
Urinary Lithiasis

The 3rd most common disorder of urinary tract after
*UTI
* prostate disorders.
Without medical intervention stone recurrence rate
after surgery can be as high as 50% within 5yr
*Stone occurrence is relatively uncommon before
age 20 but peaks in incidence in the fourth to sixth
decades of life
*men are affected 2-3 times more frequently than
women

ETIOLOGHY

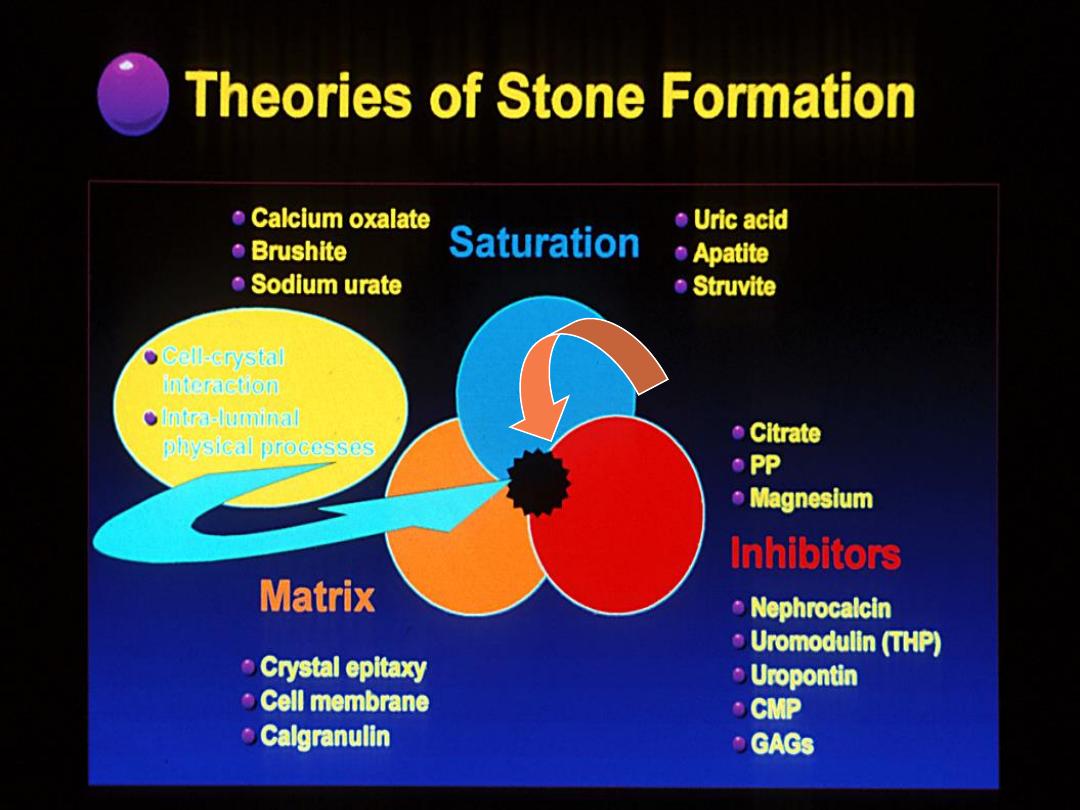
Nucleation and Crystal Growth, Aggregation, and
Retention
Crystal
are the main component of urinary stone
Matrix
or noncrystalline only 2-10% of the weight.
(mainly protein)
*Nuclei are the earliest crystal structure that will not
dissolve
Magnesium and citrate inhibit crystal aggregation.
Nephrocalcin, an acidic glycoprotein made in the
kidney, inhibits calcium oxalate nucleation, growth,
and aggregation
•
Infection?

1- Mass precipitation theory
suggests that the distal tubules or collecting ducts, or
both, become plugged with crystals, thereby
establishing an environment of stasis, & further
stone growth.
This explanation is unsatisfactory; tubules are conical
in shape and enlarge as they enter the papilla, thereby
reducing the possibility of ductal obstruction
.

2- Carr hypothesis
calculi form in obstructed lymphatics and then
rupture into adjacent fornices of a calyx.
Arguing against Carr’s theory are the grossly visible
early stone elements in areas remote from fornices
.
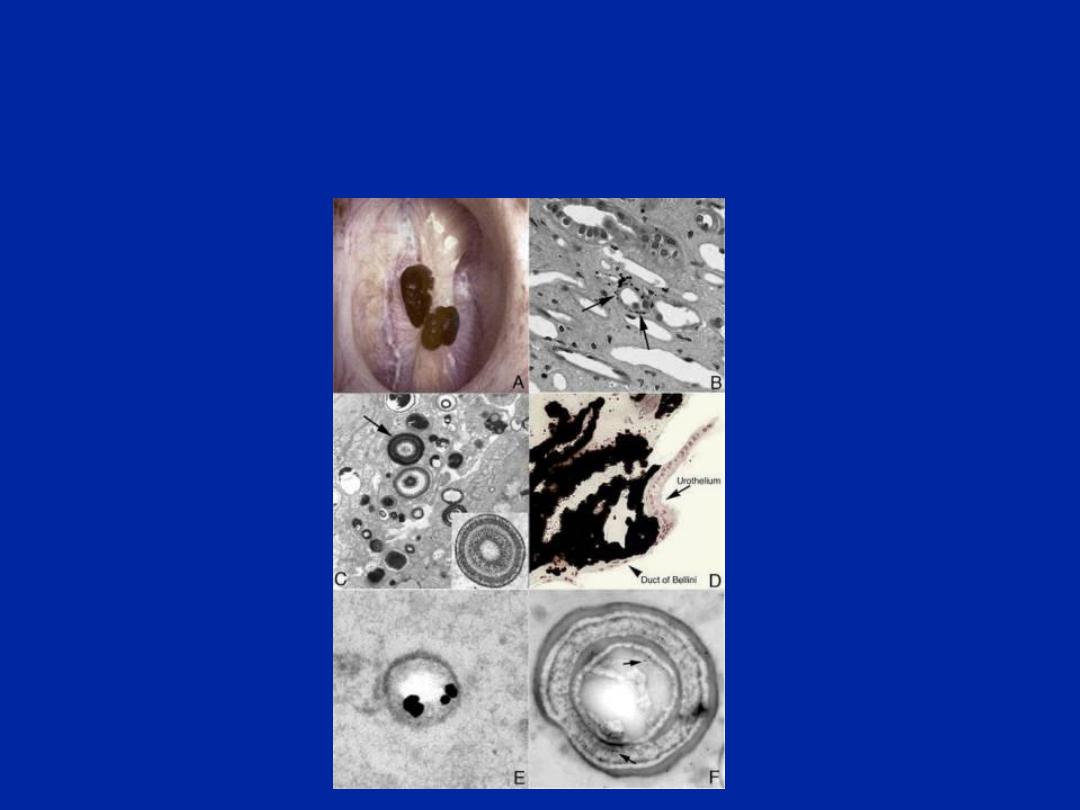
Randall
’s plaque
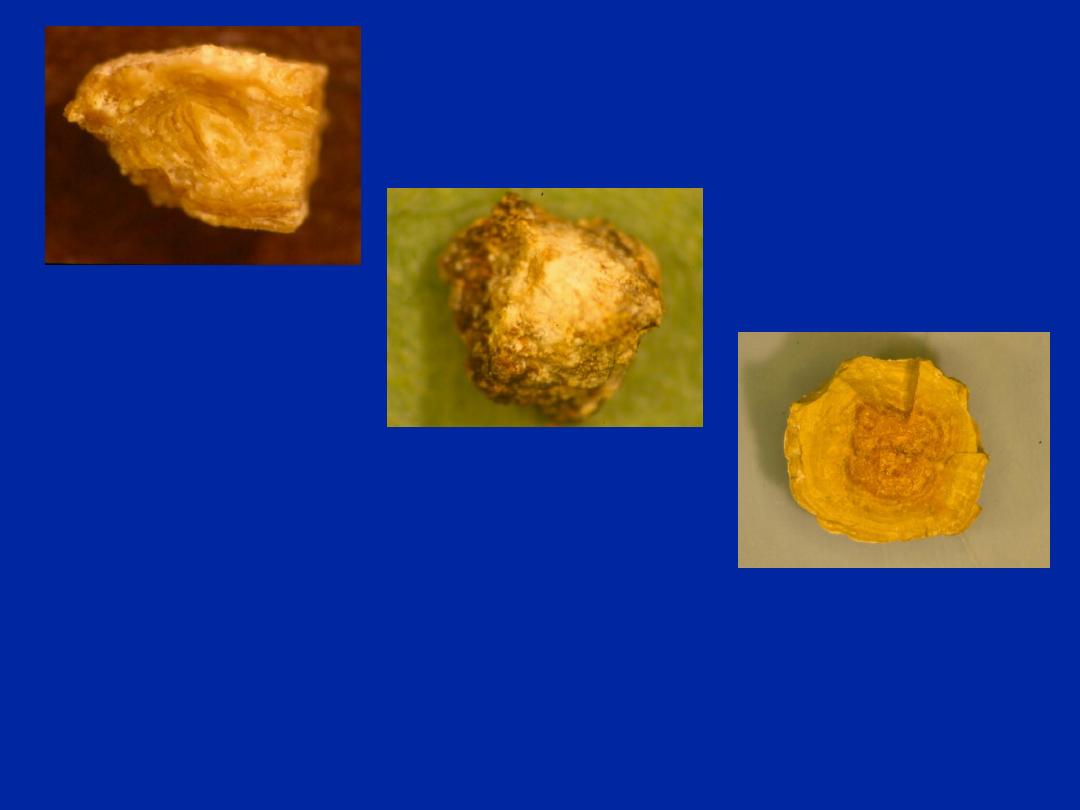
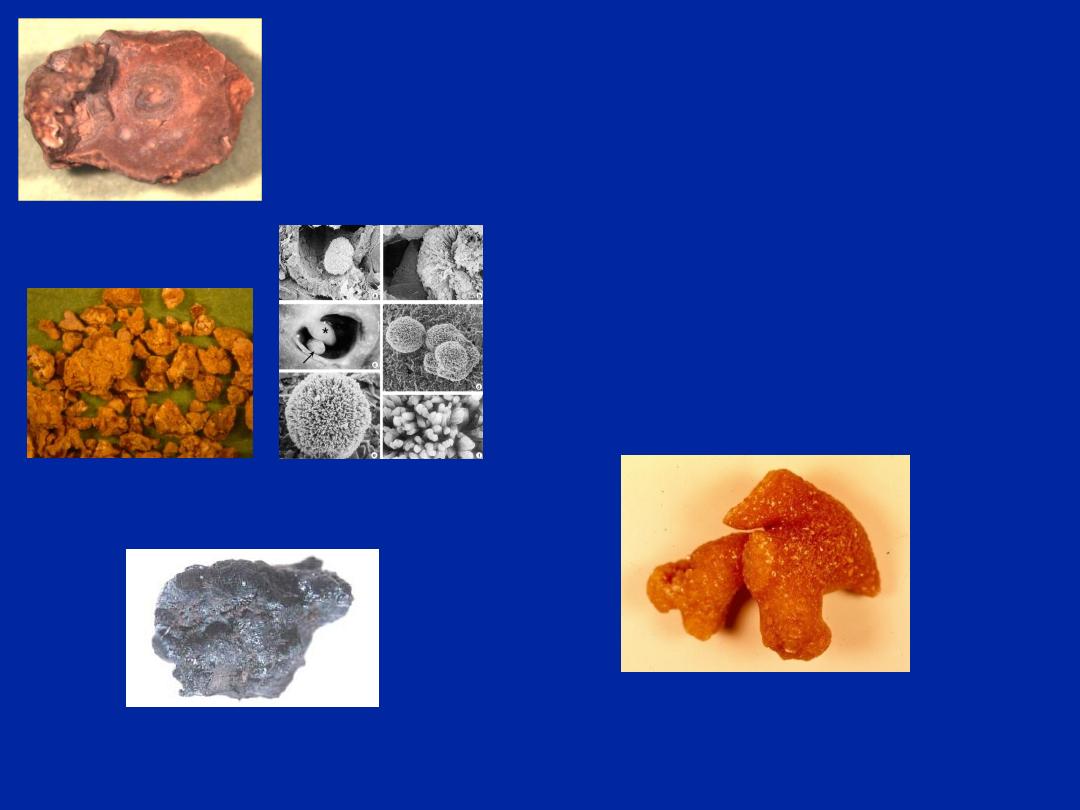
Calcium apatite
in BBM of thin
limbs of Henle
’s
loop
Laminated
microspherules
of white apatite
crystals and
black organic
matrix
Islands of
crystals in the
interstitium
Osteopontin
Alpha trypsin
inhibitor
3. Randell
’s plaque
(Randall,1940)

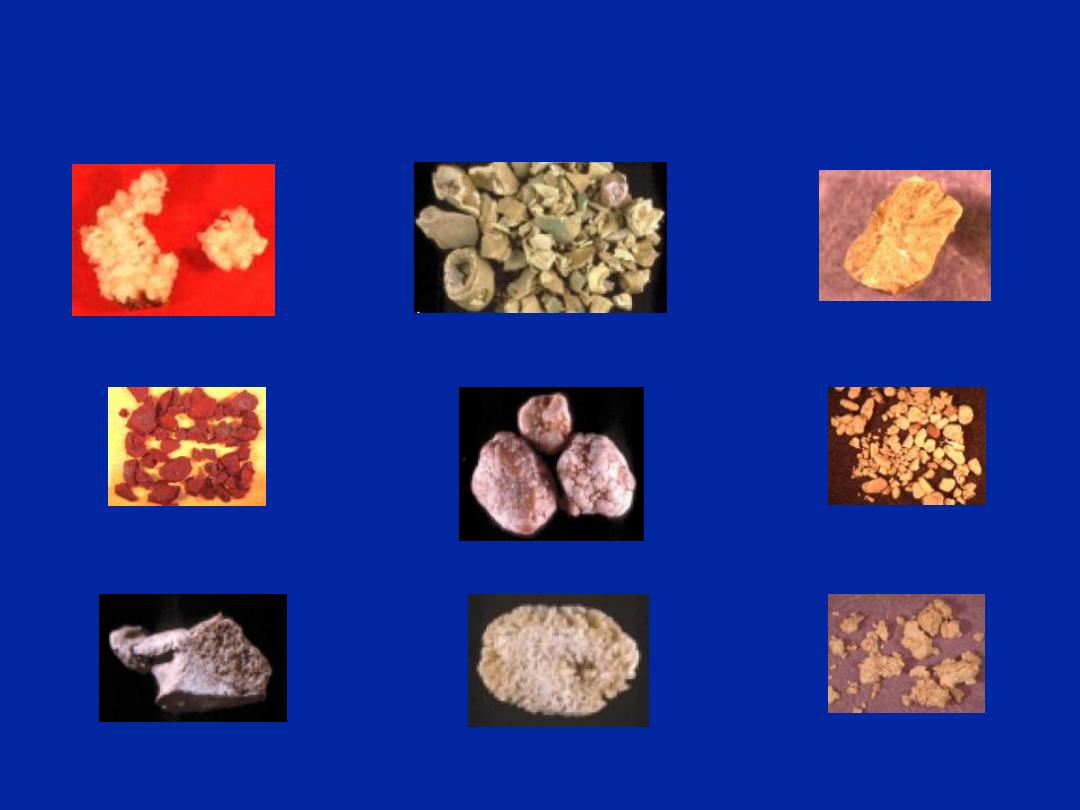
Types of calcium stone
1-absorptive hypercalciuric nephrolithiasis
Due to increase calcium absorption from small bowel
predominantly the jejunum resulting in hypercalciuria
(>4mg/kg) or (>150-200mg/24hr).
Its of 3types;
type1-dietary independent (15%)
*Cellulose phosphate- binding ca. in bowel prevent its
absorption.
*hydrochlorothiazides-reduce renal excretion
of ca.
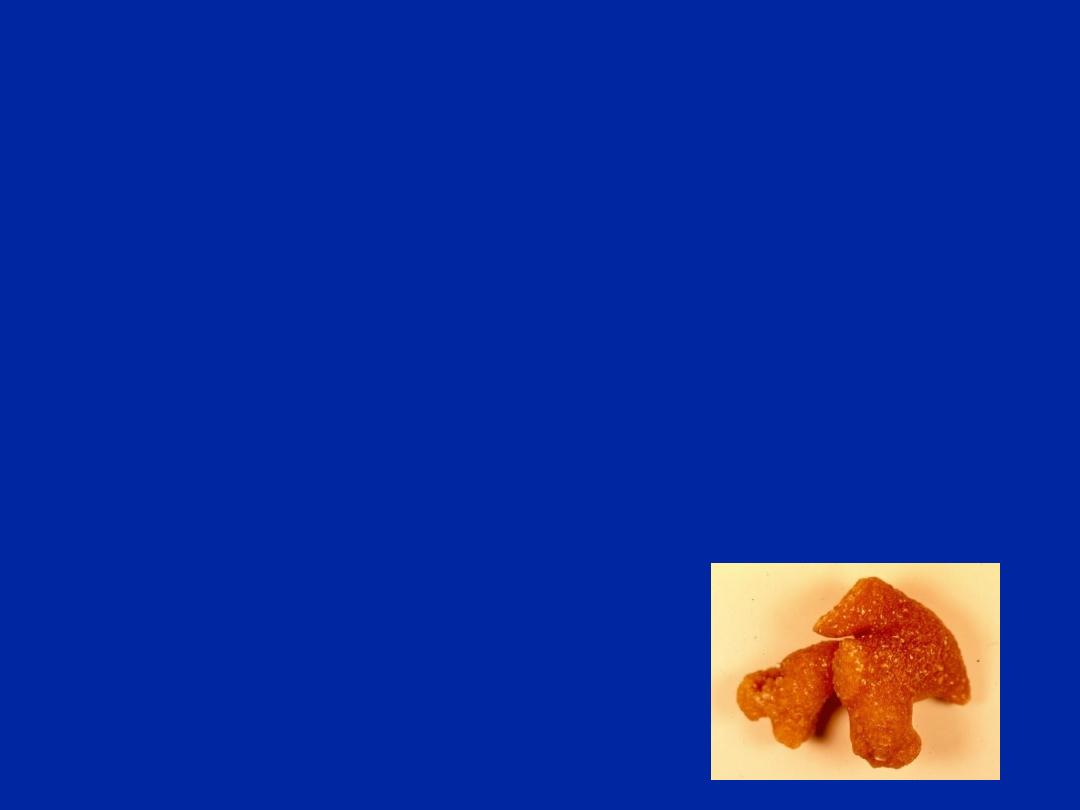
Calcium Oxalate

Type 2- dietary dependent
Common
Treated by calcium restricted diet
(no specific therapy)

Type3-phosphate renal leak (5%)
lead to decrease serum phosphate—increase V D3
synthesis—increase ca absorption &excretion.

2-resorptive hypercalciuria;
hyperparathyrodism 50% presented with renal stone.
suspected in Pt. with ca. phosphate stone, women with
recurrent ca. stones & those with both nephrocalcinosis
& nephrolithiasis .
Hypercalcemia is most consistent sign.
Calcium Phosphate

3-Renal induced hypercalciuria.
Intrinsic renal tubular defect in ca. excretion. lead to
secondary hyperparathyroidism
effectively treated by hydrochlorthiazide.

4-Hyperuricosuric calicium nephrolithiasis
5-Hyperoxaluric calcium nephrolithiasis
6-Hypocitrateuric ca.nephrolithiasis
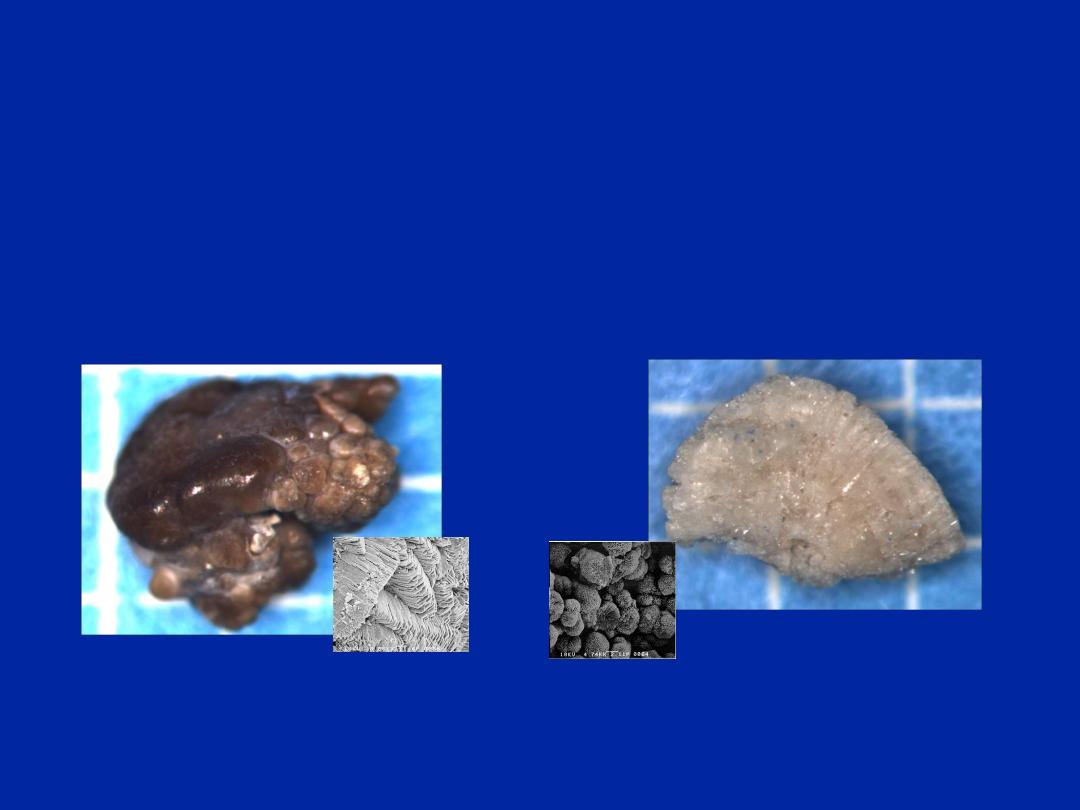
Calcium Oxalate
Calcium Phosphate
(60-70%)
Stone
types

B. Non calcium calculi.
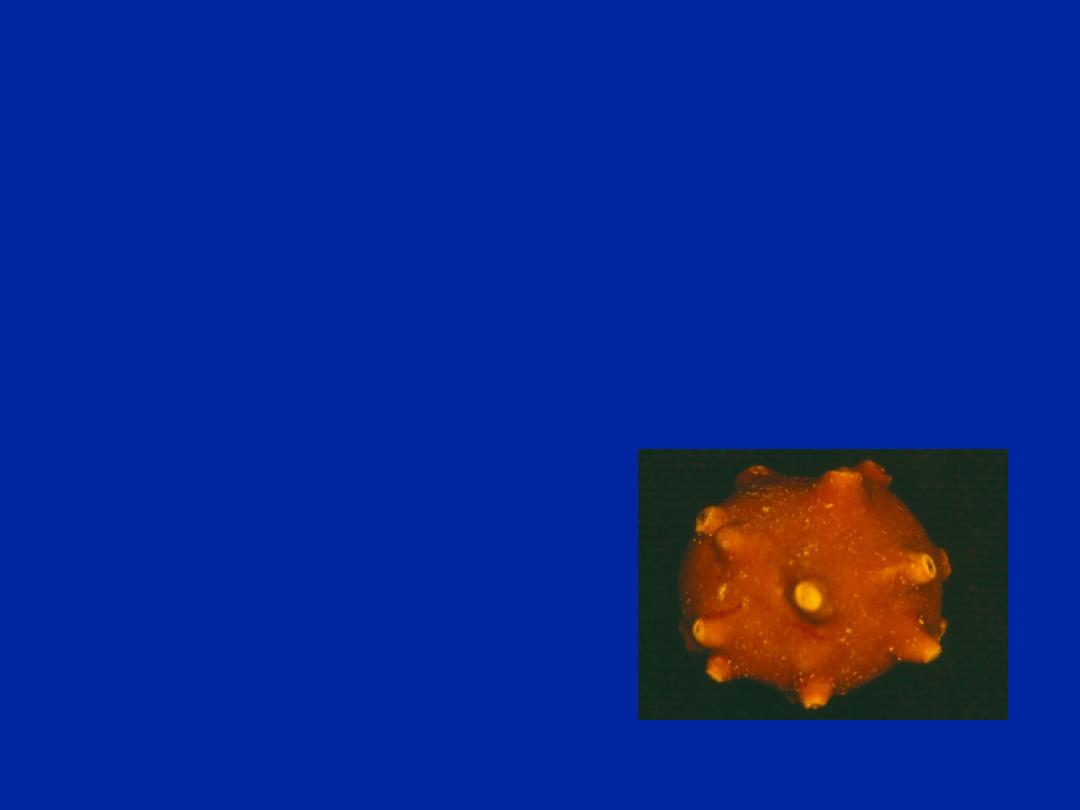
1- Struvite.
composed of MAP
(magnesium, ammonium, & phosphate).
Infection stone
urea splitting organisms
proteus,
pseudomonas
providencia,
klebsiella,
staph. &
mycoplasma.
Struvite (10-15%)

Most commonly in women & may recur rapidly.
usually staghorn calculus.
The high ammonium concentration derived from urea
splitting lead to alkaline urinary ph ranges from 6.8-
8.3
*normal urinary ph=5-7 in which MAP crystal
soluble.
2- Uric acid stone
Less than 10-15% of all urinary stones usually in men.
Specially pt. with gout,
myeloproliferative disease,
rapid weight loss, &
those treated with cytotoxic drugs.
Uric Acid (10-15%)
3-cystine
Secondary to inborn error of metabolism.
Resulting in an abnormal intestinal & renal absorption
of amino acid cystine, ornithine, lysine, & arginine.
Cystine lithiasis is the only clinical manifestation of
this defect.
penicillamine can reduce urinary cystine level it
complexes with amino acid—more soluble.
Cystine (1%)
Calcium Carbonate
Calcium Citrate
Ammonium Urate
(laxative abuse)
Uncommon
types of Stones
Xanthine
2,8-dihydroxyadenine
adenine phosphoribosyltransferase (APRT)
Cystine (1%)
dibasic AA transporter
Alcaptonuria
homogentisate 1,2-dioxygenase
Hereditary
Disorders
•
Polycystic kidney Disease
•
Medullary Sponge Kidney
•
Horseshoe kidney
Ciprofloxacin
Indinavir
Traimeterene
Sulfamethoxazole
Oxypurinol
Phenazopyridine
Phenytoin
Aminophylline
Drugs & Metabolites
(<1%)
Amoxicillin
herringlab.com

Urinary Calculus Disease:
Signs and Symptoms:
Colic nature of the pain
– Rapid onset
– Unable to achieve comfortable position (writhing)
Radiates from flank to groin
– Testis/labia
Associated nausea/emesis
– May develop ileus
Hematuria
– Gross, microscopic (present in 90%; absence doesn’t r/o)
Irritative LUTS
– May indicate stone near the UVJ/distal ureter
BEWARE OF FEVER
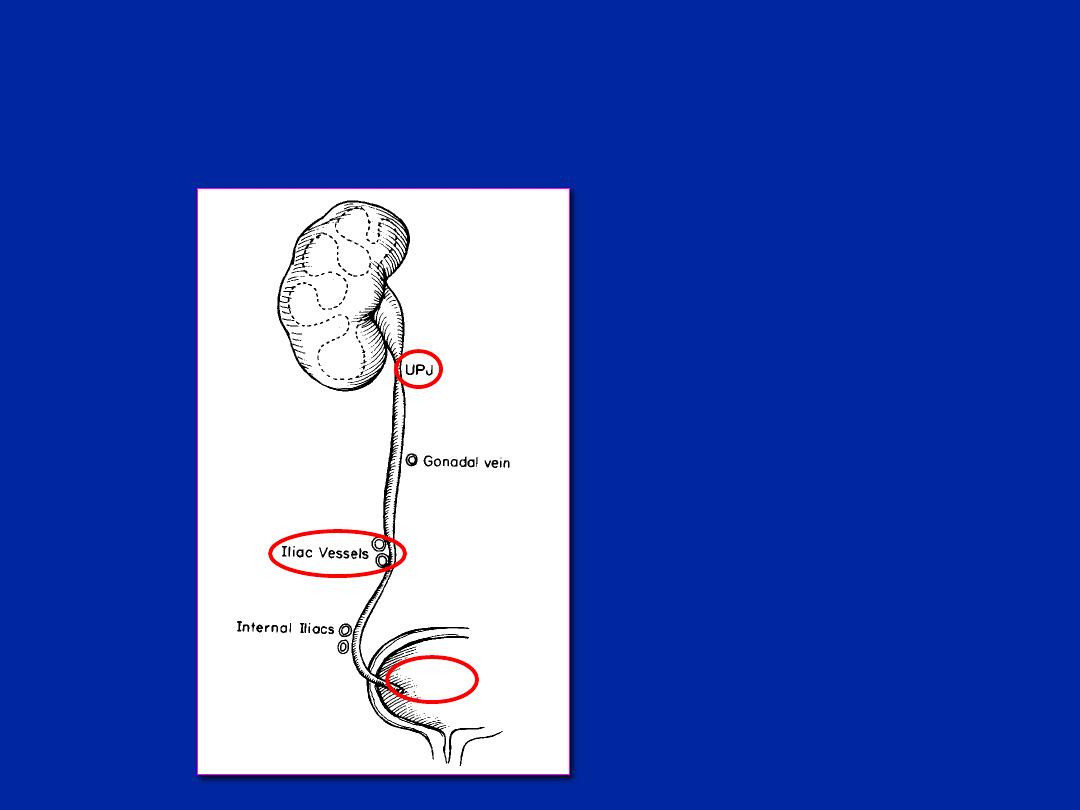
Urinary Calculus Disease:
Where do stones get stuck?
1)
UPJ: Ureteropelvic
Junction where the
renal pelvis meets the
ureter
2)
Pelvic brim: at the
level of the common
iliac vessels
3)
UVJ: Uretero-vesical
junction where the
ureter meets the
bladder
UVJ

Urinary Calculus Disease:
Differential Diagnosis
Bowel:
– Inflammatory bowel disease, appendicitis, diverticulitis
Gynecologic:
– PID, ruptured ovarian cyst, ectopic pregnancy
Neurologic/Musculoskeletal:
– Radicular pain, herpes zoster, muscle spasm/strain
Genito-urinary:
– Cystitis, pyelonephritis, torsion, UPJ obstruction

Urinary Calculus Disease:
Investigations
AFTER CAREFUL History and Physical
Labs:
– Urinalysis (microscopy is gold standard to look for crystals)
– Consider Pregnancy Test (HCG) in females
– CBC&diff (Look for ↑WBC, creatinine (R/o renal failure)
Imaging:
– KUB (Kidney-Ureter-Pelvis) Plain Radiograph of abd/pelvis
– Non-contrast Low-Dose CT abdopelvis (NCCT)
– IVP - more or less historical or in remote settings
– Ultrasound - first line in pregnancy
– Retrograde pyelography ( too invasive)

Urinary Calculus Disease:
Urinalysis (Microscopic)
90% will have at least microhematuria
May have some pyuria
– May not indicate UTI
May have crystals
– Not specific for stone disease

Urinary Calculus Disease:
Diagnosis - Imaging
KUB: First-line for initial and FU imaging
80-90% of stones are radio-opaque
Phleboliths (calcified pelvic vessels could be mistaken for
ureteral stones)
IVP:
Can
’t use in patients with Iodine allergy or Renal
Failure
Demonstrates stone location & degree of obstruction
Time consuming & contrast risk
CT (Non-contrast) LOW-DOSE protocol
Quick, sensitive, GOLD STANDARD for renal colic
Concurrent intra-abdominal pathology
Fulgham et al., J Urol, 2013
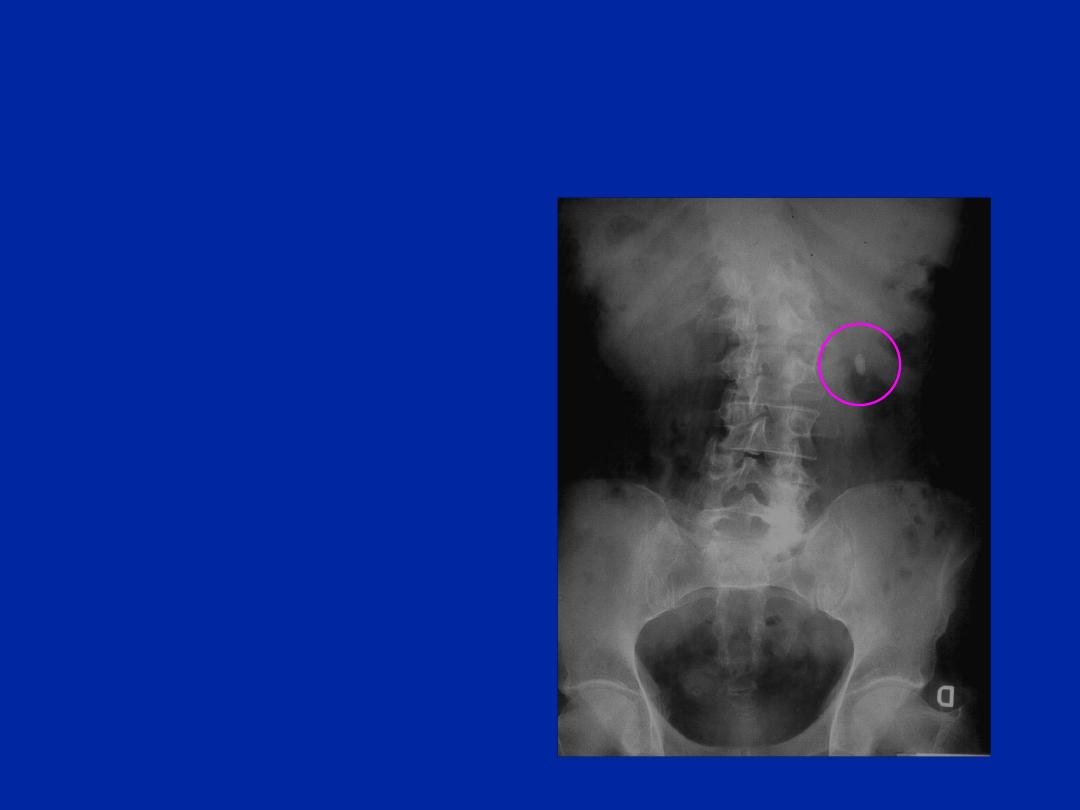
Diagnosis:
KUB
Advantages:
– 80-90% of stones are
radio-opaque
– Minimal radiation
Disadvantages:
– No detection of
concurrent pathology
– Bowel gas
– Easy to miss mid-
ureteral stones over
the sacrum

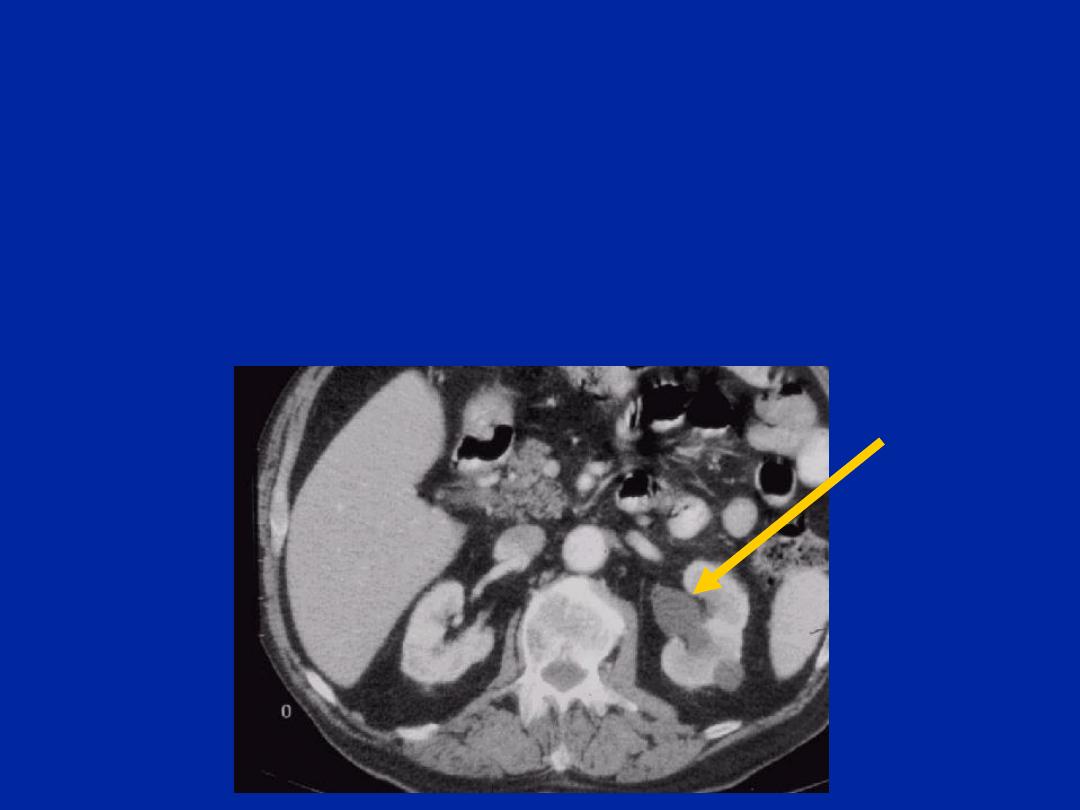
Diagnosis: Non-Contrast
“Renal
Colic
” Low-Dose CT Abd/Pelvis
Advantages:
– All stone types are visible except indinavir
» Sensitivity - 97%; Specificity - 96%
– Rapid
– Readily available
– Does not require contrast
– Other pathologies identified
– Information about stone and collecting system
obtained
Fulgham et al., J Urol, 2013

Diagnosis: Non-Contrast
“Renal
Colic
” Low-Dose CT Abd/Pelvis
Disadvantages:
– Increased radiation dose compared with KUB
» should always use Low-Dose protocols especially in
thin (BMI <30) patients
– Cost
– No physiologic information such as obstruction
– Has supplanted the KUB
» KUB useful for following radio-opaque stones and
determining suitability for Shockwave Lithotripsy
(SWL)
Fulgham et al., J Urol, 2013

Diagnosis:
Intravenous Pyelogram (IVP)
Scout film
Intravenous contrast
Serial Xrays
– Nephrogram phase (1min)
– Pyelogram phase (5 min)
– Delayed views (ureter)
– Post void
Time consuming (up to 2 hrs)
Contrast reaction risk
Can
’t use in patients with
Iodine allergy or Renal Failure

Diagnosis: Non-contrast CT (NCCT)
What are you looking for?
Stone size (height and width)
Stone density (Stones >500HU are opaque on KUB)
Location
– Renal (Pelvis; upper, mid, or lower calyx)
– Ureteral (UPJ, proximal, mid, distal, or UVJ)
Presence of hydronephrosis or hydroureter
Evidence of stranding
Gas in the collecting system
– Emphysematous (necrotizing) infection
– Rare but important finding necessitating urgent
broad spectrum antibiotics and drainage with NT
Diagnosis:
Non-contrast CT
Hydronephrosis (Note the L renal pelvis is
dilated when compared with R renal pelvis)
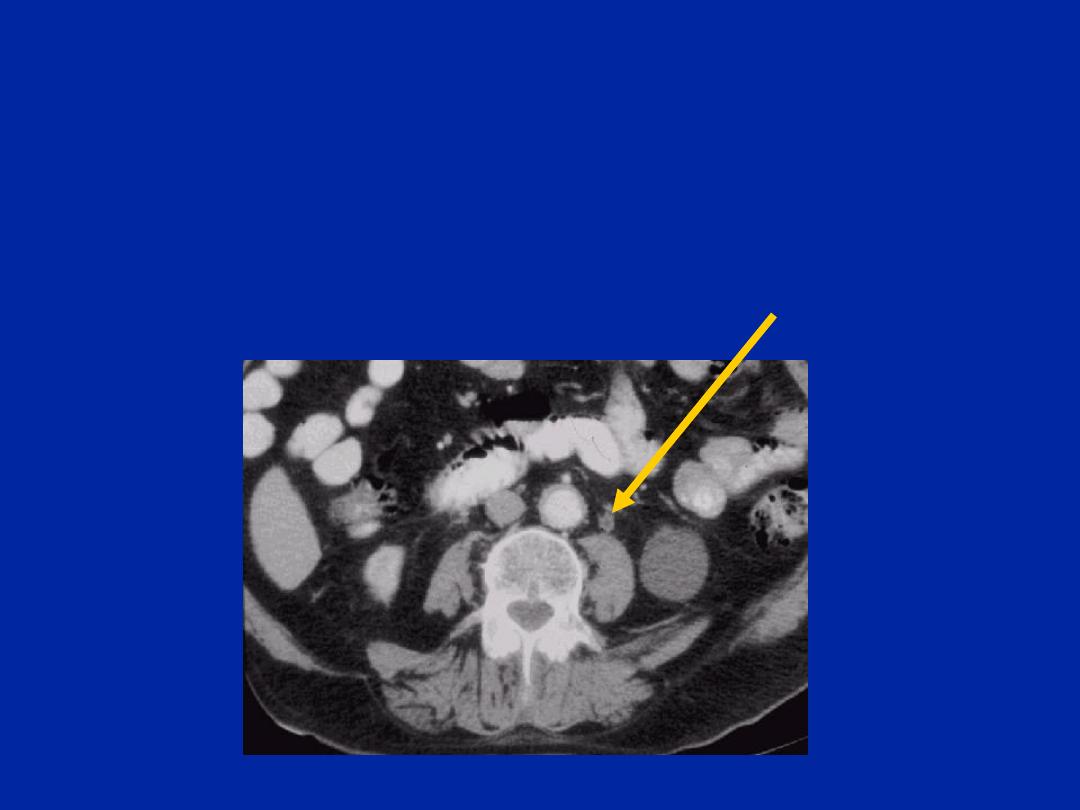
Non-contrast CT:
Ureteral Calculus
Dilated ureter above stone (hydroureter)
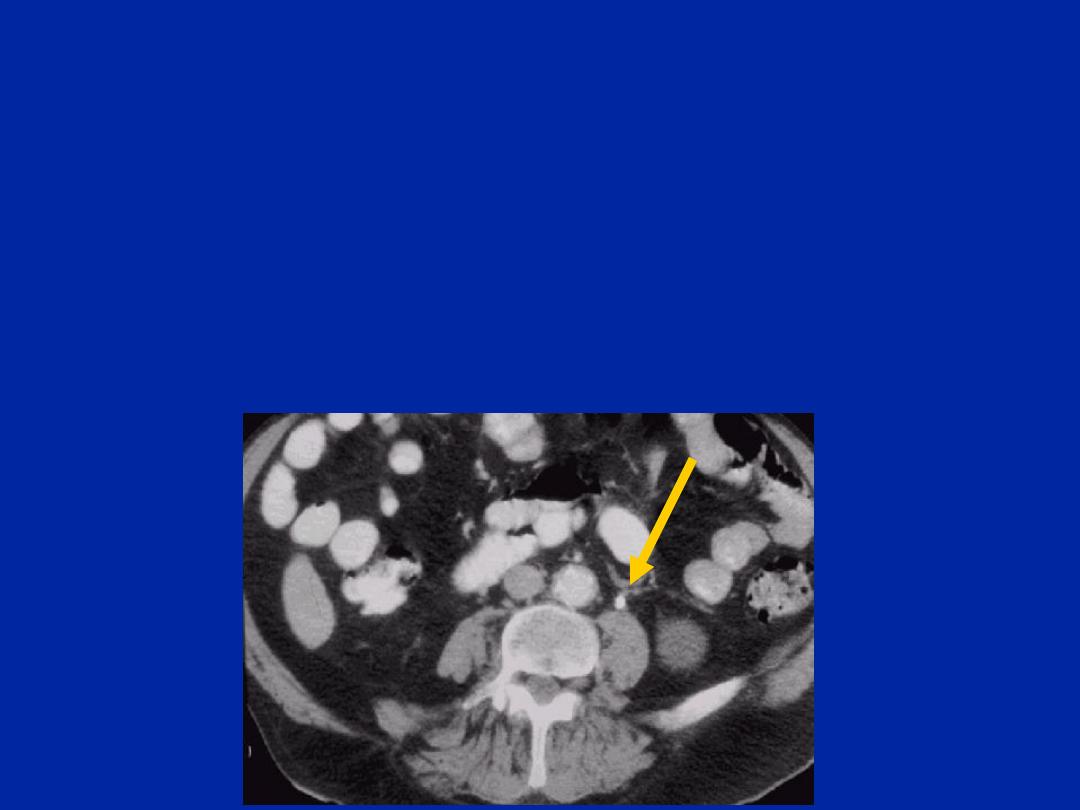
Ureteral Calculus:
Non-contrast CT
Stone visualization & location (i.e. L proximal ureter)
All stones, except indinavir, are
“opaque” on CT
“Tissue ring” sign

Calculus Disease:
Initial Management of Renal Colic
Pain control
– Narcotics
» Oral/IM/IV
– NSAIDS (renal function) (Avoid if planning SWL)
» Oral/rectal/IV
– Acetaminophen
– Anti-emetics
IV hydration prn
IF FEVER - CONSULT UROLOGY
– DISCUSS ANTIBIOTICS
Alpha-blockers as medical expulsive therapy (MET)
– Tamsulosin (Explain that these are off-label and
associated with dizziness and retrograde ejaculation)

Calculus Disease:
Initial Management Based on Size
<5mm (renal or ureteral)
– Discharge home with instructions to drink >2L of water/day
– Tamsulosin for ureteral stones
– 90% will pass spontaneously
– Should follow-up with urology within 1-2 weeks
» Fear is silent obstruction (painless) with UPJ or proximal ureteral
stones leading to irreversible renal loss
>5mm or signs of obstruction
– Consult urology
– +/- tamsulosin
Urinary Calculus Disease:
CONSULT UROLOGY URGENTLY IF:
Obstructing stone + FEVER/Infection
Bilateral Ureteral Stones
– Renal failure
Solitary Kidney
– Impending renal failure
These require urgent decompression
with ureteral (double J) stents or
nephrostomy

Urinary Calculi: Treatment
1.
Extracorporeal shock wave lithotripsy (SWL)
» Ureteral stones <1cm or renal stones <2cm
2.
Ureteroscopic laser lithotripsy (URS)
» Ureteral stones or SWL failures
3.
Percutaneous nephrolithotomy (PCNL)
» Large >2cm renal stones

Renal Calculi: Clinical Points
Spontaneous stone passage depends on:
1)
Location: Proximal vs. distal (distal stones
more likely to pass)
2)
Size: ~90% of stones <5mm will pass
3)
Time since onset: Most stones pass by ~40
days
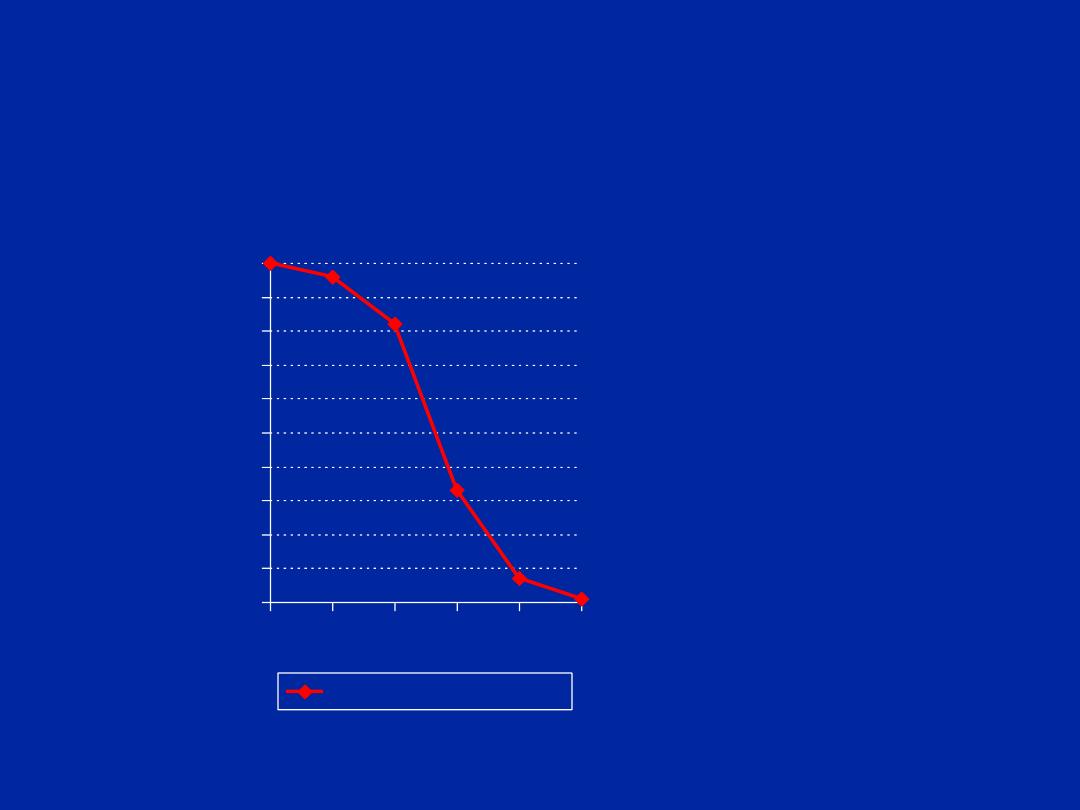
Stone Size:
Probability of Spontaneous Stone Passage
0
10
20
30
40
50
60
70
80
90
100
1
2
4
6
8
10
%
P
a
ss
a
g
e
Stone Passage Rate
•
Probability of
passage:
–
<4mm- ~90%
–
4-7mm- ~50%
–
>7mm- <10%
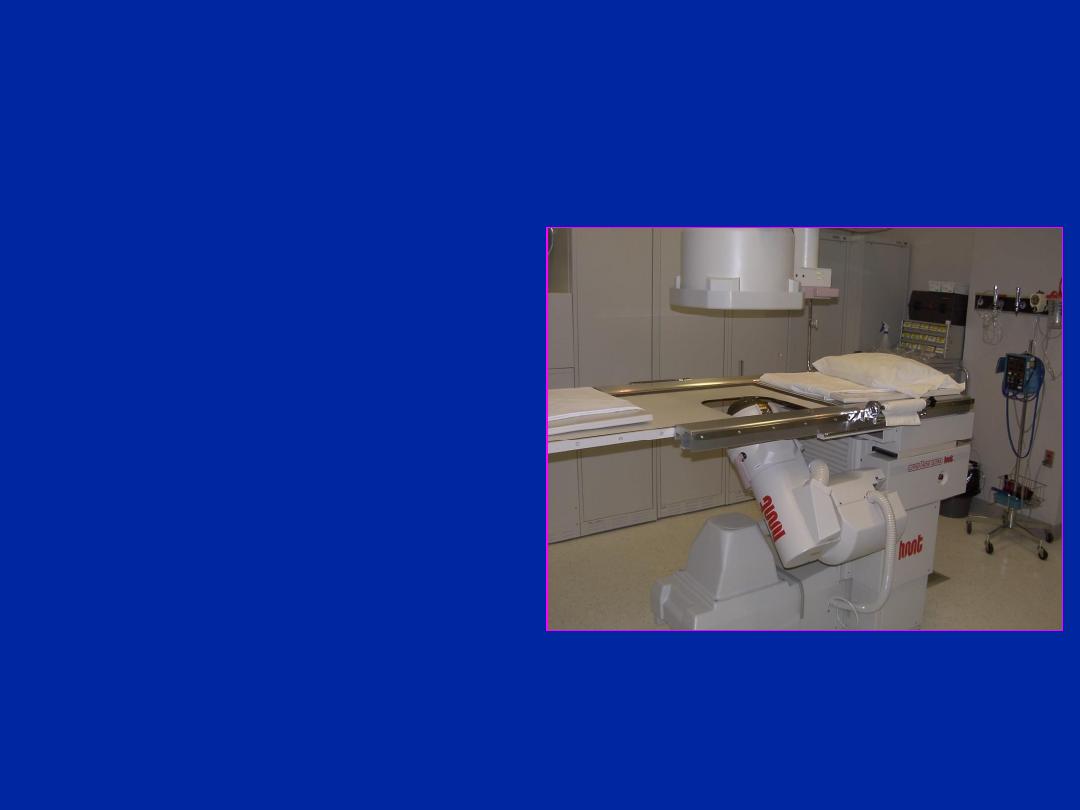
Urinary Calculus Disease Treatment:
Extracorporeal Shockwave Lithotripsy
(SWL)
Least invasive
Conscious sedation
Fragments stones that
the patient then passes
High patient satisfaction
May require more time
to become stone free
Renal calculi <2cm or
ureteral calculi <1cm

SWL:
Absolute Contra-indications
Pregnancy
Bleeding Disorder/anticoagulation
(NSAIDS pre-op)
Febrile UTI
Obstruction Distal to the stone being
treated

SWL:
Relative Contra-indications
Radiolucent stones due to difficulty in
localizing. To localize these stones:
– Could use ultrasound
– Could use retrograde pyelography or IVP
Pacemaker (Need to use gated shockwaves;
Pacemakers in the path of shockwaves
could be damaged)
Calcified renal artery/AAA
Severe orthopedic deformities

Post SWL follow-up:
Tamsulosin improves stone-free rates
KUB in 2-4 weeks post-treatment
May continue to pass fragments for
several weeks
Ultrasound to rule out silent obstruction

SWL success depends on:
Stone Size
(Better if <1cm)
Stone Location
(Better if renal pelvic)
Stone Density/ Composition
(Better if HU<1000)
– Hounsfield unit density on NCCT
Patient Habitus
(Better if skin-to-stone distance <10cm)
Worse if associated renal anomalies:
– UPJ Obstruction
– Horseshoe kidney

Complications of SWL
Hematuria
Hematochezia
Ureteral obstruction - 5-30%
– Depends on size of initial stone
– “steinstrasse” (stone fragments obstructing ureter)
– Intervention as per other ureteral stones
Sepsis - 1%
Perinephric Hematoma - <1%
Hypertension/DM- no convincing evidence that SWL
leads to long term HTN or DM

When do we not use SWL?
Stone Burden
– >2cm in largest diameter or multiple stones
Stone composition
– Particularly cystine or brushite stones
Patient needs to be stone-free such as pilots
– Or stone-free faster
Patient habitus (skin-to-stone distance >10cm)
Failed SWL
– 2nd treatment reasonable
– Diminishing returns of 3 or more treatments

Ureteroscopic (URS) Holmium Laser
Lithotripsy for Ureteral Stones
Advantages:
– Near 100% stone free rate
– Low retreatment rates
– Treatment available in most centres
» SWL tends to be in regional centres only
Disadvantages:
– General anesthesia is usually required
– Ureteral stent (DJ) may be left
» Stent symptoms are bothersome to patients
– Lower patient satisfaction
Typically for ureteral calculi and
SWL failures
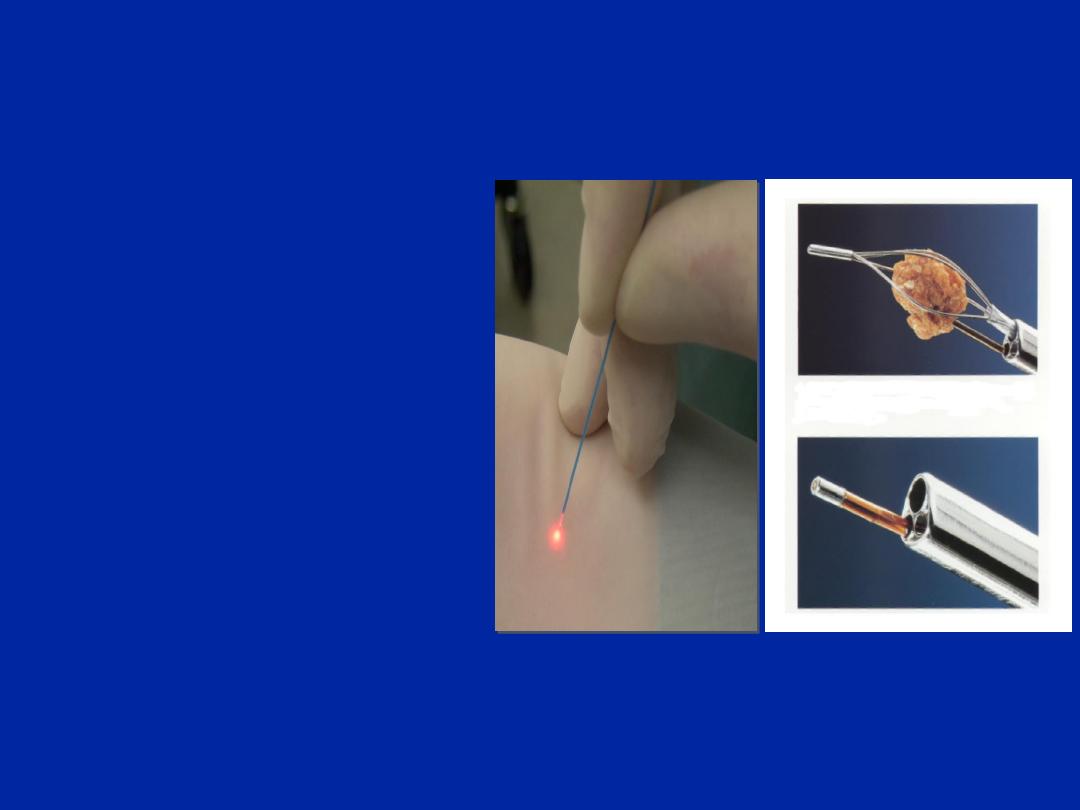
Ureteroscopic Equipment:
Scopes are either:
– Semi-rigid
– Flexible
Stone Fragmentation
– Holmium:YAG laser
Stone Retrieval
– Baskets
– Graspers
One of the best innovations in urology over the last
2 decades
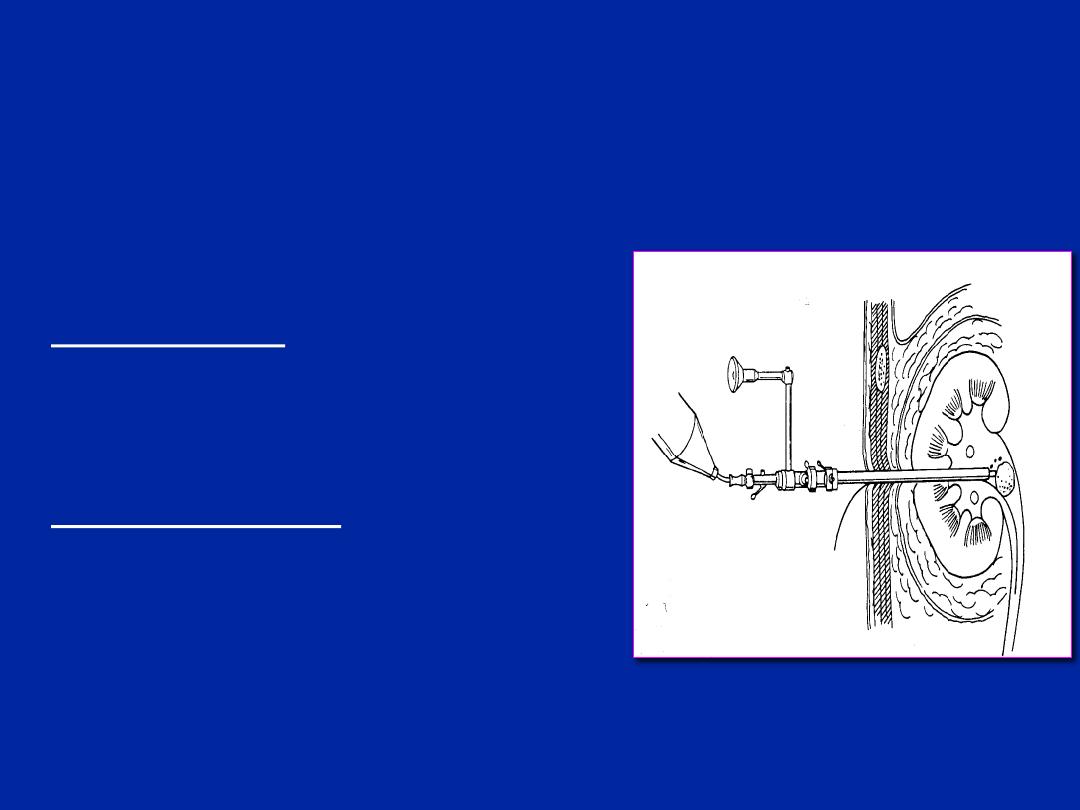
Urinary Calculus Disease:
Percutaneous
Nephrolithotripsy
Typically for large (>2cm) renal
calculi
Advantages:
– Ability to remove large or multiple
stone burden with high success
rate (>95%)
Disadvantages:
– General anesthesia
– More invasive than URS
– Risk of bleeding <5% require
transfusion
– Injury to surrounding organs
– Risk of hydropneumothorax

Percutaneous Nephrolithotripsy:
Complications
Sepsis or SIRS
Bleeding requiring transfusion or selective
angioembolization.
Perforation of the renal pelvis
Stricture
– UPJ or infundibulum
Residual stone fragments
Hemothorax/pleural effusion (<10%)
Adjacent organ injury (colon perforation)

STONE PREVENTION

Stone Prevention:
Basic Work-Up for ALL PATIENTS
Urinalysis and culture
– Urea splitting organisms (Proteus, Pseudomonas,
Klebsiella, mycoplasma, Serratia, Staph Aureus)
– Acidic urine - uric acid/cystine/CaOxalate stones
– Alkaline urine - struvite stones
Serum electrolytes (Na, K, Cl, HCO
3
), urea,
creatinine, and uric acid
If elevated normalized serum calcium then obtain
PTH to rule out Primary Hyperparathyroidism
Send stone for analysis

Stone Prevention:
Detailed Metabolic Work-Up Indications
Children (<18 years of age)
Bilateral, recurrent or multiple stones
Non-calcium stones (e.g., uric acid, cystine)
Pure calcium phosphate stones
Complications from stones (AKI, sepsis, or admission)
Any stone requiring percutaneous nephrolithotomy
Solitary kidneys (anatomical or functional)
Patients with renal insufficiency
Systemic disease (gout, osteoporosis, bowel disorders,
hyperparathyroidism, renal tubular acidosis,etc.)
High-risk occupations (e.g., pilots, firemen)

Stone Prevention:
Detailed Metabolic Work-Up:
In addition to the Basic metabolic work-up, it includes:
Two 24-hour urine collections:
Volume, creatinine, calcium, sodium, potassium,
oxalate, citrate, uric acid, magnesium
Cystine if suspect cystine stone or if the stone
analysis is cystine

Stone Prevention:
General Advice
Increase Hydration to 2-3L per day to achieve daily
urine output of 2.5L
Diet:
– Maintain normal calcium intake (1000-1200mg with meals)
» Used to advice low calcium diets
– Proven to be false
– Minimize foods high in oxalate (Spinach, peanut, rhubarb)
– Minimize salt (<2300mg/d) and animal protein
– Increase fiber, vegetables and citrus-rich fruits
Consider urinary alkalinization:
– Mainly for uric acid and cystine stones
– Potassium citrate - preferred
– Sodium citrate - alternative

Stone Prevention:
Calcium Stones (80%)
Most stones are calcium oxalate
Some are calcium phosphate or mixed
Etiology
– Hypercalciuria
» Increased intestinal absorption
» Bone resorption (
↑PTH)
» Renal leak
– 25% also have hyperuricosuria
– Hyperoxaluria
» Usually increased intestinal absorption - SB
resection/IBD
» Ingestion of oxalate-rich foods
– Hypocitraturia

Stone Prevention:
Prevention of Calcium Stones:
Hydration - 2-3L of urine per day
Normal dietary calcium intake (1000-
1200mg/d)
Dietary limitations:
– Salt - potentiates hypercalciuria
– Oxalates – Tea/chocolate/Spinach/Rhubarb
– Animal protein
Consider Thiazide for hypercalciuria
Consider potassium citrate for acidic urine
(pH<6.0) and hypocitraturia

Stone Prevention:
Struvite Stones (5-10%):
Triple phosphate
– Calcium Magnesium, ammonium phosphate
Alkaline urine pH due to urea splitting
organisms
– Proteus, Pseudomonas, Klebsiella, Mycoplasma,
Serratia, Staph Aureus
– NOT E COLI
Must clear all stone material and infection
– SWL often not useful
May form staghorn stones quickly

Stone Prevention:
Uric Acid Stones (10%):
Radiolucent - not visible on KUB
Occur in patients with low urine volume
and acidic urine (pH<6.0)
– Purine-rich diets
– High cell turnover - cancer treatment
Prevention:
– Hydration
– Alkalinize urine

Stone Prevention:
Cystine Stones:
Usually first detected in children
– Often positive family history
AR defect in absorption of dibasic amino acids
– COLA
– Only cystine is insoluble
Rapid formation of staghorn stones
Must remove all stone material aggressively
– SWL has limited application
Prevention:
– Hydration (Need to produce >3L of urine per day)
– Low salt and animal protein
– Alkalinize, penicillamine, thiola, captopril (not effective)

Thank you
