Dr. Noor
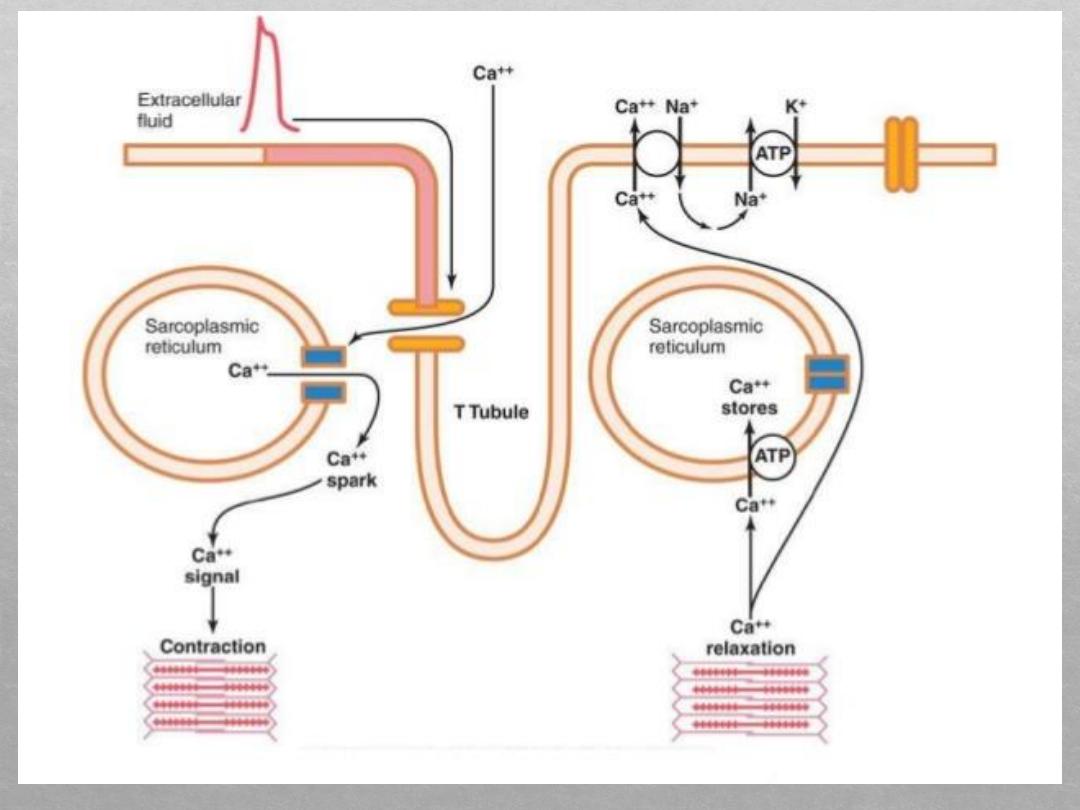
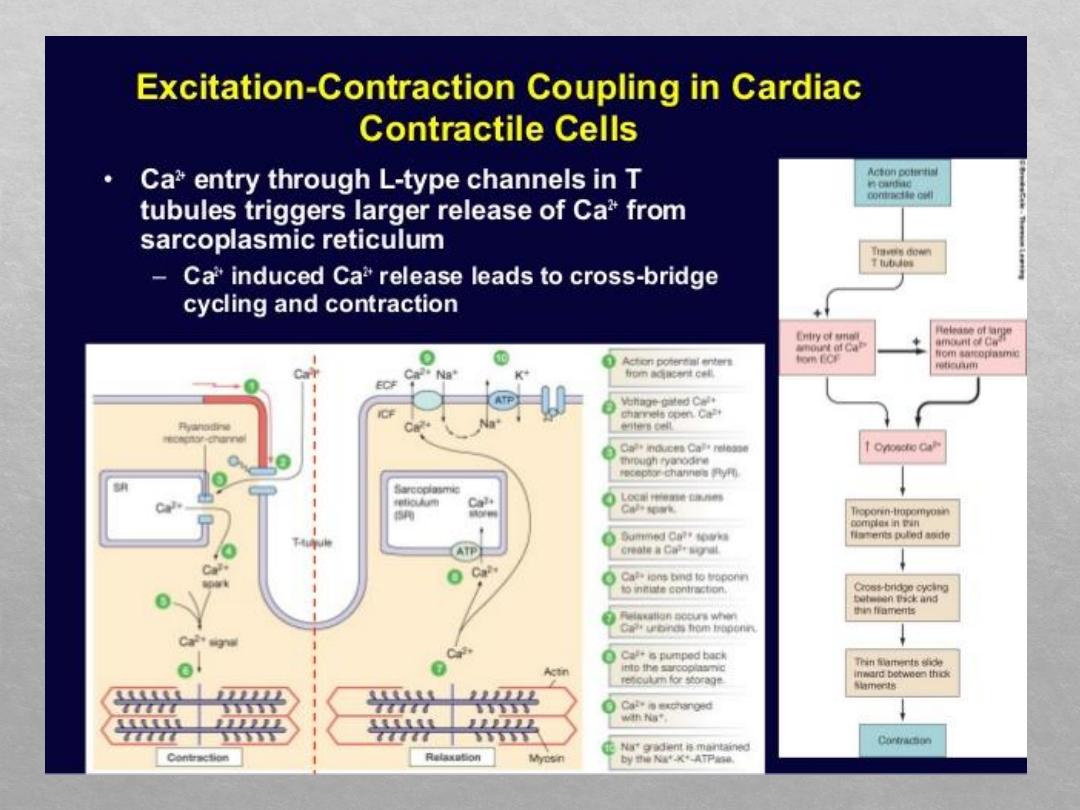
This mechanism of excitation-contraction coupling
is the same as that for skeletal muscle, but there is a
second effect that is quite different. In addition to the
calcium ions that are released into the sarcoplasm
from the cisternae of the sarcoplasmic reticulum,
calcium ions also diffuse into the sarcoplasm from
the T tubules themselves at the time of the action
potential, which opens voltage-dependent calcium
channels in the membrane of the T tubule .
Calcium entering the cell then activates calcium
release channels, also called ryanodine receptor
channels, in the sarcoplasmic reticulum membrane,
triggering the release of calcium into the sarco-
plasm. Calcium ions in the sarcoplasm then interact
with troponin to initiate cross-bridge formation and
contraction by the same basic mechanism.
The strength of contraction of cardiac muscle depends
to a great extent on the concentration of calcium ions
in the extracellular fluids.
In contrast, the strength of skeletal muscle contraction
is hardly affected by moderate changes in extracellular
fluid calcium concentration because skeletal muscle
contraction is caused almost entirely by calcium ions
released from the sarcoplasmic reticulum inside the
skeletal muscle fiber.
At the end of the plateau of the cardiac action potential,
the influx of calcium ions to the interior of the muscle
fiber is suddenly cut off, and calcium ions in the sarco-
plasm are rapidly pumped back out of the muscle fibers
into both the sarcoplasmic reticulum and the T tubule–
extracellular fluid space. Transport of calcium back into
the sarcoplasmic reticulum is achieved with the help of a
calcium–adenosine triphosphatase (ATPase) pump.
Duration of Contraction
. Cardiac muscle begins to
contract a few milliseconds after the action potential
begins and continues to contract until a few
milliseconds after the action potential ends.
Therefore, the duration of contraction of cardiac
muscle is mainly a function of the duration of the
action potential, including the plateau— about 0.2
second in atrial muscle and 0.3 second in ventricular
mature contraction.
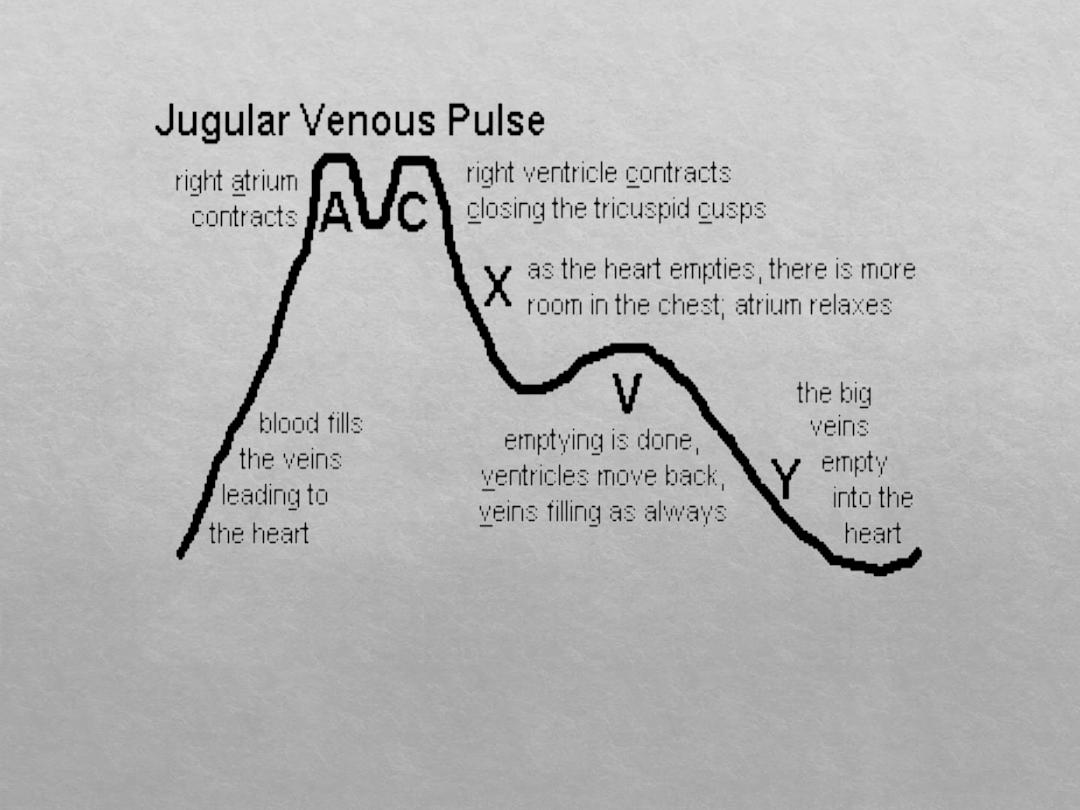
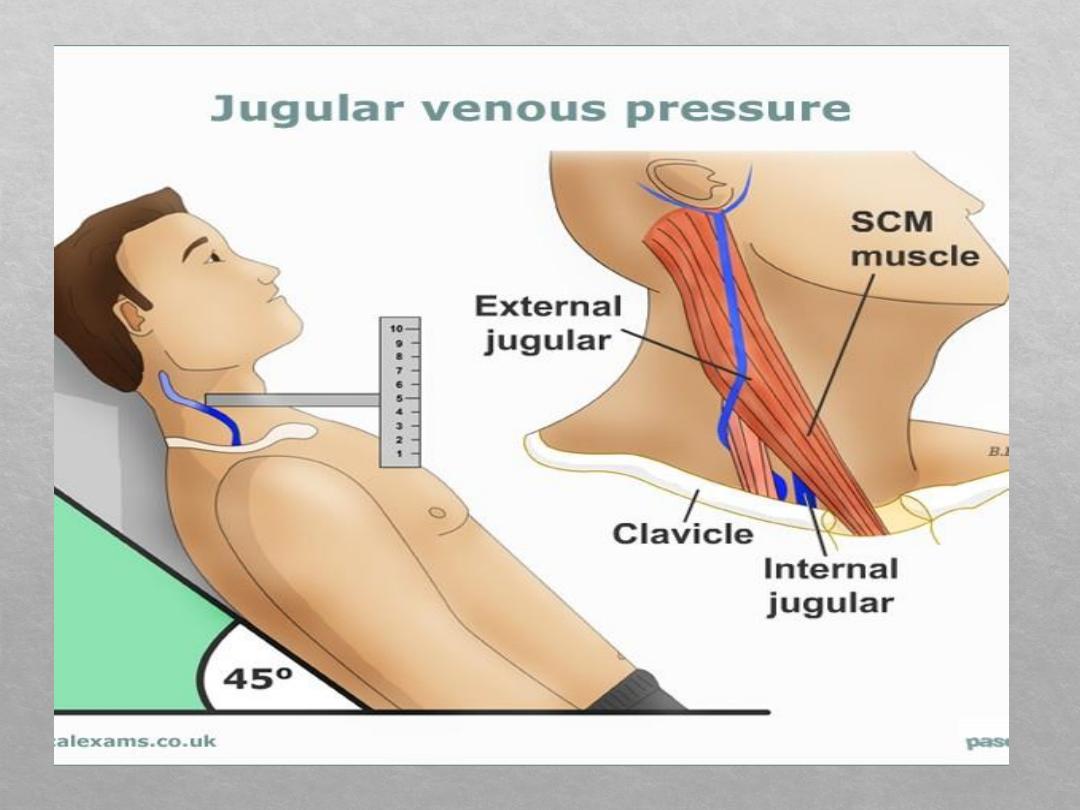
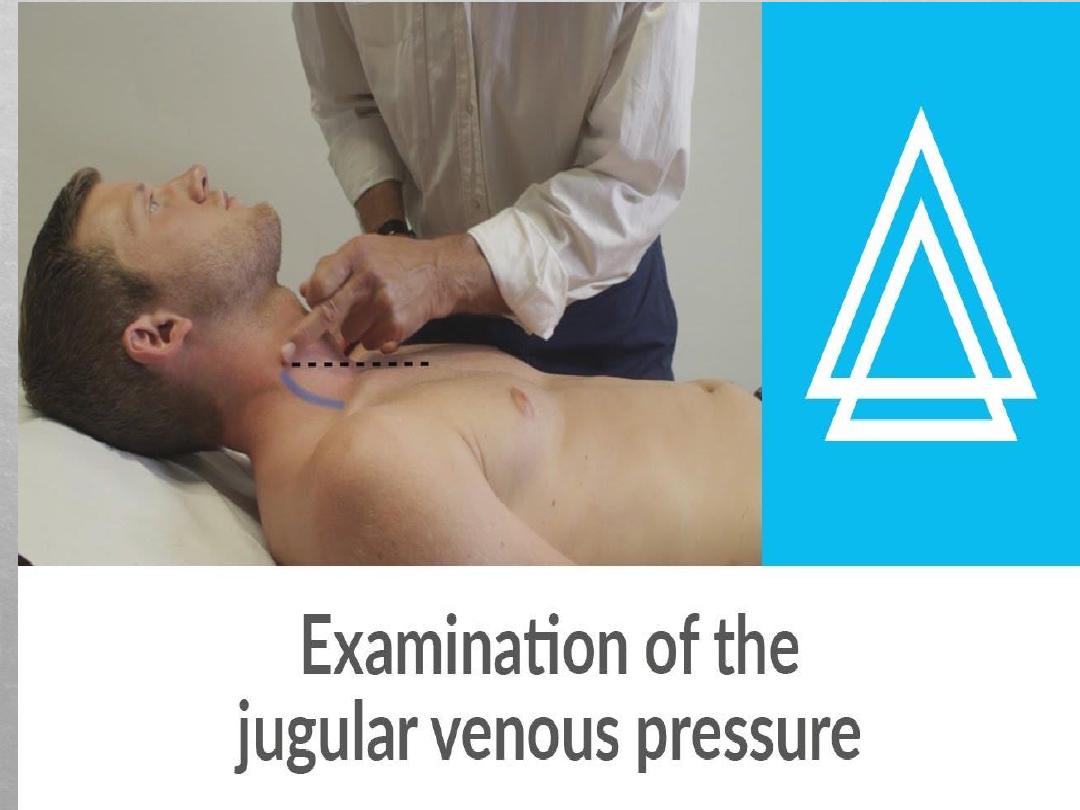
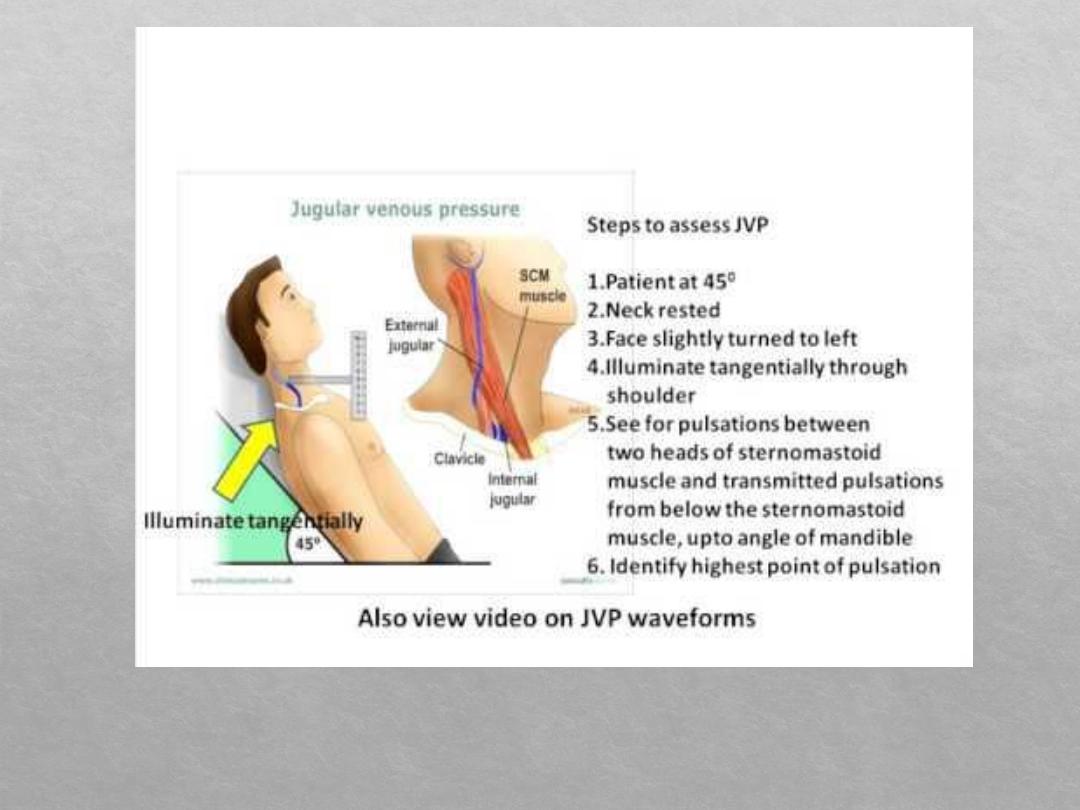
Jugular venous pressure
The jugular venous pressure (JVP, sometimes referred
to as jugular venous pulse) is the indirectly observed
pressure over the
via visualization of
the
. It can be useful in the
differentiation of different forms of
. Classically three upward deflections and two
downward deflections have been described.
The upward deflections are the "a" (atrial contraction),
"c" (ventricular contraction and resulting bulging of
tricuspid into the right atrium during isovolumetric
systole) and "v" = venous filling
The downward deflections of the wave are the "x" (the
atrium relaxes and the tricuspid valve moves
downward) and the "y" descent (filling of ventricle
after tricuspid opening).
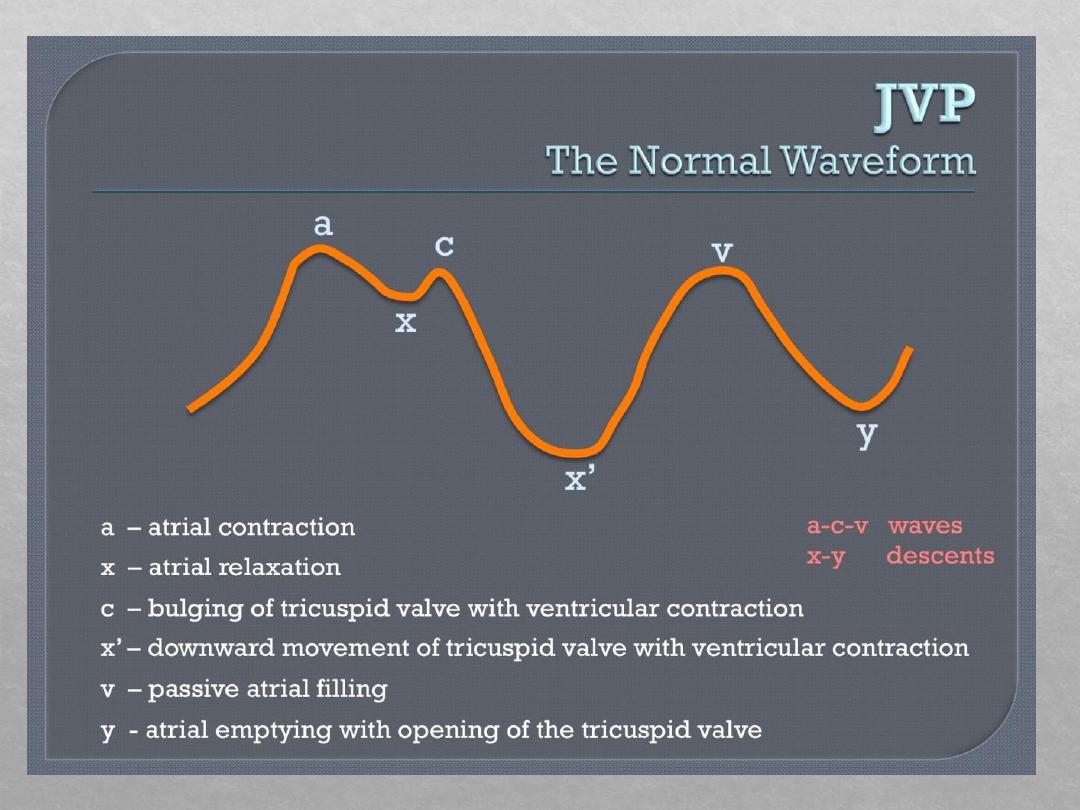
JVP waveform
The jugular venous pulsation has a biphasic waveform.
The " a " wave corresponds to right Atrial contraction
and ends synchronously with the carotid artery pulse.
The peak of the 'a' wave demarcates the end of atrial
systole.
The " c " wave corresponds to right
ventricular Contraction causing the triCuspid valve to
bulge towards the right atrium.
The " x' " (x prime) descent follows the 'c' wave and
occurs as a result of the right ventricle pulling the
tricuspid valve downward during ventricular systole.
(As
is ejected, the ventricle takes up less
space in
, allowing relaXed atrium to
enlarge). The x' (x prime) descent can be used as a
measure of right ventricle contractility.
The " x " descent follows the 'a' wave and corresponds
to atrial relaXation and rapid atrial filling due to low
pressure.
The " v " wave corresponds to Venous filling when
the tricuspid valve is closed and venous pressure
increases from venous return
The " y " descent corresponds to the rapid emptYing
of the atrium into the ventricle following the opening
of the tricuspid valve