Blood Physiology
Lecture 7
Dr. Suroor
Immunity
Immunity
is body's ability to resist or eliminate
potentially harmful foreign materials or abnormal
cells like bacteria, virus, toxic substances.
Immunity is of two types:
I. Innate immunity.
II. Acquired immunity.
Consists of following activities:
Defense against invading pathogens (viruses & bacteria)
Removal of 'worn-out' cells (e.g., old RBCs) & tissue debris (e.g.,
from injury or disease)
Identification & destruction of abnormal or mutant cells (primary
defense against cancer)
Rejection of 'foreign' cells (e.g., organ transplant)
Inappropriate responses:
Allergies - response to normally harmless substances
Autoimmune diseases
The immunity of 2 main types : Innate (natural)& Acquired
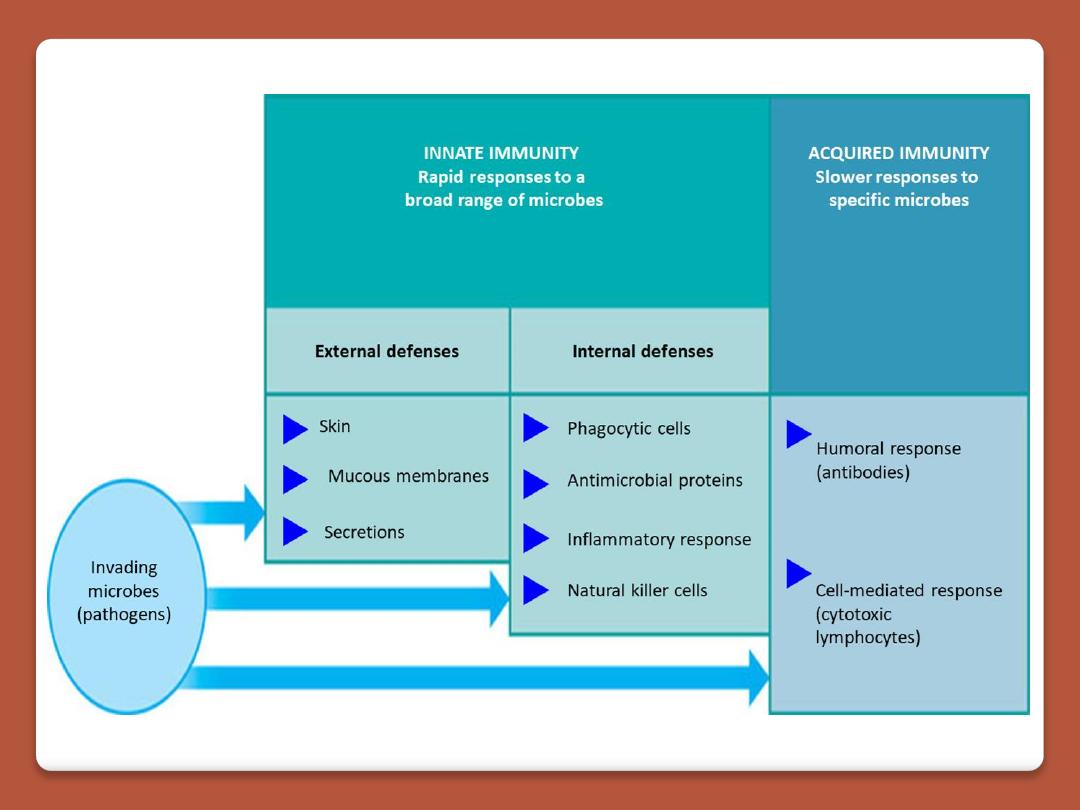
Innate immunity is the inborn capacity of the body to resist
pathogens. if the organisms enter the body, innate immunity
eliminates them before the development of any disease.
It is called the natural or non-specific immunity, represents the
first line of defense against any type of pathogens
Innate or natural immunity involving:
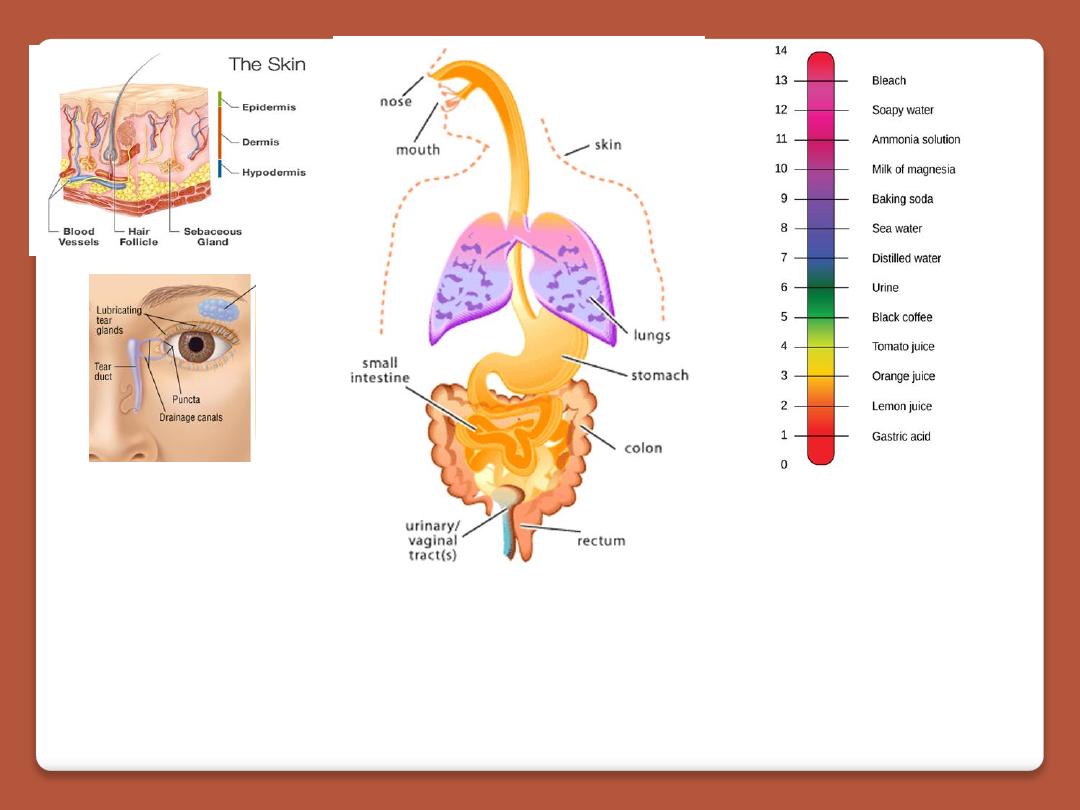
1. Phagocytosis of bacteria and other invaders by white blood cells
and cells of the tissue macrophage system
2. Destruction of swallowed organisms by the acid secretions of the
stomach and the digestive enzymes.
3. Resistance of the skin to invasion by organisms.
4. Presence in the blood of certain chemicals and cells that attach to
foreign organisms or toxins and destroy them.
Innate immunity
relies on mechanisms already existing before microbe infects host
is the first line of defense
has no memory for subsequent exposure
relies on non specific mechanisms
The cells that mediate innate immunity include neutrophils,
macrophages, and natural killer (NK) cells, large lymphocytes
cytotoxic one . All these cells respond to lipid and carbohydrate
sequences unique to bacterial cell walls and to other substances
characteristic of tumor and transplant cells.
„
ACQUIRED IMMUNITY OR SPECIFIC IMMUNITY
Acquired immunity is the resistance developed in the body
against any specific foreign body like bacteria, viruses, toxins,
vaccines or transplanted tissues , known as specific
immunity.
It is the most powerful immune mechanism that protects the
body from the invading organisms or toxic substances.
Lymphocytes
are responsible for acquired immunity
Two types of acquired immunity develop in the body:
1. Cellular immunity
2. Humoral immunity
Adaptive immunity
develops following entry of microbe into the host
comes into action after innate immunity fails to get rid of
microbe
has memory to deal with subsequent exposure
happens through specific cells
T cells (cell mediated)
B cells (antibody mediated
Humoral immunity
is mediated by circulating immunoglobulin
antibodies in the γ-globulin fraction of the plasma proteins. Humoral
immunity is a major defense against bacterial infections.
Immunoglobulins
are produced by B lymphocytes, and they activate the
complement system and attack and neutralize antigens.
Cellular immunity
is mediated by T lymphocytes. It is responsible for
delayed allergic reactions and rejection of transplants of foreign tissue.
Cytotoxic T cells attack and destroy cells that have the antigen which
activated them. Cellular immunity constitutes a major defense against
infections due to viruses, fungi, and a few bacteria such as the tubercle
bacillus. It also helps defend against tumors.
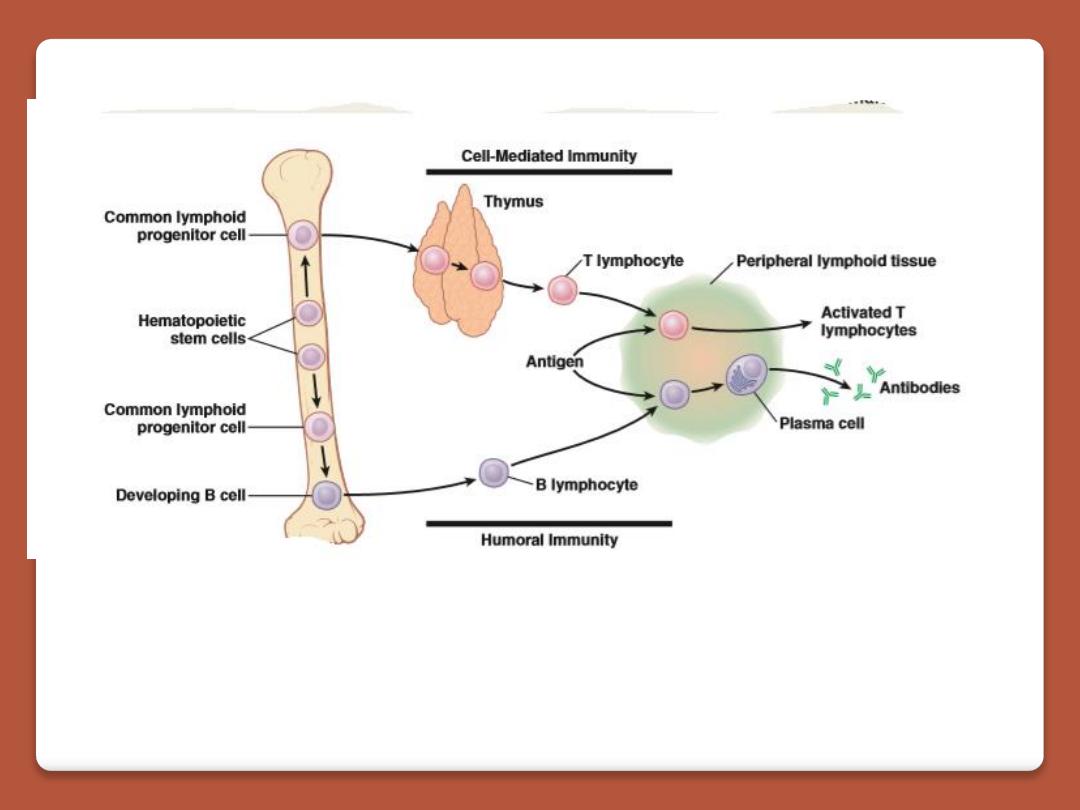
Development of the Immune System
During fetal development, lymphocyte precursors
come from the bone marrow. Those that populate
the
thymus
become transformed by the environment in
this organ into the lymphocytes responsible for cellular
immunity
(T lymphocytes).
humoral immunity
(B lymphocytes
the transformation
to B lymphocytes occurs in
bursal equivalents
, ie, the
fetal liver and, after birth, the
bone
marrow. After
residence in the thymus or liver, many of the T and B
lymphocytes migrate to the lymph nodes and bone
marrow. Most of the processing occurs during fetal and
neonatal life. However, there is also a slow, continuous
production of new lymphocytes from stem cells in
adults.
B cells
differentiate
into plasma cells and memory B cells.
Memory B cells “remember” specific antigens and can launch fast
immune response if antigen is encountered again.
three major types
of T cells
:
cytotoxic T cells, helper T cells, and
memory T cells.
There are two subtypes of
helper T cells
:
T helper 1 (TH1) cells secrete IL-2 and γ-interferon and are concerned
primarily with cellular immunity;
T helper 2 (TH2) cells secrete IL-4 and IL-5 and interact primarily with
B cells in relation to humoral immunity.
Cytotoxic T cells
destroy transplanted and other foreign cells, with their
development aided and directed by helper T cells.
Markers on the surface of lymphocytes are assigned CD (clusters of
differentiation) numbers on the basis of their reactions to a panel of
monoclonal antibodies. Most
cytotoxic T
cells display the glycoprotein
CD8,
CD8+ T cells destroy infected cells containing microbes or
microbial proteins and
helper T
cells display the glycoprotein
CD4.
CD4+ T cells activate phagocytes to kill microbes
These proteins are closely associated with the T cell receptors and may
function as coreceptors.
Natural killer cells
are also cytotoxic lymphocytes, though they are not
T cells. limits the spread of tumors and microbial infections by inducing
apoptosis in cells, limiting tissue damage
Memory B Cells & T Cells
After exposure to a given antigen, a small number of activated B
and T cells persist as memory B and T cells. These cells are readily
converted to effector cells by a later encounter with the same
antigen. This ability to produce an accelerated response to a
second exposure to an antigen is a key characteristic of acquired
immunity. The ability persists for long periods of time, and in
some instances (eg, immunity to measles) it can be lifelong.
It had been argued that the long life of memory cells involves
their repeated exposure to small amounts of antigen.
Role of the T Cells in Activation of the B
Lymphocytes.
Most antigens activate both T lymphocytes and B
lymphocytes at the
same time
, some of the
T-cells that
are formed, called T-helper cells, secrete specific
substances (collectively called lymphokines) that activate
the specific
B lymphocytes
. Indeed, without the aid of
these T-helper cells, the quantity of antibodies formed by
the B lymphocytes is usually slight.
Formation of Antibodies by Plasma Cells
.
Before exposure to a specific antigen, the clones of B
lymphocytes remain dormant in the lymphoid tissue. Upon entry
of a foreign antigen, macrophages in lymphoid tissue phagocytize
the antigen and then present it to adjacent B lymphocytes.
the antigen is presented to T cells at the same time, and
activated T-helper cells are formed. These helper cells also
contribute to extreme activation of the B lymphocytes. The B
lymphocytes specific for the antigen immediately enlarge and take
on the appearance of lymphoblasts
The mature plasma cell then produces gamma globulin antibodies
at an extremely rapid rate—about 2000 molecules per second for
each plasma cell. the antibodies are secreted into the lymph and
carried to the circulating blood. This process continues for several
days or weeks until finally exhaustion and death of the plasma
cells occur.
Antibodies
are gamma globulins called immunoglobulins (Ig) that
have molecular weights between 160,000 and 970,000 and
constitute about 20 percent of all the plasma proteins.
All the immunoglobulins are composed of combinations of
light and
heavy polypeptide chains
. Most are a combination of two light and
two heavy chains, some of the immunoglobulins have combinations
of as many as 10 heavy and 10 light chains, which give rise to high-
molecular-weight immunoglobulins.
in all immunoglobulins, each heavy chain is paralleled by a light
chain at one of its ends, thus forming a heavy-light pair, and there
are always at least 2 and as many as 10 such pairs in each
immunoglobulin molecule.
Ig as designated end of each light and heavy chain, called the
variable portion; the remainder of each chain is called the constant
portion. T
he variable portion
is different for each specific antibody,
and it is this portion that attaches specifically to a particular type of
antigen.
The constant portion
of the antibody determines other
properties of the antibody. A combination of noncovalent and
covalent bonds (disulfide) holds the light and heavy chains together.
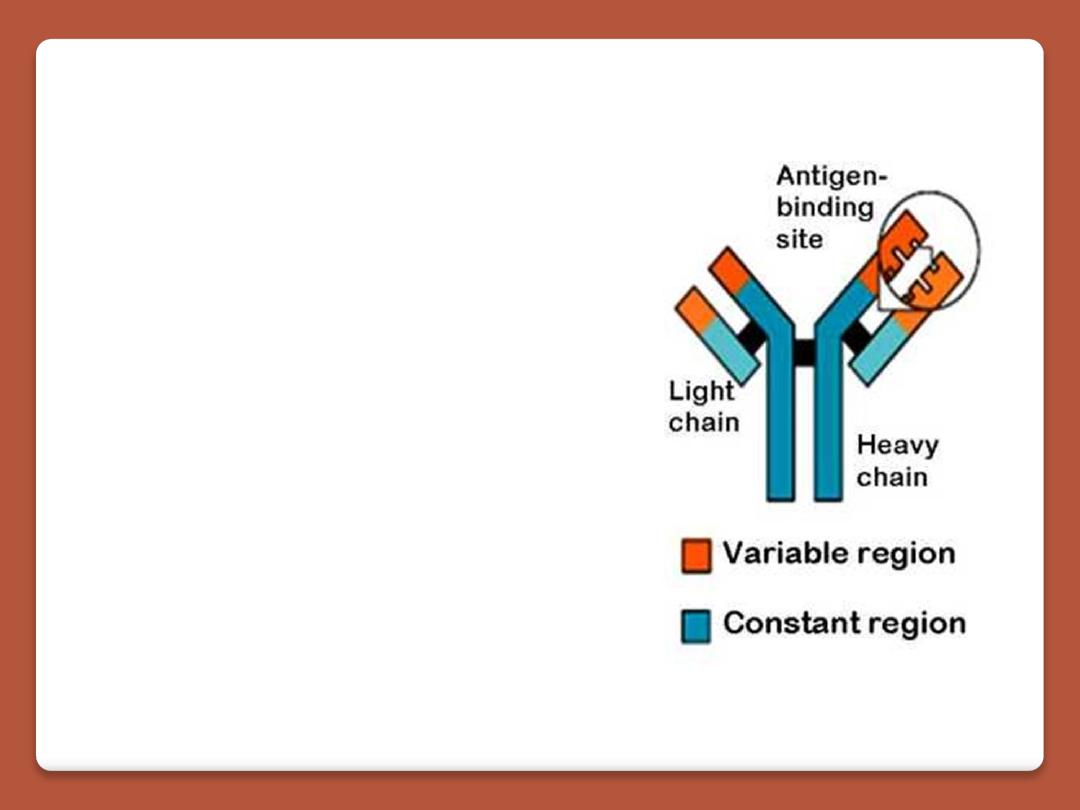
Belong to the gamma-globulin
fraction of serum proteins
Y-shaped or T-shaped polypeptides
2 identical heavy chains
2 identical light chains
All immunoglobulins are not
antibodies
Five kinds of antibodies
IgG, IgM, IgA, IgD, IgE
these classes of antibodies are of particular importance:
IgG,
which is a bivalent antibody and constitutes about 75 percent
of the antibodies of the normal person, and IgE, which constitutes
only a small percentage of the antibodies but is especially involved
in allergy. The IgM class is a large share of the antibodies formed
during the primary response are of this type. These antibodies
have 10 binding sites that make them exceedingly effective in
protecting the body against invaders, even though there are not
many IgM antibodies
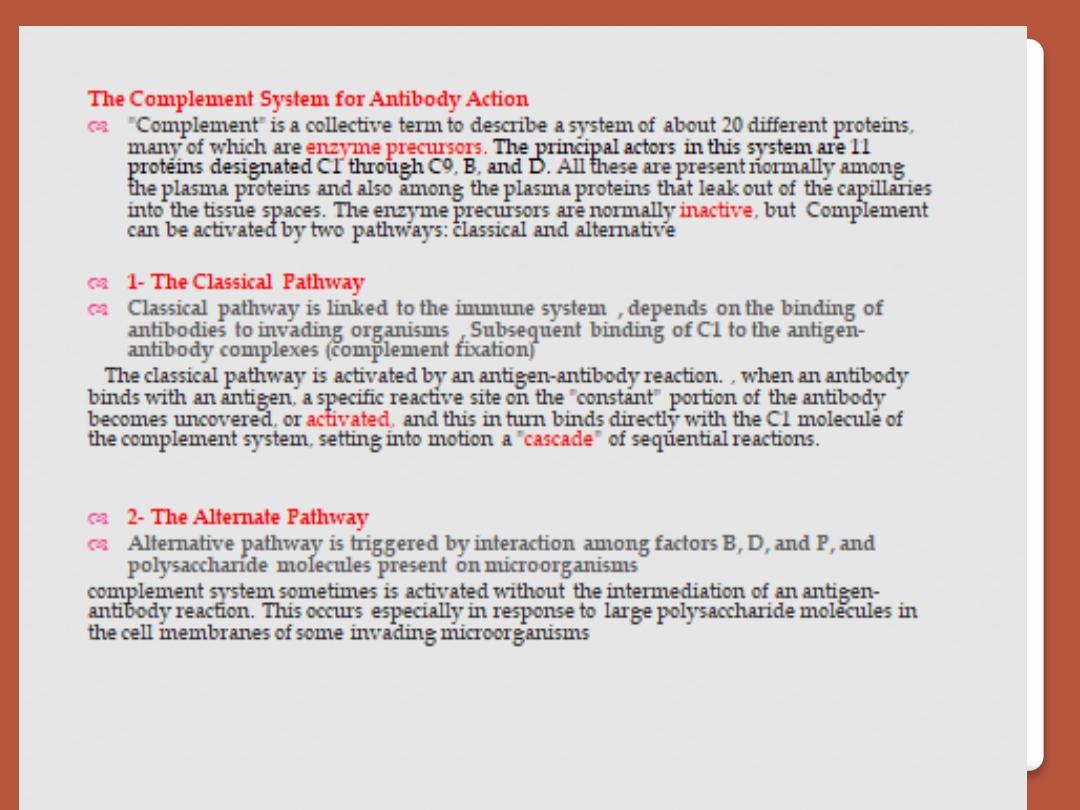
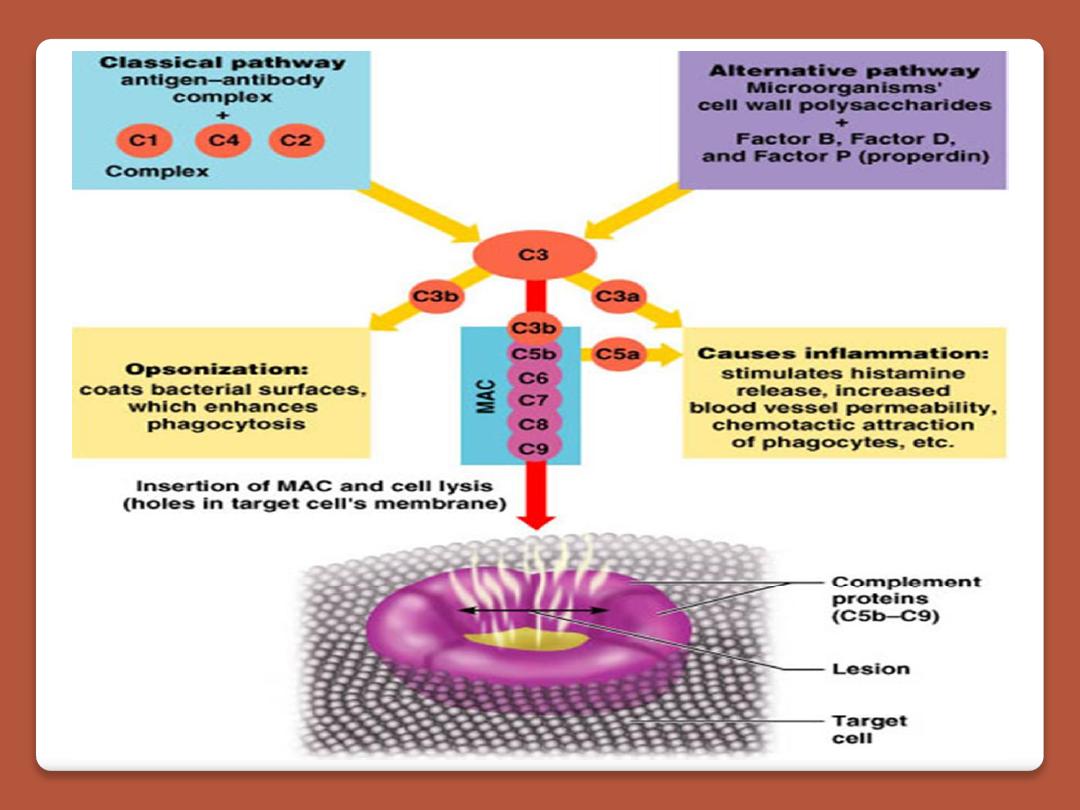
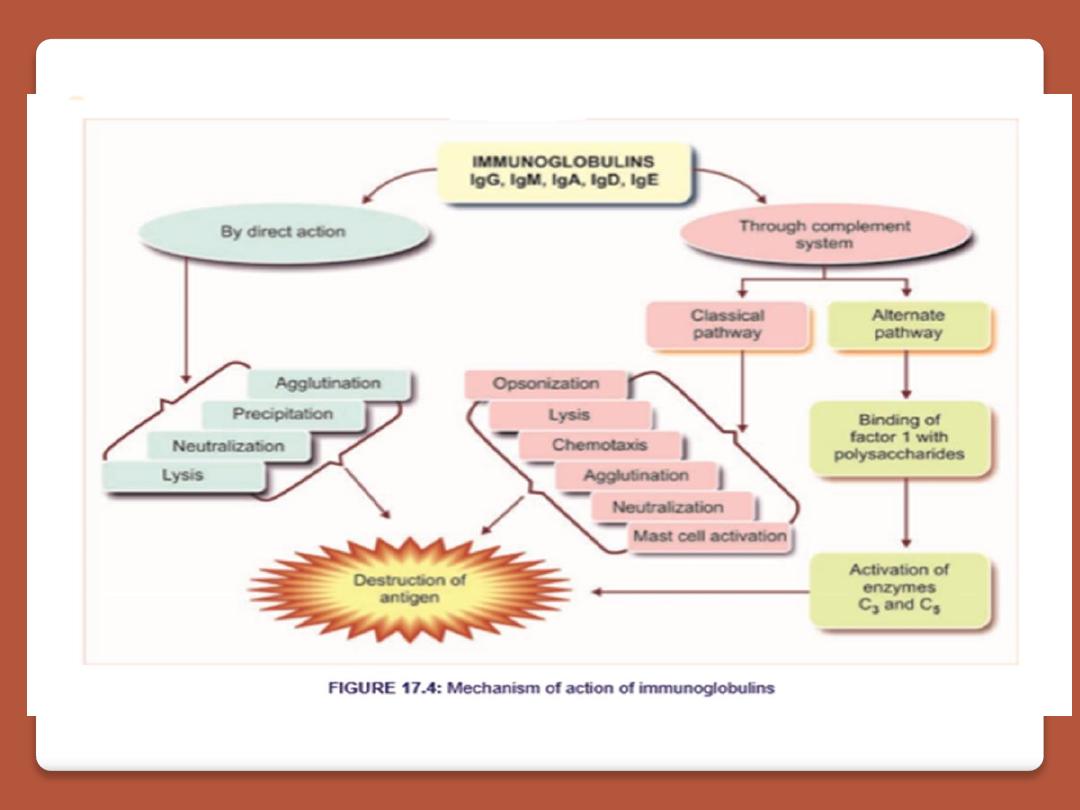
Mechanisms of Action of Antibodies
Antibodies act mainly in two ways to protect the body against
invading agents: (1) by direct attack on the invader and (2) by
activation of the “complement system” that then has multiple
means of its own for destroying the invader.
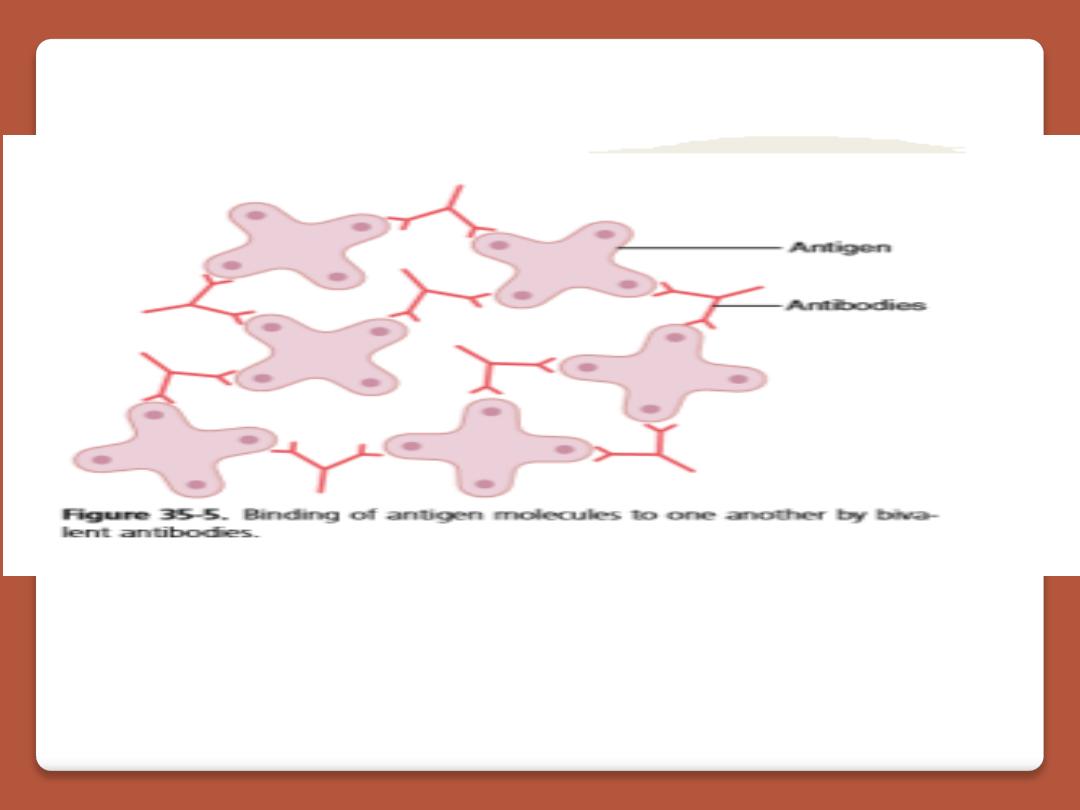
Because of the bivalent nature of the antibodies and the
multiple antigen sites on most invading agents, the antibodies
can inactivate the invading agent in one of several ways, as
follows:
1. Agglutination, in which multiple large particles with antigens
on their surfaces, such as bacteria or red cells, are bound
together into a clump
2. . Precipitation, in which the molecular complex of soluble
antigen (such as tetanus toxin) and antibody becomes so
large that it is rendered insoluble and precipitates
3. . Neutralization, in which the antibodies cover the toxic sites
of the antigenic agent
4. Lysis, in which some potent antibodies are occasionally
capable of directly attacking membranes of cellular agents and
thereby cause rupture of the agent
.
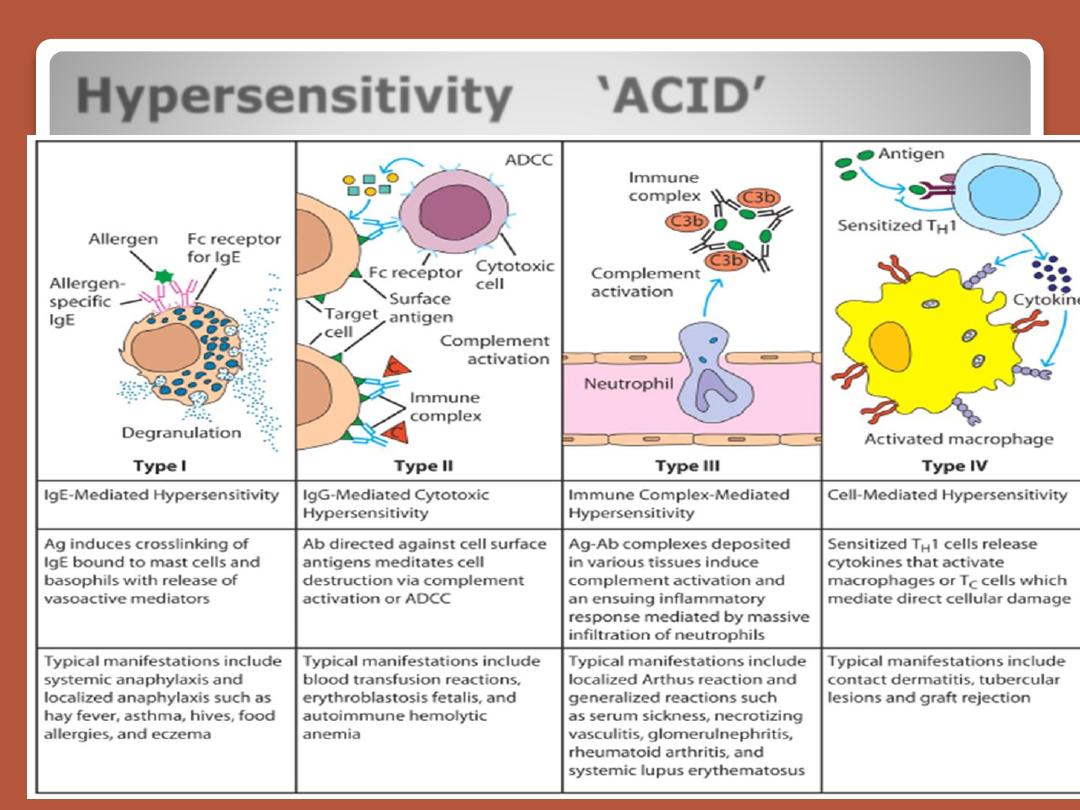
Hypersensitivity ‘ACID’

