
1
THI-QAR MEDICAL COLLEGE
SURGICAL DEPARTMENT.
GERNERAL SURGERY
DR.ALAA JAMEL
Breast
Objective
1-to know the anatomy ,blood supply, lymphatic drainage of the breast
2-to know the congenital anomaly of the breast.
3-to know what means ANDI and what that represent.
4-who you mange patient with breast disease and what means triple
assessments.
5-to know the benign condition of the breast , ..
5-to know the acute and chronic inflammatory condition of the breast.
6-to know predisposing factor of breast cancer.
7-who we can do early diagnose breast cancer
8-to know the types of breast cancer.
9-To know who we can stage the disease.
10-to know the main line of treatment breast cancer
11-to know what means gynicomastia and who we can reach to the cause
and who we treat
anatomy.
The protuberant part of breast is overlying the second to the sixth ribs and extending
from the lateral border of the sternum to the mid axillary line. in females with a
large breast may extend from the clavicle above to the 7 or 8 rib below.
Axillary tail;

2
Is of considerable surgical importance because in which a high percentage of breast
cancer occur and contain a lot of lymph nodes. in some normal subject it's palpable
and in a few can be see premenstrual or during lactation. A well develop axillary tail
is some time mistaken for amass of enlarge l.n. or lipoma.
Functional Anatomy;
The breast is composed of 15 to 20 lobes which are each composed of several
lobules.
The lobule is the basic structural unit of the mammary gland ,the no. and the size of
the lobules vary In enormously. they are most numerous in a young women ( 10 to
100 lobules) empty via ductules into lactiferous duct of which there are (15 to 20 )
THE LIGAMENT OF COOPER;
Are hollow conical projections of fibrous tissue filled with breast tissue. The apices of
the cones being attach firmly to the superficial fascia and thereby to the skin over
lying the breast. These ligament accounts for the dimpling of the skin over lying
carcinoma.
AREOLA;
It contains involuntary muscle .its epithelium contain numerous sweet gland and
sebaceous gland.
Sebaceous gland enlarge during pregnancy and serve to lubricate the nipple during
lactation (Montgomery's tubercles)
THE NIPPLE;
Its cover by thick skin .near its apex open lactiferous duct. It contains smooth muscle
fiber arranged concentrically and longitudinally thus it's an erectile structure which
points outwards. It not contain sweet glands.
LYMPHATIC DREANAGE;
Lateral part of breast Lymph drain 85% to the axillary l.n and 15% to the internal
mammary l.n.
Medial part goes to parasternum and mediastinum l.n
Some lymphatic vessels to the posterior intercostals nodes
Some lymphatic vessels cross the sternum to the contralateral breast

3
Across the lymphatic system of body transmit to the peritoneum , live abdomen
Axillary l.n arrange in the fallowing group
1-lateral group along the axillary vein
2-anterior group along lat.thoracic vessels
3-posterior group along sub scapular vessels
4- central embedded in the fat of center of axilla
5- interpectoral, few l.n lying between pect. Minor and pect.major muscle
6-apical group which lie above the level of pectorals minor muscle tendon
And receved lymph from all the other group and its in continuity with
supraclavicular node then to the subclavain lymph trunk
Internal mammary l.nlie along the internal mammary vessel.
DESCRIBE THE 3 LEVELS OF LYMPH NODES AND INCLUDES IN EACH.
Level 1 lateral to the pectorals minor muscle .
Level 2 behind pect .minor Muscle .
Level 3 medial to the pect. Minor.
THE TISSUE LAYERS OF THE BREAST FROM THE MOST SUPERFAICIAL TO
THE DEEPEST.
Epidermis,dermis, super facial layer of super facial fascia,coopers ligaments
,glandular tissue.deep layer of super facial fascia, retro mammary space , deep
investing fascia ,pectorals major muscle.
DIAGNOSIS OF BREAST DISEASE;
Depend on triple assessment which include
1-history and clinical examination
2-radiological imaging
a-mammography
b-U/S both for diagnosis and to guide biopsy

4
c-magnetic resonance imaging( MRI) which not affected by breast tissue density as
the mammography.
3-biopsy usually U/Sguided; FNAC and core biopsy
a
-
F.N.ACusing a 21 G or 23 G needle and 10 ml syringe with multiple passes through
the lump without releasing the negative pressure in thesyringe. Disadvantage is
cannot distinguish invasive cancer from carcinoma in situ
CORE BIOPSY
1-.givea definitive preoperative diagnosis
2-difrentiate duct carcinoma in situ and invasive carcinoma
3- allow the tumor to be stained for receptor status which important before
commencing neoadjuvant therapy
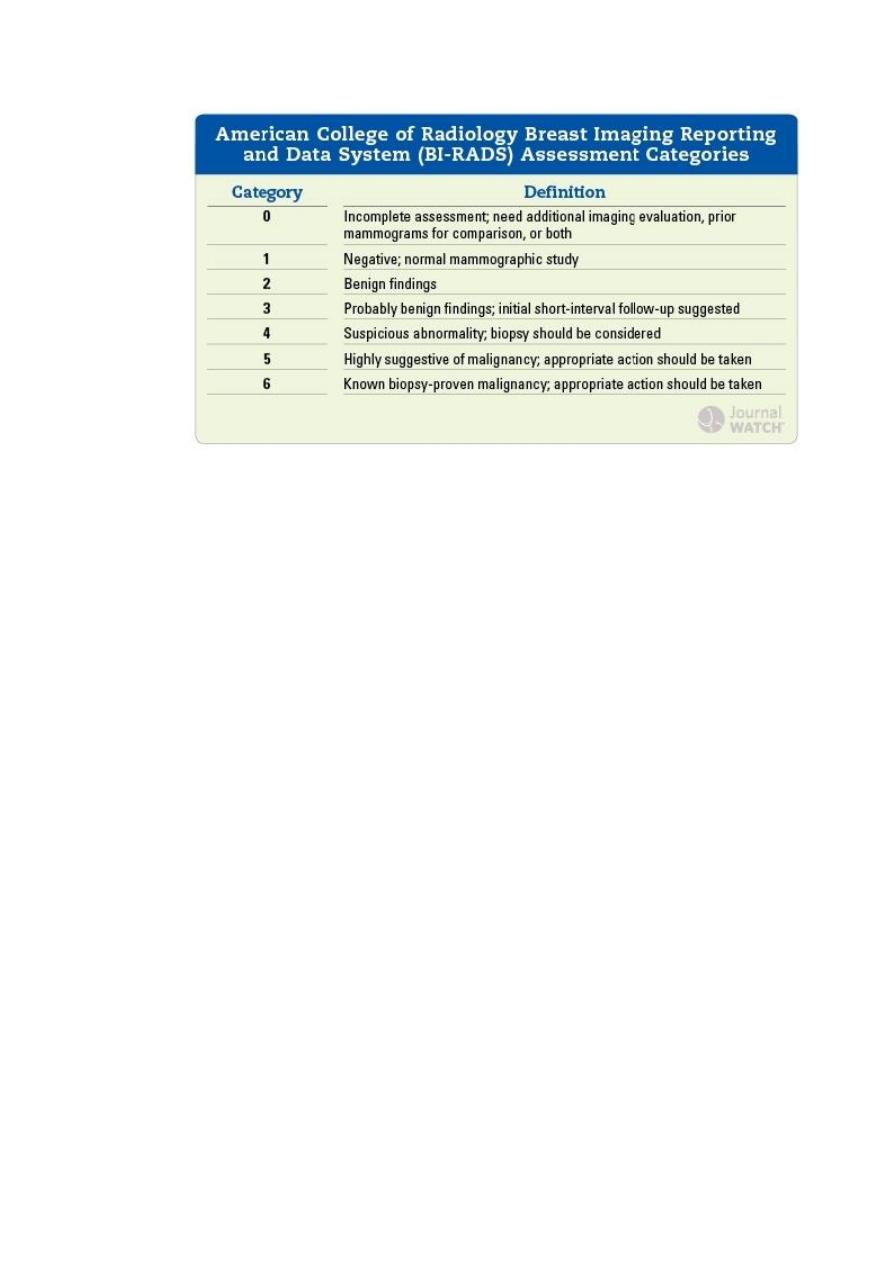
MAMOGRPHY
Its soft tissue radiographs are taken by placing the breast in direct contact with
ultrasensitive film and exposing it to low voltage and high amperage x ray .the dose
of radiation is approximately 0.1 cGY, soit's very safe investigation. The sensitivity of
the test increase with the age as the density of breast decrease . it take in 2 veiw
craniocaudal and medilateral oblique.
Breast cancer tend to be more radio dense than the normal tissue
Criteria that increase chance of cancer in patient without palpable mass appear in
the mammographyare;
1-microcalcification2-irregular mass with calcification 3- structural distortion with
2
more than 5 microcalcification lcm
-
asymmetry with calcification 5
-
calcification 4
6-indistict margin
5
Abnormalities of the nipple;
**May be absent usually associated with amazia(congenital absence of
breast).Supernumerary nipple not uncommonly occurs along aline extending from the
anterior fold of axilla to the fold of the groin.
**Nipple retraction
May be at puberty or later in life
At puberty also known simple nipple inversion is of unknown etiology, 25% bilateral,
it may cause problem during lactation and infection may occur
Treatment
Usually unnecessary and may resolve spontaneously during pregnancy and lactation
Simple cosmetic surgery may resolve the problem.
Recent retraction may consider of pathological significant, slit like retraction of the
nipple may be due to duct ectezia or chronic periductal mastitis ,but circumferential
retraction with or without under ling lump may be due to carcinoma.
**CRACKED NIPPLE
This may occur during lactation and may cause acute infective mastitis .so when
nipple become cracked during lactation it should be rested for 24-48 hours and the
breast should be emptied with a breast pump ,feeding should be resumed as soon as
possible.
PAPILLOMA OF THE NIPPLE
Treatment with excision
ECZEMA OF NIPPLE
Rare condition and often bilateral and usually associated with eczema elsewhere on
the body

6
PAGETS DISEASE
Must be distinguish from eczema .it represent an underlying malignant disease
DISCHARGE OF THE NIPPLE
It occur from one or more lactiferous ducts ,management depend on;
1- presence of a lump 2- presence of blood in the discharge 3- discharge from single
duct or more.
•
BLOOD STAINED
a-duct papilloma when blood arises from asingle duct
b-Intra duct carcinoma--
b
-
C-Invasive carcinoma ( rare)
•
Clear. intra duct papilloma or clear serous as in physiological in parouse women/
•
Multi colored. (Often multi duct); duct ectasia (discharge commonly yellow, brown,
green).
•
Milky; galactorria may follow lactation but also can be drug induced or
manifestation of hyperprolactenimea( or occasionally hypothyroidism)
•
purulent ;breast abscess
TREATMENT; by triple assessment to exclude carcinoma by occult blood test and
cytology And the majority of cases of nipple discharge are benign and this.
symptoms is rarely presenting feature of breast cancer even when blood –stain clear
Single duct or blood stain discharge required further investigation
If a lump is present it should be manage by triple assessment
In the absent of a lump the management of discharge is the fallow
Multi colore dmulti duct discharge. If clinical examination and mammography are
normal, a diagnosis is duct ectesia is likely and no further treatment is required.
Clear single –duct discharge
If mammography is normal the diagnosis is likely to be an intraduct papilloma and
excision of infected duct(microductomy ) is indicated
Bloody nipple discharge
The present of blood in the discharge should be confirmed by cytology .if blood is
present mammogram( for women over 35 year of age) is performed with biopsy of
any abnormal tissue.
If mammography is normal ,amicroductomy is performed if a single duct can be
identified ,a total duct clearance(cone excision of the major ducts) is performed if a
single duct cannot be clearly identified.
SYMPTOMS OF BREAST DISEASE
7
There are 5 common symptoms of breast disease that warrant urgent attention.
1-Anew discrete lump
2- Nipple discharge _blood stain or persistence nipple discharge
3- Nipple retraction or distortion of resent onset
4-altered breast contour or dimpling
5-Suspected beget disease-
Other common symptoms that required further investigation include persistence a
symmetrical nodularity, breast pain (mastalgia).Family history of breast cancer
LUMP IN THE BREAST
95% of breast lump will be one of the four following
1-carcenoma of the breast
2- Cyst
3-fibroadenoma
4- fibroadenosis
In addition the fallowing less common causes need to be consider
1-Trauma (fat necrosis)
2-Other cyst
a-Galactocel
b-Abscess
c-Cyst adenoma
d-Retention cyst of Montgomery gland
PAIN IN THE BREAST(MASTALGIA)
It can be separated to cyclical and non-cyclical mastalgia.
Cyclical type most common and due to alteration of normal cyclical pattern that occur during
reproductive years
So it may be worse premenstrual and relieve after menstruation
Non-cyclical mastalgia causes

8
1-breast abscess
2-carcenoma of the breast
3-Tietze's syndrome (chondritis of costal cartilage, is of unknown etiology
4-chest wall lesion….herpes zoster
Treatment of mastalgia
Cyclical mastalgia may become significant clinical problem if the pain and
tenderness interfere with women's life .beginning of treatment is reassurance that
these symptoms are not associated with cancer.
Must use an appropriate fitting and supportive bra should be worn through the day
and soft bra(as sport bra) at the night +avoiding caffeine may be help
If these measure not help can be use oil of evening primrose in adequate dose over 3
months will help more than one half of women
For those who have intractable pain, antigonodotrphin hormone such as danazol or
prolactin inhibitor as promocriptine .
For non cyclicalmastalgia is important to exclude extra mammary causes
.
DUCT ECTESIA
This is a dilatation of the breast ducts associated with peri ductal inflammation, the
disease more common in smoking women.
This condition may associated with periductal mastitis or even abscess or fistula
formation and in some cases indurate mass may appear beneath the areola which
mimic carcinoma . Fibrosis may develop which may cause slit-like nipple retraction.
TREATMENT
Must exclude malignancy by triple assessments if the condition associated with mass
or recent nipple retraction.
Start with antibiotic (augmantine or fluxacillin and flagyl).and if not response
surgical major duct excision may need
.
BREAST CYST;
These occur in last decade of reproductive life due to a non-integrate involution of
stromal and epithelium .they are often multiple and may be bilateral and it may
mimic breast cancer
Diagnosis by uls. and aspiration .
Because needle biopsy of breast masses may produce artifacts that make
mammography assessment more difficult, many surgeons prefer to image breast
masses before performing either fine needle aspiration or core needle biopsy. The
volume of a typical cyst is 5 to 10 mL, but it may be 75 mL or more. If the fluid that is

9
aspirated is not bloodstained, then the cyst is aspirated to dryness, the needle is
removed, After aspiration, the breast is carefully palpated to exclude a residual mass.
indeed the majority of cysts are now aspirated under ultrasound guidance. When
cystic fluid is bloodstained, fluid can be sent for cytologic examination.
pneumocystogram can be obtained by injecting air into the cyst and then obtaining a
repeat mammogram. When this technique is used, the wall of the cyst cavity can be
more carefully assessed for any irregularities
Treatment
Solitary cyst and small cyst can be aspirated and if it resolve completely and no
blood stain fluid no further treatment need. About 30% recur and need another
aspiration
If there's residual mass or blood stained fluid a core biopsy or excisional biopsy for
histological examination
Periductal Mastitis.
Painful and tender masses behind the nipple-areola complex are aspirated with a 21-
gauge needle attached to a 10-mL syringe. Any fluid obtained is submitted for culture
for the detection of anaerobic organisms. In the absence of pus, women are started on
a combination of metronidazole and dicloxacillin while awaiting the results of
culture. Antibiotics are then continued based on sensitivity tests. Many cases respond
satisfactorily to antibiotics alone, but when considerable purulent material is present,
repeated ultrasound guided aspiration is performed and ultimately in a proportion of
cases surgical treatment is required. Unlike puerperal abscesses, a subareolar abscess
is usually unilocular and often is associated with a single duct system. which come to
surgery, the surgeon may either undertake simple drainage with a view toward formal
surgery, should the problem recur, or proceed with definitive surgery. In a woman of
childbearing age, simple drainage is preferred, but if there is an anaerobic infection,
recurrent infection frequently develops. Recurrent abscess with fistula is a difficult
problem. Treatment of periductal fistula was initially recommended to be opening up
of the fistulous track and allowing it to granulate. This approach may still be used
especially if the fistula is recurrent after previous attempts at fistulectomy. However,
nowadays the preferred initial surgical treatment is by fistulectomy and primary
closure with antibiotic coverage.41 Excision of all the major ducts is an alternative
option.
GALACTOCEL
Its rare condition, usually present with a solitary sub areolar cyst and always dates
from lactation it contains milk
Fibroadenomas.

10
Most fibroadenomas are self-limiting and many go undiagnosed, so a more
conservative approach is reasonable . Careful ultrasound examination with core-
needle biopsy will provide for an accurate diagnosis. Ultrasonography may reveal
specific features that are pathognomonic for fibroadenoma and in a young woman
(e.g., under 25 years) where the risk of breast cancer is already very low a core-
needle biopsy may not be necessary. Cryoablation and ultrasound-guided vacuum
assisted biopsy are approved treatments for fibroadenomas of the breast, especially
lesions <3 cm. Larger lesions are often still best removed by excisionTherefore,
women should be counseled that the options for treatment include surgical removal,
cryoablation, vacuum assisted biopsy, or observation.
PHYLLODES TUMOUR
Phyllodes means leaf-like
This tumour have many of clinical features. Its a true neoplasm with wide range of
characteristics from benign to malignant .they arise from stromal cell of the breast
and are classified as low, intermediate or high grade depending on their
microscopically feature .they are rarely metastasize but can recur locally if in
adequate excised.
C.F
Usually present as affirm discrete lump, large ,some time massive. Occasionally
ulceration of overlying skin occurs because of pressure necrosis .it mobile on chest
wall .it may be metastasis via the blood stream. despite the name of
cystosarcomaphyllodes they are rarely cystic and very rarely develop feature of
sarcomotoustumor.
TREATMENT
All phyllodtumour should treated by wide local excision to prevent recurrence .if
large tumour mastectomy with immediate reconstruction.
Sclerosing Disorders.
The clinical significance of sclerosing adenosis lies in its imitation of cancer. On
physical examination, it may be confused with cancer, by mammography, and at
gross pathologic examination. Excisional biopsy and histologic examination are
frequently necessary to exclude the diagnosis of cancer. The diagnostic work-up for
radial scars and complexsclerosing lesions frequently involves stereotactic biopsy. It
usually is not possible to differentiate these lesions with certainty from cancer by
mammographic features, so a larger tissue biopsy is recommended either by way of
vacuum assisted biopsy or an open surgical excisional biopsy.
GYNAECOMASTIA;

11
Gynecomastia refers to an enlarged breast in the male. Physiologic gynecomastia
usually occurs during three phases of life: the neonatal period, adolescence, and
senescence. Common to each of these phases is an excess of circulating estrogens in
relation to circulating testosterone. Neonatal gynecomastia is caused by the action of
placental estrogens on neonatal breast tissues, whereas in adolescence, there is an
excess of estradiol relative to testosterone, and with senescence, the circulating
testosterone level falls, which results in relative hyperestrinism. In gynecomastia, the
ductal structures of the male breast enlarge, elongate, and branch with a concomitant
increase in epithelium. During puberty, the condition often is unilateral and typically
occurs between ages 12 and 15 years. In contrast, senescent gynecomastia is usually
bilateral. In the nonobese male, breast tissue measuring at least 2 cm in diameter must
be present before a diagnosis of gynecomastia may be made. Mammography and
ultrasonography are used to differentiate breast tissues.
Causes
1-drugs as digoxin,cimetidin
2-liver cirrhosis
3-renal failure
4-hypogonodism
5-supra renal tumour
6-testicular tumour
7-Idiopathic
TRUMATIC FAT NECROSIS
It may be acute or chronic, associated with history of trauma ,or even in direct due to
contraction of pectoralis major and is common result of seat beat injury after sudden
deceleration injury or surgical truma.its important because it mimic to breast
carcinoma.
C.F
it commonly presented with firm irregular ,paainless lump. And there may be history
of trauma, its often associated with skin thickening or retraction, the lump usually
decrease in size with the time
TREATMENT
Mammography and ulscannot distinguish it from carcinoma so best treatment by core
biopsy and the palpable mass should be removed.
ACUTE INFLAMATION OF THE BREAST

12
Bacterial Infection
Staphylococcus aureus and Streptococcus species are the organisms most frequently
recovered from nipple discharge from an infected breast.17 Typically breast
abscesses are seen in staphylococcal infections and present with point tenderness,
erythema, and hyperthermia. When these abscesses are related to lactation they
usually occur within the first few weeks of breastfeeding. If there is progression of a
staphylococcal infection, this may result in subcutaneous, subareolar, interlobular
(periductal), and retromammary abscesses (unicentric or multicentric). Previously
almost all breast abscesses were treated by operative incision and drainage but now
the initial approach is antibiotics and repeated aspiration of the abscess, usually
ultrasound guided aspiration. Operative drainage is now reserved for those cases
which don’t resolve with repeated aspiration and antibiotic therapy or if there is some
other indication for incision and drainage (e.g., thinning or necrosis of the overlying
skin). Preoperative ultrasonography is effective in delineating the required extent of
the drainage procedure. While staphylococcal infections tend to be more localized
and may be situated deep in the breast tissues, streptococcal infections usually present
with diffuse superficial involvement. They are treated with local wound care,
including application of warm compresses, and the administration of
IV antibiotics (penicillins or cephalosporins). Breast infections may be chronic,
possibly with recurrent abscess formation. In this situation, cultures are performed to
identify acid-fast bacilli, anaerobic and aerobic bacteria, and fungi. Biopsy of the
abscess cavity wall should be considered at the time of incision and drainage to rule
out underlying breast cancer in patients where antibiotics and drainage have been
ineffective.
Zuska’s disease, also called recurrent periductal mastitis, is a condition of recurrent
retroareolar infections and abscesses. Smoking has been implicated as a risk factor
for this condition. This syndrome is managed symptomatically by antibiotics coupled
with incision and drainage as necessary.
CHRONIC INFLAMATORY ABSCES
Its occur due to inadequate drainage or using antibiotic ..its difficult to diagnosed its
mimic ca. breast diagnosis by biopsy and histological examination.
MONDOR'S DISEASE
Its thrombophlebitis of superfascial veins of breast and anterior chest wall
The pathognomonic feature is athrombosed subcutaneous cord usually attached to
the skin
Diff.diagnosis
Lymphatic permeation from an occult carcinoma of the breast
Treatment need only rest and analgesia.

13
Aberrations of Normal Development and Involution
The basic principles underlying the aberrations of normal
development and involution (ANDI) classification of benign breast conditions are
the following: (a) benign breast disorders and diseases are related to the normal
processes of reproductive life and to involution; (b) there is a spectrum of breast
conditions that ranges from normal to disorder to disease; and (c) the ANDI
classification encompasses all aspects of the breast condition, including
pathogenesis and the degree of abnormality .30 The horizontal component of Table
17-2 defines ANDI along a spectrum from normal, to mild abnormality (disorder),
to severe abnormality (disease). The vertical component indicates the period during
which the condition develops
Table 17-2
ANDI classification of benign breast disorders Normal Disorder
Disease
Early reproductive years(age 15–25 y)
NORMAL DISORDER DISEASE
Lobular development Fibroadenoma Giant fibroadenoma
Stromal development Adolescent hypertrophy Gigantomastia
Nipple eversion Nipple inversion Subareolar abscess
Mammary duct fistula
Later reproductive years(age 25–40 y)
NORMAL DISORDER DISEASE
Cyclical changes of menstruation Cyclical mastalgia Incapacitating
mastalgia
Nodularity
Epithelial hyperplasia of pregnancy Bloody nipple discharge
Involution (age 35–55 y)
NORMAL DISORDER
Lobular involution Macrocysts —
Sclerosing lesions
Duct involution
Dilatation Duct ectasia Periductal mastitis
Sclerosis Nipple retraction —

14
BREAST TUMOUR
CLASSIFICATION
1-BENIGN
a-intraductal papilloma
b-phyllodetumour
2-MALIGNANT
a-primary
Intraductalcarcinoma
Lobular carcinoma 15% often multifocal and bilateral
Invasive carcinoma
Paget's disease of the nipple
Sarcoma
b-secondary
Direct invasion from tumour in the chest wall
Metastatic deposit from melanoma
CARCINOMA of breast
It’s the most common cause of death in the middle aged women in the world
One in nine women will develop breast cancer during their lifetime.
Any age may be affected but is rare below the age of 30 years.
One in 10 breast lump will prove to be malignant.
15
AETIOLOGY
•
AGE it increase with age
•
Genetic factor
a-family history
b-gene carriage……BRCA1 and BRCA2 these are autosomal dominant genes
•
Hormonal factors
Mostly due to exposure to
estrogen
a-gender women are 100 time more common than male b-
menarche and menopause
early menarche and late menopause ,associated with high risk
c-parity ..nulliparous women higher risk from multiparous.breast feeding decrease the
chance
d-hormone replacement therapy ..may slightly increase the risk
DIET
A high intake of alcohol is associated with an increase risk of developing breast cancer.
•
-Benign breast disease
A number of benign breast disease increase risk of malignancy as present of duct
hyperplasia increase risk fivefold.
•
-Radiation exposure
Exposure to ionizing radiation in adolescence or early child hood can cause marked
increase the risk
.
PATHOLOGY;
Breast cancer may arise from the epithelium of the duct system any where from
the nipple to the terminal duct unit which is in the breast lobule.
Carcinoma which arise in the TDLU(terminal duct lobular unit)but which have
not penetrated through the basement membrane are known as carcinoma in situ .which
are 2 type
1-duct carcinoma in situ which be classified to low, intermediate, or high grade
2-lobular carcinoma in situ
classification of ca. breast are
a-carcinoma in situ b- invasive carcinoma
classification;
1-duct carcinoma 2- lobular carcinoma
3- tubular 4- modulary rare

16
5- papillary 6- paget disease rare
7- inflammatory carcinoma rare
Duct cis;
Its not palpable disease , diagnose by localizing needle , treated by lumpectomy and if
large with radiotherapy.
Lobular cis;
Its occur only in females because it arise from the lobule . its multiscentric and even
multi focal, most of patients devlope invasive duct carcinoma in feuture
Diagnosed by mammography which appear as microcalcification around the area but
not in the lumin.
Managements by 1-observatrion
2-chemoprevention by tamoifin
3- prophylactic bilateral mastectomy
SPREAD
LOCAL the tumour enlarge and involve other portion of breast. involvement skin, S.C
tissue lead to skin dimpling, retraction of the nipple and ulceration and invade pectoralis
muscle and the chest wall.
Lymphatic it occur primarily to the axillaryl.n and internal mammary l.n.then spread to
the supraclavicular , abdominal,midiastinal and then to the opposite axilla
Blood stream ; most commonly to the lung. Liver and bone vertebrae femur ribs
(osteolytic) and to the brain ovaries and supra renal gland
CLINICL FEATURE
Any portion of breast including the axillary tail may involved
But Most frequently affect upper lateral quadrant, Most of patient present as a hard
breast lump which may be associated with nipple retraction, change in breast contours
nipple discharge .dimpling of skin cutaneous odema
Lymphangiosarcoma
It’s a rare complication of lymphedema with an onset many years after original
treatment.it take form of multiple subcutaneous nodule in the upper limb and must
distinguish from recurrent carcinoma of the breast.the prognosis is poor.

17
PROGNOSTIC FACTORS
1-axillary l.n status
2-tumour grade
3-tumour size
4-N.P.I(Nottingham prognostic index)
Is calculated as N.P.I =O.2*diameter(cm)+grade+nodal status
Tumour score between 1-3
Other prognostic factors are presence of lympho vascular invasion, hormonal receptors
Brca1 brca2
17 13
Increase chance of IDC
Poorly differentiated well
Hormone receptors -ve +ve
May develop ovarian, colonic, prostetic ca . increase stomach cancer
INVESTIGATION
Diagnosis of breast cancer depend on triple assessment
Staging investigation
Depend on the size oftumour and the presence of other symptoms. The fallowing invest
.may be indicate to assess the extent of spread
1-F.B.C.
2-LIVER F.T.
3-CXR
4-ISOTOP BONE SCAN
5-LIVER ULS
18
STAGING;
Staging depend on many factors which are;
Tumour size, l.n metastasis, the tumour invasive or not, metastasis beyond the breast
tissue.
Stage 0; non invasive tumor carcinoma in situ means not metastasis beyond the duct or
lobules.
Stage 1; the tumor less than 2 cm and not metastasis beyond the breast
Stage 2; A; tumor less than 2 cm with epsilateral aillary l.n involve OR tumor size
between 2-5 cm but without involvement of l.n
B; tumor size between 2-5 cm with axillary l.n involve OR more than 5 cm
without l.n involvement
Stage 3; A; size less than 5 cm with l.n involvement which adherent together producing
clump. OR
More than 5 cm with l.n involvement but not as a clump
B; any size of tumor but spread to the skin, chest wall, or swelling of the breast
C; any size of tumor with spread to the l.n in area above or below clavicle or
chest wall or skin of breast.
Stage 4; when there is a distal metastasis beyond the breast tissue.
Use the T.N.M classification
T= tumour sizeT1,T2,T3,T4. Tis—no palpable tumour
T1-less than2 cm .t2 –2-5cm .t3 5-10cm .t4 more than 10 cm or any tumour invading
skin or chest wall
N=L.N involvementno—no nodal metastasis n1—mobile epsilateral axillary l.n --,N2 –
fixed epsilateral axillary l.n,N3—supraclavicular epsilaterall.n
M=metastasis M0 on distant metastasis,M1distant metastasis
TREATMENT
Two basic principles of treatment are
1- to reduce the chance of local recurrence
2-reduce the risk of metastasis spread

19
The treatment options for each woman depend on the1- size and location of the tumor in
her breast, 2-the results of lab tests (including hormone receptor tests),3- and the stage
(or extent) of the disease.4- To develop a treatment plan to fit each patient's needs, 5-
woman's age and menopausal status, 6-her general health,
7-and the size of her breasts
Methods of Treatment
Methods of treatment for breast cancer are local or systemic. Local treatments are used
to remove, destroy, or control the cancer cells in a specific area. Surgery and radiation
therapy are local treatments. Systemic treatments are used to destroy or control cancer
cells throughout the body. Chemotherapy and hormonal therapy are systemic treatments.
A patient may have just one form of treatment or a combination. Different forms of
treatment may be given at the same time or one after another.
Treatment of early breast cancer will usually involve surgery with or without
radiotherapy
Systemic therapy such as chemotherapy or hormonal therapy is added if there are
adverse prognostic factor such as l.n invasion
At the other end a locally advanced or metastatic disease is usually treated by systemic
therapy to palliate symptoms
Type of surgery
Simple MASTECTOMY ,BREAST SPARING SURGERY ,LUMPECTOMY(REMOVE
LUMP +SOME NORMAL TISSUE around it and somel.n of axilla
Simple Mastectomy (remove all breast +some of l.n) indicated to
A-large tumour in relation to breast size
B-center tumour beneath or involve nipple
C-multifocal tumour
D-local recurrence
E-patient preference.
modified radical mastectomy (patey)(remove whole breast+most of l.n+lining over the
chest muscle

20
Radical mastectomy (Halsted radical mastectomy)removebreast+chest muscle +all of the
l.n+andsom additional fat and skin.
For many years, this operation was considered the standard one for with breast cancer,
but it is very rarely used today and only in cases of advanced cancer in which the cancer
has spread to the chest muscles.
Post operative complication:
Infection, hematoma. recurrence. nerve injury in axillary surgery,failure to local
control.seroma.pain, restriction of arm movement.
surgical management of the axilla
Axillary l.n status is the most important prognostic indicator in the treatment of invasive
breast cancer ,so axillary surgery should performed on all patient with operable breast
cancer .there are 2 surgical option
SENTINEL L.N BIOPSY
Its first axilleyl.n draining the cancer field is identified, excised and examined for
metastasis
Patient with negative sentinel l.n require no further axillary surgery
1
-
1-axillary sampling
A minimal 4 node should be removed for histological analysis. If one of thesel.n involve
so further treatment is necessary by axillary clearance or radiotherapy
2-axillary clearance
Normally carried out to the level 2 which include node
lateral and deep to pectorals minor.
Which nerve may be injured during axillary surgery?
3 nerves which are
ADJUVANT SYSTEMIC THERAPY
A-hormonal therapy
Is used to keep cancer cells from getting the hormones they need to grow
Tamoxifen is the most widely used it reduce annual recurrence rate by 25%and 17%
reduced annual rat
e of death.
Its mostly affected on estrogen receptor + disease(ER)
Other hormonal agents is LHRH agonist which produce reversible ovarian
suppression

21
CHEMOTHERAPY
6 monthly cycle of cyclophosphamide ,methotrexade,and 5 fluorouracil
(CMF) will achieve 25% reduction in the risk of relapse over 10 to 15 year
period. its use to pre and pos menopausal poor prognosis women
Radiotherapy
Used high energy rays to kill cancer cellsand stop them from growing.use
either external radiation or implant radiation)treatment given 5 days
aweekfor5 to 6 week.
Radiation alone or with chemotherapy or hormonal therapy is some time used
befor surgery to destroy cancer cells and shrink the tumour.
BREAST RECONSTRUCTION
Its either immediate or delay type
The most common type of reconstruction is using a silicone gel implant under
pectorals major muscle
Typical reconstruction involve the use of myocutanous flap if latissimusdorsi
or rectus abdominis muscle augmented where necessary with a silicon
implant
Reconstruction for an individual depend on several factors which are
1-breast size
2-adiquancy of skin flap
3-whether radiotherapy is planned or has previously been used
1
-
abdominal size and previous abdominal operation
Paget's disease of the nipple
Its occurs in the middle aged and elderly women it represent as
UNILATERAL red, bleeding,eczematous lesion of the nipple
and areolar epithelium.its associated with an intraduct carcinoma of the
underlying breast of 50%of cases.Which may or may not form of palpable
mass
Diagnosis by biopsy microscopically it characterized by the
presence of large ,ovoid cells with abundant ,clear,pale staining cytoplasm in
the malpigian layer of the epidermis.
Treatment

22
Treatment will determined by any underlying
breast cancer detecting on clinical examination or radiological investigation .
Surgical management include mastectomy and axillary surgery for
lesion associated withinvasivecarcinoma .
Breast Cancer During Pregnancy
Breast cancer occurs in 1 of every 3000
pregnant women, and axillary lymph node metastases are present in up to 75%
of these women.304The average age of the pregnant woman with breast cancer
is 34 years. Fewer than 25% of the breast nodules developing during pregnancy
and lactation will be cancerous. Mammography is rarely indicated because of its
decreased sensitivity during pregnancy and lactation; however, the fetus can be
shielded if mammography is needed. radiation cannot be considered until the
fetus is delivered. A modified radical mastectomy can be performed during the
first and second trimesters of pregnancy, even though there is an increased risk
of spontaneous abortion after first-trimester anesthesia. During the third
trimester, lumpectomy with axillary node dissection can be considered if
adjuvant radiation therapy is deferred until after delivery. Lactation is
suppressed. Chemotherapy administered during the first trimester carries a risk
of spontaneous abortion and a 12% risk of birth defects. There is no evidence of
teratogenicity resulting from administration of chemotherapeutic agents in the
second and third trimesters. For this reason, many clinicians now consider the
optimal strategy to be delivery of chemotherapy in the second and third
trimesters as a neoadjuvant approach, which allows local therapy decisions to be
made after the delivery of the baby. Pregnant women with breast cancer often
present at a later stage of disease because breast tissue changes that occur in the
hormone-rich environment of pregnancy obscure early cancers. However,
pregnant women with breast cancer have a prognosis, stage by stage, that is
similar to that of nonpregnant women with breast cancer.
CARCENOMA OF THE MALE BREAST
This account for less than 1% of all cases of breast cancer .it affect old ege
group.
It present with firm, painless sub areolar lump
Treatment is by extended mastectomy with lymph node clearance.

23
Prognosis is worse than in women
Post operative radiotherapy reduce local recurrence but dose not affect over
all survive
Most tumour response to tamoxifen.for advance disseminated disease
chemotherapy can produce reasonable palliation.
Other tumours of the breast;
Lipoma ; a true lipoma is very rare
Sarcoma of the breast;
Its usually of the spindle- cell variety and account for 0.5% of malignant
tumour of the breast .it tend to occur in ypnger women between the ages of 30
and 40 years.
Treatment ; simple mastectomy fallowed by radiotherapy .
DR. ALAAJAME
