Odontogenic infection/ Incision and Drainage
Principles for management of odontogenic infections• Assess disease severity and systemic state.
• Emergency surgical or medical intervention as needed.
• Evaluate patient.
• Decide on setting of care (outpatient or admission).
• Pus/discharge—swab for culture and sensitivity test.
• Start antibiotics empirically and then change as per sensitivity test.
• Treat surgically with adjunctive medical support.
• Rehabilitate.
• Evaluate the patient frequently.
• What is incision & drainage :
Incision and drainage (I&D) is the foremost surgical method in treating space infection.Incisions are used to gain surgical access to deeper tissues with minimal damage to the surrounding vital structures.
A ‘pen grasp’ is used to hold the scalpel in one hand, while the other hand is used to firmly hold and stabilize the skin or mucosa.
Indications for I&D:
• Space infections that has localized pus collection with a clinically evident point of fluctuance. Example: buccal space infection with point of fluctuance on face.• Space infections that has pus collection with no clinical sign of fluctuance but requires immediate drainage to prevent progression. Example: masseteric space infection—only clinical sign is trismus.
• Nonsuppurative space infection such as Ludwig’s angina, where I&D serves as a method of decompression of the tissue planes, but could be lifesaving.
Principles that’s should be used when possible with incision and drainage:
1. Incise in healthy skin and mucosa when possible, if incision placed at the site of maximum fluctuance where the tissues are necrotic or beginning to perforate can result in a puckered, unesthetic scar.
2. Place the incision in an esthetically acceptable area, such as under the shadow of the jaw or with a natural skin crease (langer’s lines).
3. When possible, place the incision in a dependent position to encourage drainage by gravity.
4. Dissect bluntly, with a closed surgical clamp or finger, through deeper tissues and explore all portions of the abscess cavity thoroughly so that compartmentalized areas of pus are disrupted and excavated.
5. Extend the dissection to the roots of teeth responsible for the infection.
6. Place a drain and stabilize it with sutures.
7. Consider the use of through-and-through drains in bilateral, submandibular space infections.8. Do not leave drains in place for an overly extended period; remove them when drainage becomes minimal.
The presence of the drain itself can produce some exudate
and can be a portal for secondary bacterial invaders.6
9. Clean wound margins daily under sterile conditions to remove debris.
• Surgical steps of I&D.
• Local anesthesia / general anesthesia• Aspiration the pus for C&S.
• Stab incision: made over a point of maximum fluctuation in the most dependent area along the skin creases, through skin and subcutaneous tissue.
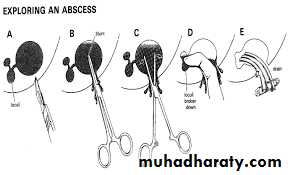
• If pus is not encountered, further deepening of surgical site is achieved with sinus forceps (to avoid damage to vital structures).
• Closed forceps are pushed through the tough deep fascia and advanced towards the pus collection. ( Hillton Method).
• Abscess cavity is entered and forceps opened in a direction parallel to vital structures.Pus flows along sides of the beaks.
• Explore the entire cavity for additional loculi.
• Placement of drain: A soft corrugated rubber drain is inserted into the depth of the abscess cavity; and external part is secured to the wound margin with the help of suture
• Drain left for at least 24 hours or until the regression of signs and symptoms.
• Dressing: dressing is applied over the site of incision taken extraorally without pressure.
Ludwig's angina
Ludwig’s angina is a form of a firm, acute, toxic and severe diffuse cellulitis that spreads rapidly, bilaterally affecting the submandibular, sublingual and submental spaces.The condition has established for its unique identity among general medical personnel with three ‘F’
It was to be feared
It rarely become fluctuant
And it was often fatal
Etiology
Ludwig’s angina is a disease primarily of dental origin although various causes can also be related.• Odontogenic infection: It is generally of dental origin, following infection of the second and third mandibular molars (70%–80%). Acute periodontal abscess, Acute pericoronal abscess.
• Traumatic injuries of orofacial region.
• Submandibular and sublingual sialadenitis
• Secondary infections of oral malignancies
• Pharyngeal infection or tonsillitis.
• Iatrogenic: Use of contaminated needle for giving local anesthesia
• Cervical lymphoid tissues
• Miscellaneous: Foreign bodies such as fish bone
Clinical features/ General examination
Patient looks toxic, very ill, dehydrated,
chills and malaise.
Marked pyrexia
Difficulty in swallowing (dysphagia)
Impaired speech and hoarseness of voice
Extraoral examination
• Bilateral suprahyoid swelling is observed, with a hard, cardboard-like consistency.• Swelling is firm/hard brawny involving bilateral submandibular and submental regions which soon extend down the anterior part of the neck of the clavicles, swelling present with ill-defined borders. It is nonpitting, not-fluctuating and tender on palpation.
• Airway obstruction and cyanosis may occur due to progressive hypoxia
Shallow breathing, trismus, Fatal death may occur in untreated case of Ludwig's angina within 10– 24 h due to asphyxia
Difficulty in swallowing and breathing, chills, fever, drooling of saliva, restricted tongue movements and inability to close the mouth are the most presenting clinical features of the illness.
Intraoral examination:
• Swelling develops rapidly and involves sublingual spaces causing elevation of tongue against the palate.• Increased salivation, difficulty in swallowing with hot potato speech is noted.
• Drooling of saliva due to reduced control of muscles and jaw posture.
• Backward spread of infection leading to oedema of the glottis, which leads to obstruction of airway.
Potential complications
septicaemia, upper respiratory airway obstruction and provoke oedema of the epiglottis. can also spread to the submassetric, pterygopalatine spaces, parapharyngeal and paratonsillar spaces and from there it can proceed to the mediastinum, producing thoracic empyema.
Rarely the infection may spread below and reach close to carotid sheath, pterygopalatine fossa, leading to cavernous sinus thrombosis with subsequent meningitis.
Diagnosis
Diagnosis is made on the basis of clinical findings, although CT studies can help to determine the extent of the infection, especially when there is abscess formation.Treatment
Combination of intensive antibiotic therapy and early intubation to control the airway coupled with surgical drainage of fascial spaces when pus is presenting.Immediate intravenous infusion of 500mg of metronidazole and 500mg of amoxicillin usually brings rapid improvement. The regime repeated 8-hourly
If patient allergy to penicillin use erythromycin lactobionate 600 mg given slowly intravenously every 8 hr.
Cavernous Sinus Thrombosis
One of the most severe complications of a maxillary odontogenic infection.The cavernous sinuses are positioned on either side of the sella turcica and sphenoid bone body.
They are intracranial compartments that serve as bilateral venous drainage channels for the middle cranial fossa.
Hematogenous spread of infection from the jaw to the cavernous sinus may occur anteriorly via the inferior or superior ophthalmic vein or posteriorly via emissary veins from the pterygoid plexus
The contents of the cavernous sinus include cranial nerves
• CN II Optic n• CN III Oculomotor n.
• CN IV Trochlear n.
• CN VI Abducent n
• the first and second divisions of cranial nerve V (ophthalmic n. & maxillary n.)
• the internal carotid artery.
On clinical exam, any of the structures that receive innervation from these nerves may be affected
Signs and symptoms
papilledema, exophthalmos, proptosis, diplopia, ophthalmoplegia, eyelid edema, chemosis, upper eyelid ptosis,sympathetic plexus damage on the internal carotid artery), and vision loss (optic nerve and central retinal artery and vein damage).
Pulsating exophthalmos where carotid pulse is transmitted through the retro bulbar oedema
Untreated infection will spread to opposite side giving rise to bilateral signs.
Treatment :
Cavernous sinus thrombosis will require energetic antibiotic therapy and heparinization to prevent extension of thrombosisNeurosurgical consultation is essential as a matter of great urgency.