Blood Coagulation
Terms should be recognized..
Procoagulants
or hemostatic agents are the substances which accelerate the process of
blood coagulation. (chemical that promotes clotting)
anticoagulant
- chemical that inhibits clotting
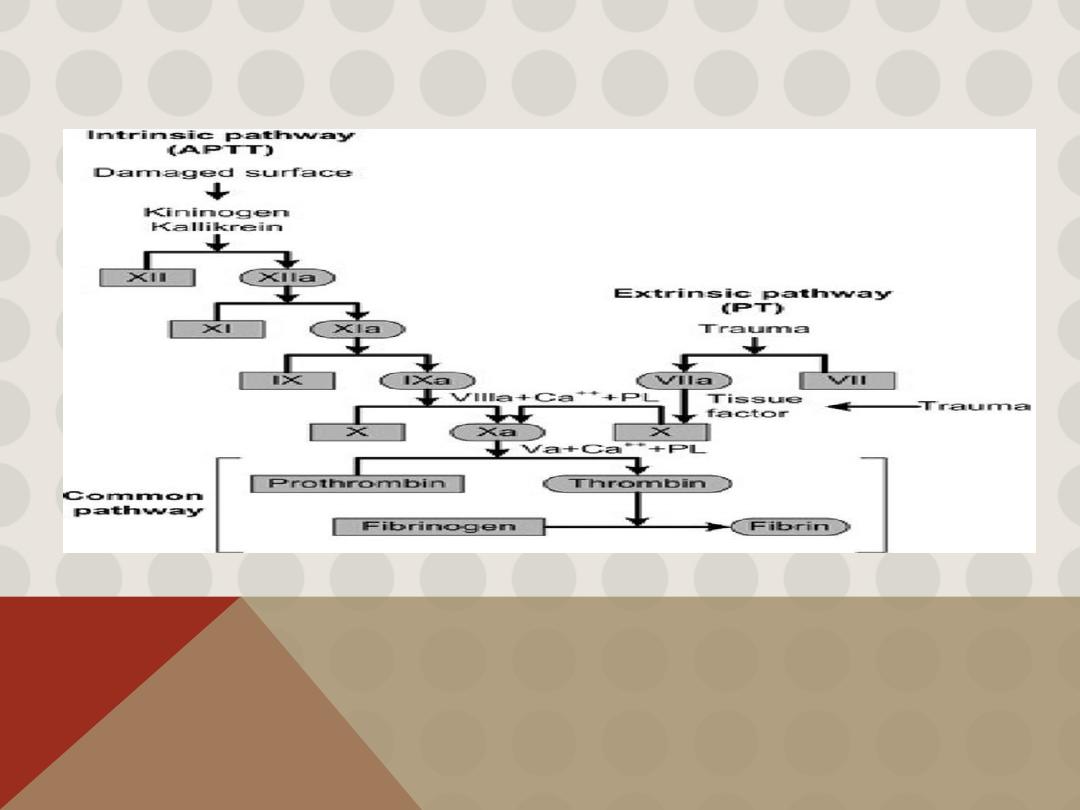
A- intrinsic pathway -
within the damaged vessel
B-.extrinsic pathway
- in outer tissues around vessel
Coagulation or clotting is
defined as the process in which blood loses its fluidity and
becomes a jelly-like mass few minutes after it is shed out or collected in a container.
Cascade
refers to a process that occurs through a series of steps, each step initiating the
next, until the final step is reached
**The liver is the site of synthesis of all coagulation factors except VWF
Most of the clotting factors are proteins in the form of enzymes. Normally, all the factors
are present in the form of inactive
proenzyme.
These proenzymes must be
activated
into
enzymes
to enforce clot formation. It is carried out by a series of proenzyme-
enzyme conversion reactions. First one of the series is converted into an active
enzyme that activates the second one, which activates the third one; this continues
till the final active enzyme thrombin is formed.
In general, blood clotting occurs in
three stages:
1.Formation of prothrombin activator
2.Conversion of prothrombin into thrombin
3. Conversion of fibrinogen into fibrin.
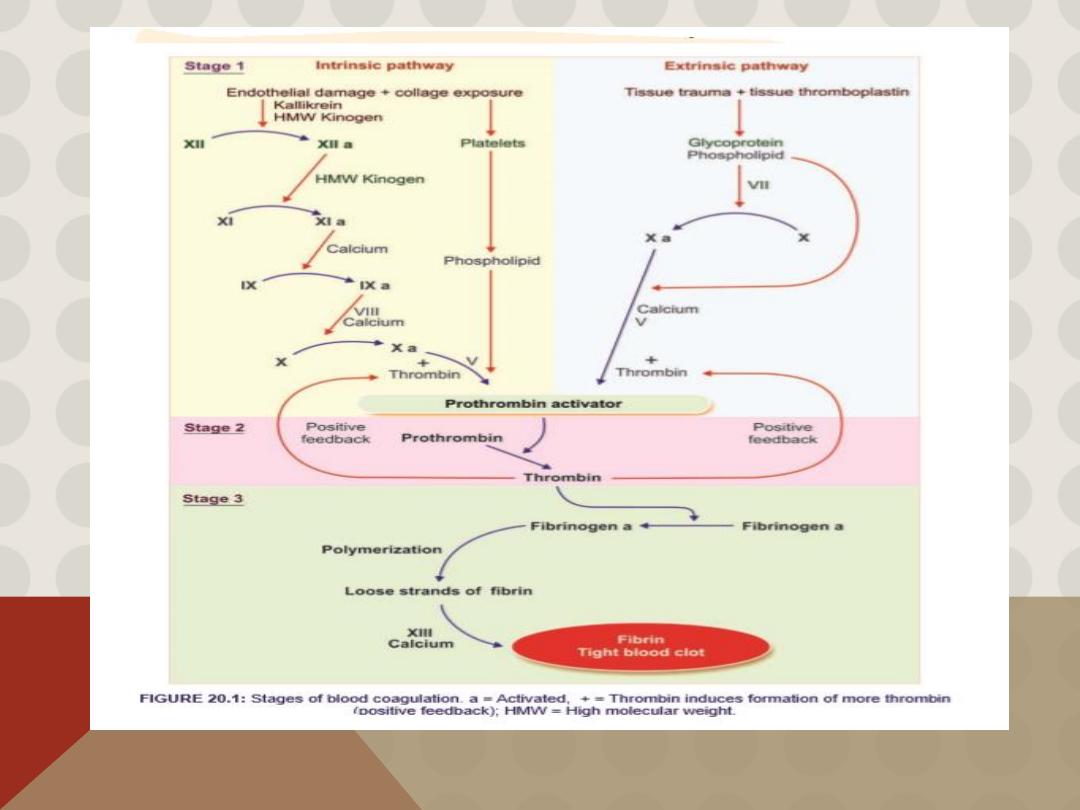
STAGE 1: FORMATION OF PROTHROMBIN ACTIVATOR
Blood clotting commences with the formation of a substance called prothrombin activator, which converts
prothrombin into thrombin. Its formation is initiated by substances produced either within the blood or
outside the blood. Thus, formation of prothrombin activator occurs
through two pathways: i. Intrinsic pathway
ii. Extrinsic pathway.
i.
Intrinsic Pathway for the Formation of Prothrombin Activator is initiated by platelets, which are within
the blood itself .
Sequence of Events in Intrinsic pathway
i.
During the injury, the blood vessel is ruptured. Endothelium is damaged and collagen beneath the
endothelium is exposed.
ii.
ii. When factor XII (Hageman factor) comes in contact with collagen, it is converted into activated
factor XII in the presence of kallikrein and high molecular weight (HMW) kinogen.
iii.
iii. The activated factor XII converts factor XI into activated factor XI in the presence of HMW kinogen.
iv.
iv. The activated factor XI activates factor IX in the presence of factor IV (calcium).
v.
v. Activated factor IX activates factor X in the presence of factor VIII and calcium.
vi.
vi. When platelet comes in contact with collagen of damaged blood vessel, it gets activated and
releases phospholipids.
vii.
vii. Now the activated factor X reacts with platelet phos pholipid and factor V to form prothrombin
activa tor. This needs the presence of calcium ions.
viii. viii. Factor V is also activated by positive feedback effect of thrombin
ii.
Extrinsic Pathway
for the Formation of Prothrombin Activator is initiated by the tissue
thromboplastin, which is formed from the injured tissues.
Sequence of Events in
Extrinsic Pathway
i.
Tissues that are damaged during injury release tissue thromboplastin (factor III).
Thromboplastin contains proteins, phospholipid and glycoprotein, which act as proteolytic
enzymes.
ii.
ii. Glycoprotein and phospholipid components of thromboplastin convert factor X into activated
factor X, in the presence of factor VII.
iii. iii. Activated factor X reacts with factor V and phospholipid component of tissue thromboplastin
to form prothrombin activator. This reaction requires the presence of calcium ions.
„
STAGE 2: CONVERSION OF PROTHROMBIN INTO THROMBIN
Blood clotting is all about thrombin formation. Once thrombin is formed, it definitely leads to clot
formation.
Sequence of Events in Stage 2
i.
Prothrombin activator that is formed in intrinsic and extrinsic pathways converts prothrombin
into thrombin in the presence of calcium (factor IV).
ii.
ii. Once formed thrombin initiates the formation of more thrombin molecules. The initially
formed thrombin activates Factor V. Factor V in turn accelerates formation of both extrinsic and
intrinsic prothrombin activator, which converts prothrombin into thrombin. This effect of
thrombin is called positive feedback effect
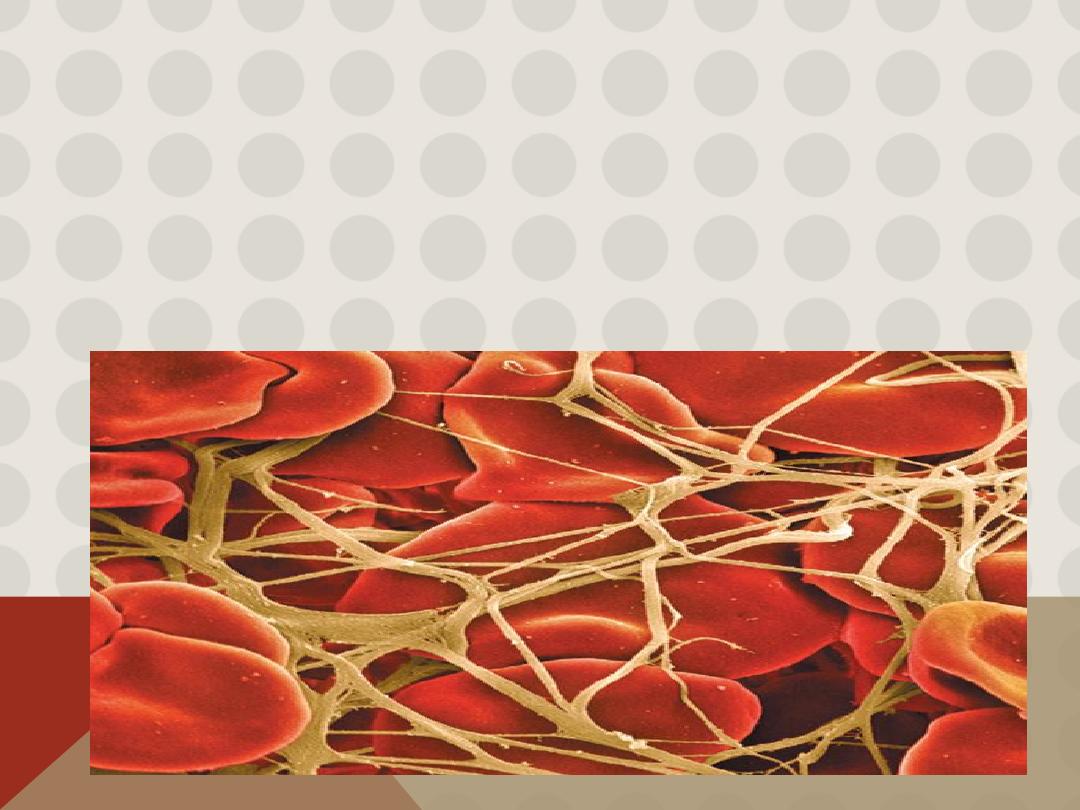
STAGE 3: CONVERSION OF FIBRINOGEN INTO FIBRIN
The final stage of blood clotting involves the conversion of fibrinogen into fibrin by
thrombin.
Sequence of Events in Stage 3
i.
Thrombin converts inactive fibrinogen into activated fibrinogen due to loss of 2 pairs
of polypeptides from each fibrinogen molecule. The activated fibrinogen is called
fibrin monomer.
ii.
ii. Fibrin monomer polymerizes with other monomer molecules and form loosely
arranged strands of fibrin.
iii. Later these loose strands are modified into dense and tight fibrin threads by
fibrin-
stabilizing factor (factor XIII)
in the presence of
calcium ions
. All the tight fibrin
threads are aggregated to form a meshwork of stable clot.
Role of Calcium Ions in the Intrinsic and Extrinsic Pathways
calcium ions are required for promotion or acceleration of all the bloodclotting reactions.
in the absence of calcium ions, blood clotting by either pathway does not occur. .
However, when blood is removed from a person, it can be prevented from clotting by
reducing the calcium ion concentration below the threshold level for clotting, either by
deionizing the calcium by causing it to react with substances such as citrate ion or by
precipitating the calcium with substances such as oxalate ion.
Red blood cells trapped in a fibrin mesh
„
TESTS FOR BLOOD CLOTTING
Blood clotting tests are used to diagnose blood disorders. Some tests are also used to
monitor the patients treated with anticoagulant drugs such as heparin and warfarin.
1. Bleeding time 2. Clotting time 3. Prothrombin time 4. Partial prothrombin time
5. International normalized ratio 6. Thrombin time.
„
BLEEDING TIME Bleeding time (BT)
is the time interval from oozing of blood after a cut
or injury till arrest of bleeding. Usually, it is determined by Duke method using blotting
paper or filter paper method. Its normal duration is 3 to 5 minutes. It is prolonged in
purpura.
„
CLOTTING TIME Clotting time (CT)
is the time interval from oozing of blood after a cut or
injury till the formation of clot. It is usually determined by capillary tube method. Its
normal duration is 3 to 8 minutes. It is prolonged in hemophilia.
„
PROTHROMBIN TIME (PT
)
is the time taken by blood to clot after adding tissue thromboplastin to it .Normal duration of
prothrombin time is 10 to 12 seconds. It is prolonged in deficiency of prothrombin and
other factors like factors I, V, VII and X. However, it is normal in hemophilia.( Extrinsic
pathway)
„
PARTIAL PROTHROMBIN TIME
Or
ACTIVATED PROTHROMBIN TIME a PTT
is the time taken for the blood to clot after adding an activator such as phospholipid, along
with calcium to it. It is also called activated partial prothrombin time (aPTT). This test is
useful in monitoring the patients taking anticoagulant drugs. Phospholipid serves as
platelet substitute. Commonly used surface activator is kaolin. Its prolonged in
Hemophilia ,( intrinsic pathway assess )
PTT: Factors XII, XI, IX, VIII
PT: Factors VII, X, II, V
Bleeding time
: a controlled incision is produced in the skin and bleeding commences. The
time taken until bleeding ceases is measured. It assessed the platelets function .by ear
prick 2mm depth which should be not more than 5 min. (2-5 is normal).More than 5
indicate plt dysfunction in the presence of normal plt count.
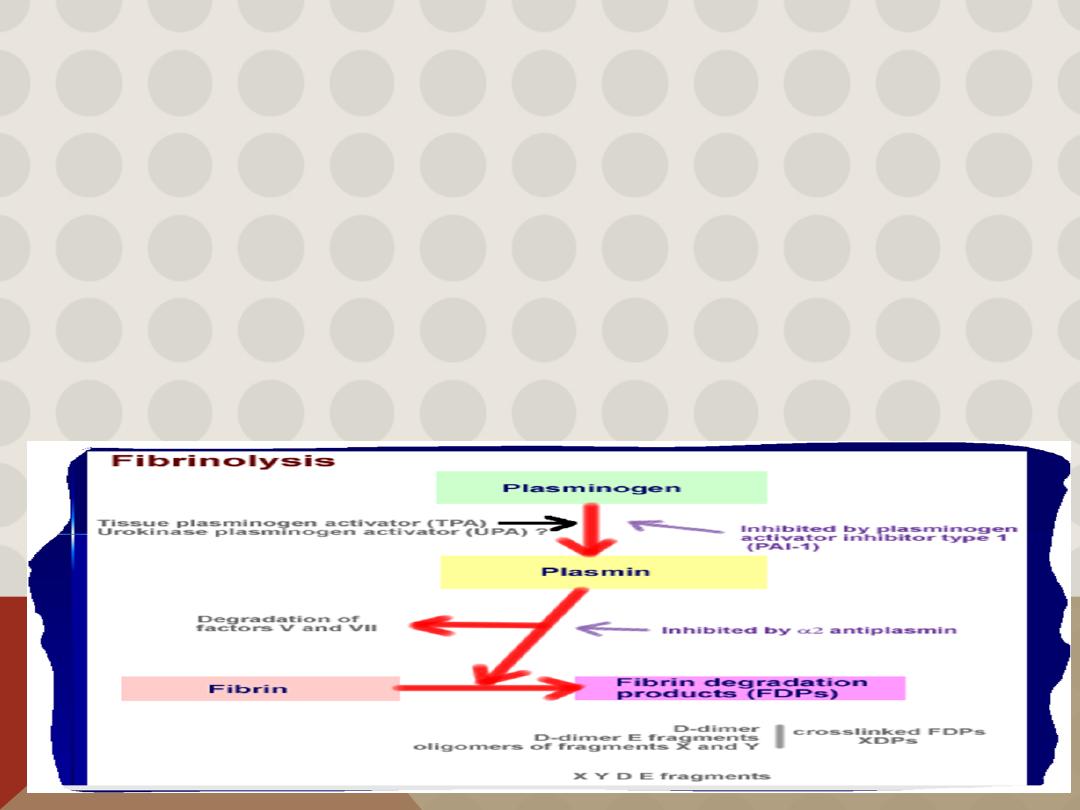
FIBRINOLYSIS
Degradation of fibrin clot by enzyme called
plasmin
Necessary to remove clot so wound healing can proceed
Plasminogen activators from blood vessels and other cells convert plasminogen to plasmin to begin
the process
Clot Eradication (Fibrinolysis)
1.healing occurs over 2 - 10 days
2.tissue plasminogen activator (TPA) - causes the activation of plasminogen
3.plasminogen--> plasmin
4.plasmin degrades proteins within the clot
VITAMIN K IS NEEDED FOR PRODUCTION OF
SEVERAL CLOTTING PROTEINS
Fat-soluble vitamin present in many foods , Some made by bacteria in gut
Necessary for synthesis of several components of coagulation cascade
Deficiency may lead to
low levels of clotting factors
, factors X, IX, VII, II, protein C and
protein S. causing a bleeding tendency
1972
Warfarin (Coumadin™): a drug that interferes with vitamin K action , used as an
anticoagulant (prevent thrombosis)
VITAMIN K DEFICIENCY
Newborn/premature infants
Poor intake
Defective absorption
generalized malabsorption
biliary disease
Diminished production by bacteria in gut (antibiotic treatment)
Vitamin K antagonists as warfarin (Coumadin)
certain antibiotics
INHERITED BLEEDING DISORDERS
Decreased production of single clotting factor
HEMOPHILIA:
complete absence of factor VIII (hemophilia A) or factor IX (hemophilia B)
sex-linked inheritance (99.99% of patients male) moderate or severe bleeding
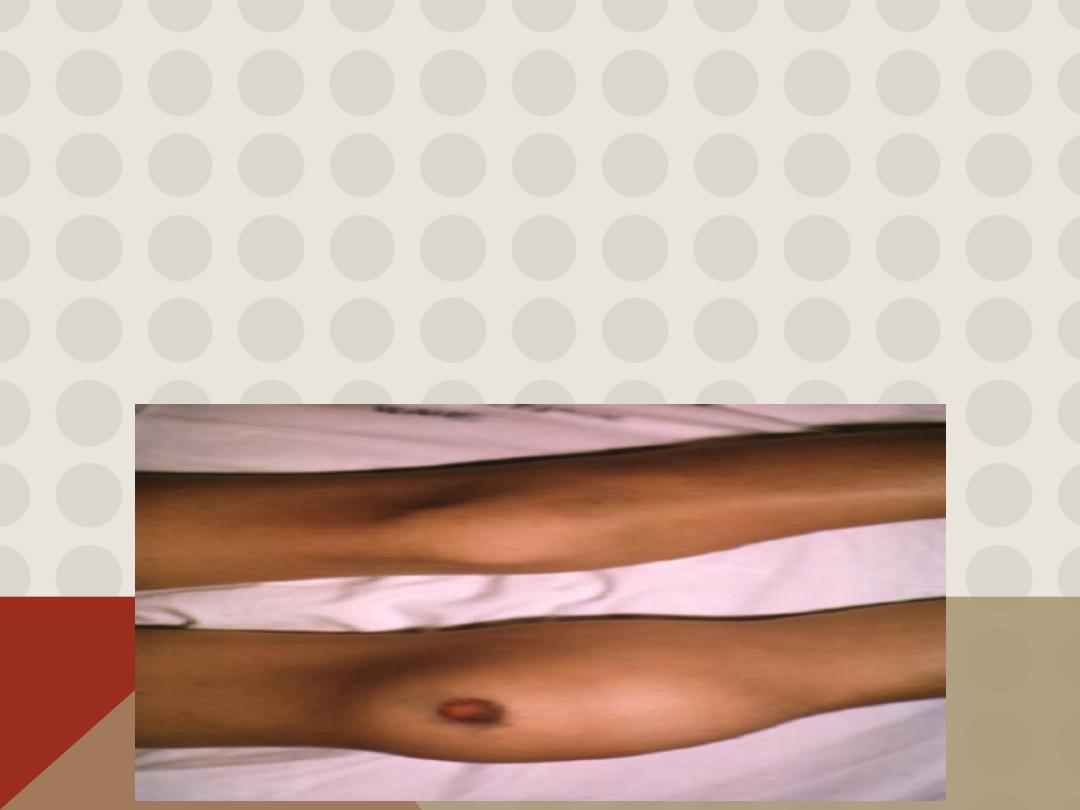
Hemarthrosis (joint bleeding)
Haematoma
A large bruise throughout the subcutaneous tissue or muscle (caused by extravasation into
the perivascular tissue) resulting in changes in the colour and shape of the affected area. A
haematoma may also be caused by
a defect in the coagulation
mechanism such as occurs in
haemophilia, leukaemia or pathological fibrinolysis.
.
Hemophilia Hemophilia
is a group of sex-linked inherited blood disorders, characterized by
prolonged clotting time. However, the bleeding time is normal. Usually, it affects the
males, with the females being the carriers.
Because of prolonged clotting time, even a mild trauma causes excess bleeding which can
lead to death. Damage of skin while falling or extraction of a tooth may cause excess
bleeding for few weeks. Easy bruising and hemorrhage in muscles and joints are also
common in this disease.
Causes of hemophilia
Hemophilia occurs due to lack of formation of prothrombin activator. That is why the
coagulation time is prolonged. The formation of prothrombin activator is affected due to
the deficiency of factor VIII, IX or XI.
Types of hemophilia
Depending upon the deficiency of the factor involved, hemophilia is
classified into three types:
. Hemophilia A or classic hemophilia: Due to the deficiency of factor VIII. 85% of people with
hemophilia are affected by hemophilia A.
Hemophilia B or Christmas disease: Due to the deficiency of factor IX. 15% of people with
hemophilia are affected by hemophilia B.
Hemophilia C or factor XI deficiency: Due to the deficiency of factor XI. It is a very rare
bleeding disorder

Symptoms of hemophilia
i
. Spontaneous bleeding.
ii. Prolonged bleeding due to cuts, tooth extraction and surgery.
iii. Hemorrhage in gastrointestinal and urinary tracts. iv. Bleeding in joints followed by swelling and pain
v. Appearance of blood in urine.
Treatment for hemophilia Effective therapy for classical hemophilia involves replacement of missing
clotting factor.
*
von Willebrand disease
: partial absence of von Willebrand factor
dominant inheritance mild or moderate bleeding
In this disorder there is either a reduced level or abnormal function of VWF resulting from a point
mutation or major deletion. VWF is produced in endothelial cells and megakaryocytes. It has two
roles.
1- It promotes platelet adhesion to damaged endothelium and
2- It is the carrier molecule for factor VIII, protecting it from premature destruction.
Three types of VWD have been described. Type 1 accounts for 75% of cases. VWD is the most common
inherited bleeding disorder. Usually, the inheritance is autosomal dominant with varying expression.
The severity of the bleeding is variable , there is mucous membrane bleeding (e.g. epistaxes,
menorrhagia), excessive blood loss from superficial cuts and abrasions.
Haemarthroses and muscle haematomas are rare, except in type 3 disease.
Laboratory findings …..The bleeding time can be prolonged.
Factor VIII levels are often low. If low, a factor VIII VWF binding assay is performed.
The APTT may be prolonged.
VWF levels are usually low.
Acquired Bleeding Disorder
Partial Absence of several clotting factors
Liver disease
Vitamin K deficiency
Disseminated Intravascular Coagulation & fibrinolysis (DIC)
Anticoagulant drugs: warfarin or heparin
Thrombolytic drugs (plasminogen activators)
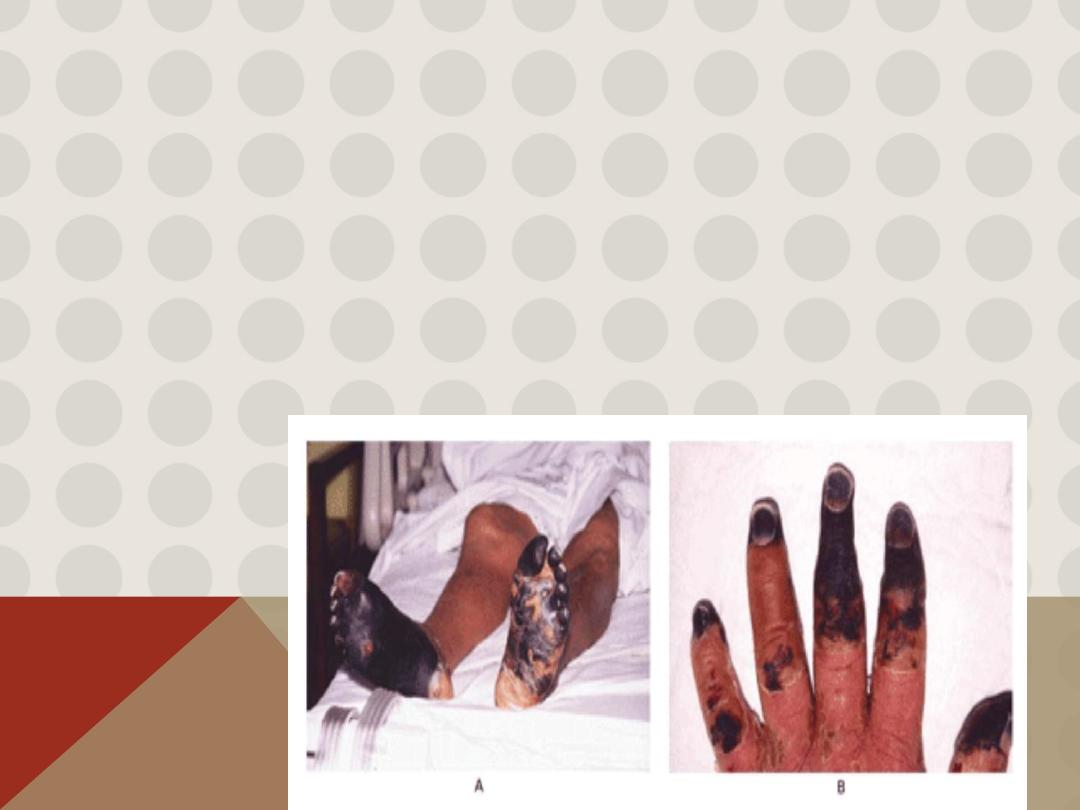
DISSEMINATED INTRAVASCULAR COAGULATION
Associated with many serious/lifethreatening diseases
Circulating blood exposed to excessive amount of tissue factor or other procoagulant
Breakdown of normal regulatory processes
Formation of circulating (soluble) fibrin
Consumption of clotting proteins and platelets
Accelerated fibrinolysis – clots break down too quickly
Bleeding and/or intravascular clotting in severe cases
Thanks for you
