Fetal monitoring during labour
Dr. Huda Adnan SahibFetal monitoring during labour
The objective of fetal monitoring during labour is the prediction & diagnosis of fetal asphyxia before fetal / newborn morbidity with particular reference to brain damage has occurred .
- Fetal asphyxia :
Is defined as a condition of impaired blood gas exchange leading , if it persists , to progressive hypoxemia & hypercapnia .
Fetal monitoring :
Is performed in all labours ,low-risk labour should be monitored by intermittent auscultation by ear ( pinard ) or by using hand-held Doppler devices .- High-risk labours employ continuous electronic FHR monitoring , either ways the rate is entered on the partogram ( every 15 min – 1/2 hr ) .
So on admission ask your self ?
Are there any risk factors present ? e.g.
1. Maternal problems :
1. previous C/S . 6. DM ( Diabetes )2. PET ( pre-eclampsia ) 7. APH ( antepartum heamorrhge)
3. Postterm pregnancy .
4. Induced labour 8. Maternal Fever .
5. Oxytocin use . 9. Epidural analgesia .
2. Fetal problem :
1. IUGR ( intrauterine growth restriction )2. Oligohydramnias .
3. Meconium stained – liquor .
4. Multiple pregnancy .
5. Abnormal Doppler arterial velocimetry .
If the answer is =No intermittent Auscultation .
=Yes( CTG )
( continuous cardiotocography )
Intermittent Auscultation of FHR :
1. For 6o sec. after a contraction .2. Every 15 – 30 min in 1st stage .
if abnormal FHR:shift to contineous CTG.
3. Every 5 min in 2nd stage .
if abnormal FHR:shift to contineous CTG.
Contineous CTG :
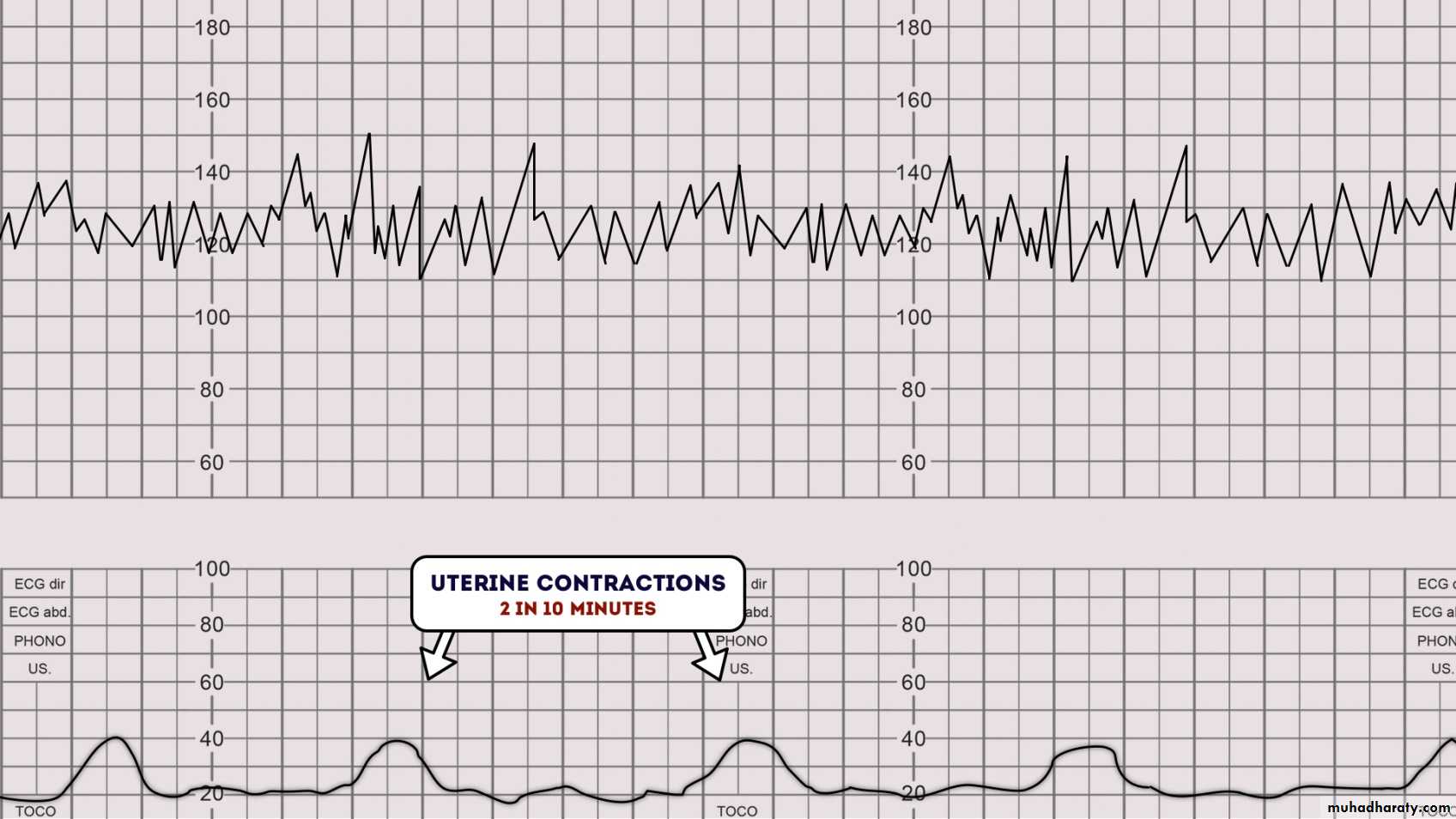
1. External machine which is a probe that measures uterine contractions and fetal heart rate & both are recorded on a paper and we see the relationship between them & assess the fetal well-being .- The female should be Lt- lateral or semi-recumbent position to avoid vena-cava compression , ( 2 transducers for : FHR + tocodynometer ) .
- Recordings are made for at least 30 mins .
2. Internal machine : More invasive , but more accurate , the probe is placed inside the amniotic sac to assess uterine contractions , but they need rupture of membranes , fetal scalp electrode for fetal ECG , it may cause ascending infection to the fetus .
Four parameters should be evaluated in each record :
1. Basal FHR , 2. variability 3. accelerations . 4. decelerations .
* Factors that cause fetal distress during labour :
I ) Maternal causes :1. Hypotension
2. sever maternal anemia
3. cardiac disease .
4. seizures
5. pulmonary diseases
6. hypertension .
II ) Fetal causes :
1. anemia ( as in Rh – Iso immunization )
2. Infection .
3. Twin to twin transfusion .
III ) Uterine causes :
1. Tetanic contractions of the uterus .2. Hyperstimulation : The commonest cause , is iatrogenic by uncontrolled oxytocin .
IV ) Umbilical cord causes :
1. Single umbilical artery blood flow to the fetus .2. Vasa – praevia .
3. Short-cord
4.placental Haematoma .
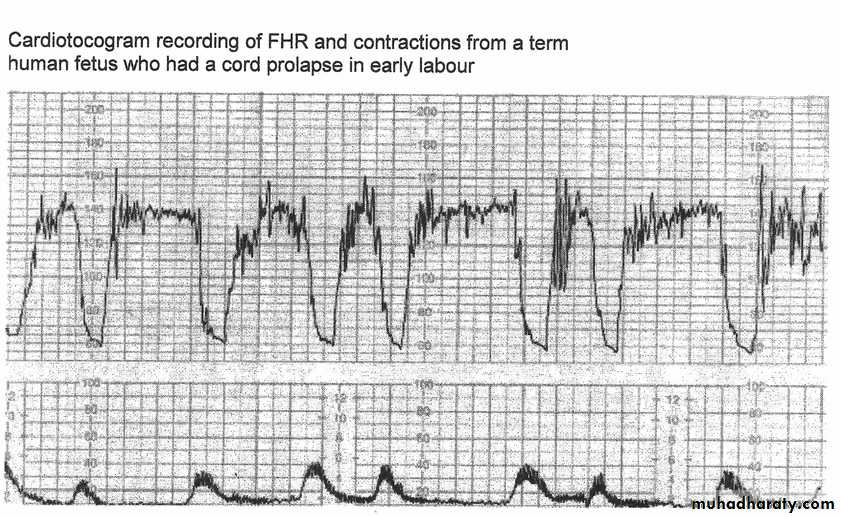
5. True-knots in umblical cord6. Prolapse of the cord .
V ) Placental causes :
1. Infection .2. placenta abruption .
3. Post mature placenta .
(reduce functioning due to aging ) .
Abnormalities of fetal heart monitering:
1. Brady cardia : Defined as a decrease in the baseline FHR to < 110 bpm .- Possible causes : 1. Fetal hypoxia . ( as late sign )
2. Medications ( Narcotics )
3. Epidural anesthesia .
4. Oxytocin ( pitocin )
5. Maternal hypotension .
6. Cord prolapse .
2. Tachy cardia : Baseline FH > 160 bpm.
Possible causes :1. Fetal hypoxia ( as early sign )
2. Medications ( ex. terbutaline )
3. Prematurity .
4. Maternal anxiety .
5. Maternal fever .
6. Fetal infection .
7. Thyrotoxicosis .
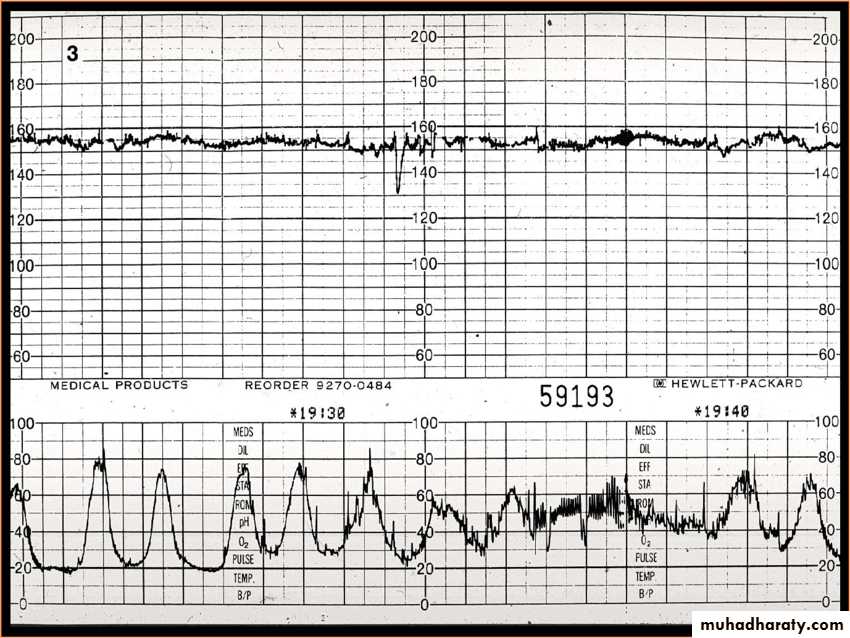
3. Absence of Variability :
variability is the most reliable sign of fetal well being . Is the normal irregular changes & fluctuations in the FHR around baseline rate , so the baseline rate should vary by at least ( 10 – 15 ) beats over a period of one minute , so the tracing appears as a jagged , rather than a smooth .- Factors affect variability
1. Hypoxia .2. Fetal infection .
3. drugs that suppress the CNS ( opoid , hypnotics )
4. extreme premature
5. Mg-sulfate use
6. Congenital heart block .
7. Fetal sleep (the baby sleeps in 20 – 40 minute cycles)
4.Absence of accelerations
Acceleration defined as a transient increase in heart rate of greater than 15 bpm for at least 15 seconds ( the 15 x 15 rule )Accelerations are a reassuring sign as they show fetal responsiveness & integrity of the mechanisms controlling the heart .
5.Decelerations : Transient fall in FHR > 15 beats lasting > 15 second .
Types of deceleration :
1.Early deceleration : Begins at or after the onset of a contraction & returns to the baseline rate by the time the contraction has finished & produces a mirror image of the contraction .- it not sign of fetal problem , It's due to vagal nerve stimulation .
2. Late decelerations : Are transitory reduction in FHR caused by utero-placenta insufficiency .
- Begins after the onset of the peak or middle of the contraction & ends after the contraction .
- The presence of late deceleration , justify secondary testing .
3.Variable decelerationIn which there is decrease in fetal heart rate not related to uterine contractions. - This results from direct myocardiac depression secondary to hypoxemia .
Normal CTG
Absent variability
Management of fetal heart rate pattern :
1- Early deceleration : The majority doesn’t fall below 100 bpm , usually is associated with uncomplicated labour , If falls < 100 bpm & is repetitive so pervaginal examination to exclude cord prolapse .
2- Late deceleration : If oxytocin in use so stopped .When the pattern has been corrected & after appropriate resolution , oxytocin may be restarted , start O2 5-6 L/min by tight-fitting O2 mask . , change position to left lateral position , increase rate of electrolytes containing fluid , assess fetal acid-base status by fetal stimulation test , if positive, so the pH is > 7.25 , or by fetal blood sampling ( for pH , lactate level )
Management of abnormal fetal heart
1. Stop oxytocin 2. O2 3. Lateral position .4. pervaginal examination to exclude cord prolapse and to determine the progress of labour .
5. If uterine activity excess, use tocolytic such as torbutaline or salbutamol.
6. If not corrected consider delivery .
Secondary Tests of fetal well-being
1. Vibroacoustic stimulation :An acceleration evoked by vibroacoustic stimulation immediately prior to scalp sampling was never associated with a pH of < 7.25 .
- It can reduce the need for scalp sampling by up to 50 % .
2. Fetal blood sampling :
- The lower limit of normal pH level is 7.20 .
- The base excess should also be measured to distinguish metabolic from respiratory acidosis .
- The amount of blood required is 25 microliter .
3. Scalp stimulation :
That fetuses that respond to scalp sampling with an acceleration almost always have an normal pH .
4. Fetal electrocardiogram : ( ECG )
5. Fetal pulse oximetry .