Liver diseases in pregnancy
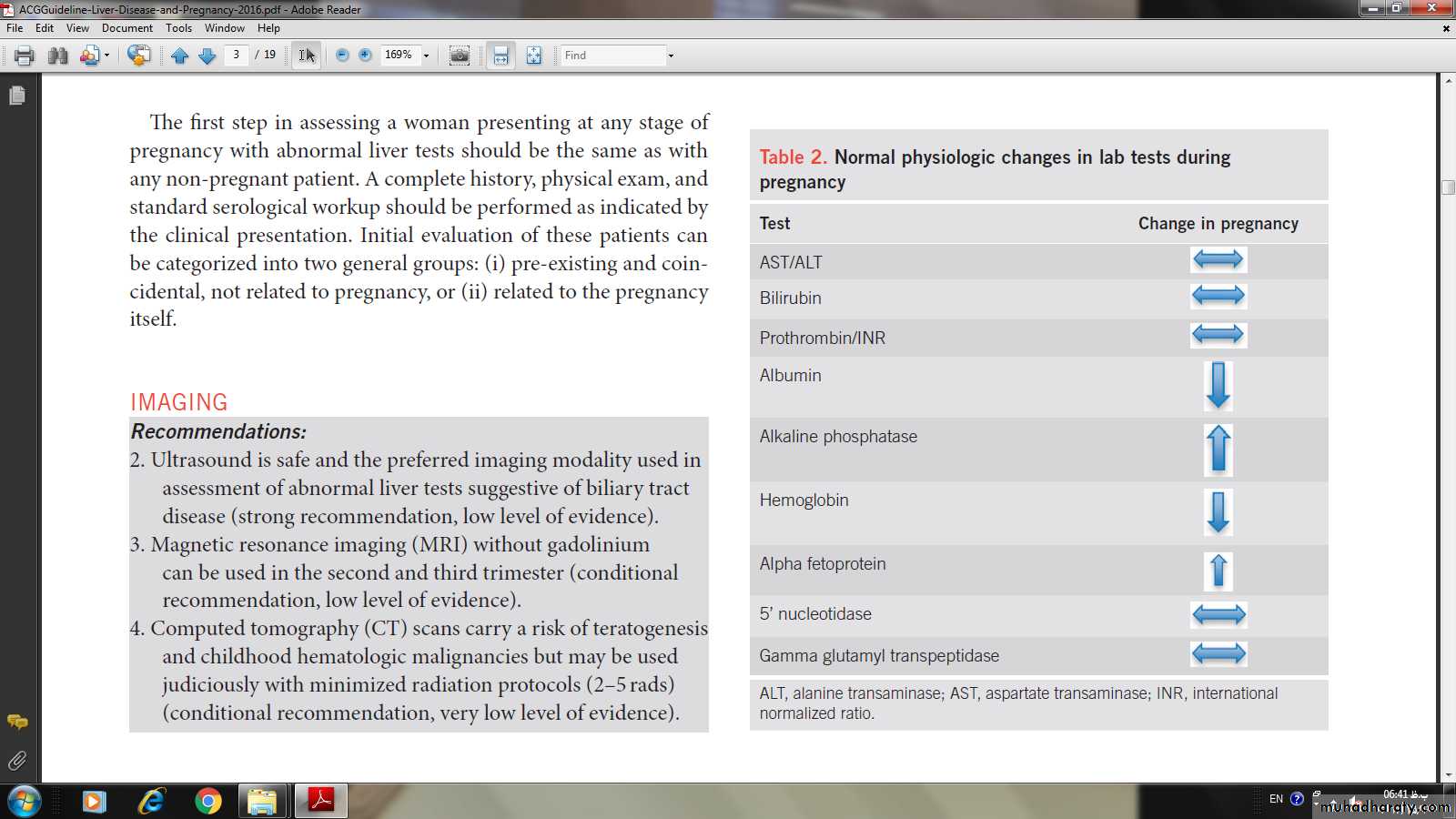
Dr. Huda Adnan SahibMetabolic changes in pregnancy appear to be of no effect in normal pregnancy.
Jaunice in pregnancy can be due to either1)diseases related to pregnancy
Hyperemesis gravidarum
Intrahepatic choestasis in pregnancy
Acute fatty liver in pregnancy
HELLP syndrom
2)diseases coincident with pregnancy
hepatitis
Fulminant hepatic failure
Liver cirhosis
Diseases unique to pregnancy
HG is defined by persistent vomiting, associated with loss of 5% or more of pre-pregnancy body weight, dehydration, and ketosis. HG is uncommon (0.3–2% of pregnancies), occurs early in the first trimester, and typically resolves by 20 weeks gestation. Risk factors for HG include molar pregnancy, multiple pregnancies, trophoblastic disease, prior HG, and fetal abnormalities (triploidy, trisomy 21, and hydropsfetalis)
Liver test abnormalities are common in HG and resolve when the vomiting stops. In all, 50–60% of hospitalized women with HG will have a mild elevation in aminotransferase levels, although AST and ALT levels more than 20 times the upper limit of normal rarely have been reported
Jaundice and hepatic synthetic dysfunction are uncommon. Although women with HG have increased rates of low birth weight (LBW) babies, small for gestational age babies, preterm birth, and poor 5-min Apgar scores, outcomes are generally favorable. Management of HG is supportive, however, given the risk for electrolyte abnormalities and dehydration, hospitalization is not infrequent
Intrahepatic cholestasis of pregnancy
IHCP occurs in incidence about 0.3-5.6% and it is the most common liver disease in pregnancyRisk factors for IHCP
advanced maternal age
history of cholestasis secondary to oral contraceptives.
personal or family history of IHCP. Some studies suggest a higher prevalence in patients with hepatitis C, cholelithiasis, and nonalcoholic fatty liver disease. Evaluation for alternative etiologies should be done if colestasis fails to resolve after delivery.
Clinical features
persistent pruritus, typically involving the palms and soles as well as the rest of the body and resolves with delivery.Jaundice occurs in <25% of IHCP patients, always after the onset of pruritus.
Fat malabsorption can result in fat-soluble vitamin defi ciencies requiring supplementation
Maternal outcomes are excellent, however, there is a risk of fetal distress, preterm labor, prematurity, and intrauterine death.
Early delivery at 37 weeks is encouraged, because intrauterine death is more common in the last month of pregnancy and few deaths occur before 37 weeks.
Investigation
1)Increased bile saltsIn IHCP, bile acid concentrations are typically >10 μ mol/l with increased cholic acid levels and chenodeoxycholic acid levels. Bile acid levels also correlate with fetal distress. Most complications occur when bile acid levels exceed 40 μ mol/l
2)Increased bilirubin level
3)liver enzymes
Aminotransferase levels may also be elevated, reaching values >1,000 U/l.
4)Ultrasonography should be performed to exclude cholelithiasis.
Treatment
Urodeoycolic acid 10-15 mg /kg woman weight.Antihistamines
Emollient
Vit k supplementation to woman after 36 wk and to the neonat after delivery in a dose of 0.1 mg i.m.
Serial liver function monitering
Delivery at 37 weeks G.A.
Preeclampsia and eclampsia
Preeclampsia is characterized by new onset hypertension (systolic blood pressure ≥140 mm Hg or dystolic blood pressure ≥90 mm Hg) and proteinuria (≥300 mg/24 h) after 20 weeks of gestation.
Organ dysfunction defines severe preeclampsia and can include hepatomegaly and hepatocellular injury. Up to 7.5% of all pregnancies are affected, but only 25% of preeclampsia cases are severe. Liver involvement is not a common expression and when it does occur symptoms are generally non specific. Eclampsia is present when grand mal seizures occur.
Hepatic involvement can present with epigastric or right upper quadrant pain, likely from hepatomegaly stretching Glisson’s capsule. Liver injury results as a consequence of vasoconstriction and fibrin precipitation in the liver. AST and ALT elevations can be striking.
Complications can include hematoma below Glisson’s capsule and hepatic rupture.
Th e magnitude of the liver chemistry abnormalities parallels the risk of adverse maternal but not fetal outcomes. Liver tests cannot exclusively be used to gauge clinical decisions, as the presence of normal liver enzymes does not exclude disease. An expectant approach is advised until after 34 weeks gestation to limit fetal morbidity. However, delivery is the only curative treatment and after 36–37 weeks there is no advantage in continuing the pregnancy.
HELLP syndrome
HELLP syndrome is characterized by hemolytic anemia, increased liver enzymes, and low platelets. HELLP affects a minority of pregnancies but complicates up to 20% of cases of severe preeclampsia/eclampsia. Although HELLP typically presents between 28 and 36 weeks of gestation, 30% manifest symptoms in the first week postpartum. Risk factors include advanced maternal age, nulliparous.The hypertension-related liver diseases share similar clinical presentations. Differentiation is difficult as there is overlap in their features. The diagnosis of HELLP is most oft en made through recognition of typical laboratory results. Signs of hemolytic anemia and thrombocytopenia with platelets <100,000 cells/μ l, elevations in AST, ALT, serum bilirubin, and lactate dehydrogenase are expected.
There are no pathognomonic clinical signs and some women with HELLP may be asymptomatic. Right upper quadrant and epigastric pain, nausea, vomiting, malaise, headache, edema, and weight gain are common complaints. Hypertension and proteinuria should be expected, occurring in up to 80% of cases. Jaundice is rare, occurring in only 5% of patients.
Maternal consequences can be sever with mortality rates of 1–3% . Progression can also be rapid but laboratory values typically begin to normalize 48 h postpartum. Fetal prognosis is most strongly linked to gestational age at delivery and birth weight.
Hepatic consequences include hepatic infarction, subcapsular hematomas, and intraparenchymal hemorrhage. When the ALT or AST is >1,000 U/l or abdominal pain radiates into the right shoulder, cross-sectional imaging can assist in excluding hepatic complications with more accuracy than ultrasound.
Hepatic infarction should be suspected with right upper quadrant pain with fever, whereas abdominal swelling or shock presentation can occur with hepatic rupture.
Management
Blood pressure control
Termination of pregnancy
Glucose supplementation
Platelete transfusion .
Glucocorticoid is of no evidence for benefit.
Surgery indicated only in unstable patient with hepatic hematoma 0r rupture capsule.
Acute fatty liver disease of pregnancy
AFLP is a rare, life-threatening condition characterized by microvesicular fatty infiltration of the liver(due to dficiency of long chain 3 hydroxyacyl CoA dehydrogenase LCHAD enzyme) leading to hepatic failure. The median gestation age at the time of identification is 36 weeks. Risk factors include twin pregnancies and low body mass index , male sex pregnancy, history of AFLP
Mortality rate reach 12.5-18%,neonatal mortality reasch 50
50%.
Clinical features
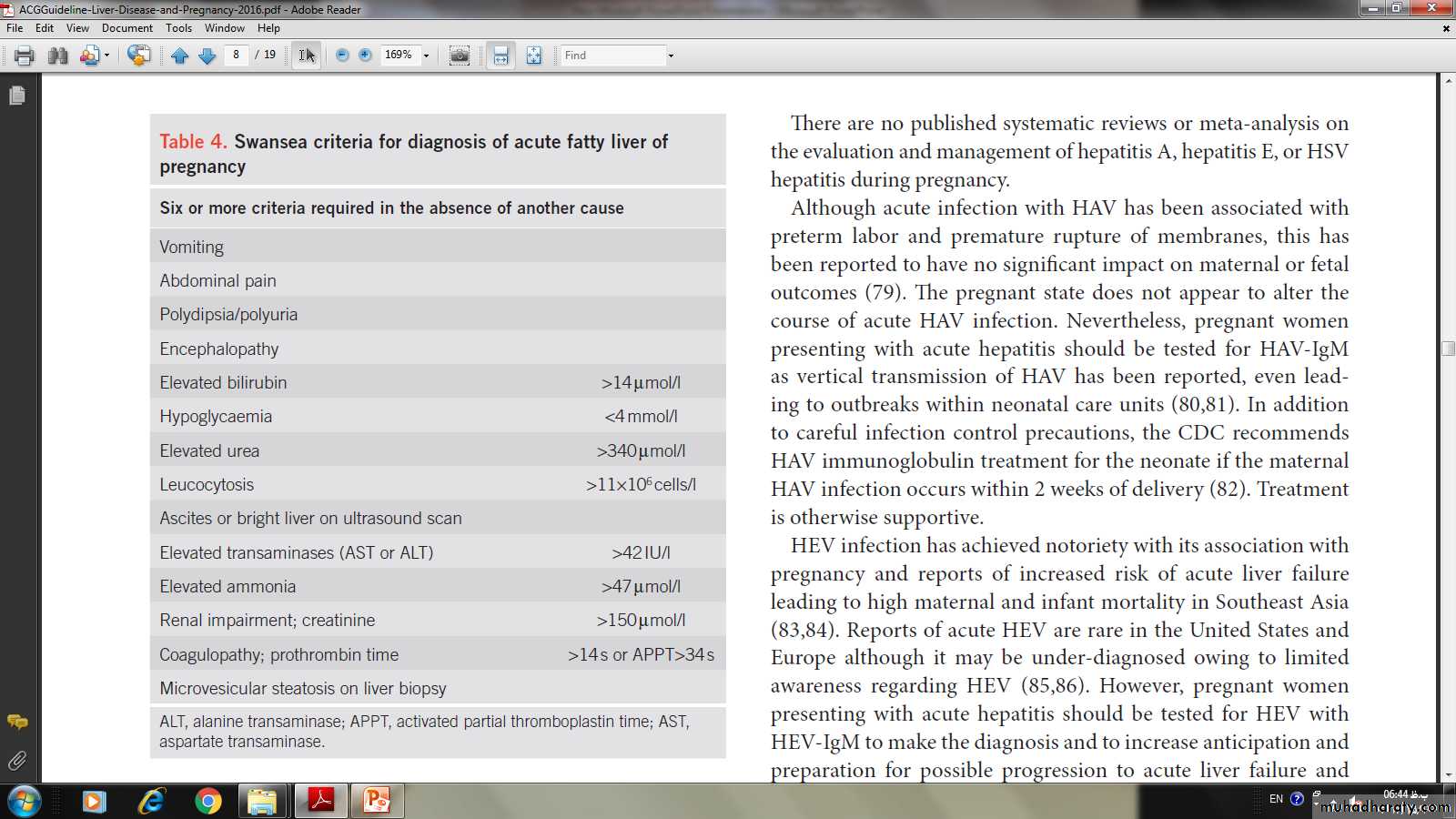
Presenting symptoms are non-specific: nausea, vomiting, and abdominal pain. Concomitant preeclampsia is present in roughly one half of the affected women. Hepatic failure can manifest with signs of hepatic dysfunction such as encephalopathy, coagulopathy, and hypoglycemia. Renal dysfunction and pancreatitis are common.The diagnosis of AFLP is usually made clinically based on compatible presentation, laboratory, and imaging results. The “Swansea Criteria” ( Table 4 ) combine symptoms and laboratory derangements
TreatmentEarly recognition, prompt delivery, and supportive care are essential to optimize maternal and fetal prognosis including correction of hypoglicemia ,coagulopathy and electrolyte disturbance, as the postpartum clinical course is dependent on the interval between symptoms and termination of the pregnancy. If hepatic function does not rapidly improve, evaluation for liver transplantation offers the patient the best chance for survival.
2) Disorders incidental to pregnancy :
Viral hepatitis A , B , D (caused by hepatitis B associated Delta agent) , hepatitis C&E ( non A – non B formally known ) .Clinical features : of hepatitis in pregnancy .
Signs and symptoms , complications identical in pregnant and non-pregnant female .
HAV : abrupt onset .
HB , C , D prolonged onset .
nausea , vomiting , abdominal pain appear before jaundice , anorexia , malaise , fever , dark urine, hepatomegaly and the symptoms improve with appearance of jaundice .
Investigations :
increase serum transaminase . with or without TSB , in serum alanine transaminase indicates acute hepatic injury .
Anti-hepatitis A and E IgM . Hepatitis e Ag indicate active hepatitis B ) , Hepatitis s Antibody Chronic hepatitis B .
Moderate increase alkaline phosphatase .
Leukocyte count normal in contrast with leukocyte in acute fatty liver of pregnancy .
( Prolonged PT , Thrombocytopenia ) in viral hepatitis .
Renal function test normal
Clinical and biochemical recovery take 1-2 months
In serve cases may perinatal mortality rate and maternal morbidity , the hospitalization indicated until she is able to eat and drink & liver function is not deteriorating . There is no transmission frm the mother to the fetus.
Hepatitis B :
1. Its course is not altered by pregnancy .
2. Hepatitis B may lead to Acute fulminant hepatic failure occasionally .
3. Preterm labour .
4. Feto-maternal transmission occur with Hepatitis B
Routes of transmission to fetus :
1) transplacental ( rare )2) Vertical transmission during delivery by contaminated amniotic fluid and birth canal secretion .
3) Through breast feeding .
4) Salivary contamination .
Prevention of neonatal infection of hepatitis B
1. Serological screening for all pregnancy ( routinely ) offered at their antenatal booking visit for anti core-antibody if positive for first time the infections status of the patient should be ascertained by serology and testing of the partner and testing for other sexually transmitted disease .
2. Intra partum fetal scalp electrodes and fetal blood sampling should be avoided and use of forceps rather than ventouse ( if needed ) .
3. Keep the membranes intact for as long as possible .
4. Administer hepatitis B . Immunoglobulin to those neonates born to high-infectivity mother .
So provided babies with immunized , there is no contraindication to breast feeding .
Hepatitis C :
The same as B , But with :Screening for Hepatitis C is not offered routinely in the Antenatal care .
Breast feeding does not appear to risk of the mother to child transmission .
Cholelithiasis is common in pregnancy owing to the increased estrogen levels, causing cholesterol supersaturation and increased gallstone formation. Cholecystitis is the second most common surgical condition in pregnancy and occurs in ~1 in 1,600 to 1 in 10,000 pregnancies. The incidence of cholelithiasis in pregnant women is 3.5% ( 10 ).
Management
*consevetave
*surgical in sver cases.
MANAGEMENT OF BILIARY DISEASE IN PREGNANCY