Lecture 3………………………………………………..Blood Physiology
1
Blood typing & transfusion Physiology
Basis of Blood grouping or Typing (Multiplicity of Antigens in
the blood cells)
At least 30 commonly occurring antigens have been found on the cell membrane of
RBCs. These can cause Ag-Ab (antigen-antibody) reaction if mixed With
plasma that contain Ab against these Ag.
According to presence or absence of these antigensblood is classified into several
groups ,Two groups of Ag can cause transfusion reactions more than others:
ABO and Rh systems of Ag.
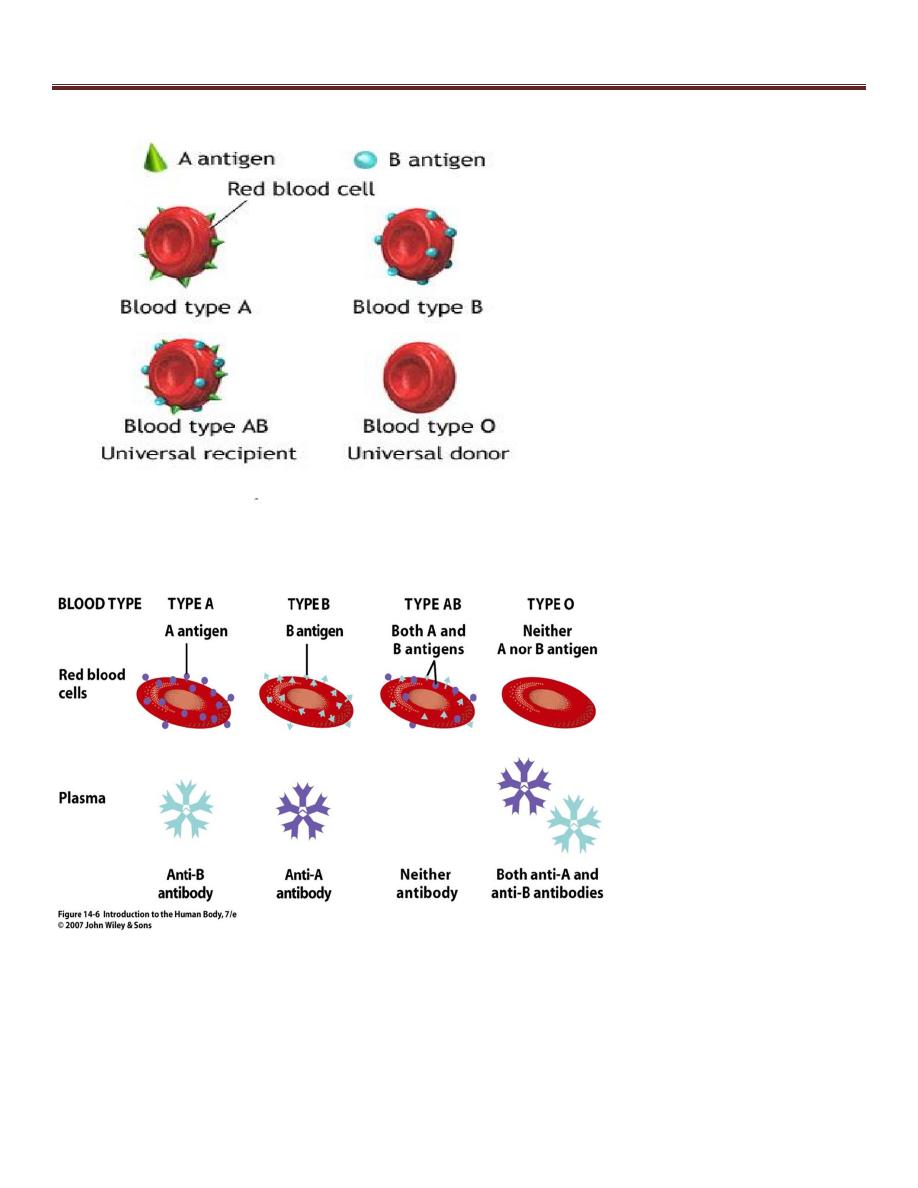
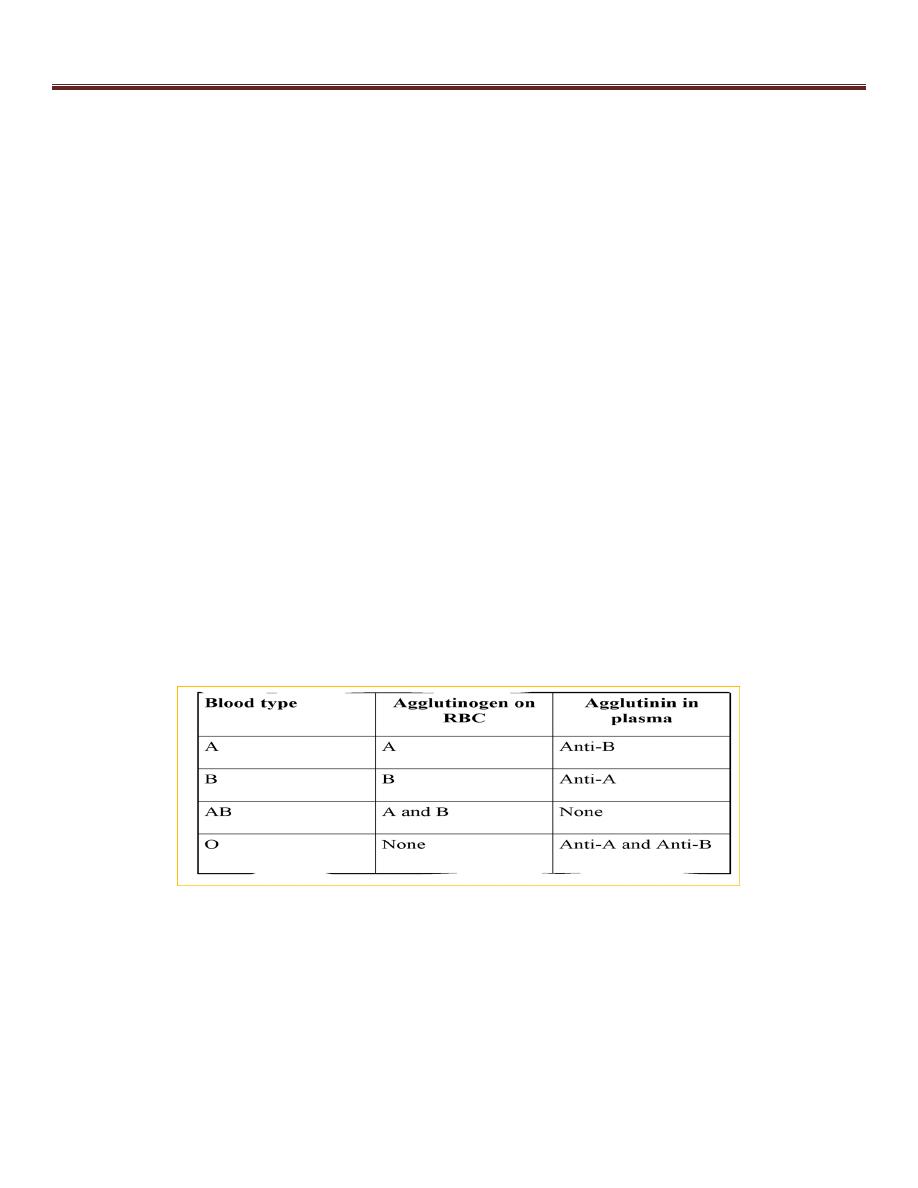
Agglutinogens - glycoproteins on the surface of blood cells causes "agglutination"
(clumping)
ABO Blood Groups - determined by presence or absence of Type A and Type B
agglutinogen proteins on the surface of RBCs cell membrane.
agglutinins - antibodies against either A or B agglutinogen , when bind agglutinins
to RBC antigens, resulting in agglutination (clumping) or hemolysis (rupture) of
RBCs
ABO system for Blood Typing
Lecture 3………………………………………………..Blood Physiology
2
Lecture 3………………………………………………..Blood Physiology
3
Blood transfusion:
1. A person with blood type A can receive blood from a donor with
blood type A. The anti-B antibodies in the recipient do not
combine with the type A antigens on the red blood cells of the
donor.
2. A person with blood type B cannot receive blood from a donor
with blood type A. The anti-A antibodies in the recipient will
combine with the type B antigens on the red blood cells of the
donor.
3.
If the wrong blood type is used, the person’s own immune
system immediately attacks the donor’s blood and causes clumps
and RBC destruction (hemolysis) that can lead to total kidney
failure and death.

Lecture 3………………………………………………..Blood Physiology
4
Transfusion reaction
Plasma antibody meets its specific surface antigen , Blood will
agglutinate and hemolysis , If donor and recipient blood types not
compatible.
Type AB
has no AB antibodies so can receive any ABO type blood
called Universal recipients.
Type O
have neither antigen so can donate to any other ABO type
called Universal donors.
Transfusion Reactions resulting from mismatched blood types
lead to :
1.Agglutination and delayed hemolysis of donor’s RBC (or immed
iate intravascular hemolysis)→ Jaundice
2. Renal failure: Renal tubular blockage by hemoglobin
Rh System for Blood Typing
The term "Rh-positive" means that the individual has agglutinogen D. The "Rh-
negative" individual has no D antigen and forms the anti-D agglutinin when
injected with D-positive cells.
85% of Caucasians are D-positive and 15% are D-negative; over 99% of Asians
are D-positive.
Lecture 3………………………………………………..Blood Physiology
5
Differences between ABO and Rh Ab?
*Anti-D (Rh)antibodies do not develop naturally without exposure of a D-negative
individual to D-positive red cells by blood transfusion or entrance of fetal blood
into the maternal circulation , Rh negative women pregnant with Rh +ve baby
.
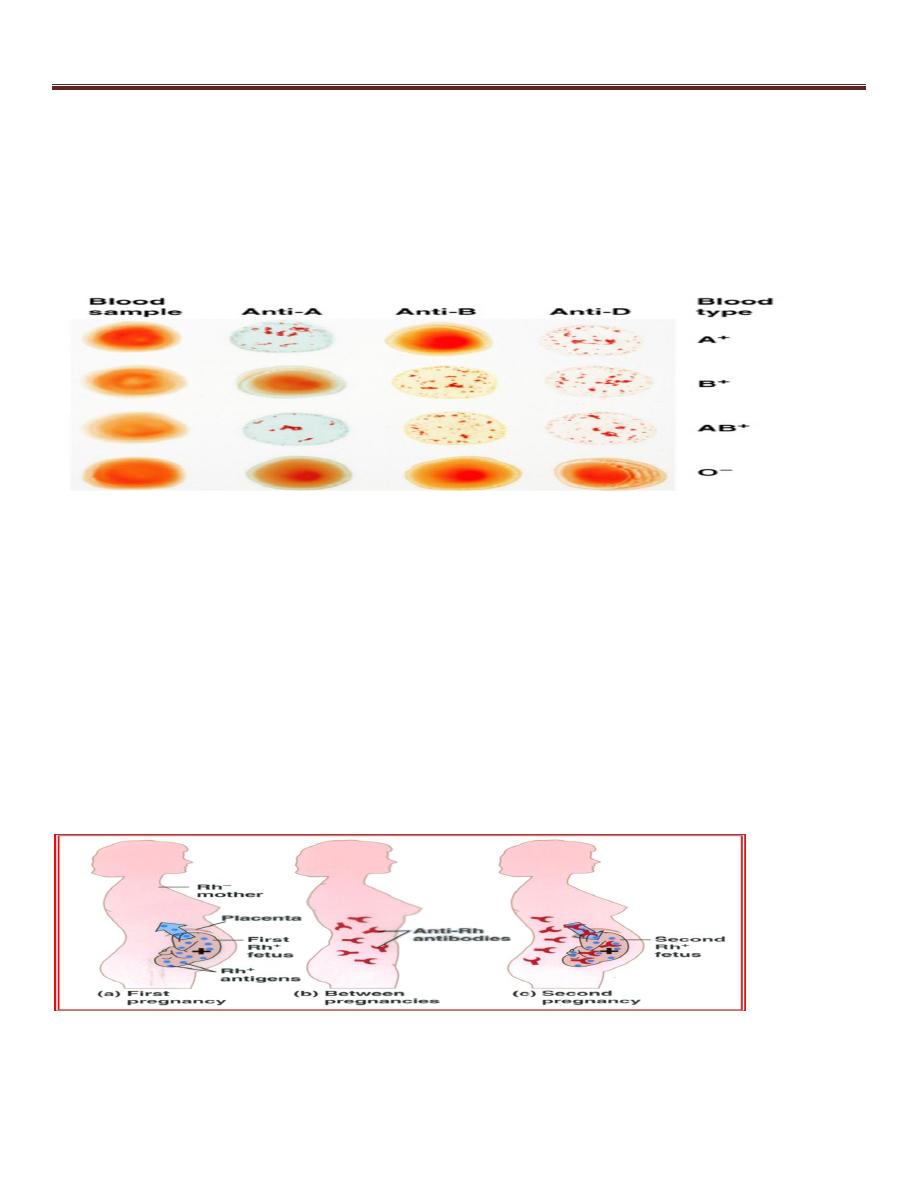
Hemolytic Disease of the Newborn (HDN)
Is most common problem with "Rh incompatibility" arises when an Rh-negative
mother carries an Rh-positive fetus.
Small amounts of fetal blood leak into the maternal circulation at the time of
delivery, and some mothers develop significant titers of anti-Rh agglutinins during
the postpartum period. During the next pregnancy, the mother's agglutinins(Abs)
cross the placenta to the fetus , cause hemolysis and various forms of hemolytic
disease of the newborn (erythroblastosis fetalis).

Lecture 3………………………………………………..Blood Physiology
6
If hemolysis in the fetus is severe, may die in utero or may develop anemia, severe
jaundice, and edema (hydrops fetalis). Kernicterus, a neurologic syndrome in which
unconjugated bilirubin is deposited in the basal ganglia
Prevention by :
* by administering a single dose of anti-Rh antibodies in the form of Rh immune
globulin during the postpartum period, (anti-D) IG.
*has reduced the overall incidence of hemolytic disease by more than 90%.
Indicated Anti-D in
:
If a woman has Rh- and gives birth to a child, or if she has a miscarriage or
abortion, she is given an injection of anti-Rh antibodies called anti-Rh gamma
globulin or RhoGAM to prevent HDN.
Action of Anti-D:
The antibodies bind to the fetal Rh antigens and inactivate them if they crossed the
placenta during birth, and the mother’s immune system does not respond by
producing antibodies.
