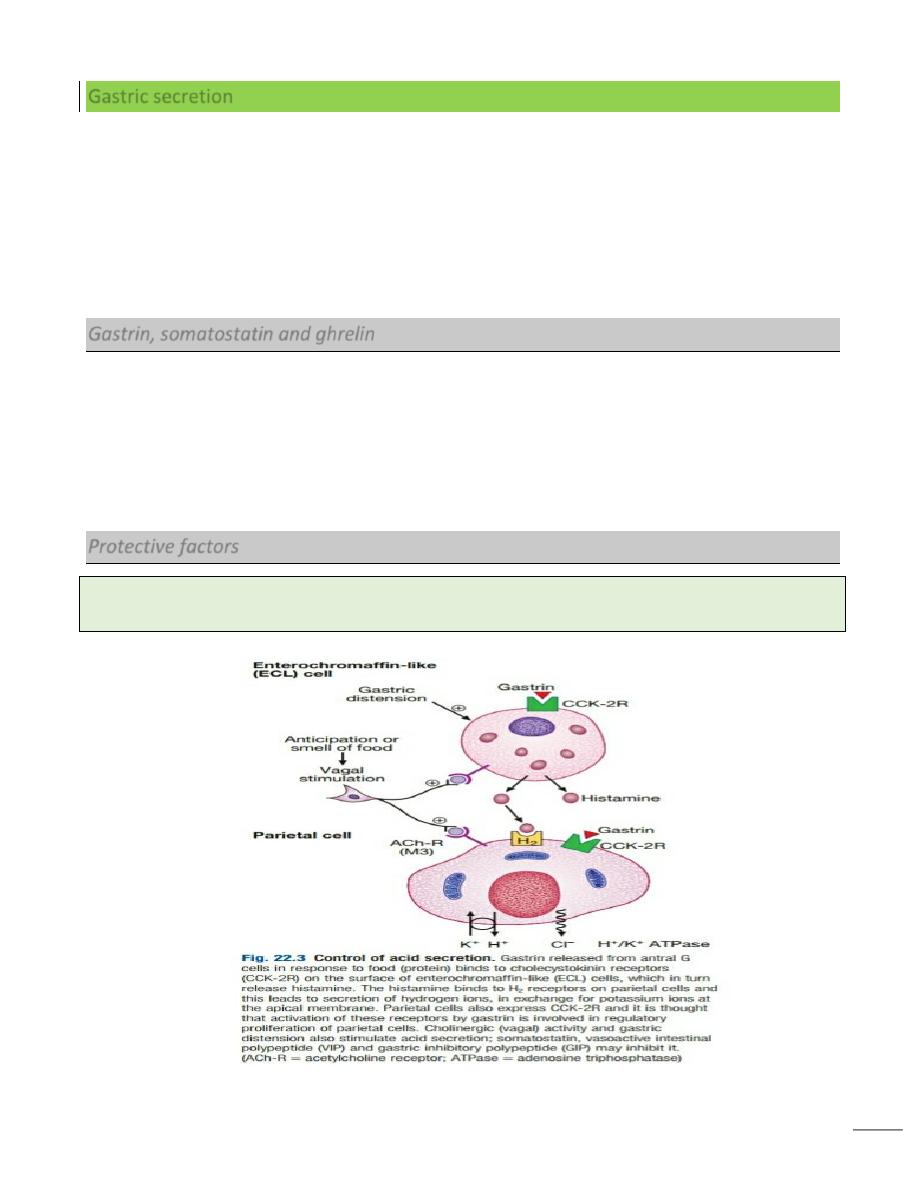
Gastric secretion
Gastrin, histamine and acetylcholine are the key stimulants of acid secretion.
Hydrogen and chloride ions are secreted from the apical membrane of gastric parietal
cells into the lumen of the stomach by a hydrogen– potassium adenosine
triphosphatase (ATPase) (‘proton pump’).
The hydrochloric acid sterilises the upper gastrointestinal tract and converts
pepsinogen – which is secreted by chief cells – to pepsin.
The glycoprotein intrinsic factor, secreted in parallel with acid, is necessary for
vitamin B12 absorption.
Gastrin, somatostatin and ghrelin
The hormone gastrin is produced by G cells in the antrum, whereas somatostatin is
secreted from D cells throughout the stomach.
Gastrin stimulates acid secretion and mucosal growth, whilst somatostatin suppresses it.
Ghrelin, secreted from oxyntic glands, stimulates acid secretion but also appetite and
gastric emptying.
Protective factors
Bicarbonate ions, stimulated by prostaglandins, mucins and trefoil factor family (TFF) peptides
together protect the gastroduodenal mucosa from the ulcerative properties of acid and pepsin.
5
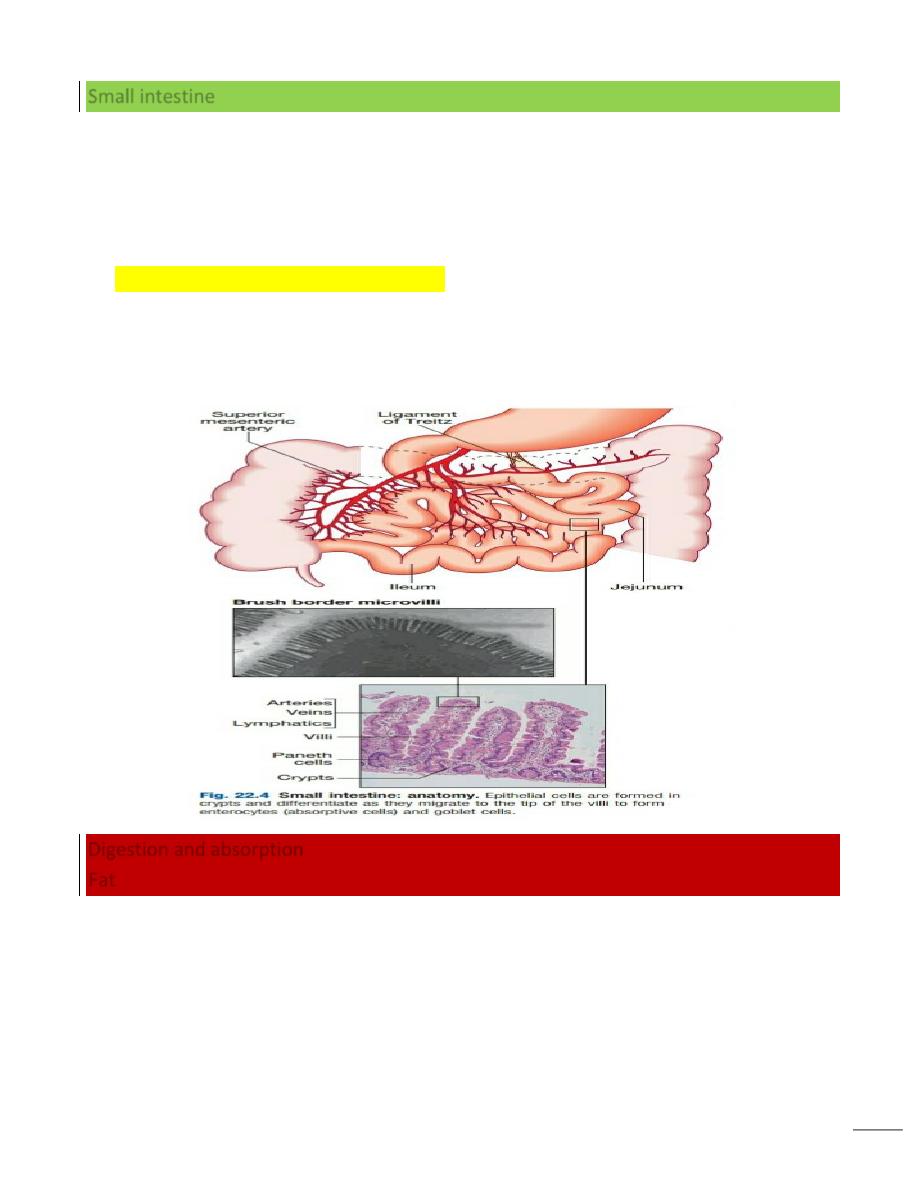
Small intestine
The small bowel extends from the ligament of Treitz to the ileocaecal valve.
During fasting, a wave of peristaltic activity passes down the small bowel every 1–2
hours.
Entry of food into the gastrointestinal tract stimulates small bowel peristaltic activity.
Functions of the small intestine are:
1. digestion (mechanical, enzymatic and peristaltic)
2. absorption – the products of digestion, water, electrolytes and vitamins
3. protection against ingested toxins
4. Immune regulation.
Digestion and absorption
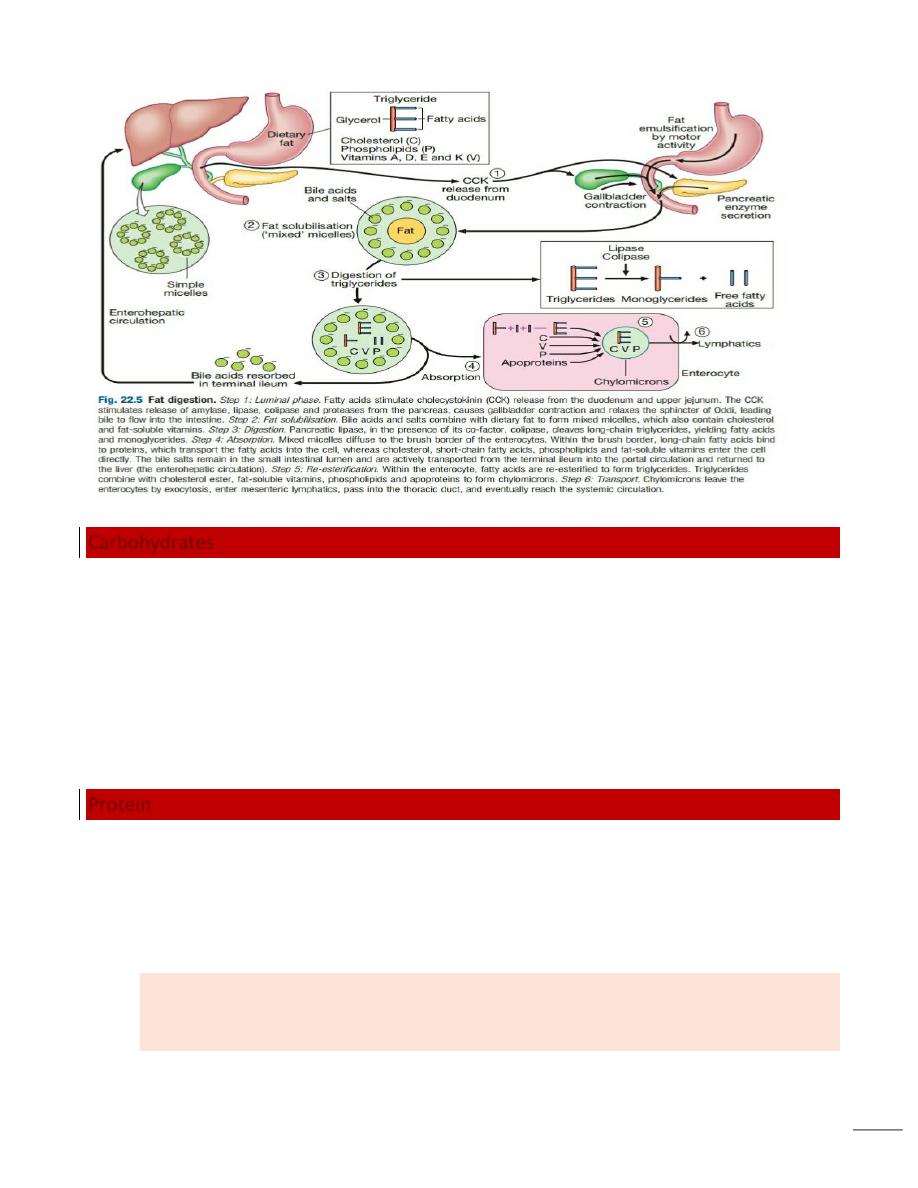
Fat
Dietary lipids comprise long-chain triglycerides, cholesterolesters and lecithin.
Lipids are insoluble in water and undergo lipolysis and incorporation into mixed
micelles before they can be absorbed into enterocytes along with the fat-soluble
vitamins A, D, K and E.
The lipids are processed within enterocytes and pass via lymphatics into the systemic
circulation.
Fat absorption and digestion can be considered as a stepwise process..
6
Carbohydrates
Starch is hydrolysed by salivary and pancreatic amylases to alpha-limit dextrins
containing 4–8 glucose molecules; to the disaccharide, maltose; and to the trisaccharide,
maltotriose.
Disaccharides are digested by enzymes fixed to the microvillous membrane to form the
monosaccharides, glucose, galactose and fructose.
Glucose and galactose enter the cell by an energy-requiring process involving a carrier
protein, and fructose enters by simple diffusion.
Protein
Intragastric digestion by pepsin is quantitatively modest but important because the
resulting polypeptides and amino acids stimulate CCK release from the mucosa of the
proximal jejunum, which in turn stimulates release of pancreatic proteases, including
trypsinogen, chymotrypsinogen, pro-elastases and procarboxypeptidases, from the
pancreas.
On exposure to brush border enterokinase, inert trypsinogen is converted to the
active proteolytic enzyme trypsin, which activates the other pancreatic proenzymes.
Trypsin digests proteins to produce oligopeptides, peptides and amino acids.
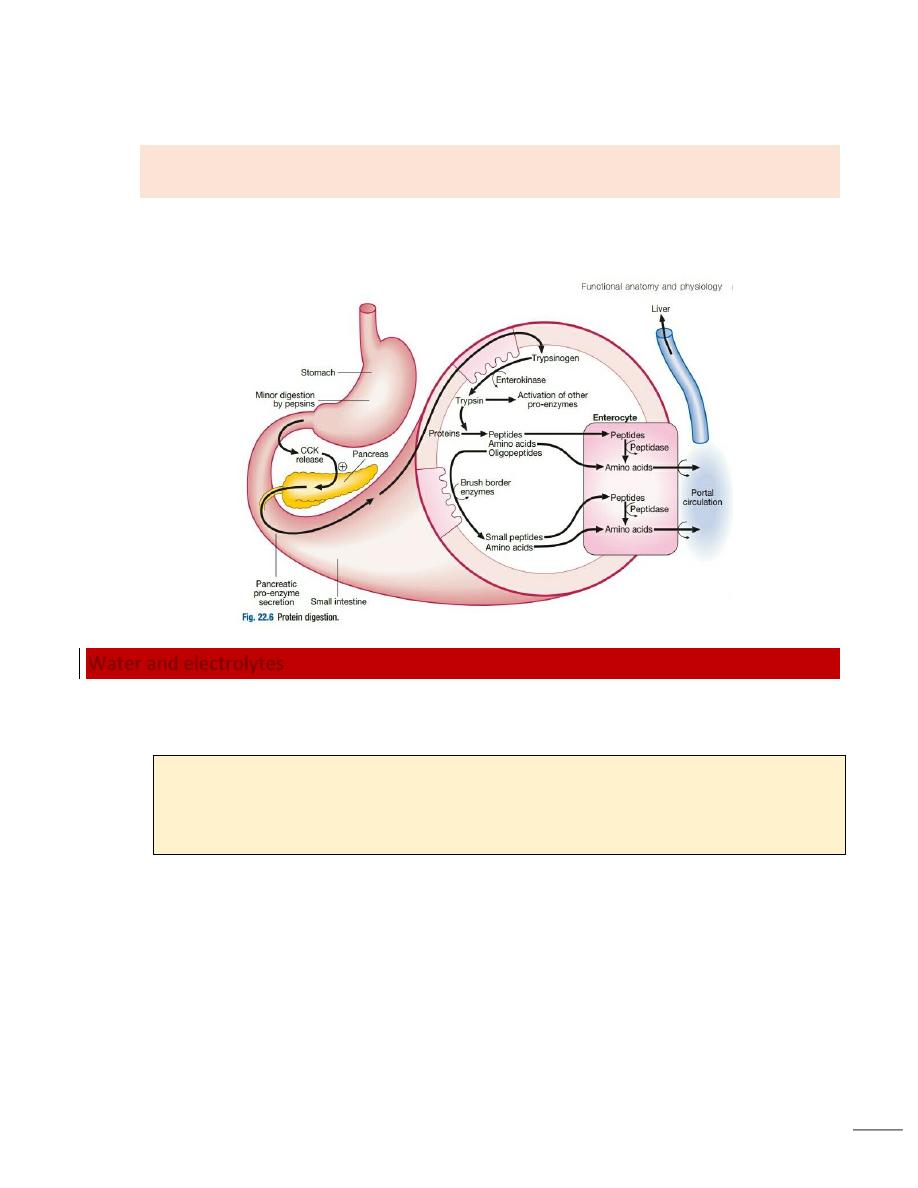
7
Oligopeptides are further hydrolysed by brush border enzymes to yield dipeptides,
tripeptides and amino acids.
These small peptides and the amino acids are actively transported into the
enterocytes, where intracellular peptidases further digest peptides to amino acids.
Amino acids are then actively transported across the basal cell membrane of the
enterocyte into the portal circulation and the liver.
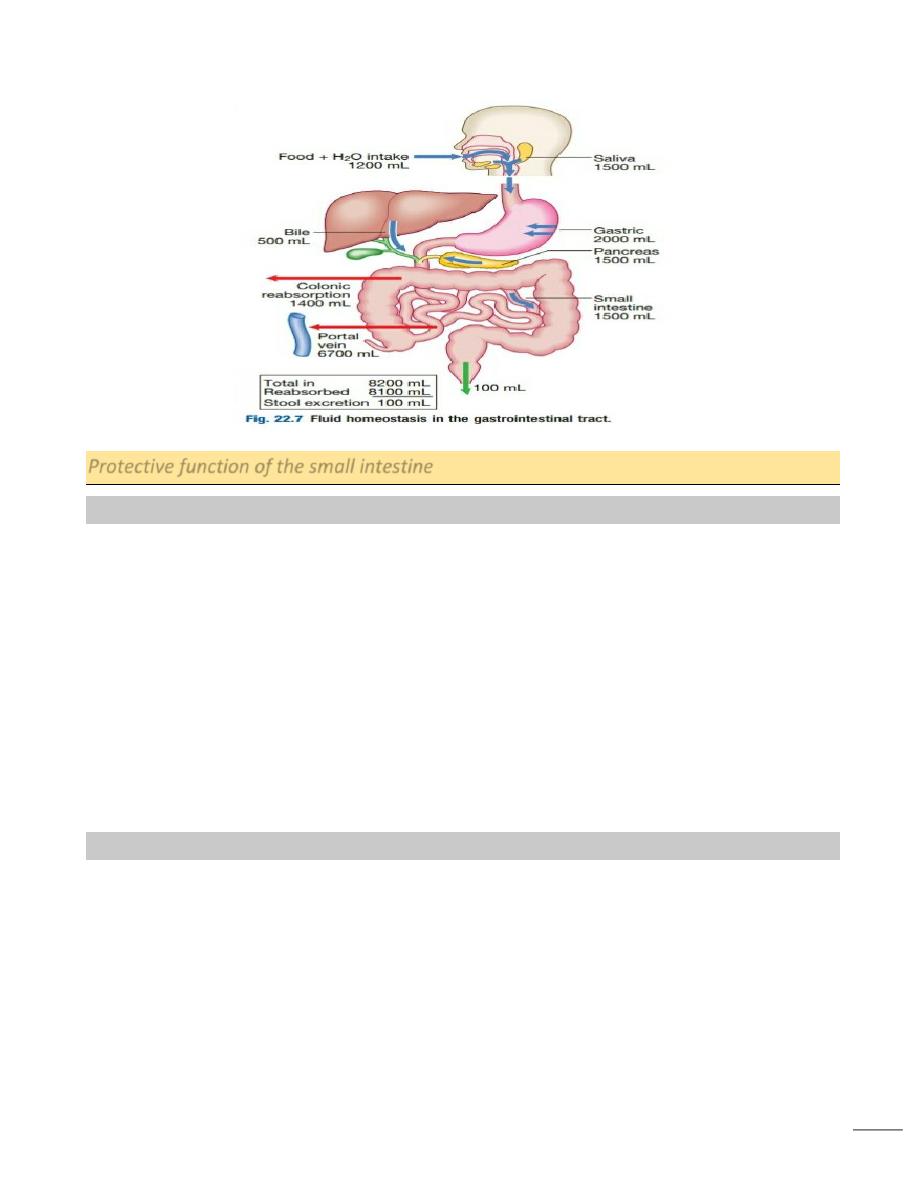
Water and electrolytes
Absorption and secretion of electrolytes and water occur throughout the intestine.
Electrolytes and water are transported by two pathways:
1. the paracellular route, in which passive flow through tight junctions between cells
is a consequence of osmotic, electrical or hydrostatic gradients
2. the transcellular route across apical and basolateral membranes by energy-
requiring specific active transport carriers (pumps).
In healthy individuals, fluid balance is tightly controlled, such that only 100 mL of the
8 litres of fluid entering the gastrointestinal tract daily is excreted in stools
Vitamins and trace elements
Water-soluble vitamins are absorbed throughout the intestine.
8
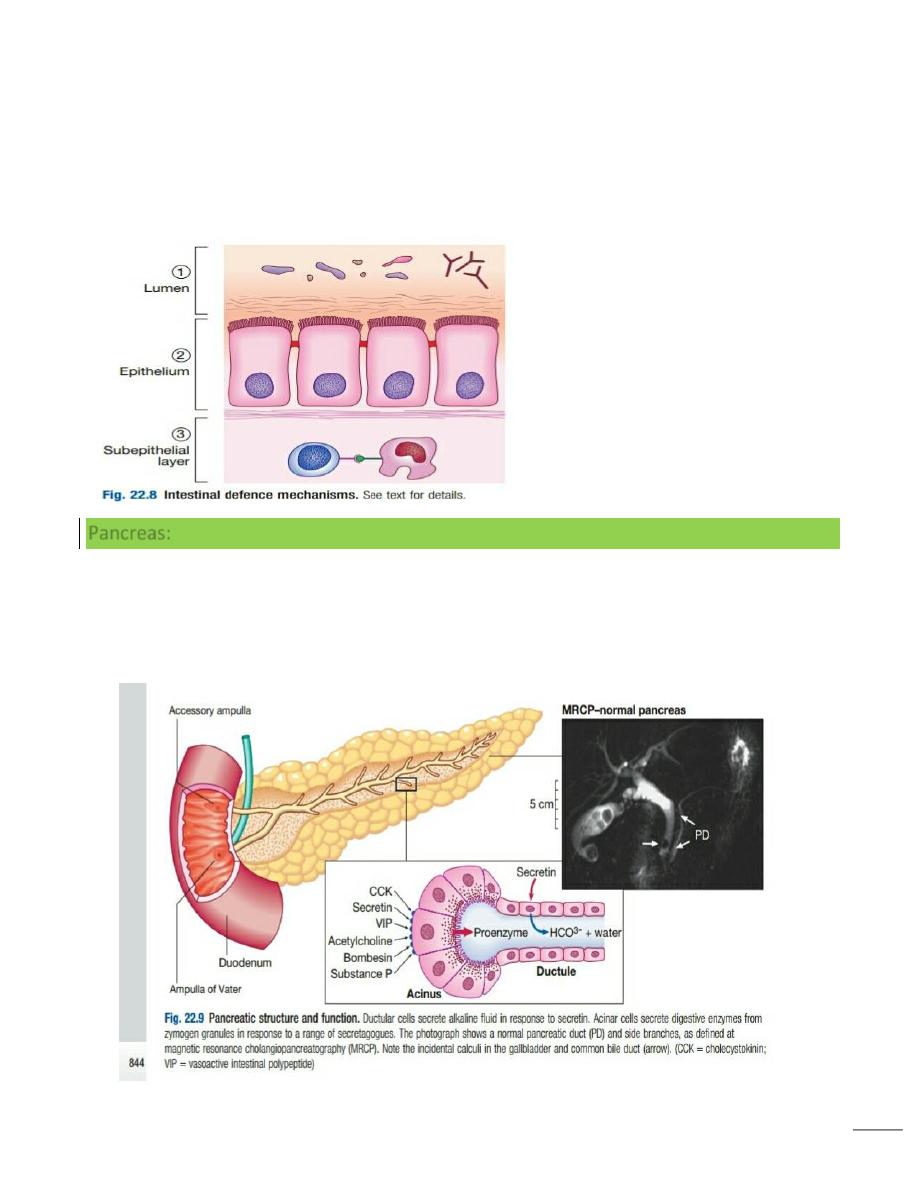
Protective function of the small intestine
Physical defence mechanisms
There are several levels of defense in the small bowel.
Firstly, the gut lumen contains host bacteria, mucins and secreted antibacterial products,
including defensins and immunoglobulins which help combat pathogenic infections.
Secondly, epithelial cells have relatively impermeable brush border membranes, and
passage between cells is prevented by tight and adherens junctions.
These cells can react to foreign peptides (‘innate immunity’) using pattern recognition
receptors found on cell surfaces (Toll receptors) or intracellularly.
Lastly, in the subepithelial layer, immune responses occur under control of the adaptive
immune system in response to pathogenic compounds.
Immunological defence mechanisms
Gastrointestinal mucosa-associated lymphoid tissue (MALT) constitutes 25% of the total
lymphatic tissue of the body and is at the heart of adaptive immunity.
Within Peyer’s patches, B lymphocytes differentiate to plasma cells following exposure
to antigens, and these migrate to mesenteric lymph nodes, to enter the blood stream via
the thoracic duct.
The plasma cells return to the lamina propria of the gut through the circulation and
release immunoglobulin A (IgA), which is transported into the lumen of the intestine.
9
Intestinal T lymphocytes help localise plasma cells to the site of antigen exposure,as well
as producing inflammatory mediators.
Macrophages in the gut phagocytose foreign materials and secrete a range of cytokines,
which mediate inflammation. Similarly, activation of mast-cell surface IgE receptors leads
to degranulation and release of other molecules involved in inflammation
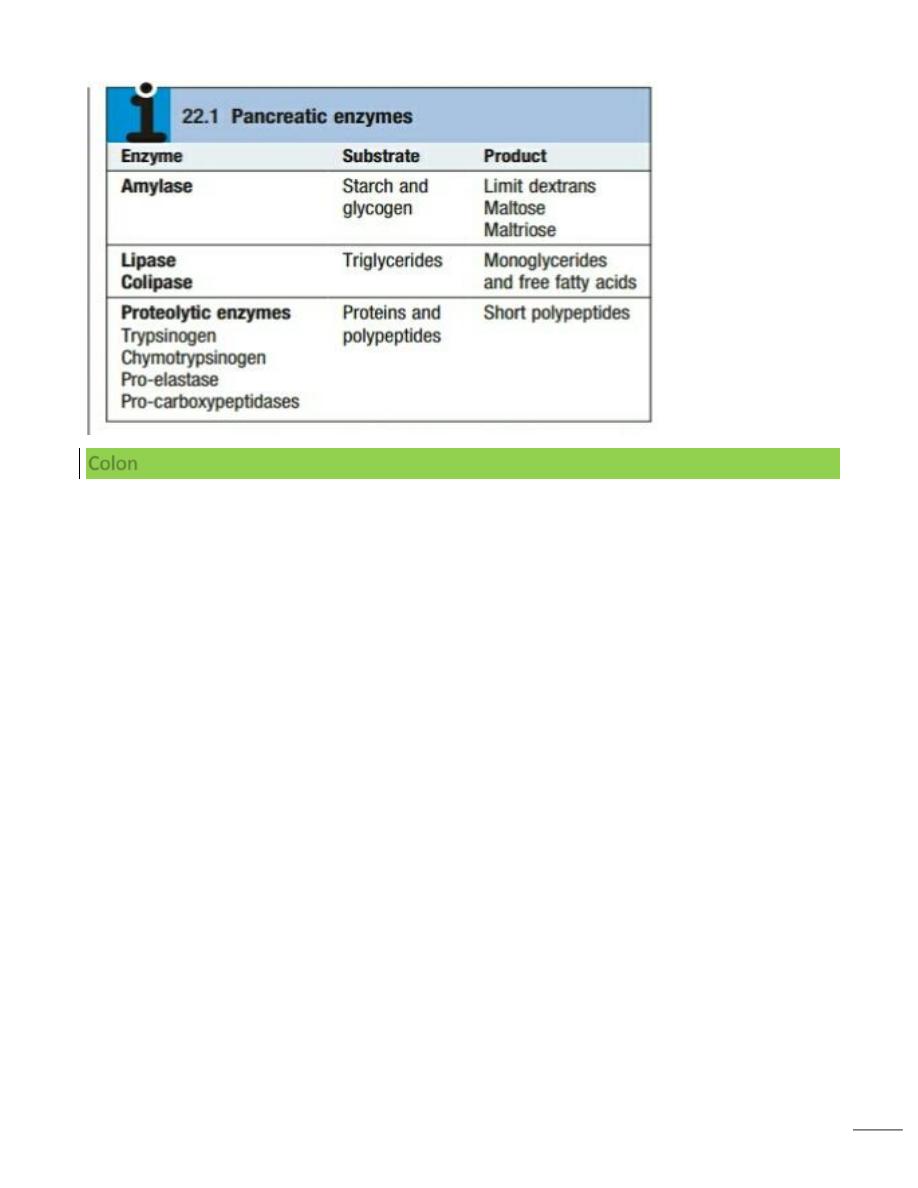
Pancreas:
The exocrine pancreas is necessary for the digestion of fat, protein and carbohydrate.
Proenzymes are secreted from pancreatic acinar cells in response to
circulating gastrointestinal hormones and are activated by trypsin.
Bicarbonate-rich fluid is secreted from ductular cells to produce an optimum alkaline
pH for enzyme activity.
10
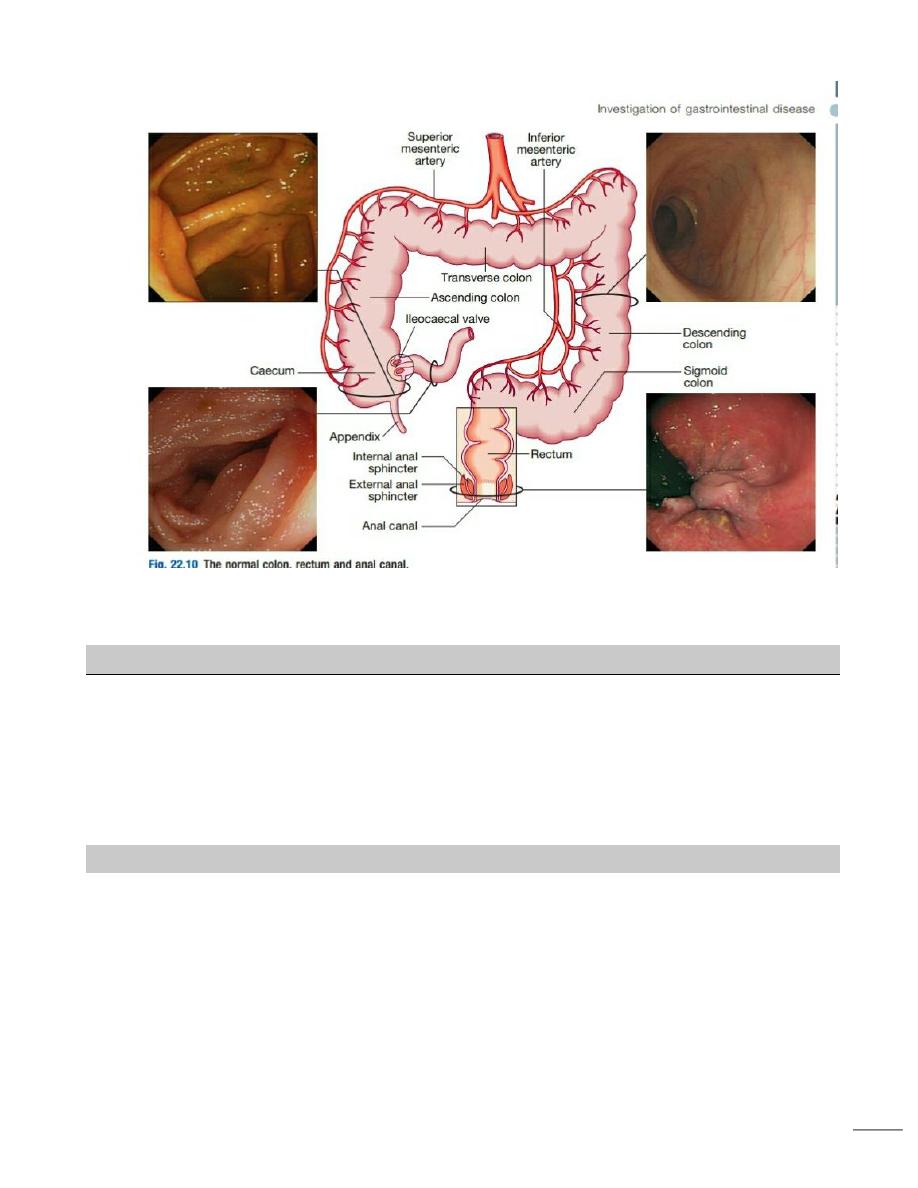
Colon
The colon absorbs water and electrolytes.
It also acts as a storage organ and has contractile activity.
Two types of contraction occur.
o The first of these is segmentation (ring contraction), which leads to mixing but not
propulsion; this promotes absorption of water and electrolytes.
o Propulsive (peristaltic contraction) waves occur several times a day and propel
faeces to the rectum.
All activity is stimulated after meals, probably in response to release of motilin and CCK.
Faecal continence depends upon maintenance of the anorectal angle and tonic
contraction of the external anal sphincters.
On defecation, there is relaxation of the anorectal muscles, increased intra-abdominal
pressure from the Valsalva manoeuvre and contraction of abdominal muscles, and
relaxation of the anal sphincters
11
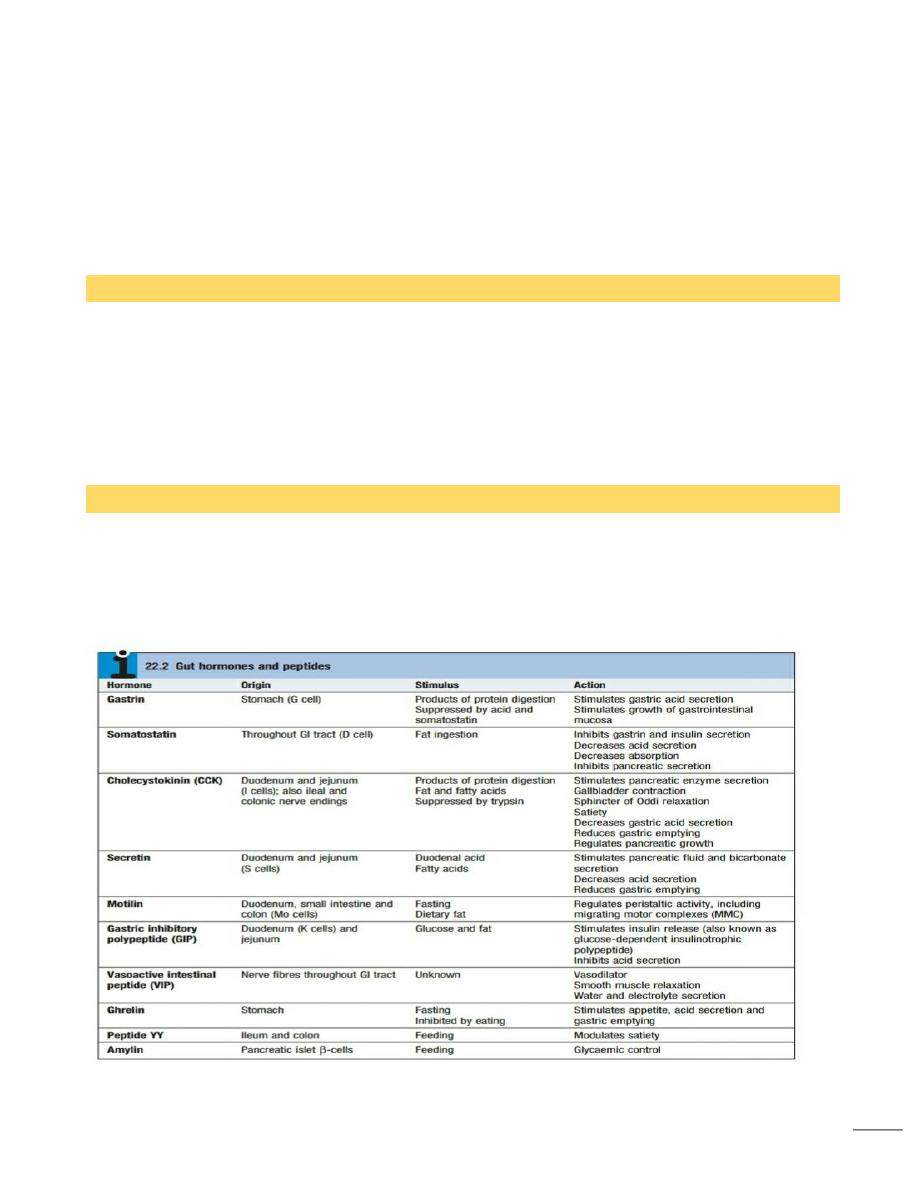
Secretion, absorption, motor activity, growth and differentiation of the gut are all modulated by
a combination of neuronal and hormonal factors.
The nervous system and gastrointestinal function
The central nervous system (CNS), the autonomic system (ANS) and the enteric nervous system
(ENS) interact to regulate gut function. The ANS comprises:
• parasympathetic pathways (vagal and sacral efferent), which are cholinergic, and
increase smooth muscle tone and promote sphincter relaxation
• Sympathetic pathways, which release noradrenaline (norepinephrine), reduce
smooth muscle tone and stimulate sphincter contraction.
The enteric nervous system
In conjunction with the ANS, the ENS senses gut contents and conditions, and regulates
motility, fluid exchange, secretion, blood flow and other key gut functions. It comprises
two major networks intrinsic to the gut wall.
The myenteric (Auerbach’s) plexus in the smooth muscle layer regulates motor control;
and the submucosal (Meissner’s) plexus exerts secretory control over the epithelium,
enteroendocrine cells and submucosal vessels.
Together, these plexuses form a two-layered neuronal mesh along the length of the gut.
12
Although connected centrally via the ANS, the ENS can function autonomously using a
variety of transmitters, including acetylcholine, noradrenaline (norepinephrine), 5-
hydroxytryptamine (5-HT, serotonin), nitric oxide, substance P and calcitonin gene-related
peptide (CGRP).
There are local reflex loops within the ENS but also loops involving the coeliac and
mesenteric ganglia and the paravertebral ganglia.
The parasympathetic system generally stimulates motility and secretion, while the
sympathetic system generally acts in an inhibitory manner
Peristalsis
Peristalsis is a reflex triggered by gut wall distension, which consists of a wave of circular
muscle contraction to propel contents from the oesophagus to the rectum.
It can be influenced by innervation but functions independently.
It results from a basic electrical rhythm originating from the interstitial cells of Cajal in the
circular layer of intestinal smooth muscle.
These are stellate cells of mesenchymal origin with smooth muscle features, which act as
the ‘pacemaker’ of the gut
Migrating motor complexes
Migrating motor complexes (MMC) are waves of contraction spreading from the stomach
to the ileum, occurring at a frequency of about 5 per minute every 90 minutes or so,
between meals and during fasting.
They may serve to sweep intestinal contents distally in preparation for the next meal and
are inhibited by eating.
13
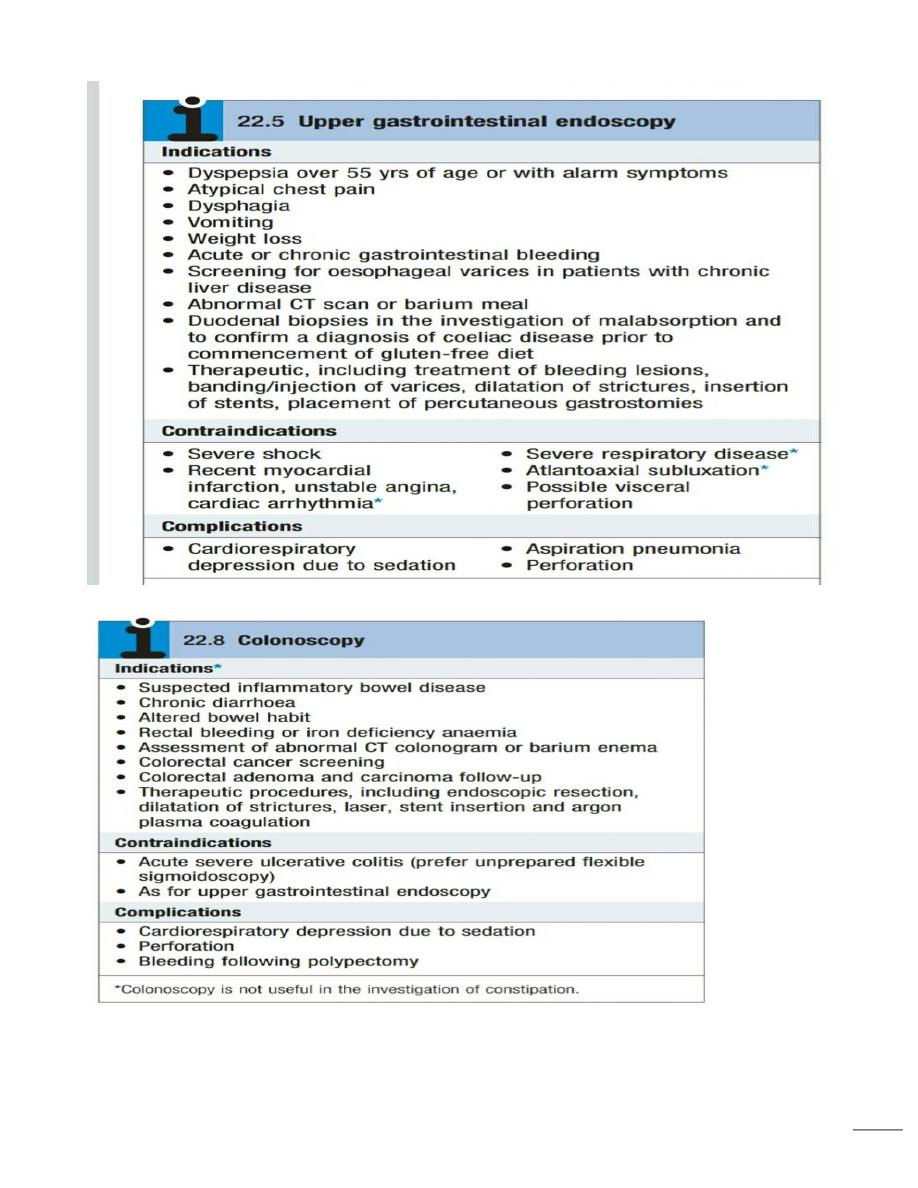
Investigation Of Gastrointestinal Disease
A wide range of tests are available for the investigation of patients with gastrointestinal
symptoms.
These can be classified broadly into tests of structure, tests for infection and tests of
function.
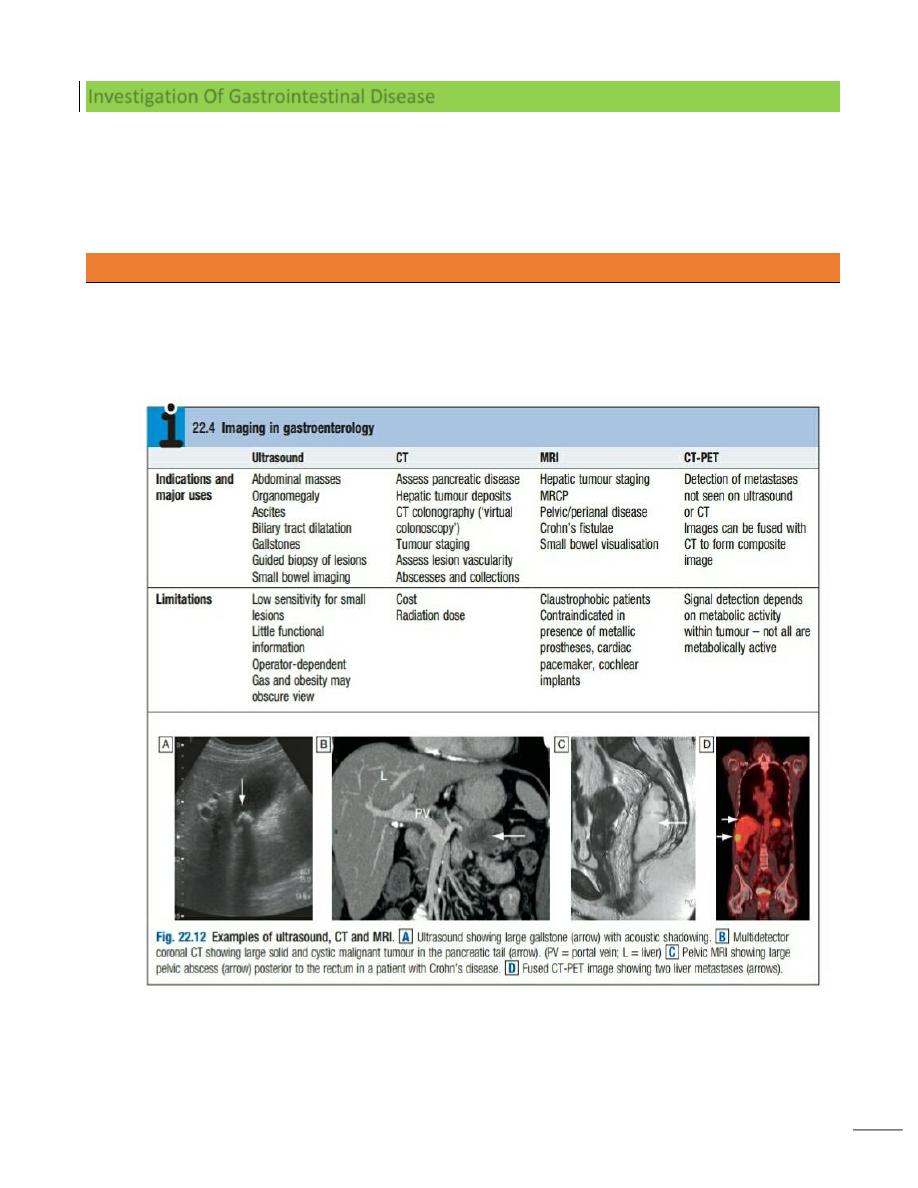
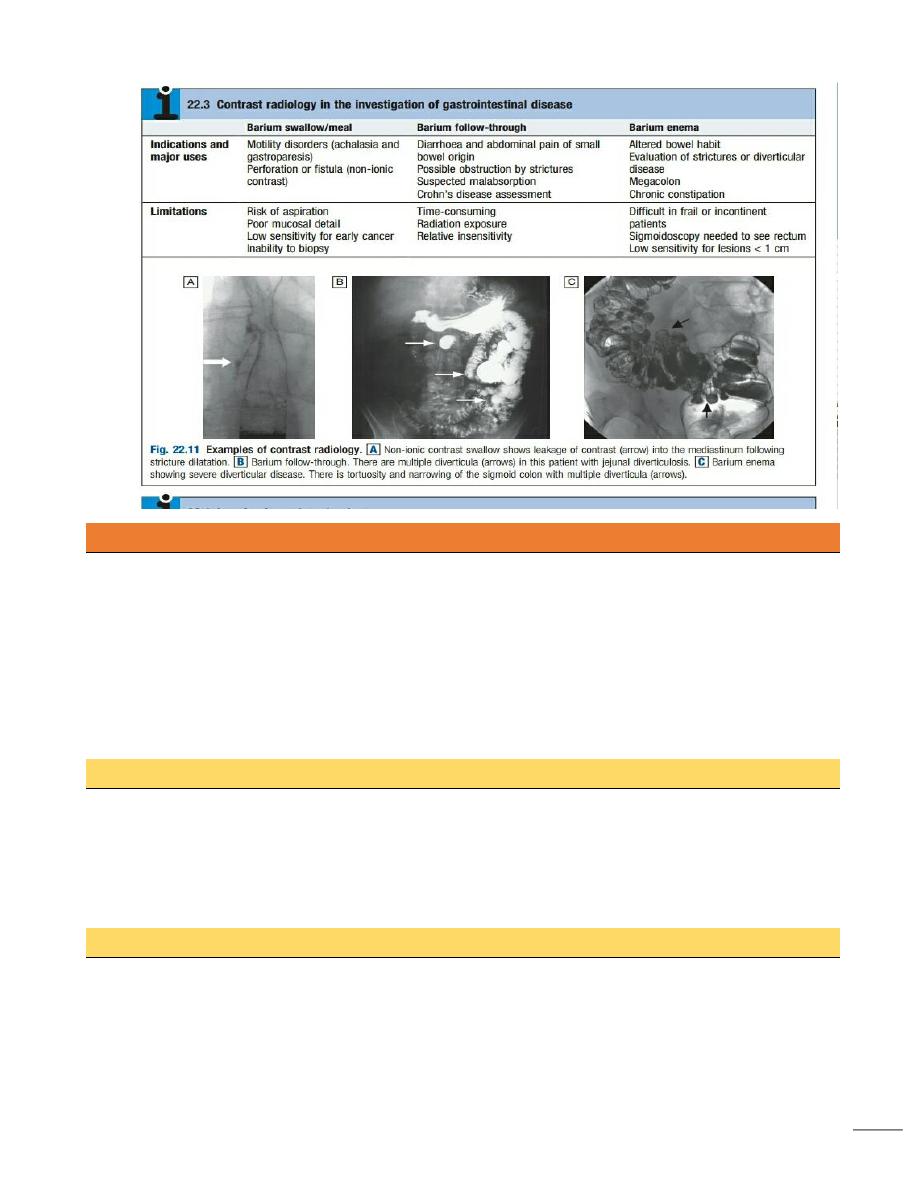
Imaging Plain X-rays
Plain X-rays of the abdomen are useful in the diagnosis of intestinal obstruction or paralytic
ileus, where dilated loops of bowel and (in the erect position) fluid level may be seen.
Calcified lymph nodes, gallstones and renal stones can also be detected.
14
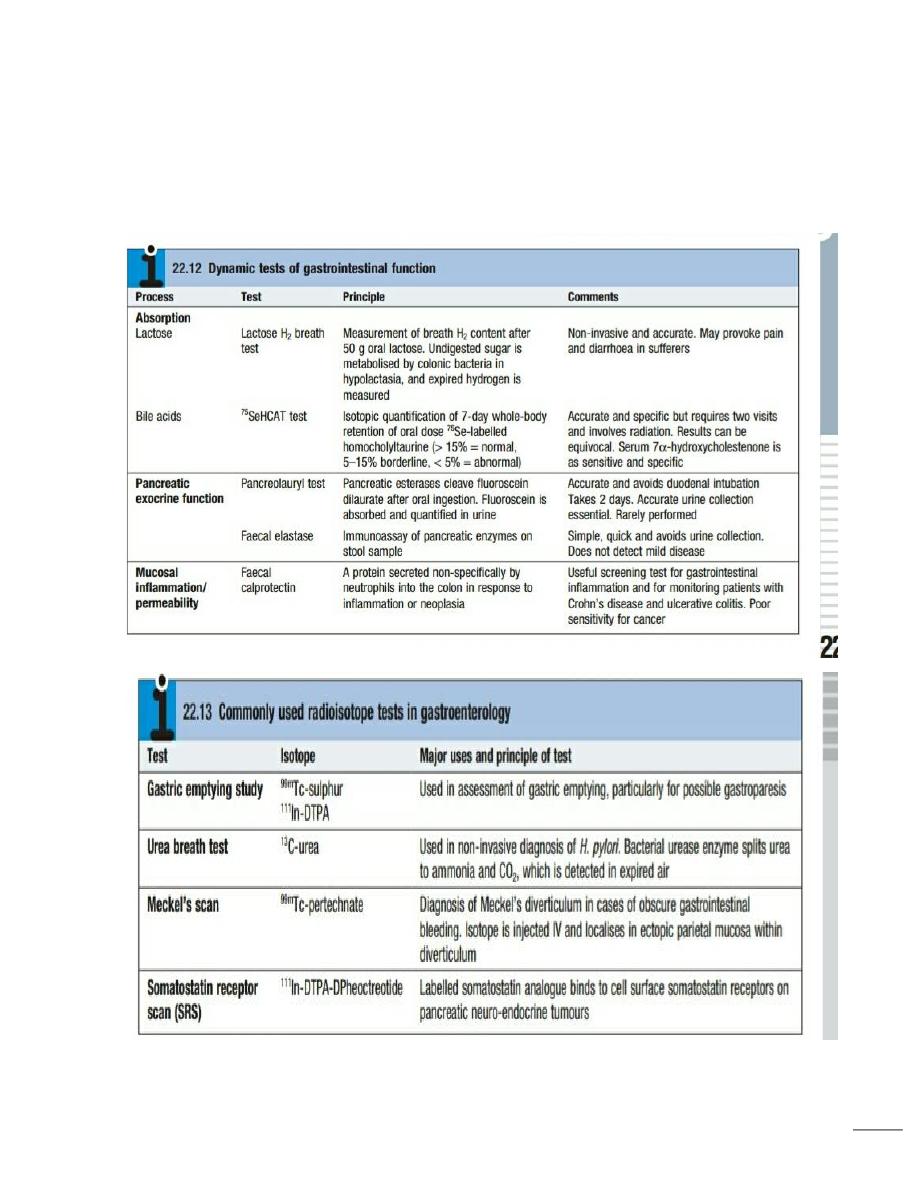
Tests of function
A number of dynamic tests can be used to investigate aspects of gut function, including
digestion, absorption, inflammation and epithelial permeability.
Some of the more commonly used ones .
In the assessment of suspected malabsorption, blood tests (full blood count, erythrocyte
sedimentation rate (ESR), C-reactive protein (CRP), folate, vitamin B12, iron status,
albumin, calcium and phosphate) are essential, And endoscopy is undertaken to obtain
mucosal biopsies.
Faecal calprotectin is very sensitive at detecting mucosal inflammation.
Gastric emptying
This involves administering a test meal containing solids and liquids labelled with different
radioisotopes and measuring the amount retained in the stomach afterwards
It is useful in the investigation of suspected delayed gastric emptying (gastroparesis) when other
studies are normal.
Colonic and anorectal motility
A plain abdominal X-ray taken on day 5 after ingestion of different-shaped inert plastic pellets on
days 1–3 gives an estimate of whole gut transit time.
15
The test is useful in the evaluation of chronic constipation, when the position of any retained
pellets can be observed, and helps to differentiate cases of slow transit from those due to
obstructed defecation.
The mechanism of defecation and anorectal function can be assessed by anorectal manometry,
electrophysiological tests and defecating proctography.
16
17
18
19
