Lymphocytes
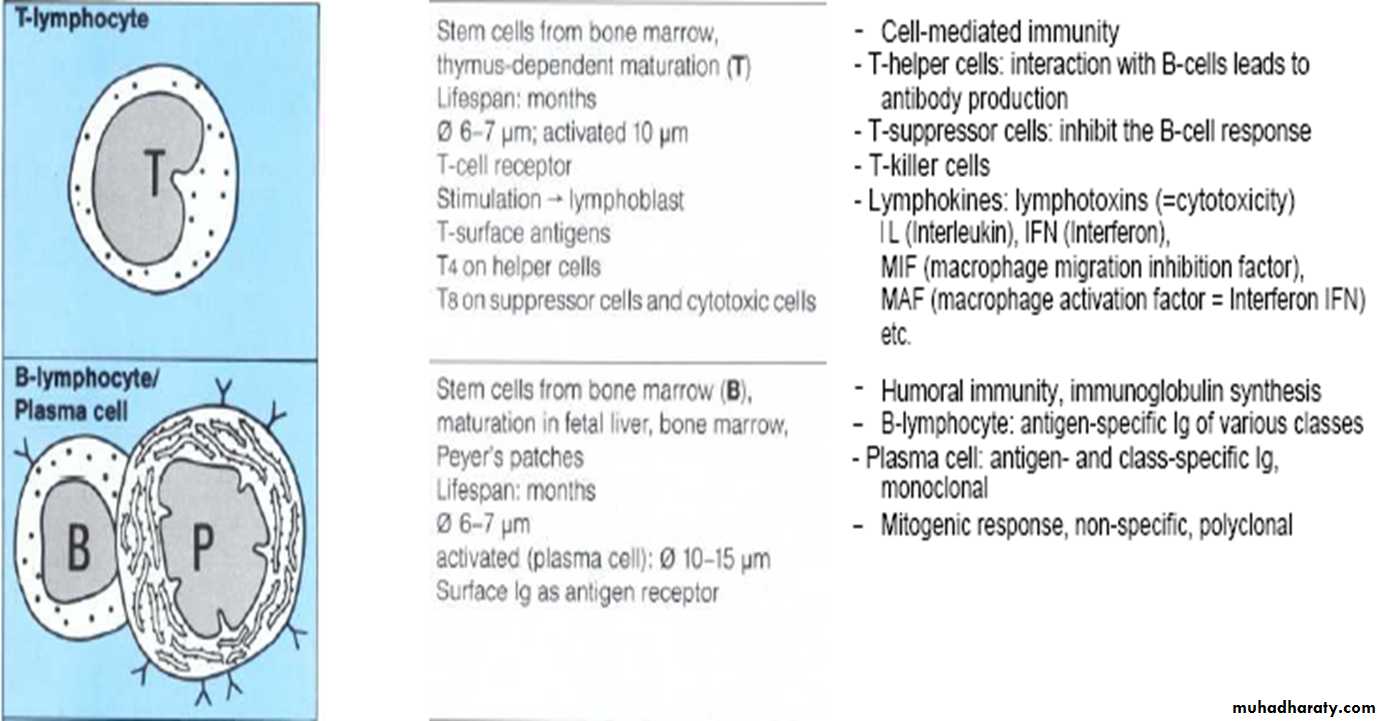
Three main types of L. are distinguished on the bases of their receptors for Ag: T, B, and NK (natural killer) cellsB & T cells are inactive & small size in blood, while NK cells are active, large & appear well differentiated in blood
B & T cells stay only 30 min & to function properly they require additional influence of lymphoid organs (L.N., thymus, spleen, tonsils & adenoids)
Lymphocytes
T cells recognize Ag using low affinity trans-membranous complex (T cell Ag receptor TCR), they are subdivided whether they posses co-receptors into CD4 or CD8CD4+ initiate & help immunity by providing proliferation & differentiation signals (T helper)
CD8+ are predominantly cytotoxic T cell involved in controlling intracellular Ag i.e. killing of cell presenting Ag (T suppressor cells)
Lymphocytes (B cells)
B cells help to control extracellular Ag, B cells recognize Ag using B cell Ag receptor (BCR) which is a high affinity Ag receptor that enable B cell to bind & ingest Ag, ingested Ag is degraded & presented to T cellsB L. that stimulated to undergo blastogenesis (Transformation of small lymphocytes into larger cells that are capable of undergoing mitosis) which consist of enlargement of cell with synthesis of protein & mitotic division that increase no. of cells which are specific for particular Ag (clonal expansion: means proliferation of Ag specific cells)
Some oral bact. like Actinomyces & some Strept. produce substances that inhibit blast transformation
Lymphocytes (B cells)
After Ag exposure, some B cells differentiate to form plasma cells which produce AB, while other B cells in the presence of T cells differentiate to memory cells that give rise to plasma cells upon 2ndary exposure to Ag & produce high affinity AB
Each Memory cell bears specific receptors which recognize Ag
Lymphocytes (NK cells)
NK cells recognize & kill certain tumor cells & virally infected cells / or cells infected by MOSuch cells posses Ag receptors including killer inhibitory receptors (KIR) & killer activating receptors (KAR)
KIR prevent NK cells from attack normal cell
Antibodies (AB)
AB is an immunoglobulin that binds to a known AgEach human posses genetically distinct ABs:
• IgE, IgM, IgD, IgG (IgG1, IgG2, IgG3 & IgG4),
• IgA (IgA1, IgA2)
IgG: Neutralizes bacterial toxins, bind to MO thereby enhance there phagocytosis
IgM: Efficient activator of Complement system
IgD: Recognizes Ag receptor on surface of lymphocytes
IgA: Secretory IgA prevents adhesion of MO to tissue surface, Serum IgA thought to modulate function of PNL by depressing chemotaxis & phagocytic activity
IgE: Acute allergic reaction
Primary & Secondary immune response (I.R.)
PD patients have circulating T L. that sensitized to Ag (MO) or their substances originating from subgingival plaque, produced following initial exposure to that Ag (Primary IR) & upon re-exposure to the same Ag they respond by proliferation & synthesizing lymphokines (Secondary IR)2ndary IR is more rapid in onset & longer in duration & it’s greater in strength due to the higher titer (of L especially B cells) & the B cells have greater specificity against Ag than primary response
Correlation exists between sensitized L. & severity of PD disease
Primary & secondary immune response (I.R.)
In normal gingiva, there are T L. while B L. & plasma cells are not seen in significant no.In gingivitis at early lesion, T-cells are predominant, later on with increased severity of the disease, B L. & plasma cells will increase
In periodontitis: plasma cells & lymphocytes mostly B are predominant
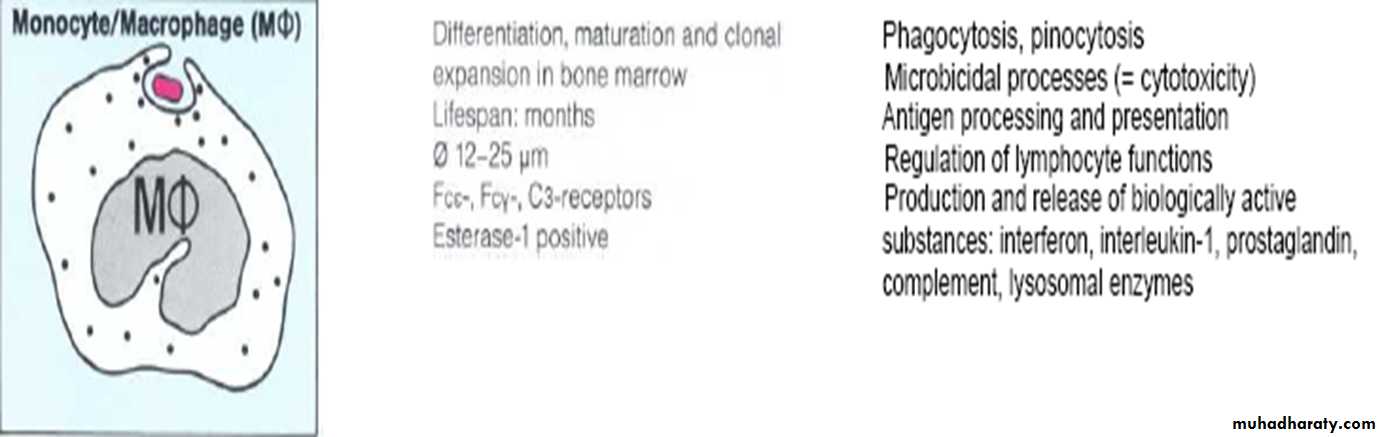
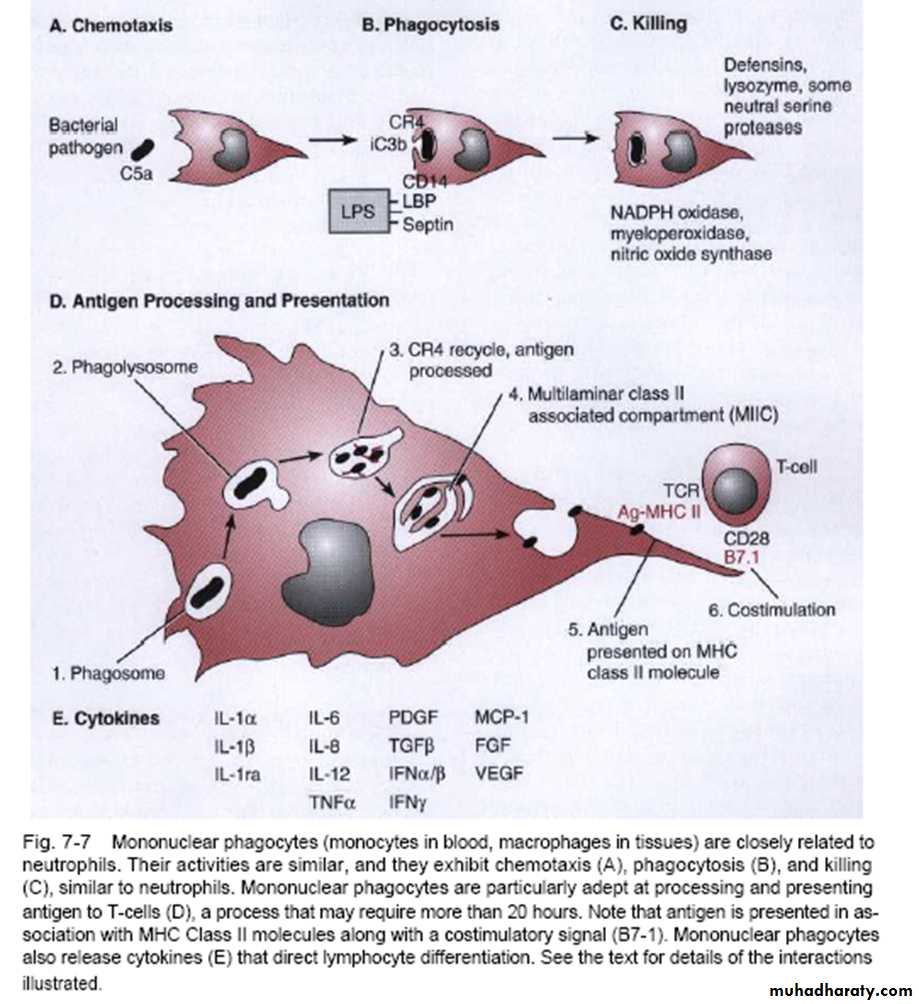
Macrophages
Are large highly phagocytic cells which are part of the Reticuloendothelial system (Mononuclear phagocytic system) (part of immune system)In inflammatory lesions, M formed by differentiation of monocytes that carried to the lesion or infected site by blood
M attracted to the site of inflam. by lymphokines & complements then retained in this site by other lymphokines ( MCF, MAF, MMIF)
• For your information:
• MCF: macrophage cytotoxicity factor• MAF: macrophage activating factor
• MMIF ( or MIF): macrophage migration inhibitory factor
Macrophages
Macrophages
Ag penetrate into connective tissue through gingival epithelium, macrophage phagocyte it & alter it to a form recognizable by the immune system, then CD4+ activated which control proliferation of other T & B cellsSo the main functions of M are:
• 1- Killing of MO (by phagocytosis)
• 2- Presenting MO (Ag) to T-lymphocytes
• 3- Production of monokines (cytokines)
Inadequate immune response
PD patients may suffer from an inadequate I.R. to gingival infection, expressed in several ways• 1. Host must recognize bact. As a foreign Ag to build or initiate I.R. (This can’t happen in some patients)
• 2. Some MO suppress I.R.
• 3. Some MO neutralize or degrade AB
• 4. Some MO exhibit Ag variation
• 5. Continuous infection with different bacteria
Inadequate immune response
Examples of bacterial challenges to the I.R.:
1. Destruction of N such as A.a.
2. Inhibition of N chemotaxis such as Capnocytophaga
3. Impairment of N adherence & phagocytosis (For ex by polysaccharide capsule of black pigmented bacteroides )
4. Degeneration of opsonizing AB & complements such as Capnocytophaga
5. Inhibition of O2 radical activity by catalase enzyme of P.g. & A.a.
6. Inhibition of lysosomal degradation
7. Degradation of lactoferrin asuch s P.g.