
1
ACUTE ST ELEVATION
MYOCARDIAL INFARCTION
(STEMI
)
By The End of This Lecture You Should Be
Able To
• Differentiate ACS from other acute chest pain emergency
conditions
• Diagnose STEMI using clinical, ECG, and biochemical tools
• Recognize the various steps of management of the patients
before and after reaching hospital
2
Objectives
• Appreciate the vital importance of time in the proper
management of STEMI
• Appreciate that STEMI is caused by complete obstruction of
a coronary artery by thrombus
• Understand that thrombus removal is the cornerstone of
management
• When the ECG shows ST elevation, attempts at reperfusion
should take priority over further investigations

Clinical Scenario 1
• A 60-year-old man with Hx of diabetes, hypertension, and
smoking is brought to the emergency room by his family
because of severe chest pain
What Conditions Cause Acute chest pain?
• ACS (STEMI, NSTEMI)
• Aortic dissection
• Acute pericarditis
• Pulmonary embolism and infarction
• Pneumothorax
• Extracardiac causes: esophageal spasm, visceral obstruction
or perforation, musculo-skeletal chest pain
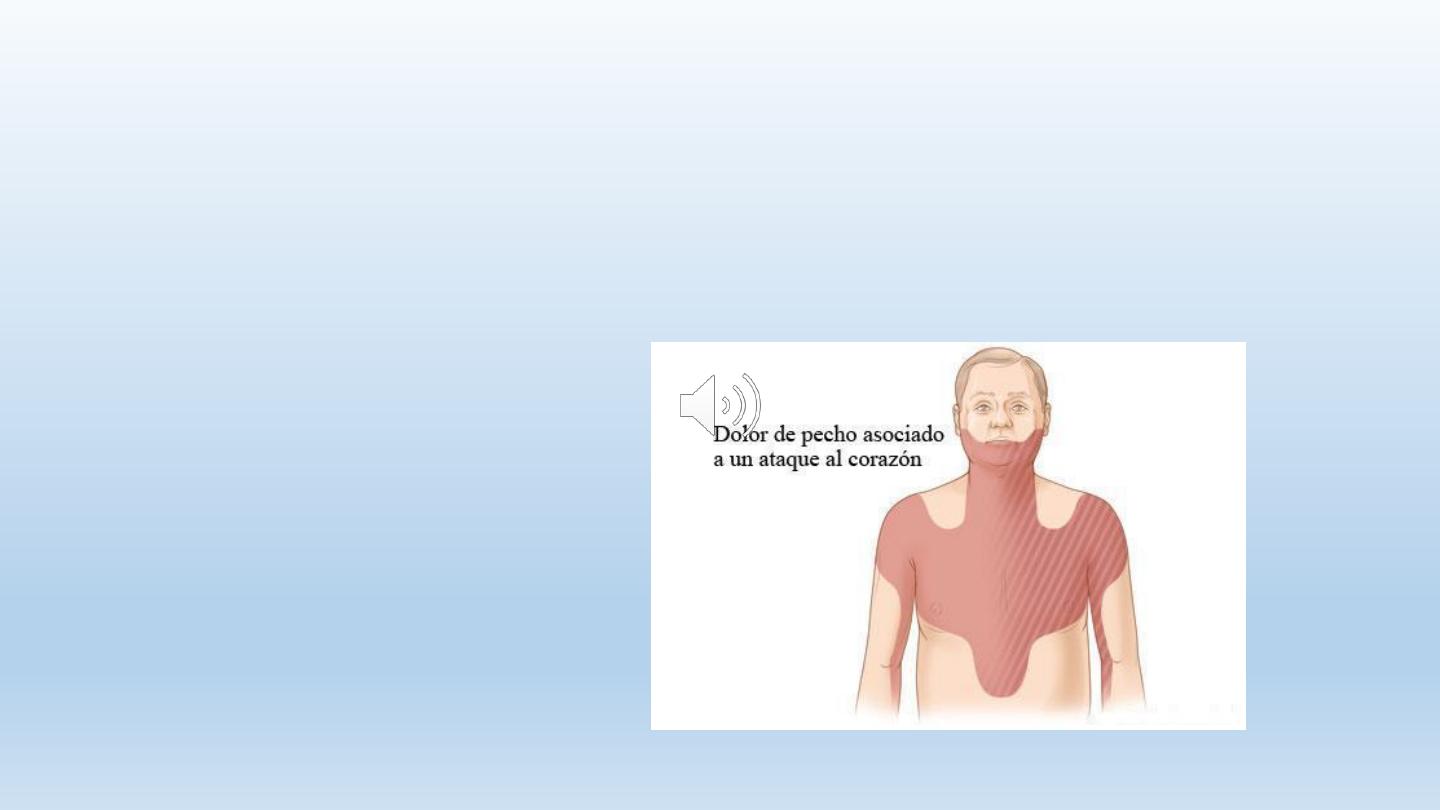
Clinical Presentation of ACS, including STEMI
Pain:
• Chest, back, shoulder, epigastrium, neck, throat, mandible,
arms, hands
• Prolonged
• Severe
• Not relieved!
7
ACS (STEMI): Clinical features
Other features
• Severe anxiety
• Nausea and vomiting
• Breathlessness
• Collapse
• Syncope

8
STEMI: PHYSICAL SIGNS
• Signs of sympathetic activation:
• Pallor
• Sweating
• Tach
ycardia
• Signs of vagal activation
• Vomiting
• B
radycardia

9
STEMI: PHYSICAL SIGNS
• Signs of impaired myocardial function
• Hypotension, oliguria, cold sweat
• Narrow pulse pressure
• Raised JVP
• S3
• Faint S1
• Diffuse apical impulse
• Lung
crepitations
10
STEMI: DIFFERENTIAL Dx
• Aortic dissection:
• Pain is abrupt & severe from the onset, tearing in nature, more in
the back
• Pulmonary embolism
• Dyspnea, tachypnea, tachycardia, hypotension
• Acute pericarditis:
• Important to differentiate, as thrombolytic therapy may cause
cardiac tamponade
• Pain is sharp, related to breathing , posture and swallowing
• Pericardial friction rub
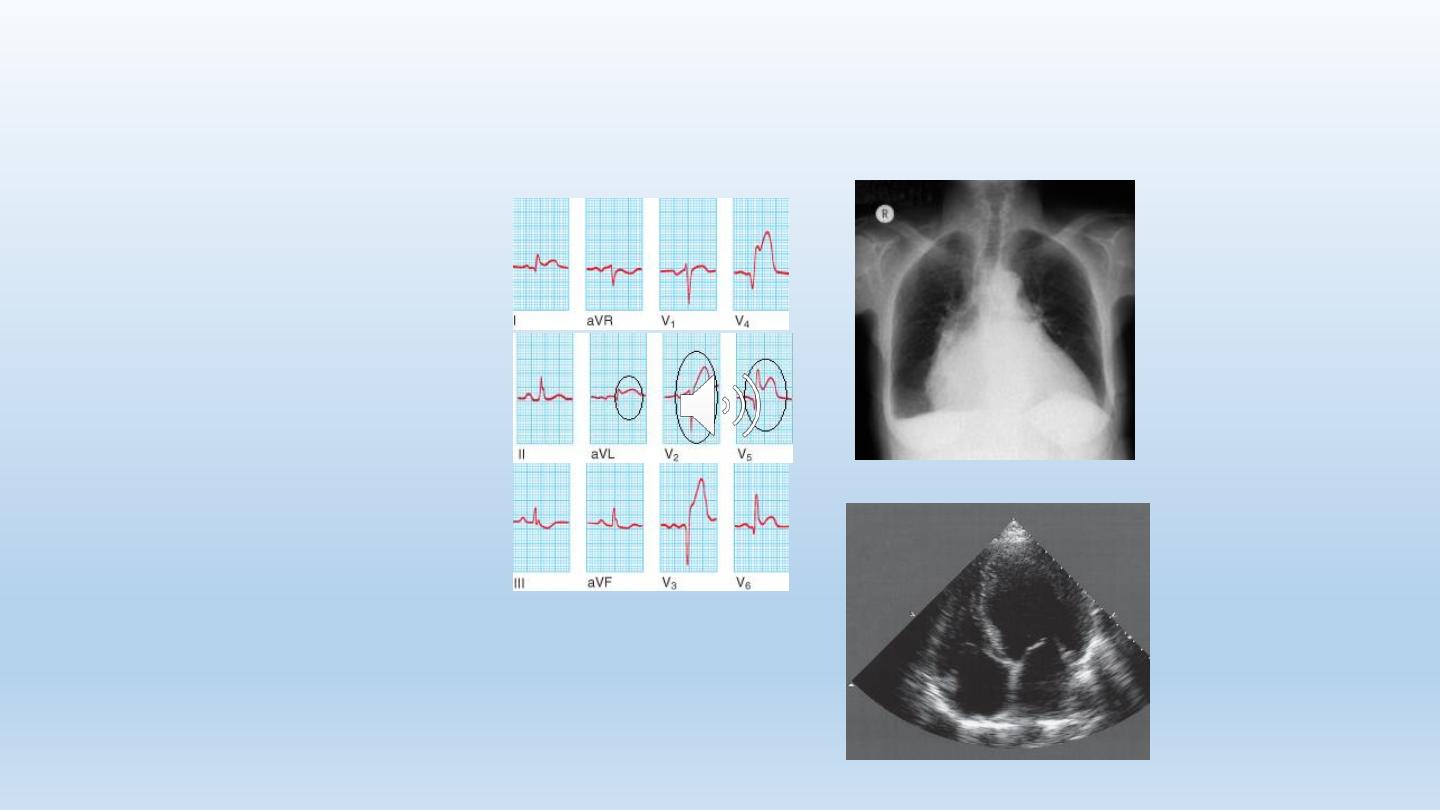
STEMI: Diagnosis & Basic Investigations
• Clinical presentation
• ECG
• Troponin (indicating myocardial cell injury)
• Enzymes indicating myocardial cell necrosis: CPK, AST,
LDH
STEMI Diagnosis, additional investigations
• Echocardiography
• CXR
• Blood tests: WBC, ESR

Tetrad of Diagnosis
•Chest pain
•Classical ECG showing ST elevation
•Raised troponin
•Raised markers of myocardial cell necrosis
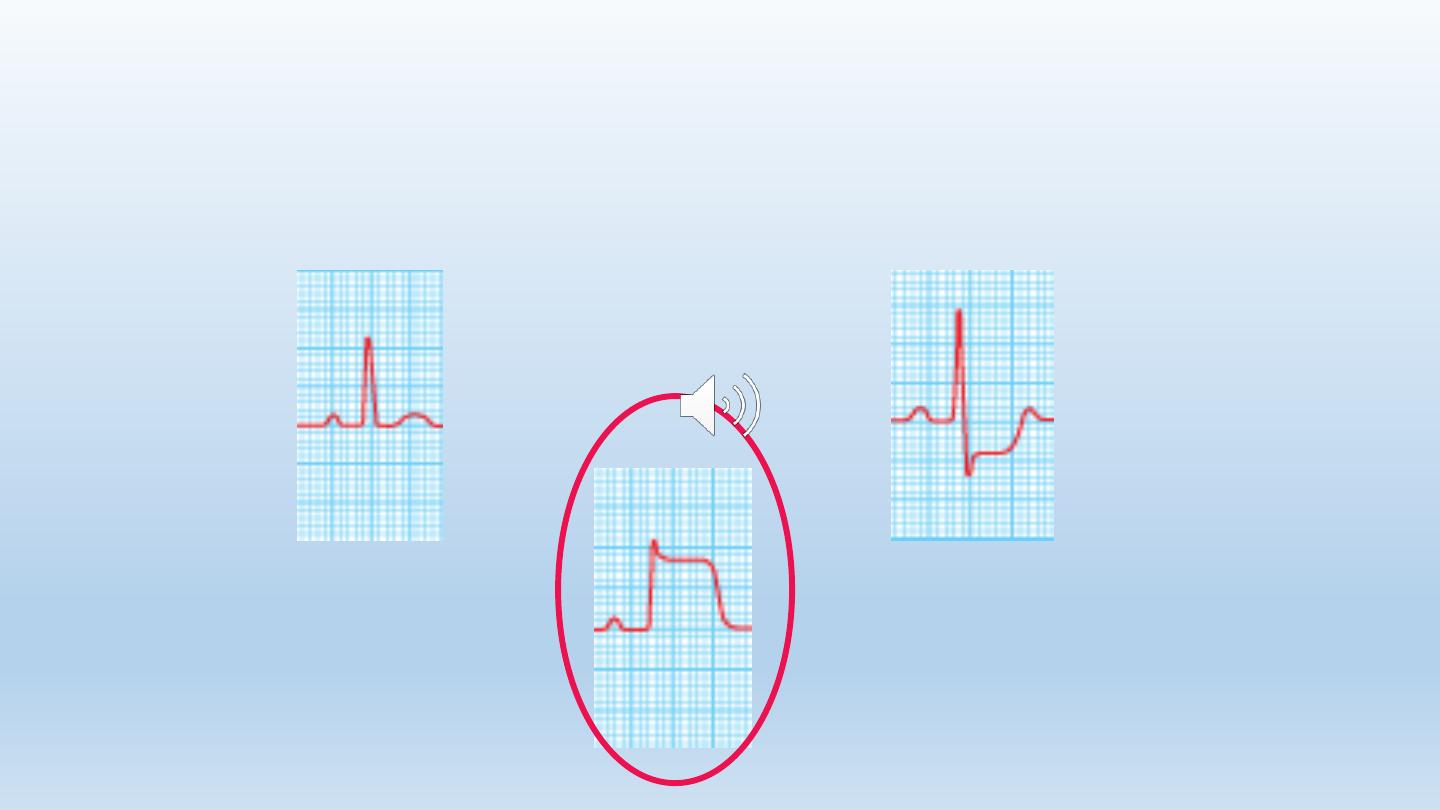
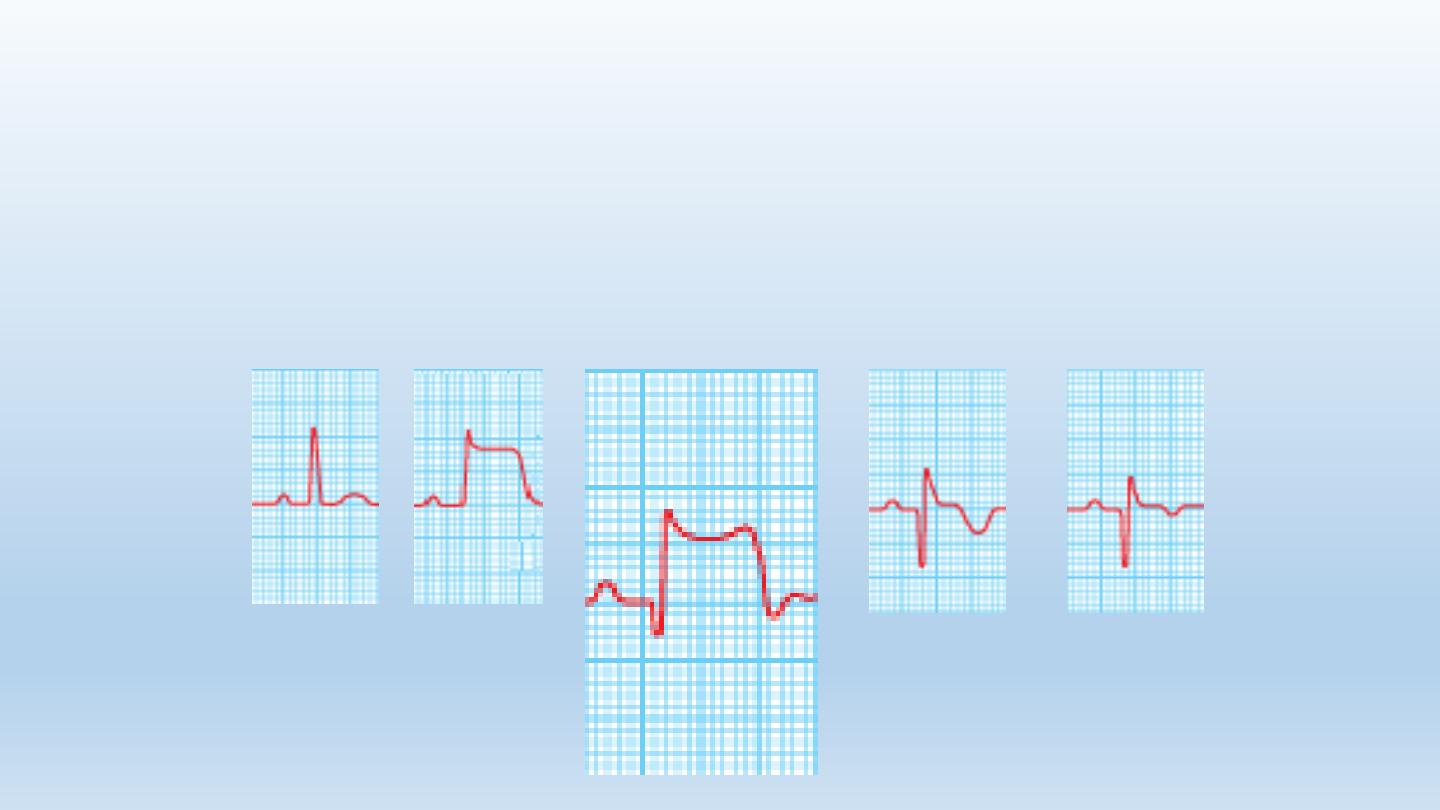
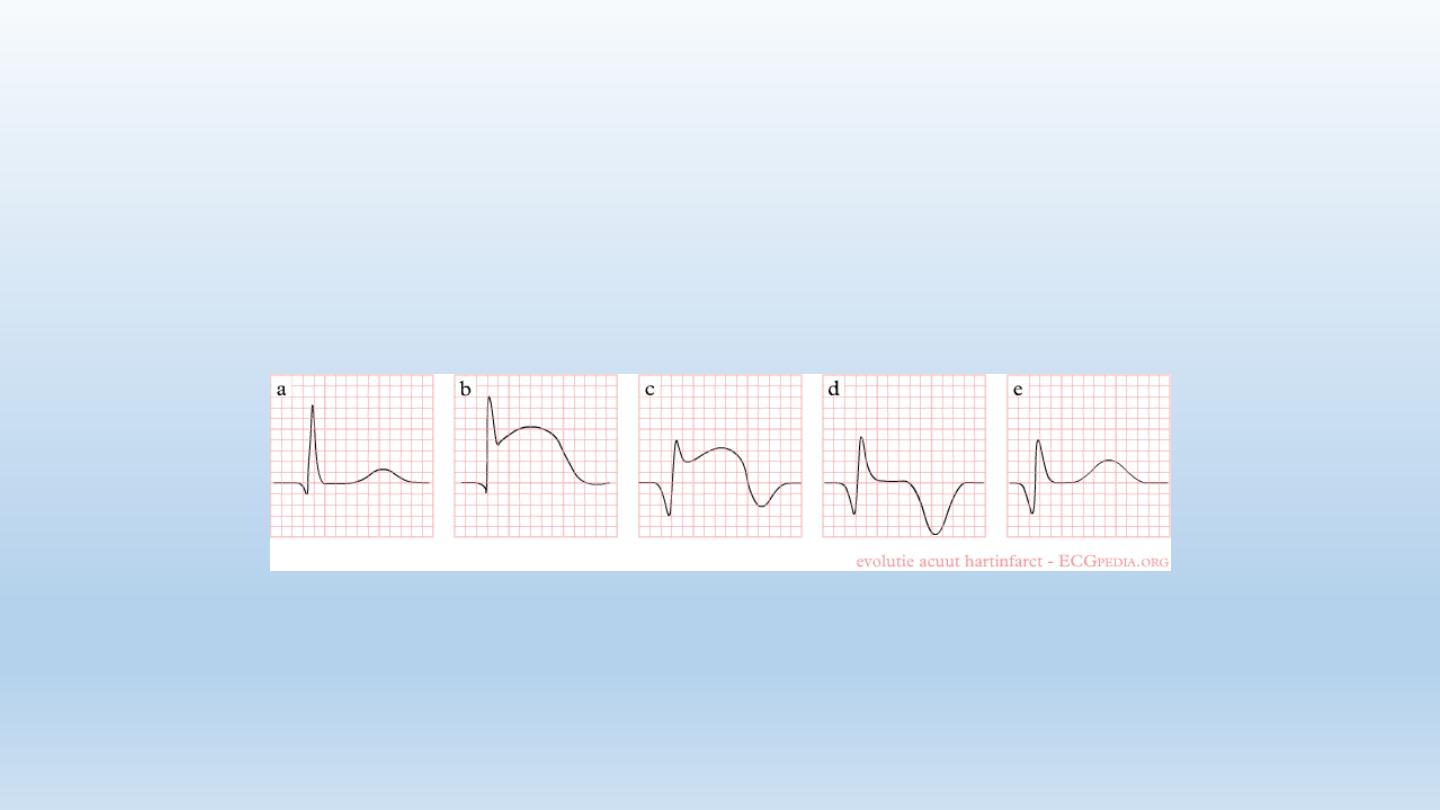
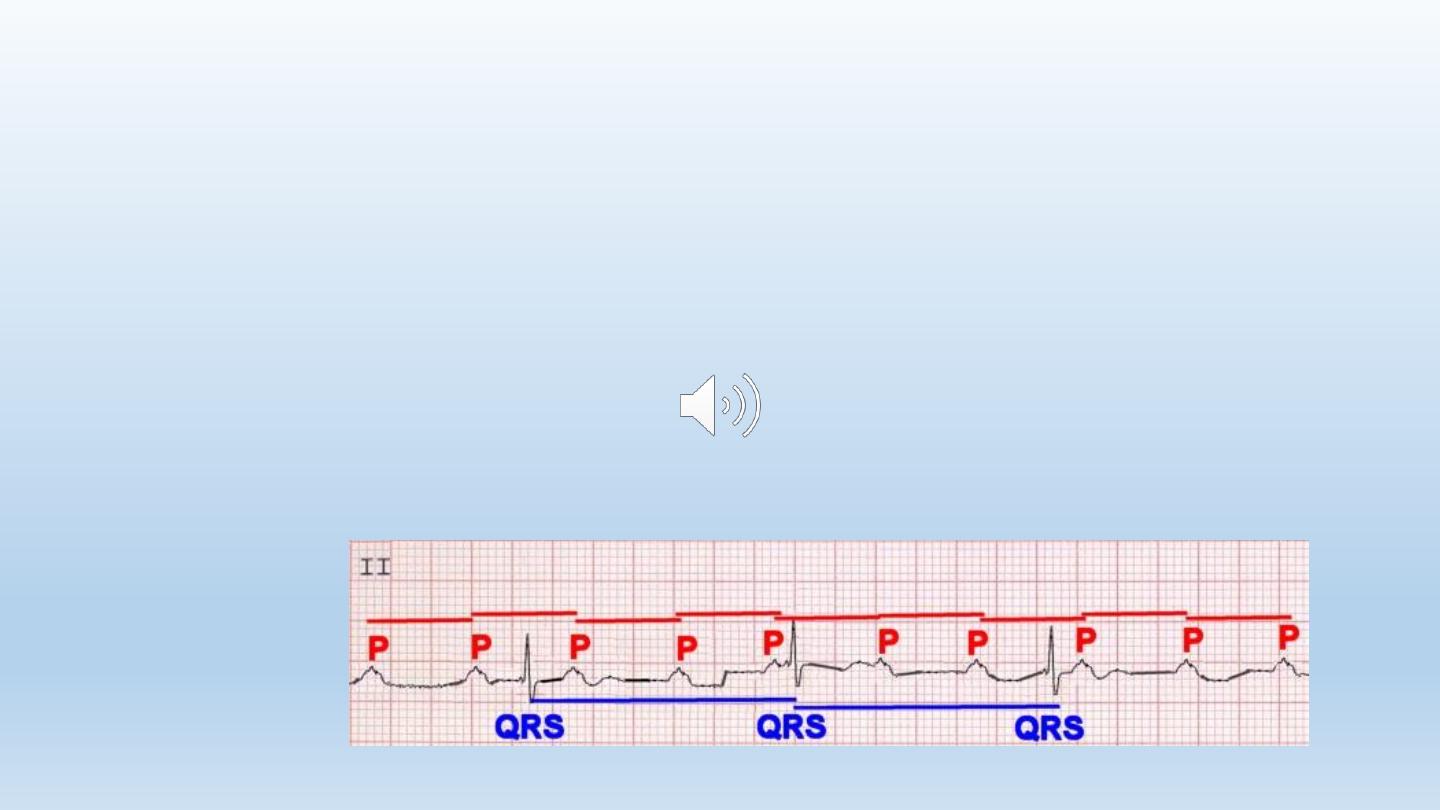
The ECG in STEMI
Sequence of changes in STEMI:
1. Tented, peaked T waves
2. Acute ST elevation (the current of injury)
3. Loss of amplitude of the R wave
4. Development of a Q wave
5. T wave inversion
6. Reduction in the magnitude of the ST elevation (ST resolution)
7. Deepening of Q waves
The ECG in STEMI
• Hyperacute T waves
16
STEMI: ECG
• ST segment elevation: the earliest ECG change
STEMI
normal
angina
17
STEMI: ECG
• Next: reduction of R wave amplitude, appearance of Q
waves, T inversion
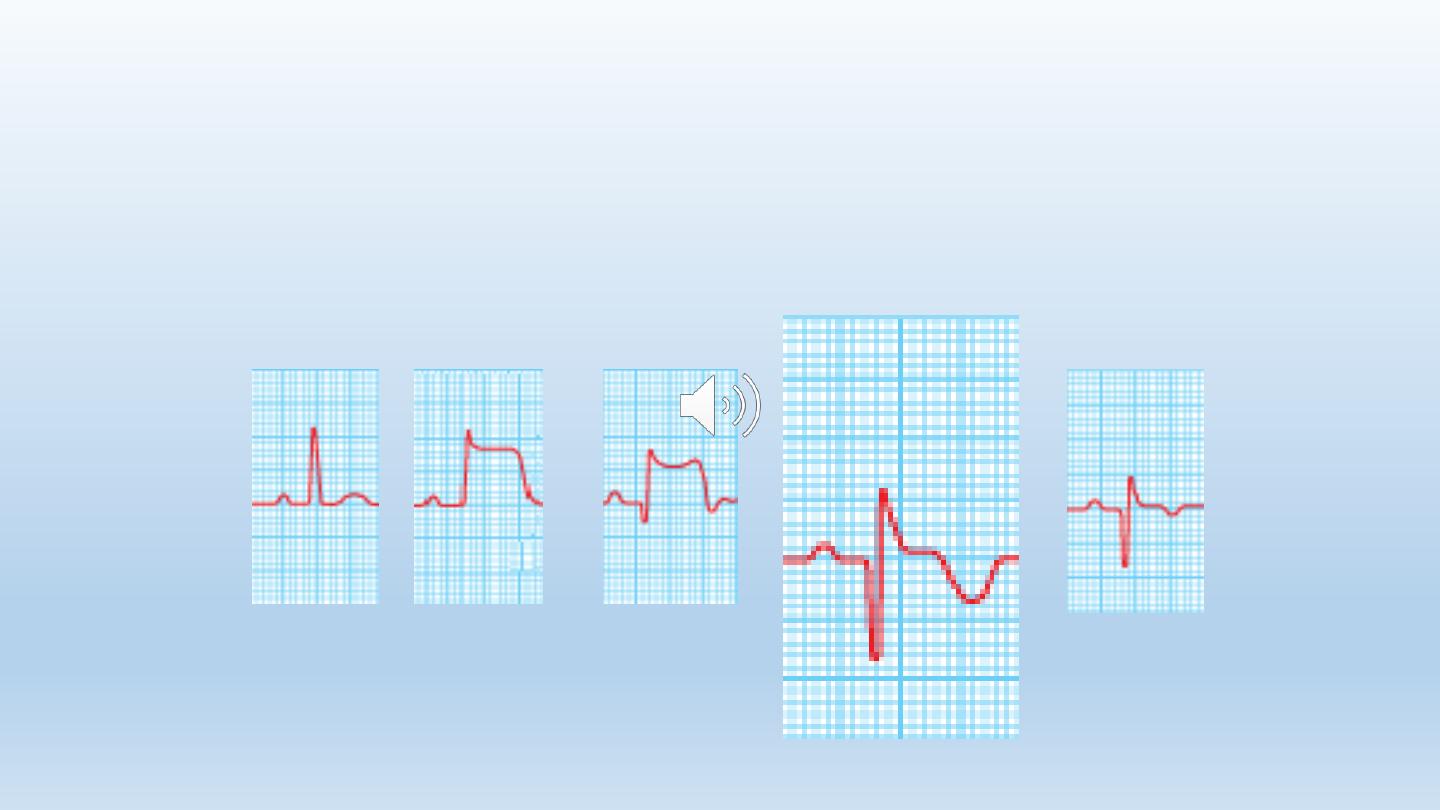
18
STEMI: ECG
• Then: deepening of Q waves, T inversion & resolution of ST
segment
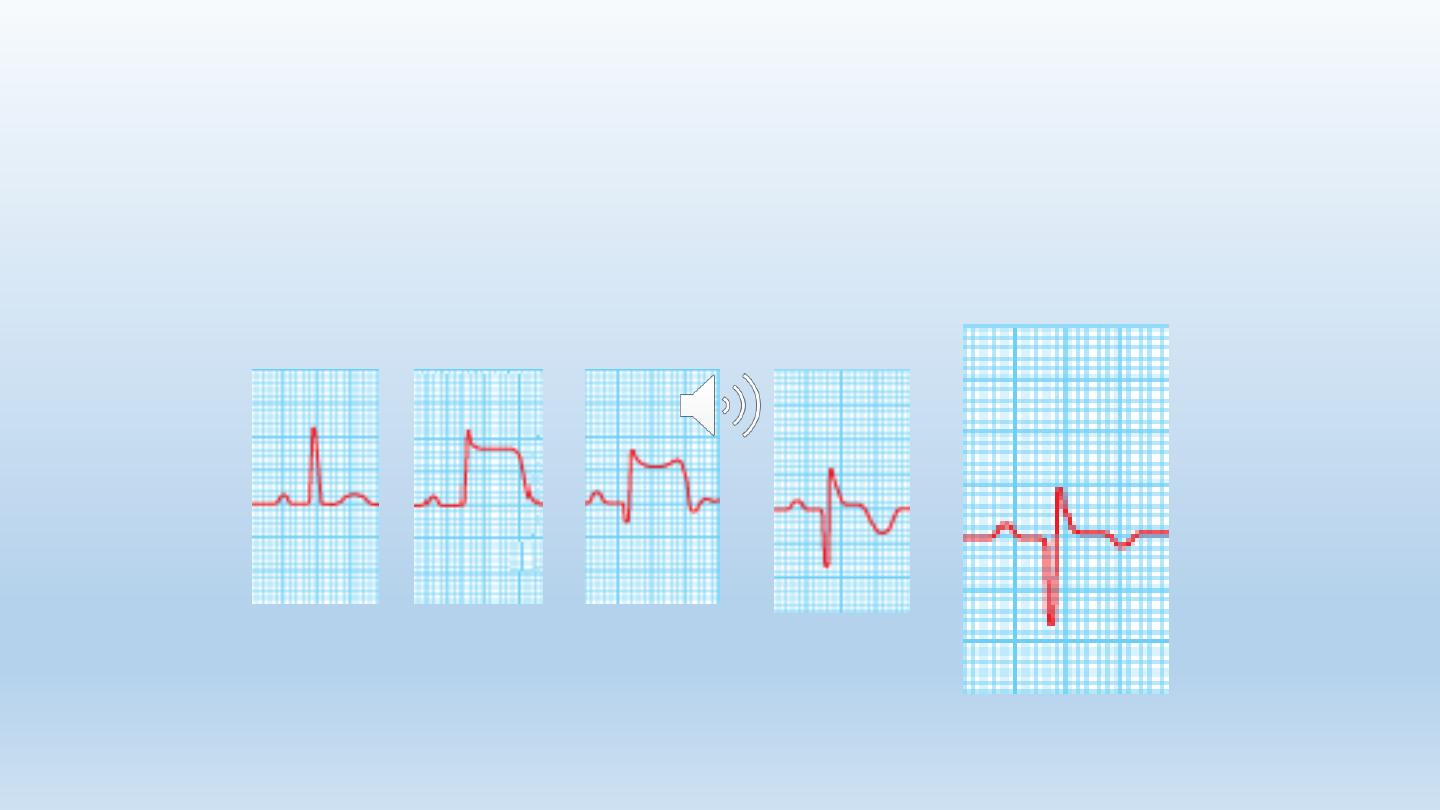
19
STEMI: ECG
• 12 weeks after MI, the ST segment returns completely to
normal
20
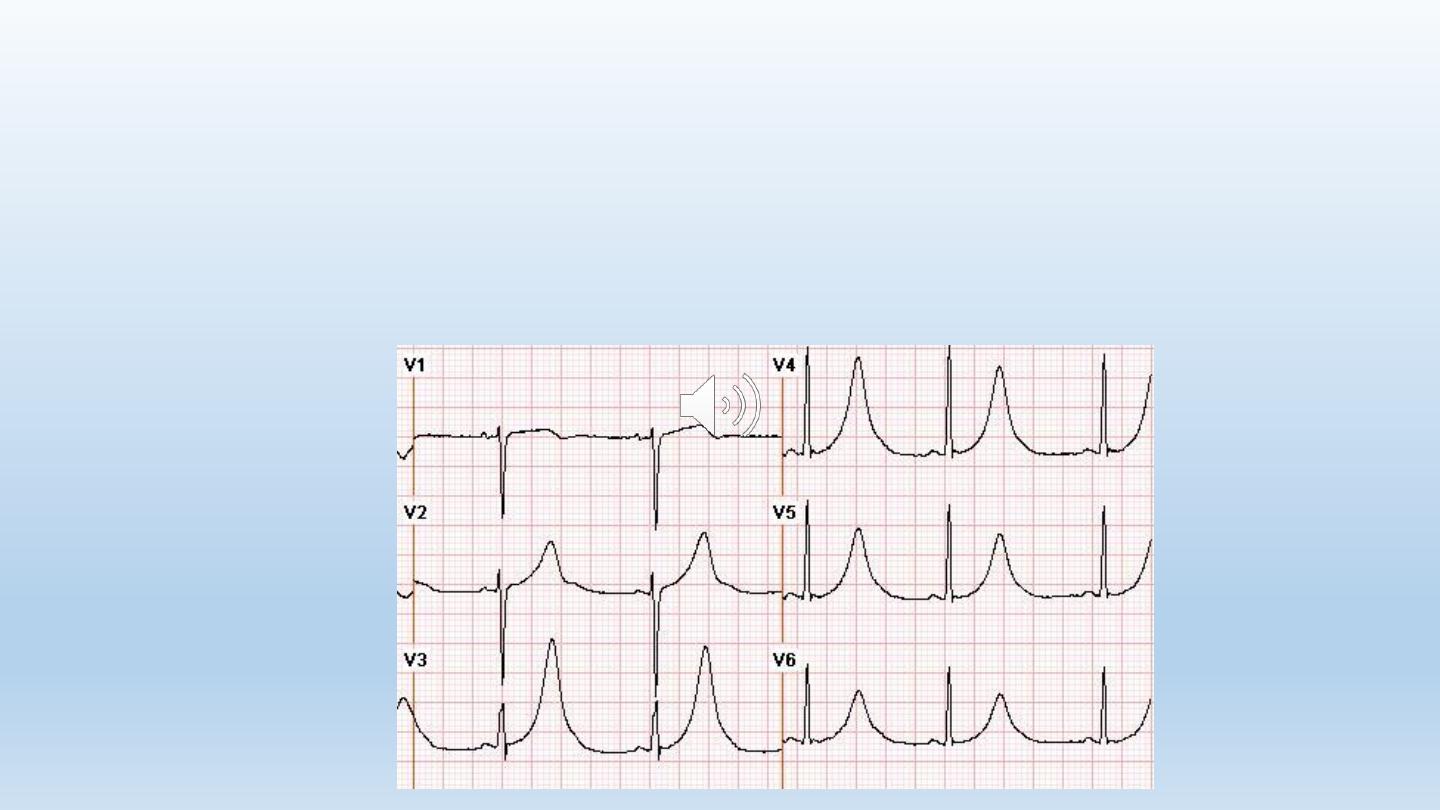
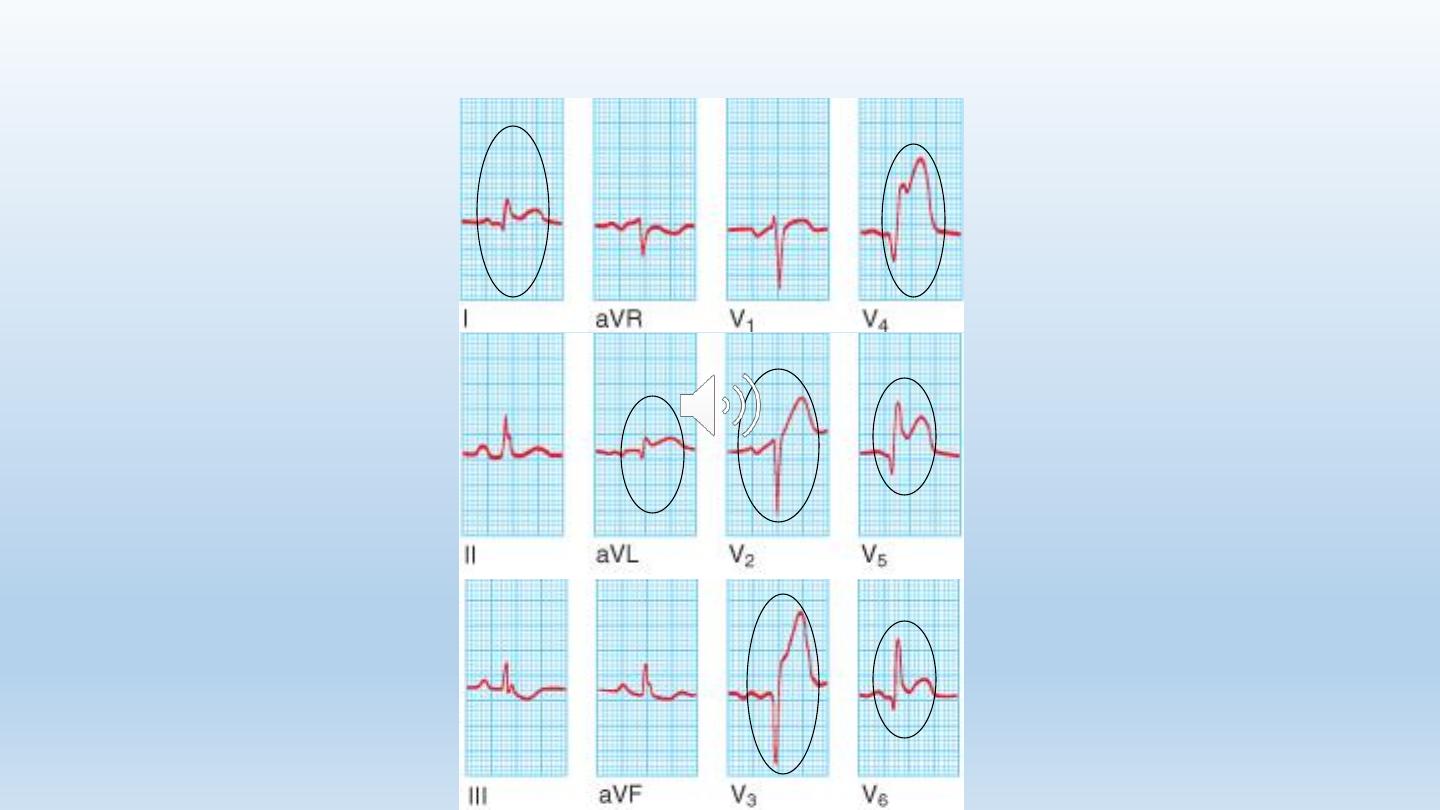
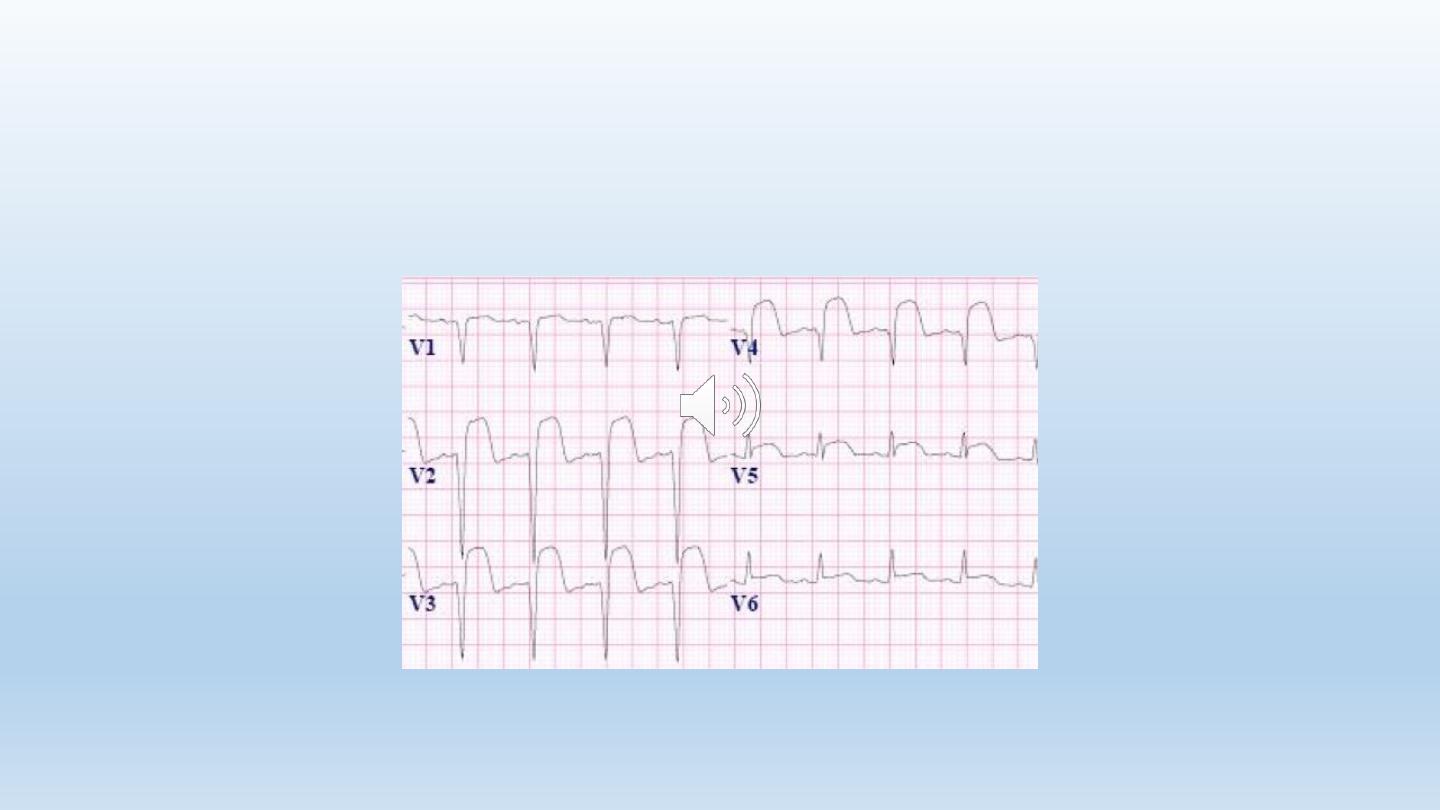
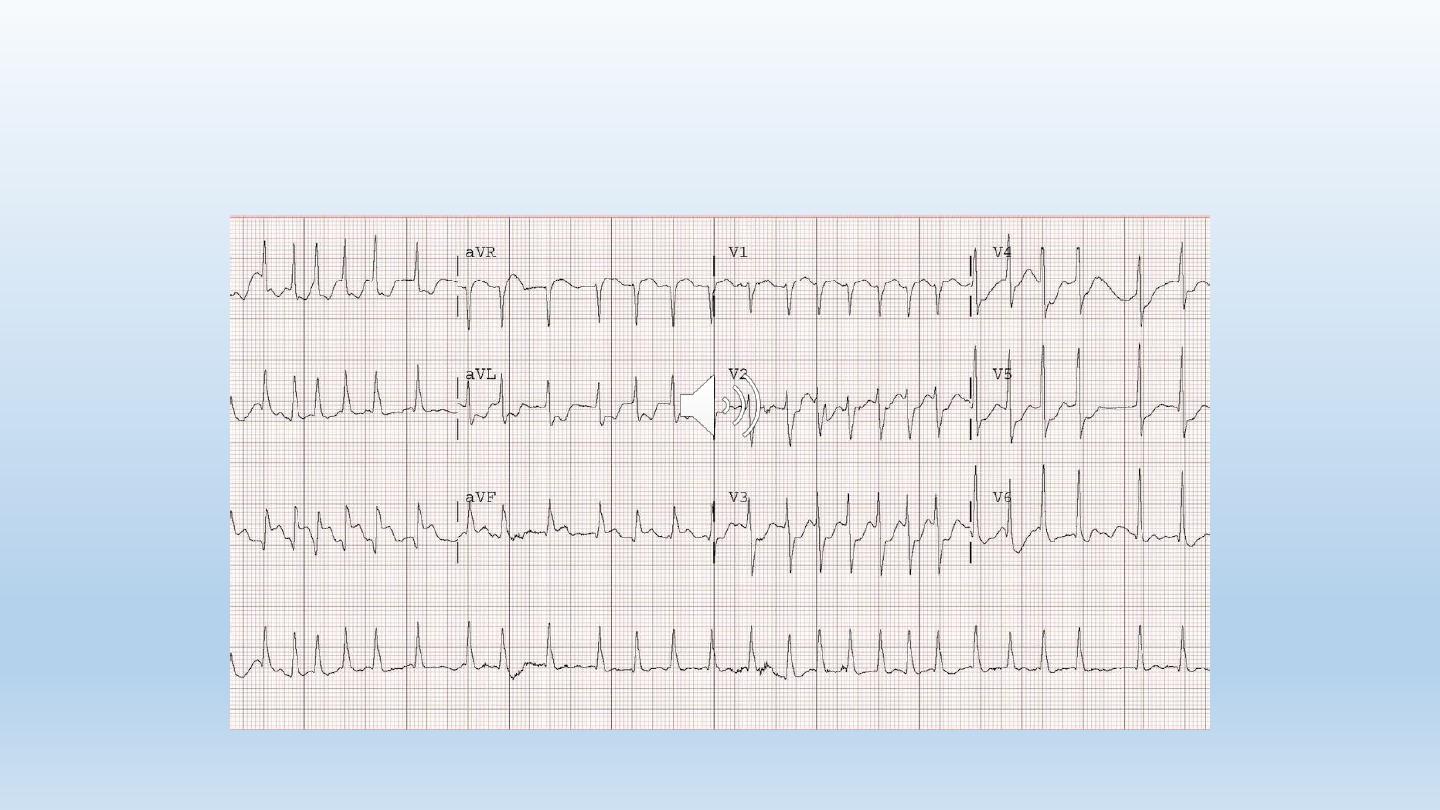
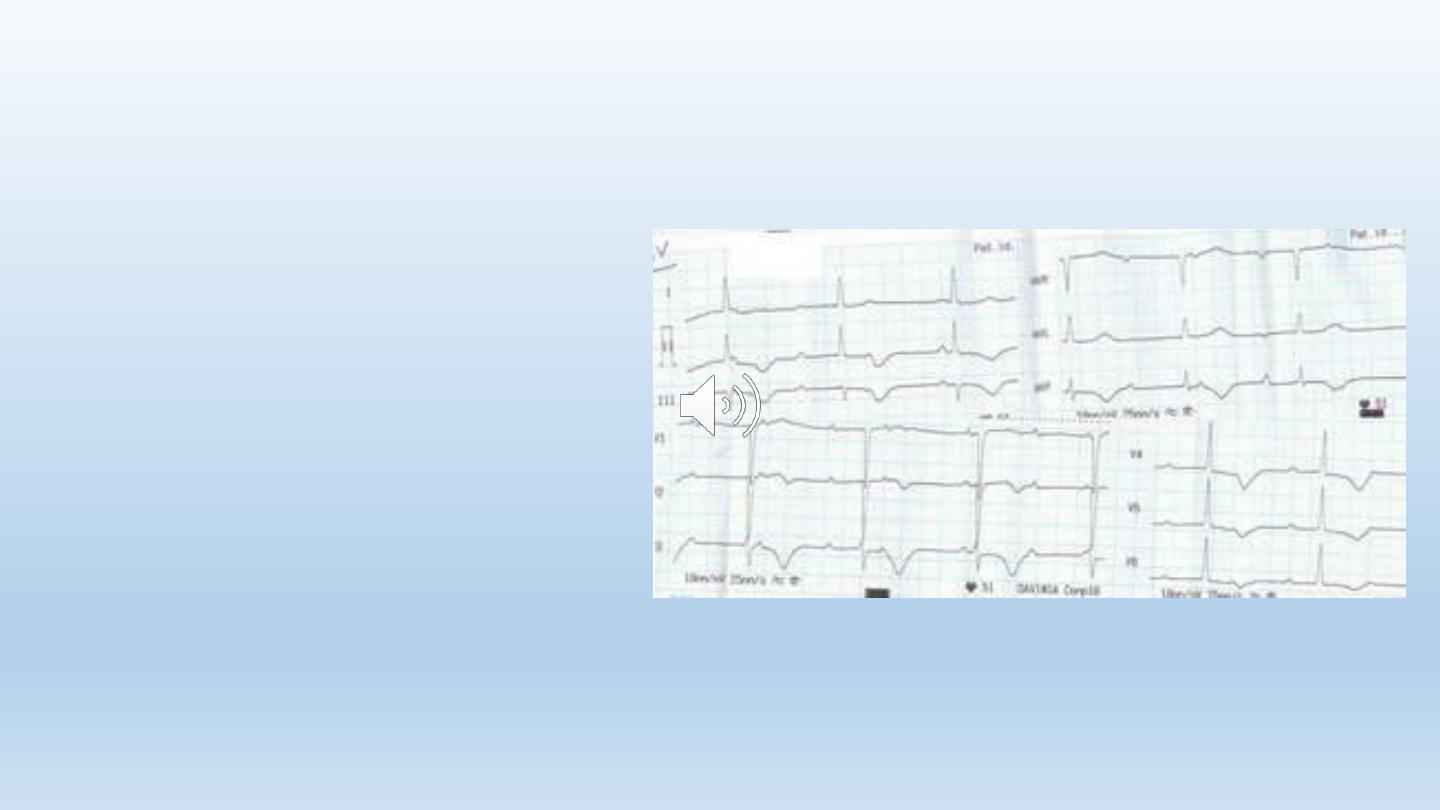
Acute Anterior MI
21
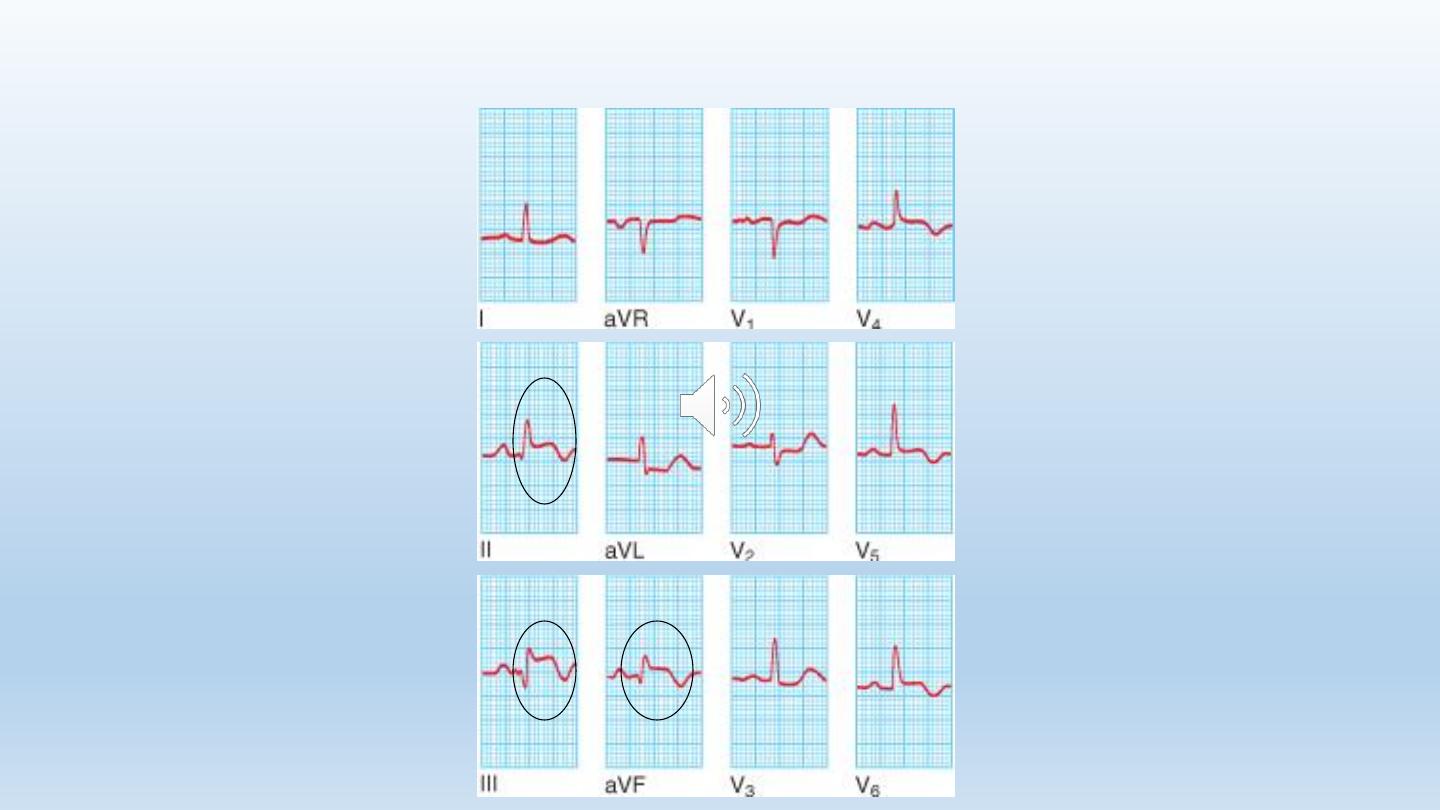
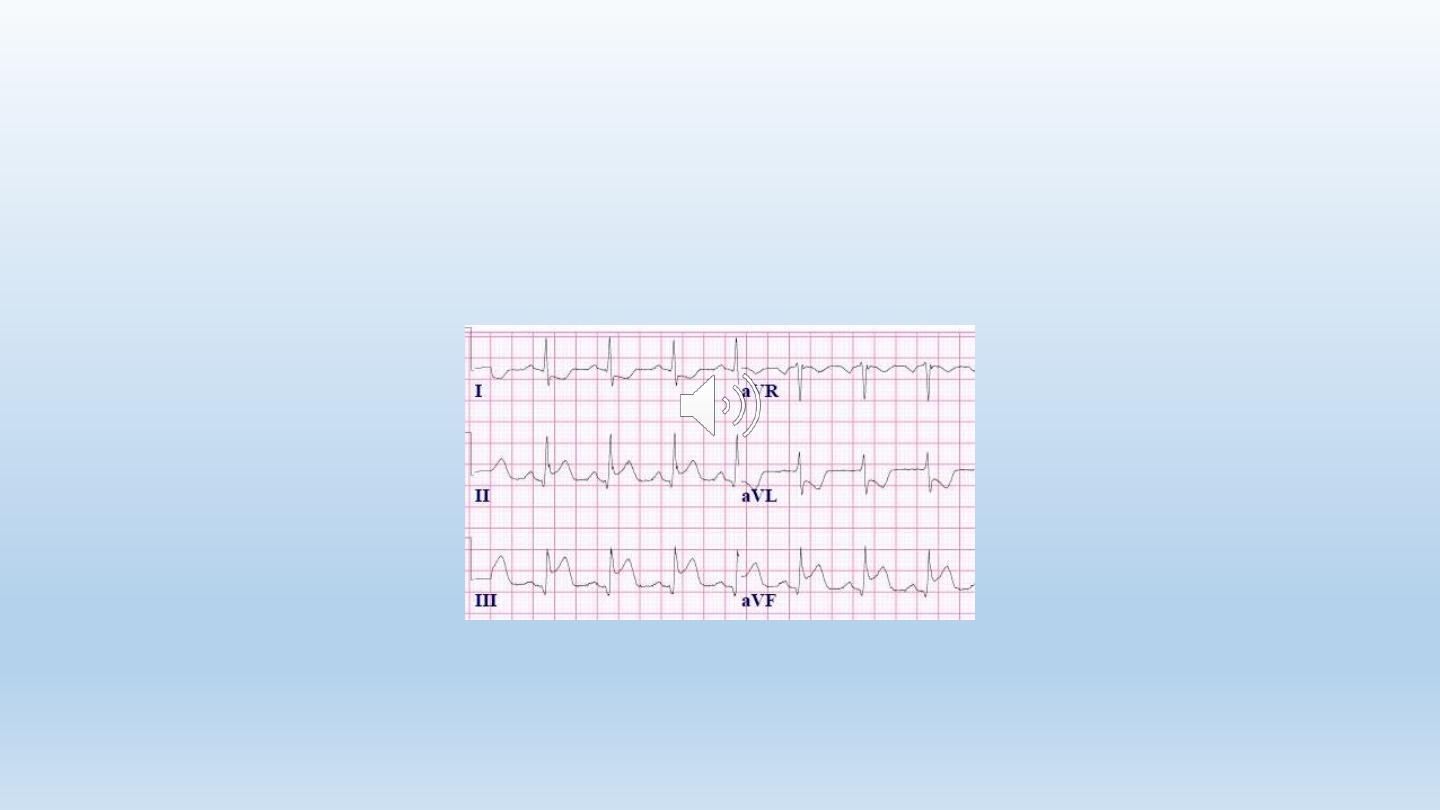
Acute inferior MI

STEMI Diagnosis:
Biochemical markers
26
Biochemical markers
• Troponin T (Tn T)
• Troponin I (Tn I)
• Creatinine Kinase (CK)
• Creatinine kinase MB (CK-MB)
• Others: AST, LDH
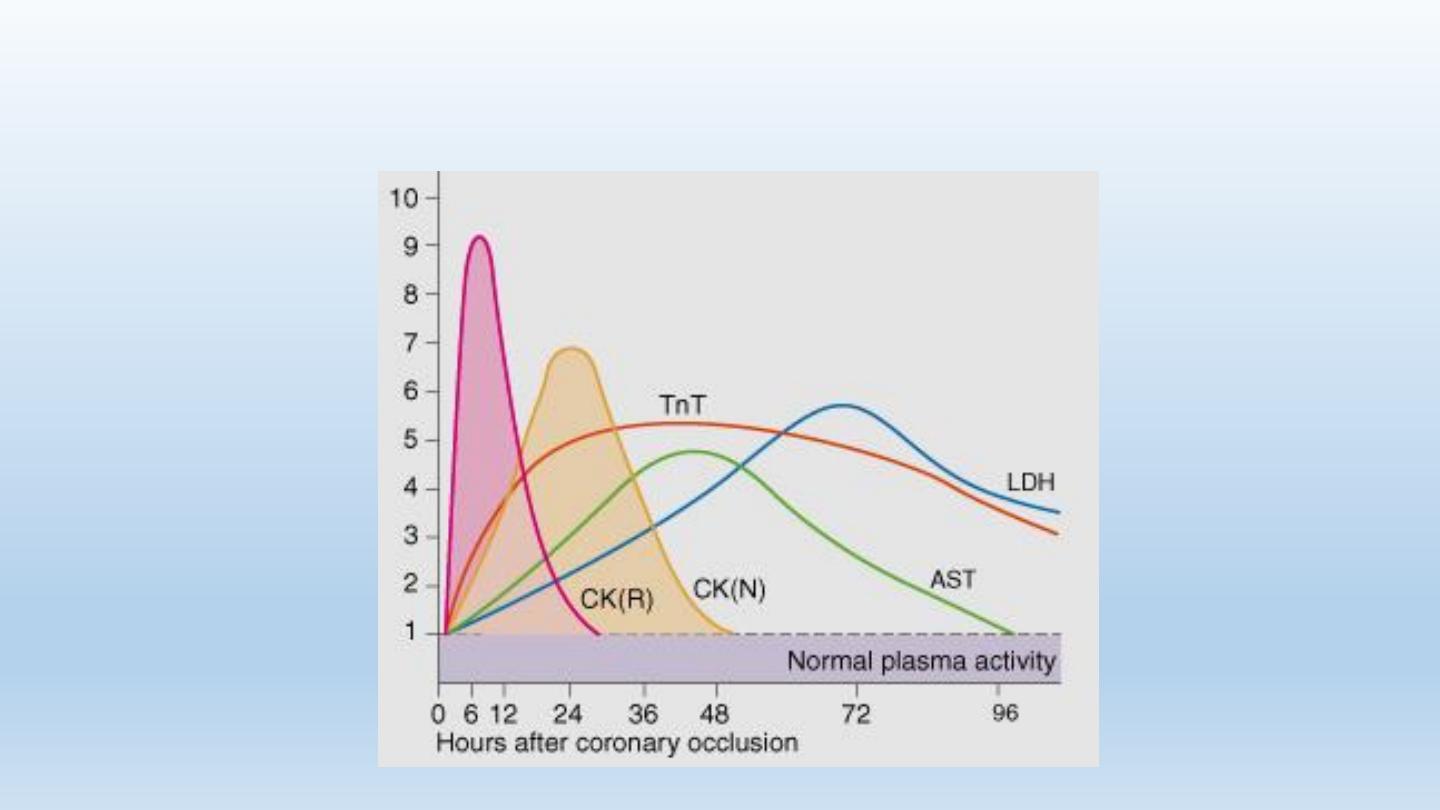
27
Biochemical Markers
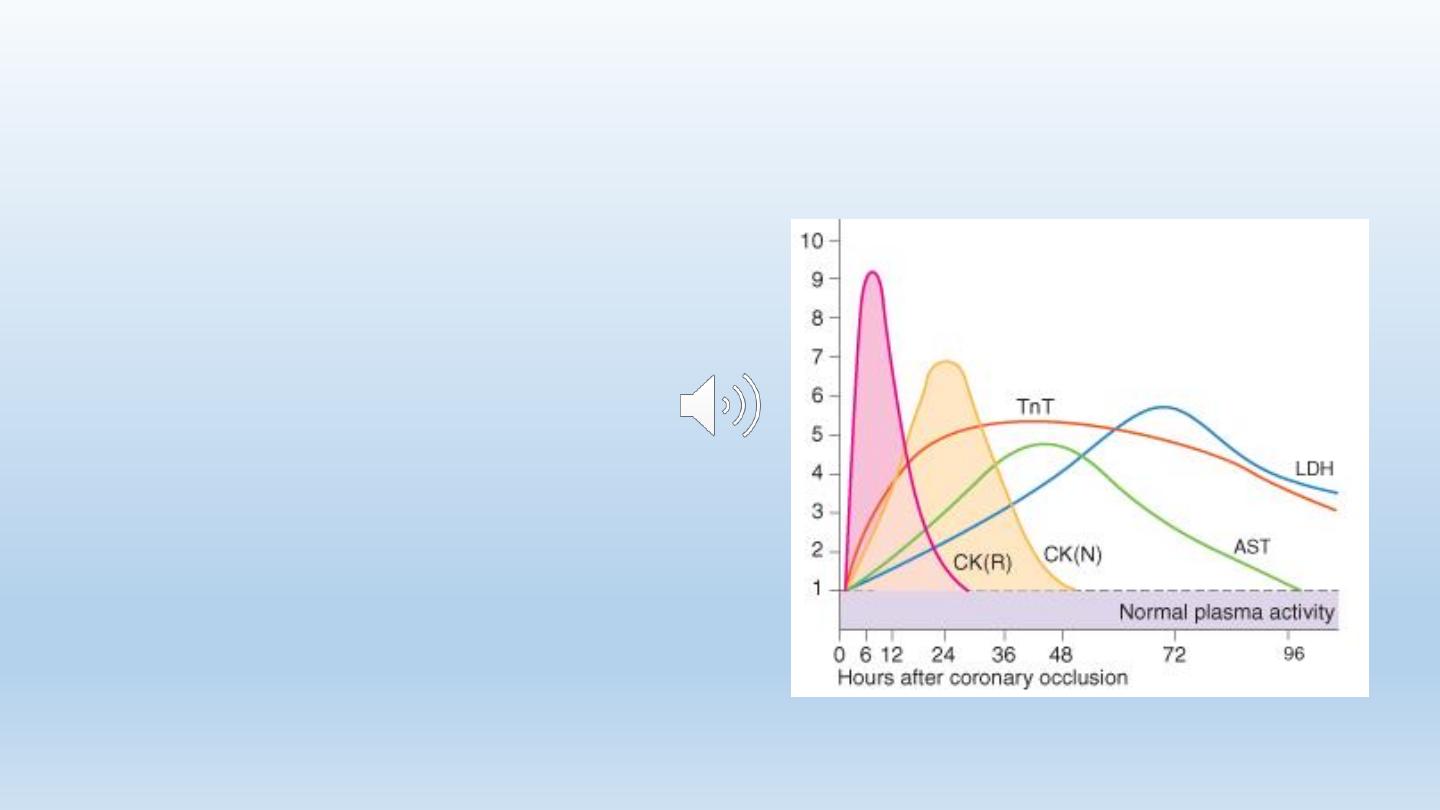
28
Biochemical Markers: Troponins
cTn-T & cTn-I:
• More specific than CK & CK-
MB
• Start to rise in 4-6 hours
• Persist in the circulation for 2
weeks
• Troponins are elevated in
unstable angina but to less
severe degree.
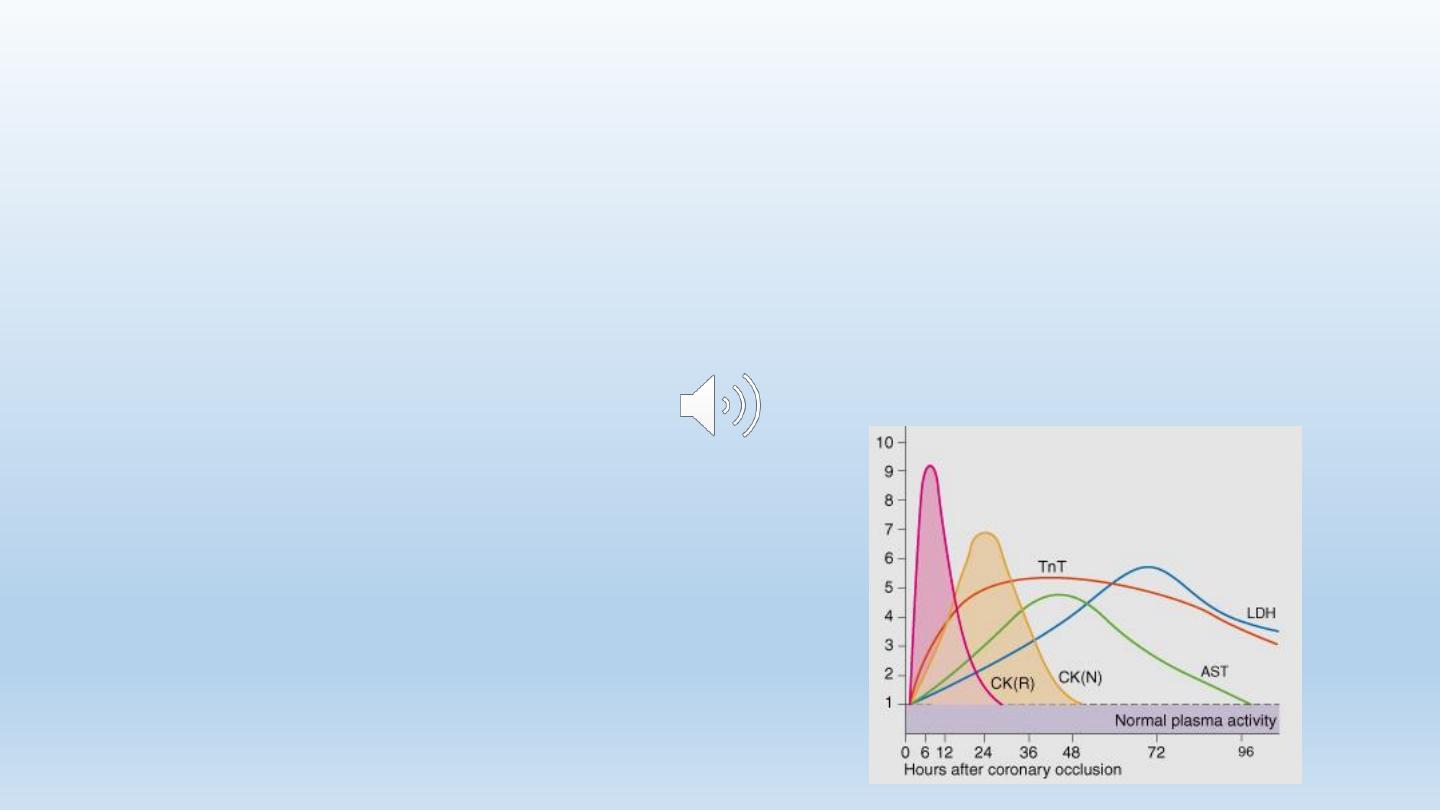
29
Biochemical Markers
CK (creatinine kinase):
• Found in skeletal muscles (MM isoenzyme), in the brain (BB
isoenzyme) and in the myocardium (MB isozyme)
• Starts to rise at 4-6 hours,
peaks at 12 hrs, and
disappears in 36-48 hrs
30
Biochemical Markers
CK is not specific for cardiac muscle, it may rise in
• Intramuscular injection
• Physical exercise
• Defibrillation
CK-MB is more specific and sensitive for cardiac muscle
injury
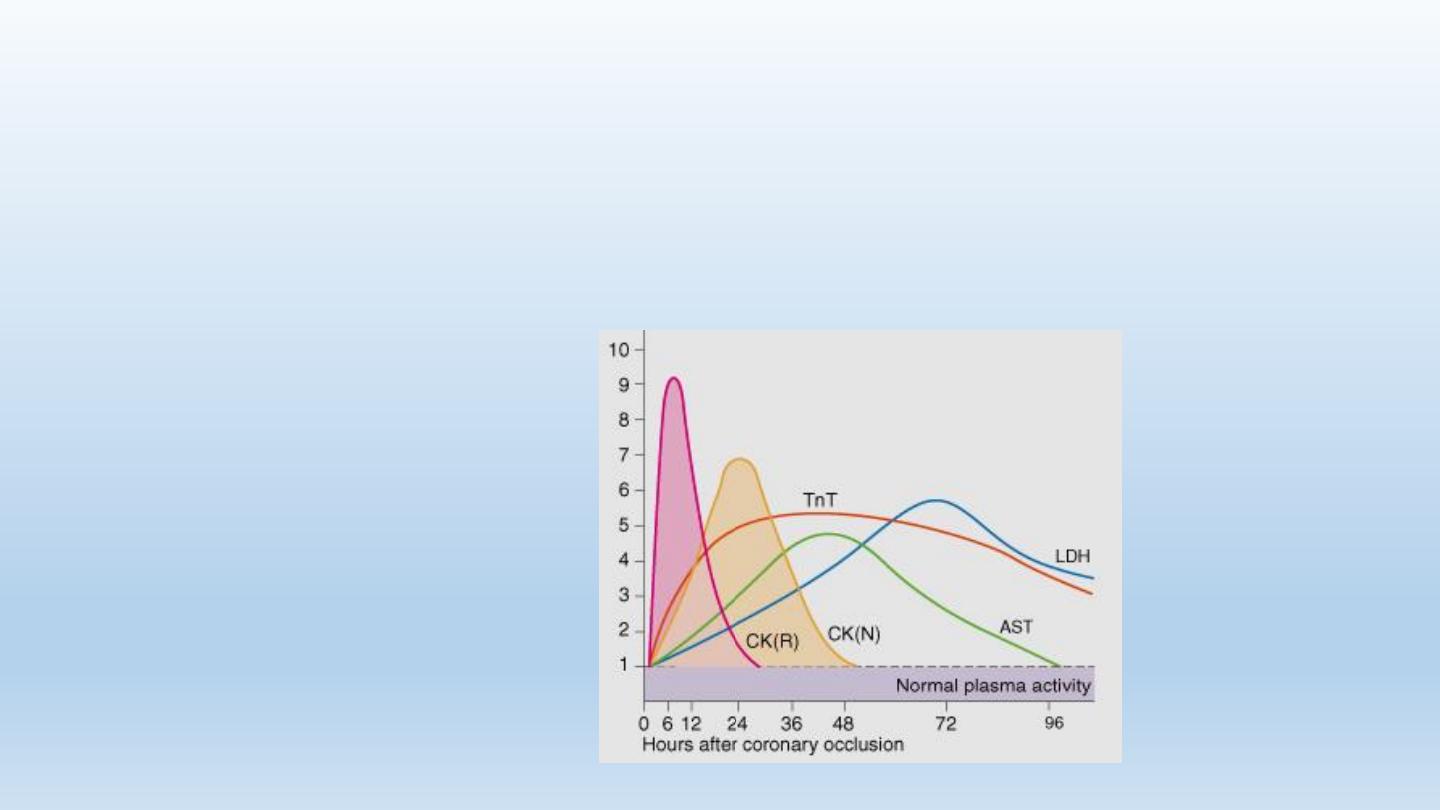
31
Biochemical Markers
CK-MB is not elevated with the administration of DC shock or
skeletal muscle injury.
Further Testing?
• If the ECG shows ST elevation, time should be
reserved for immediate management!
• Other investigations should be done after reperfusion
therapy
33
Other Blood Tests
• Leukocytosis:
• Neutrophilia
• Reaches a peak on the first day
• Correlates
with the extent of myocardial damage, i.e. with prognosis
• Erythrocyte Sedimentation Rate (ESR)
• C-Reactive Protein (CRP)
34
Chest X-Ray
• Pulmonary edema
• Heart size:
• Usually normal
• Cardiomegaly
due to old myocardial infarctions

35
Echocardiography
• Usually done after reperfusion therapy
• Can be performed at the bedside
• Useful to assess the status of the LV & RV
• Detects mechanical complications
• LV mural thrombus
• Ventricular septal rutpture
• Mitral regurgitation
• Pericardial effusion
• RV infarction
Clinical Scenario 2
• A 70-year-old man suffers severe chest pain with sweating
and severe weakness while at rest.

This patient Probably
Sustained ACS (Infarction,
Heart Attack)
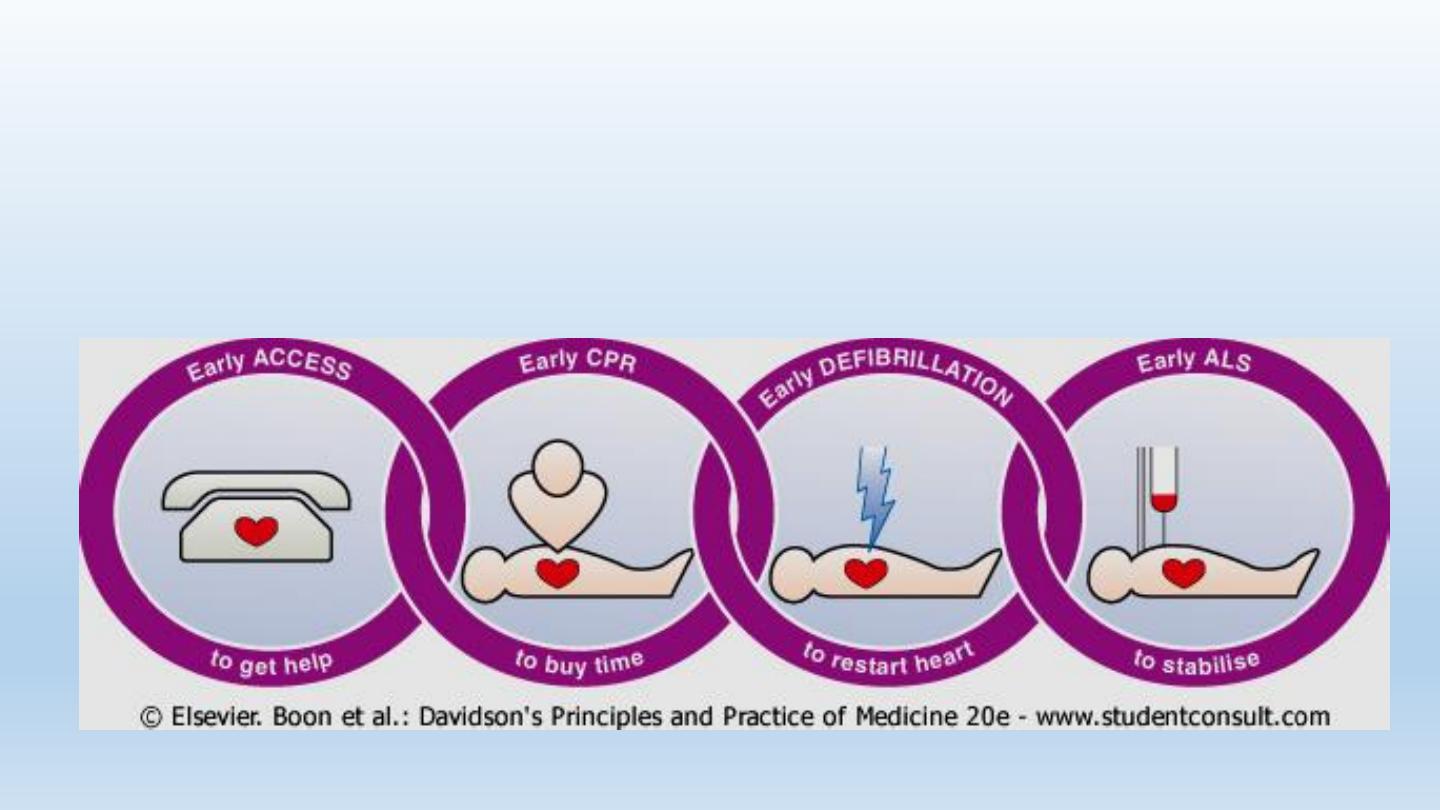
Immediate (Prehospital) management
• DO NOT PANIC!
• Call for help, ambulance
• Transfer to a safe place,
remove tight clothes,
administer sublingual
angised if available…..

Immediate (Prehospital) management
• Observe pulse, BP (if
possible) and level of
consciousness
• Transfer to hospital as
soon as possible
• What is the immediate danger to the patient?
What is the imminent danger to this patient?
Acute cardiovascular collapse & death, caused by
• Arrhythmia (VF)
• Cardiac standstill
• Patient becomes pulseless and unconscious

Immediate (Prehospital) management: CPR
• In case patient becomes pulseless and unresponsive:
administer CPR (cardio-pulmonary rescuscitation)

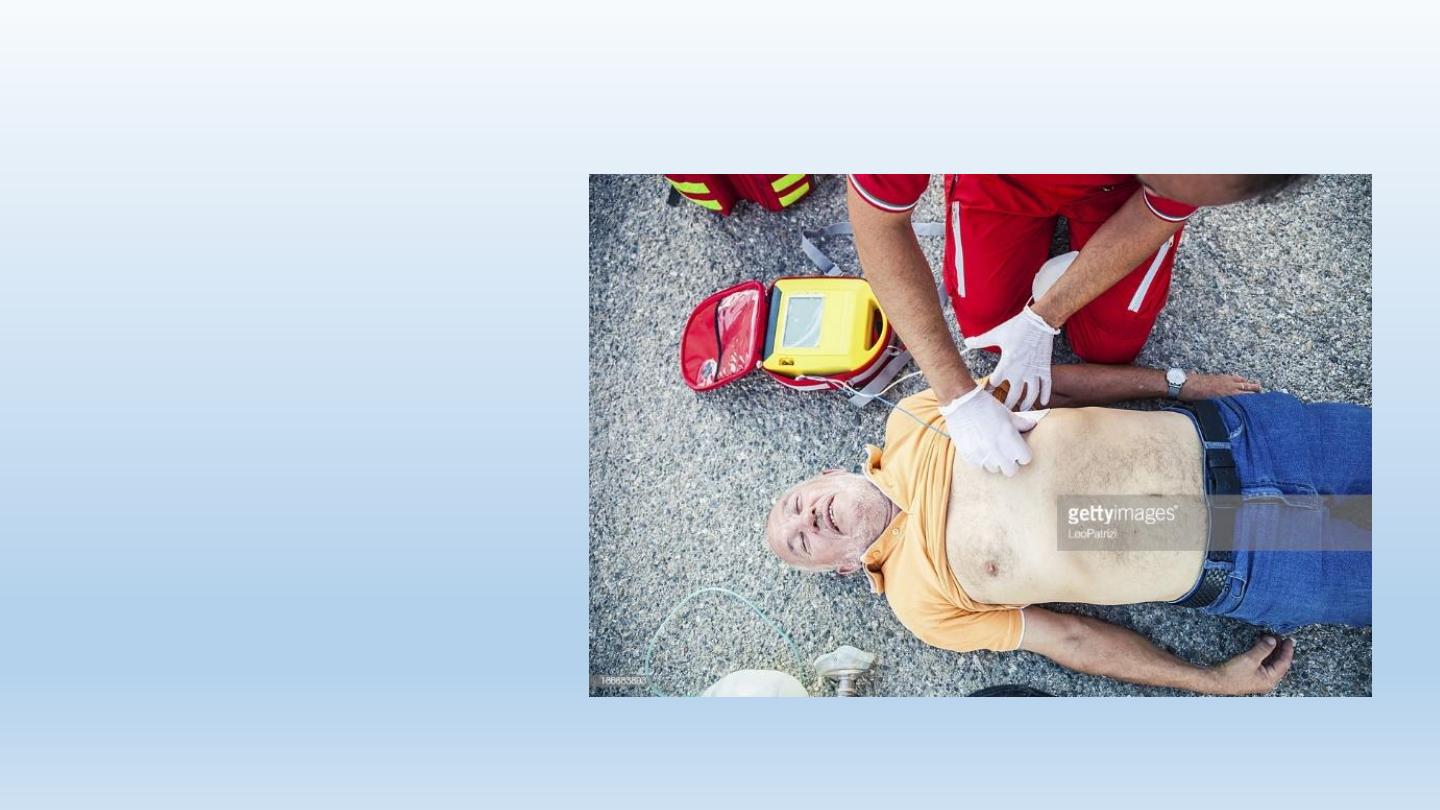
Immediate (Prehospital) management
AED: automatic
external Defibrillator:
If available, give DC
shock, continue CPR
until restoration of
pulse, repeat DC if
necessary
46
Prehospital management
• Advanced Life Support (ALS)

47
Transferring The Patient
• Rapid transfer of the patient to hospital: ambulance
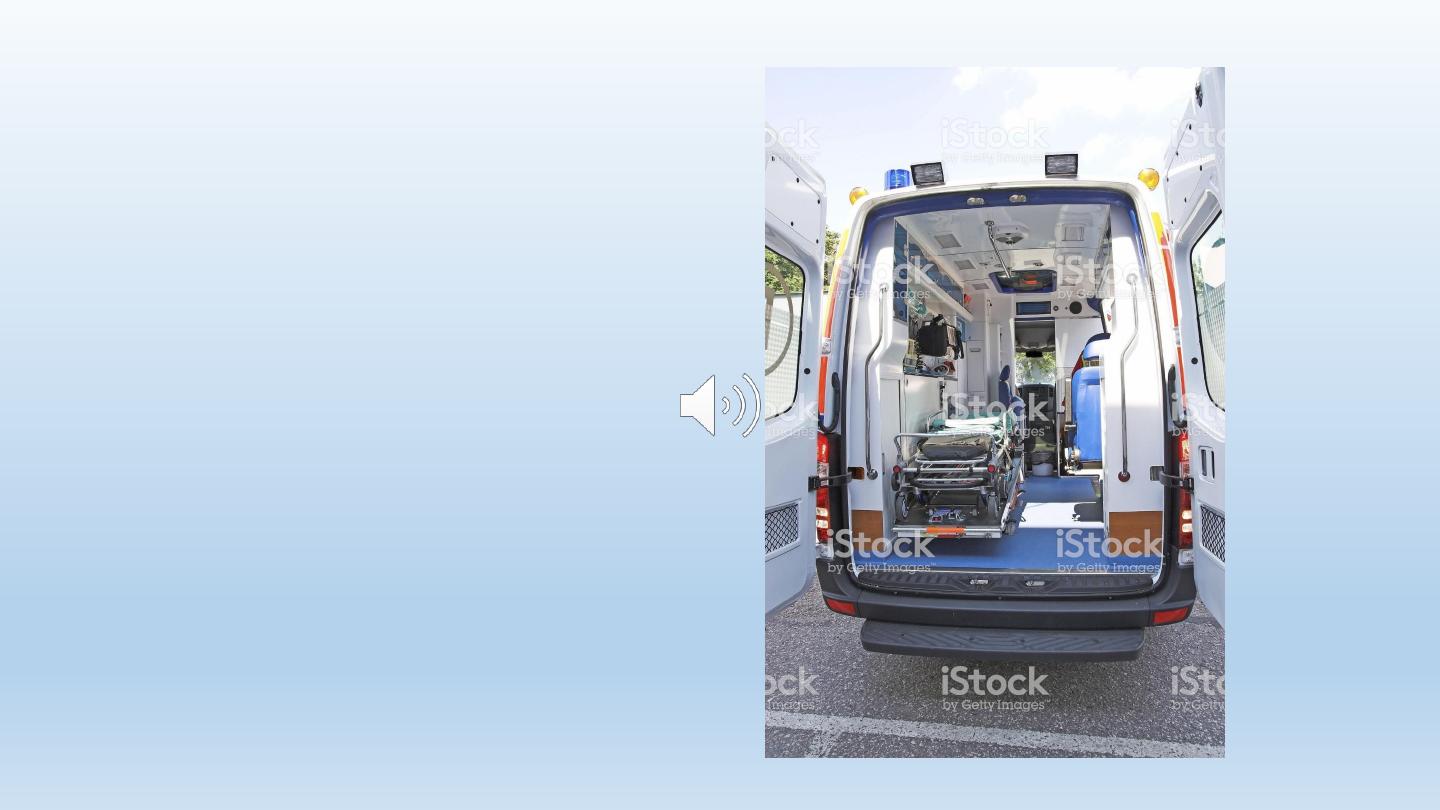
• Ambulance should be well
equipped:
• Defibrillators
• Analgesia
• Oxygen
• Monitors
• ECG machines
• Thrombolytic therapy?
49
Early managemnt: immediate measures
• Cannula
• Oxygen
• ECG monitoring
• Standard (12-lead) ECG
• Analgesia: morphine sulphate

50
REPERFUSION
THERAPY
51
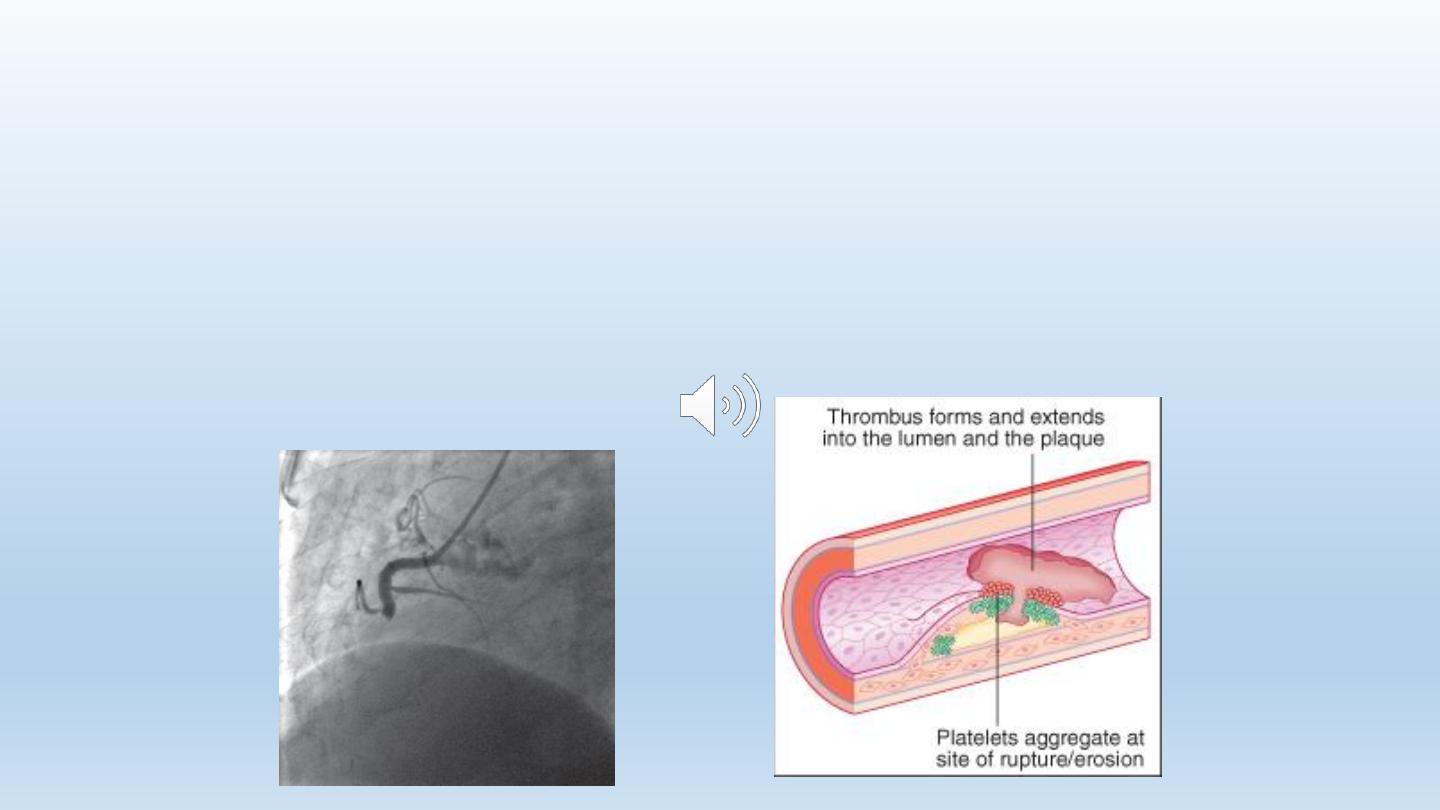
STEMI
• Myocardial necrosis caused by thrombotic occlusion of a
coronary artery
• Occlusive thrombus is formed at site of rupture of
atherosclerotic plaque
Reperfusion
• Once diagnosis is established, reperfusion should be
attempted
• Should be done as soon as possible
• The situation is an emergency: minutes mean muscle

THE KEY TO PROPER MANAGEMENT OF ACUTE
MYOCARDIAL INFARCTION IS THE TIMELY AND
IMMEDIATE REMOVAL OF THROMBUS
OBSTRUTION AND RESTORATION OF BLOOD FLOW
TO THE INFARCTED SEGMENT. THIS IS EXPECTED
TO PREVENT LOSS OF MYOCARDIUM, IMPROVE LV
FUNCTION, IMPROVE QUALITY OF LIFE, AND
PROLONG SURVIVAL.
53
54
Reperfusion
• Restoration of coronary patency
• Resolution of acute ST elevation
• Reduces myocardial infarct size
• Relieves pain
• Preserves LV function
• Improves survival
55
Reperfusion
• May reduce arrhythmias, but may exacerbate these
arrhythmias (reperfusion injury)
• Should be administered as soon as possible to achieve
maximal salvage of myocardium (minutes mean muscle)
Methods of Reperfusion
•Pharmacological (thrombolytic therapy)

Mechanical (primary PCI)
• Mechanical (primary PCI)

58
Reperfusion: Thrombolytic therapy
• Thrombolytic agents:
• Streptokinase
• Alteplase (tPA)
• Tenecteplase (TNK)
• Reteplase (rPA)
59
Reperfusion: Thrombolytic therapy
• Thrombolysis is of no benefit (and may be harmful):
• If given > 12 hours from the onset of STEMI
(preferably given within the first 6 hours)
• In cases of NSTEMI or unstable angina

60
Thrombolytic Complications
Bleeding:
• Cerebral hemorrhage :
• It may be wise to withhold treatment if there is significant risk of bleeding
• With streptokinase:
• the development of antibodies to the drug that render future administration
of the drug ineffective
• hypotension
61
Thrombolysis: Contraindications
Absolute contraindications:
• Known bleeding tendency
• Active bleeding (except menstruation)
• History of cerebrovascular occlusion within the previous year
• History of intracranial hemorrhage
• Cerebral or spinal tumor
63
Reperfusion therapy: primary PCI
• Associated with better results than thrombolytic
therapy
• Requires specialized experience and expensive
equipment
• Should be performed as soon as possible (minutes
mean muscles)
• Indicated in cases of failure of thrombolytic therapy or
when such therapy is contraindicated.
64
Objectives
• Be familiar with the management of the patient with
established myocardial infarction
• Understand STEMI complications in the CCU: Mechanical and
electrical
• Appreciate the long-term management of patients with
STEMI
Clinical Scenario 3:
• A 63-year-old diabetic woman sustained an anterior wall
STEMI.
• Was transferred in time to hospital
• Received thrombolytic therapy with t-PA with resolution of
ST changes and disappearance of chest pain
• Was transferred to the CCU
• Echo showed mild hypokinesia of the anterior wall with good
systolic function
• What is the next step in management?
67
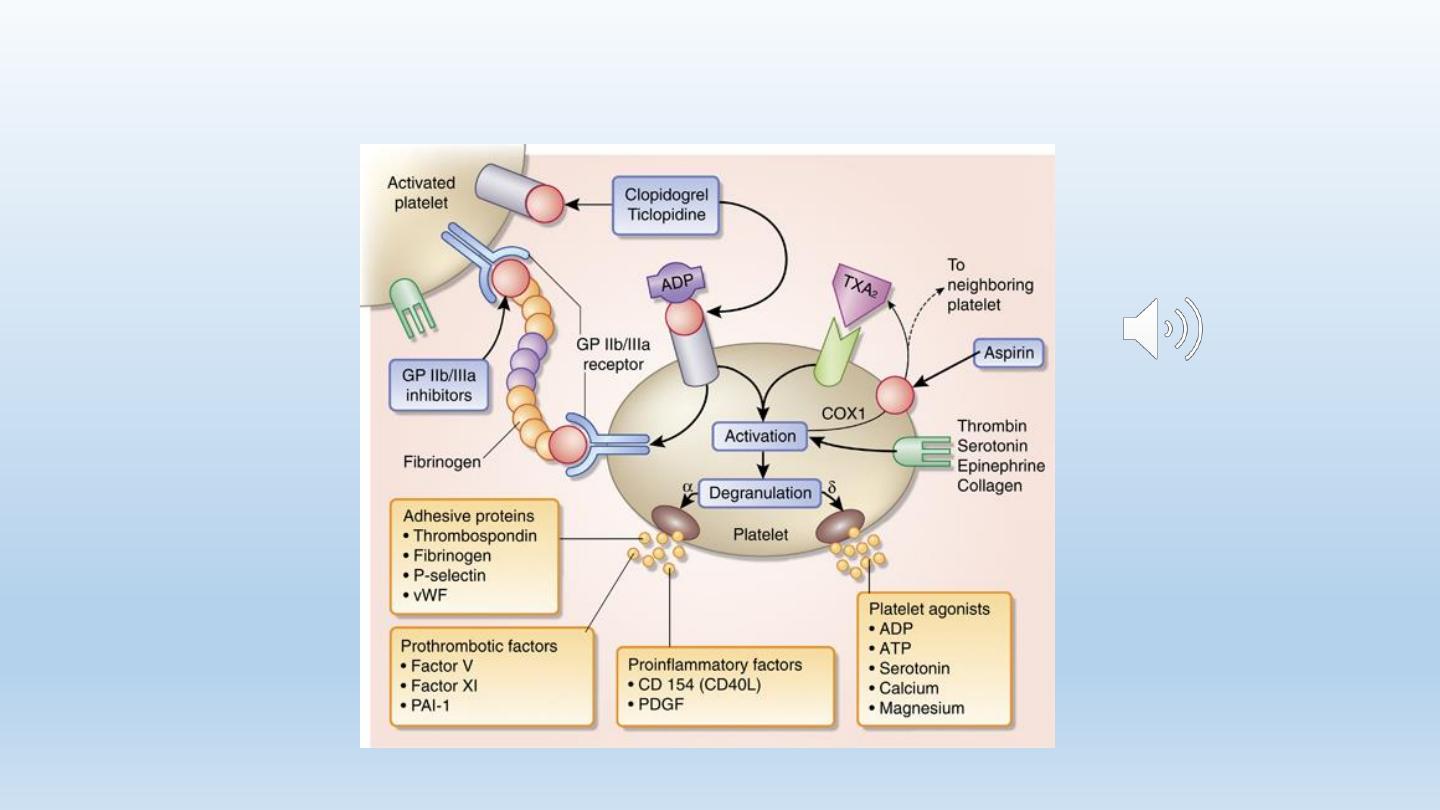
Maintaining Vessel Patency
• Aspirin
• Clopidogrel
• Anticoagulants
68
Maintaining Vessel Patency: ASA
• Oral ASA (75-350 mg/day)
• Reduces mortality
• Should be continued for life
• Combination with clopidogrel: improves outcome
69
70
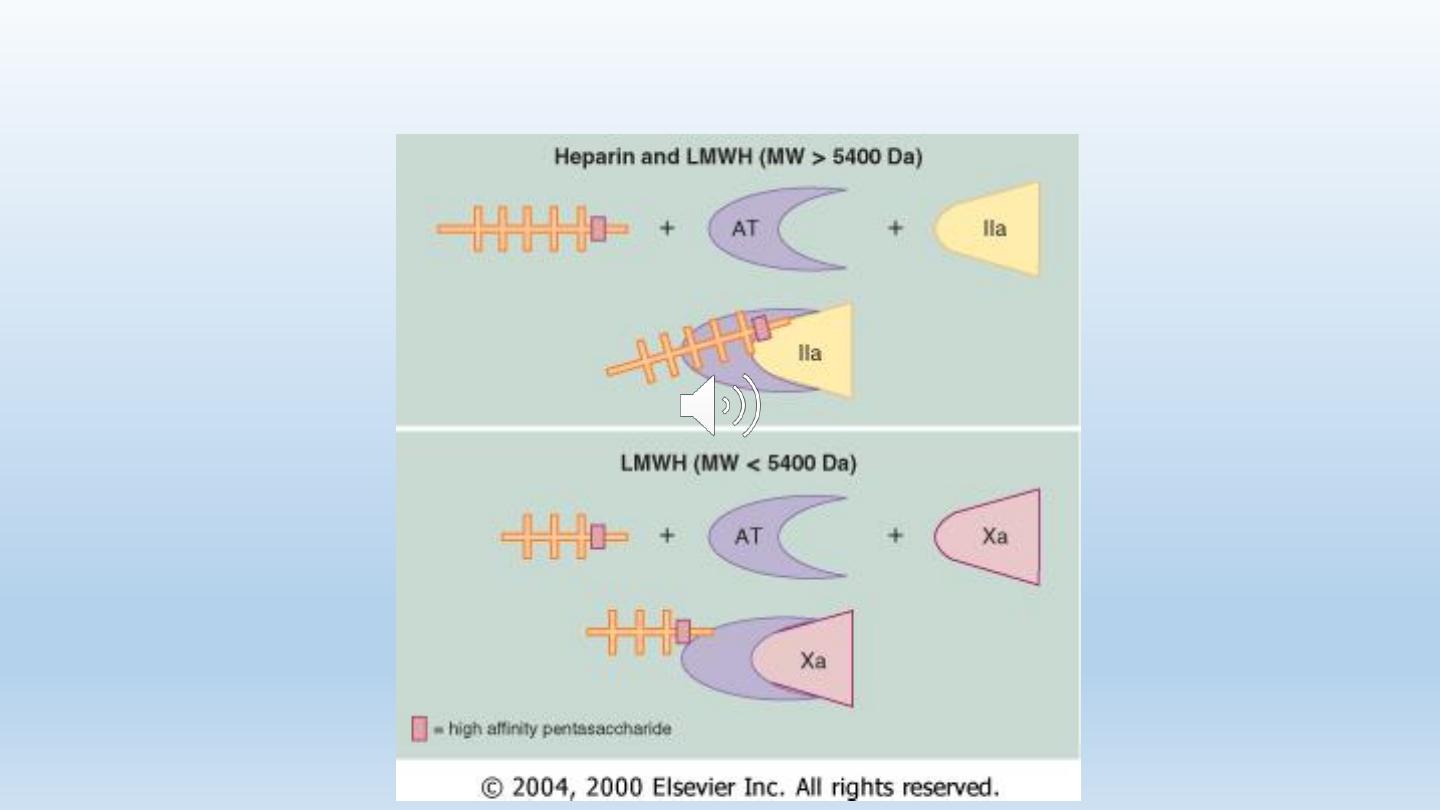
Maintaining Patency: Anticoagulants
• Heparin:
• Unfractionated heaprin and LMWH
• Improve survival of patients with STEMI
• Slight increase in the risk of intracranial bleeding
• Not given after successful primary PCI
71
Antithrombotic therapy
72
Oral Antithrombotic therapy?
• Warfarin
• Direct acting oral anti-coagulants:
• Direct thrombin inhibitors: dabigatran
• Factor Xa inhibitors: apixaban, rivaroxaban
Indications:
• Atrial fibrillation
• Extensive anterior wall MI with LV dysfunction
• The demonstration of mobile thrombus on echocardiography
73
Management of STEMI
• Early management
• Maintaining vessel patency
• Adjunctive therapy
74
Adjunctive Therapy
• β-blockers
• Nitrates (?)
• ACE inhibitors
• Lipid-lowering agents (statins)
75
Adjunctive Therapy: β-blockers
• During the acute presentation:
• i.v. administration
• Atenolol or metoprolol
• Reduce pain
• Reduce arrhythmia
• Improve short term survival
• Contraindicated:
• Congestive heart failure
• Heart block
• bradycardia
76
Adjunctive Therapy: β-blockers
Long term use of β-blockers :
•
Should be given to ALL patients unless contraindicated
•
Improve long term survival
Adjunctive Therapy: ACE inhibitors, Statins
• Essential for the secondary prevention of atherosclerosis
• ACE inhibitors are also useful to maintain LV function
• When side-effects develop to ACE inhibitors, ARBs should be
used
Complications of STEMI: Clinical Scenario 4
• A 55-year-old hypertensive and smoker sustains an extensive
anterior infarction. He is only transferred to hospital 24
hours after the attack. The ECG shows established anterior
wall MI, with deep Q waves, ST elevation, and T inversion in
the anterior leads. No thrombolytic therapy was
administered
• What are the expected complications?
79
COMPLICATIONS OF STEMI
• Short-term complications
• Arrhythmias
• Mechanical complications
• Residual ischemia
• Pericarditis
• embolism
• Long term complications
• Recurrnet ischemia
• LVdysfunction
80
complications
• Arrhythmias
• Mechanical complications
• Acute circulatory failure
• Residual ischemia
• Pericarditis
• embolism
81
complications
tachy arrhythmias
ventricular
• Arrhythmias
atrial
brady arrhythmias
82
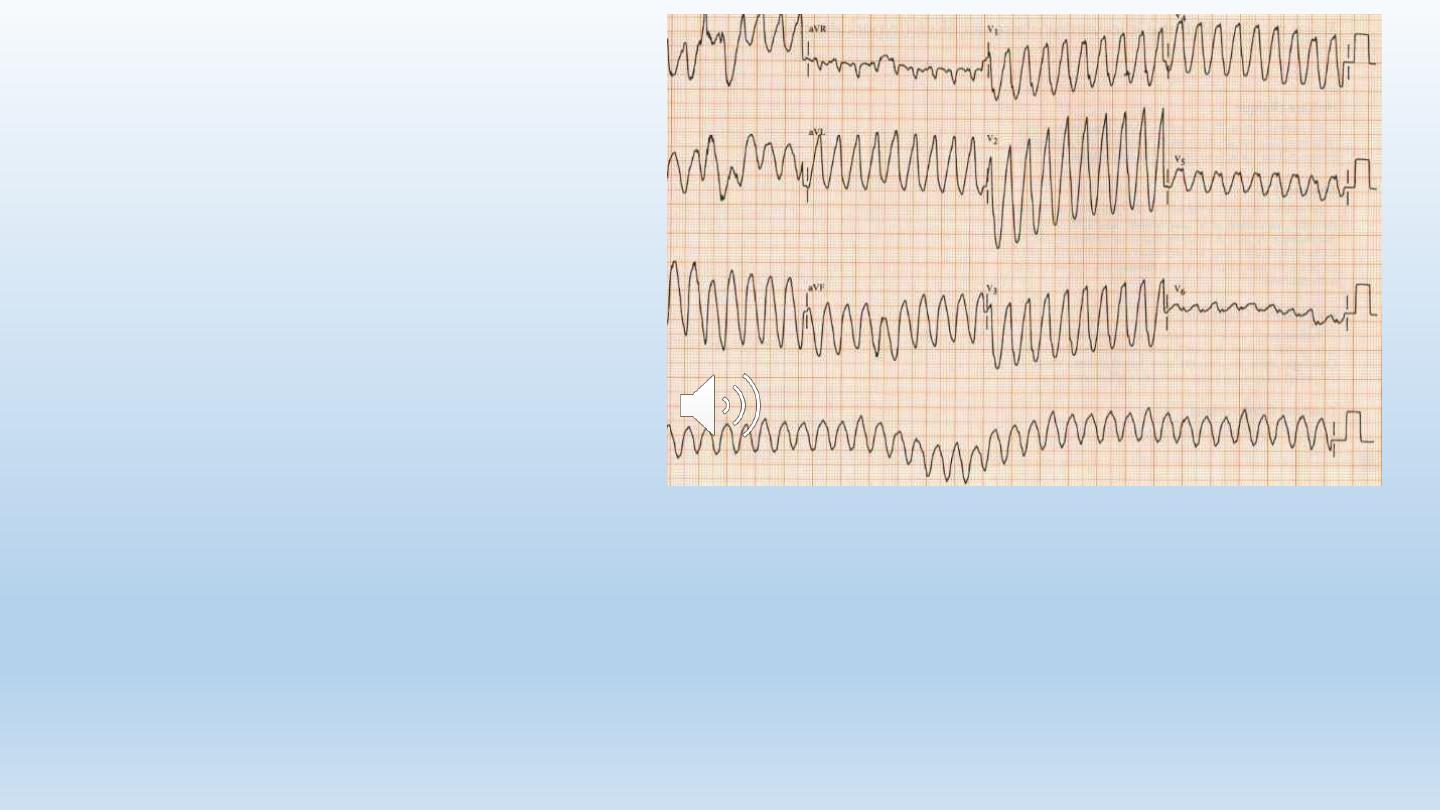
Tachyarrhythmias
• Ventricular:
– Premature ventricular ectopics (PVCs)
– Accelerated idioventricular rhythm
– Ventricular tachycardia
– Ventricular fibrillation
• Atrial
– Atrial fibrillation
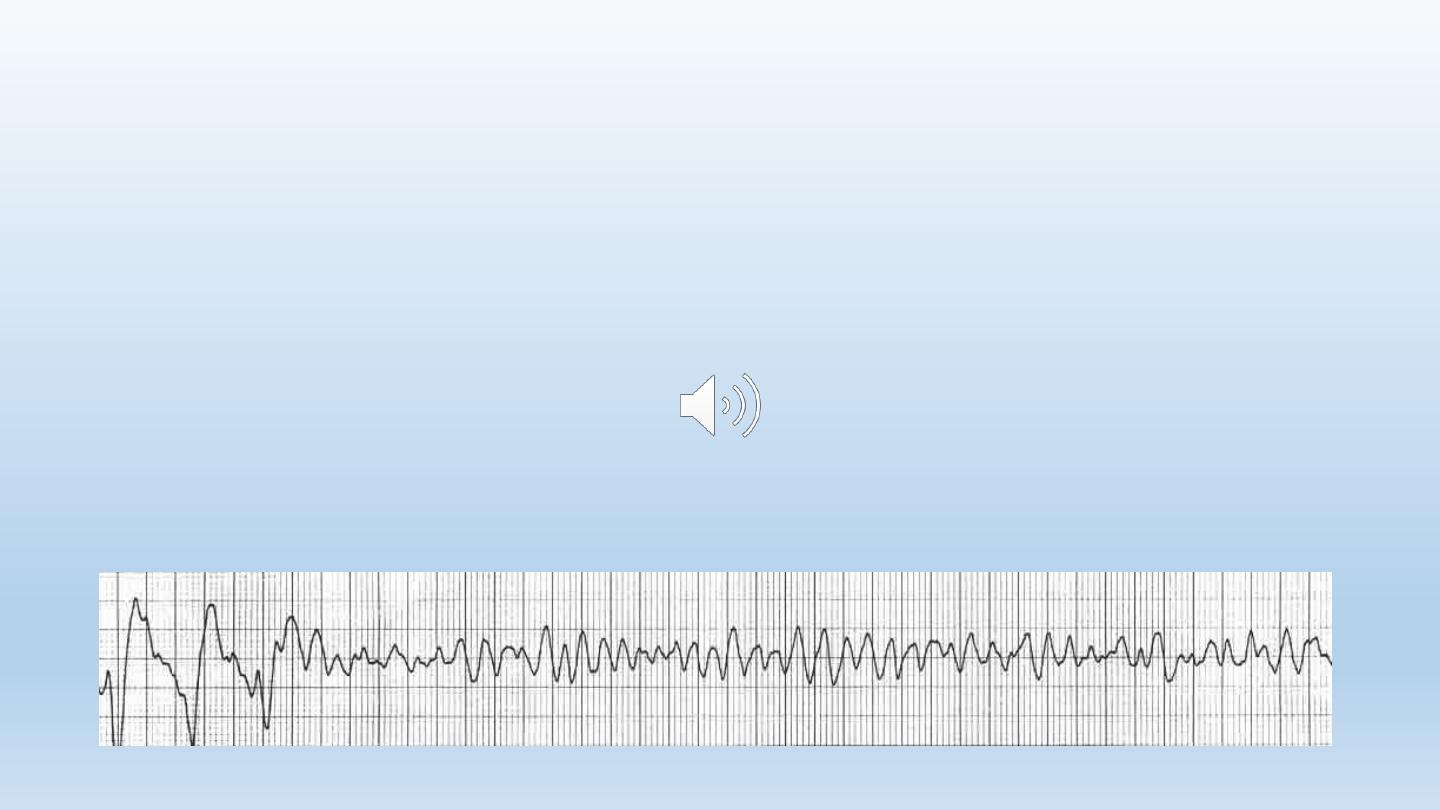
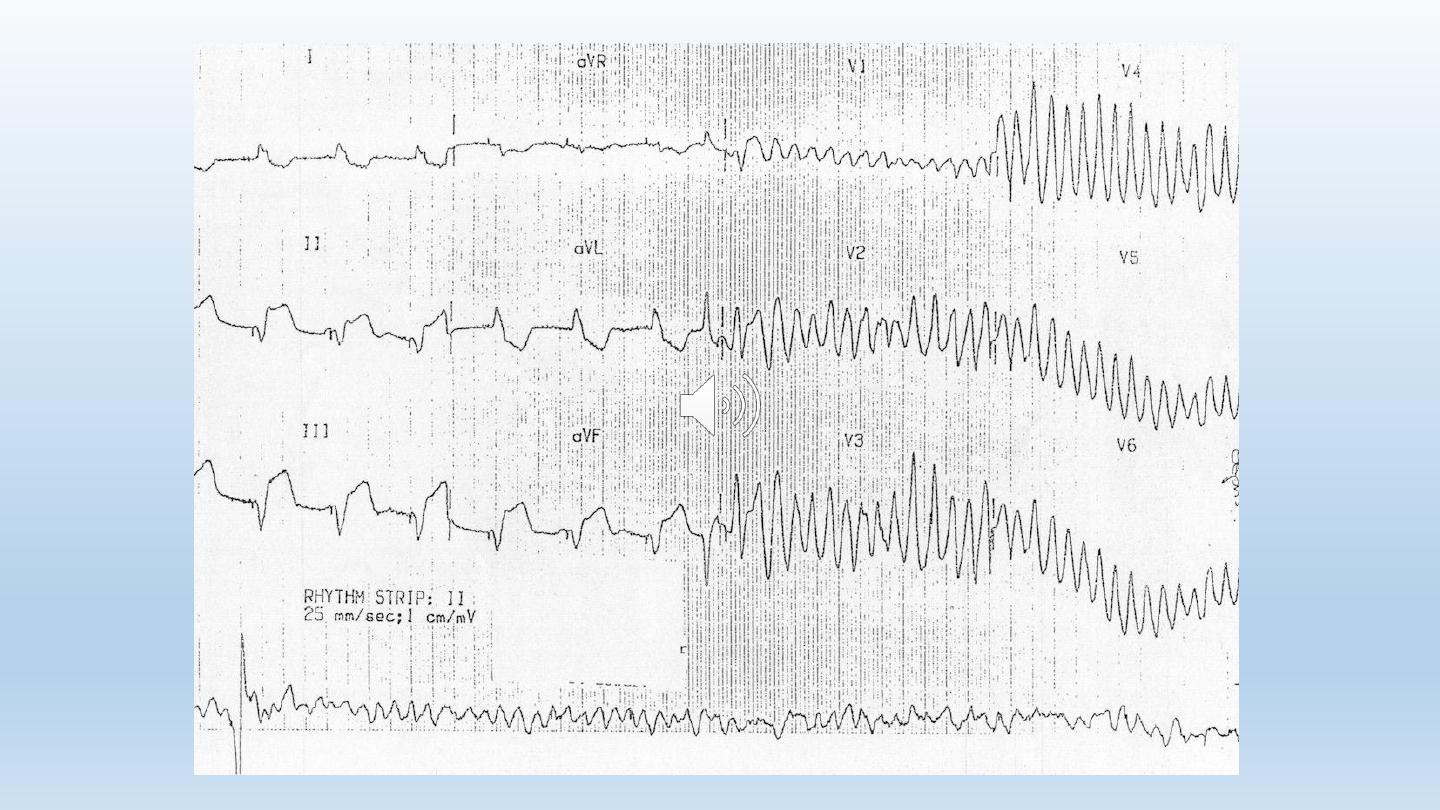
Tachyarrhythmias
The patient collapsed in the CCU!
• What is the diagnosis
• What’s the urgent treatment?
• What drug is given to prevent recurrence?
Tachyarrhythmias
Ventricular fibrillation:
• The major cause of death in
patients with STEMI before
reaching hospital
• Occurs in 5-10% of patients who
reach hospital
• Lethal arrhythmia unless treated
by prompt defibrillation
• Does not affect the long term
prognosis of acute MI.
84
Tachyarrhythmias
Atrial fibrillation:
• Common in acute MI
• Frequently transient
• May be serious if it
occurs in the context of
LV failure
85
87
Atrial Fibrillation: Treatment
• May be transient and needs no treatment
• Indications to treat:
• Rapid ventricular rate
• Hemodynamic deterioration (hypotension, CHF, pulmonary
edema)
• Emergency treatment:
• Synchronized DC shock
• Non-emergency situation:
• Infusion of β-blocker or amiodarone
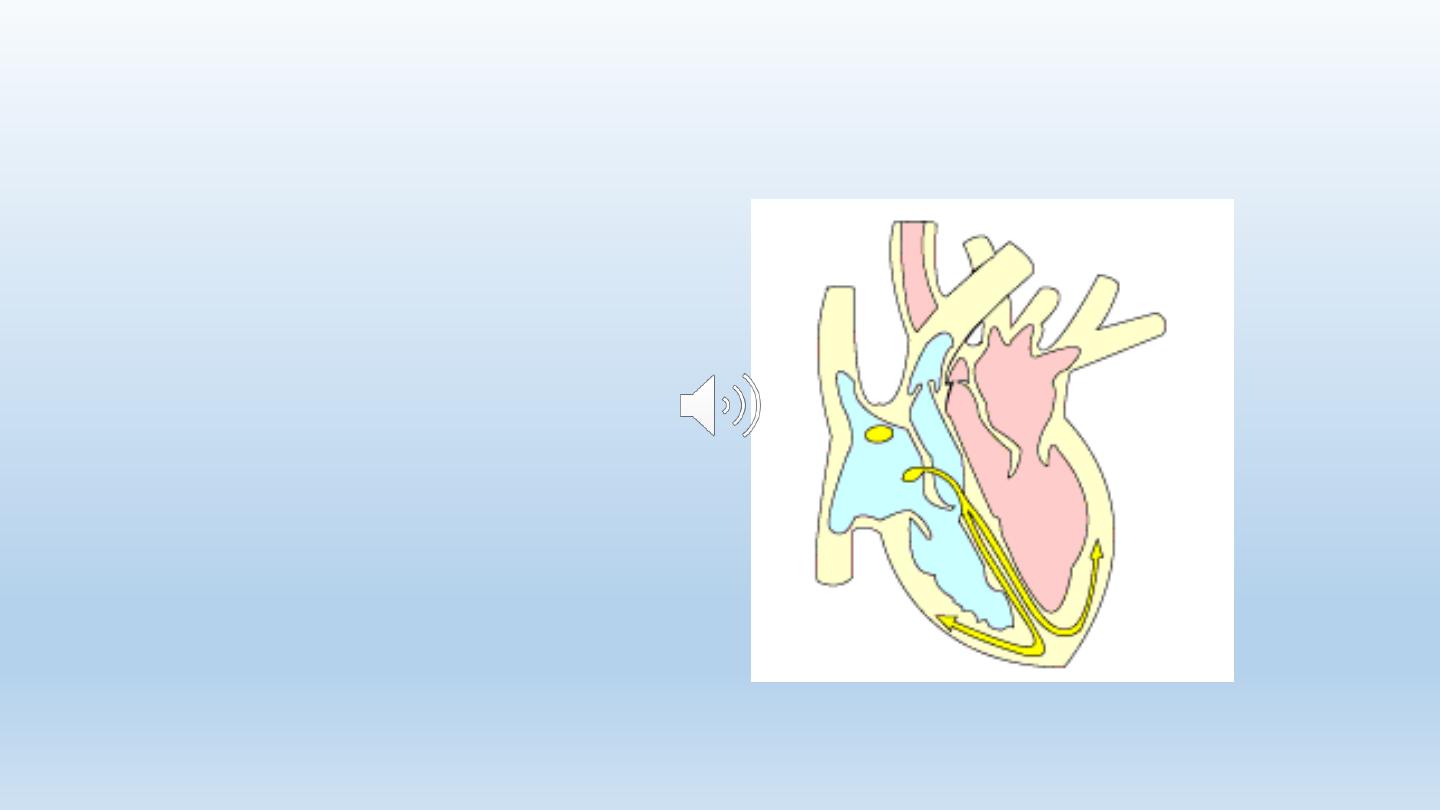
Bradyarrhythmia: AV block
In the setting of inferior MI:
• Usually temporary
• Resolves with thrombolytic
therapy
• May need atropine if persists
• If there is hemodynamic
deterioration:
temporary pacemaker insertion
88
89
Bradyarrhythmia: AV block
In the setting of anterior wall MI:
• More serious than in inferior MI
• May be complicated by sudden asystole
• Prophylactic temporary pacemaker should be inserted
90
complications
• Arrhythmias
• Mechanical complications
• Acute circulatory failure
• Residual ischemia
• Pericarditis
• embolism
91
Mechanical complications
• Papillary muscle rupture
• Interventricular septal rupture
• Ventricular free wall ruputre
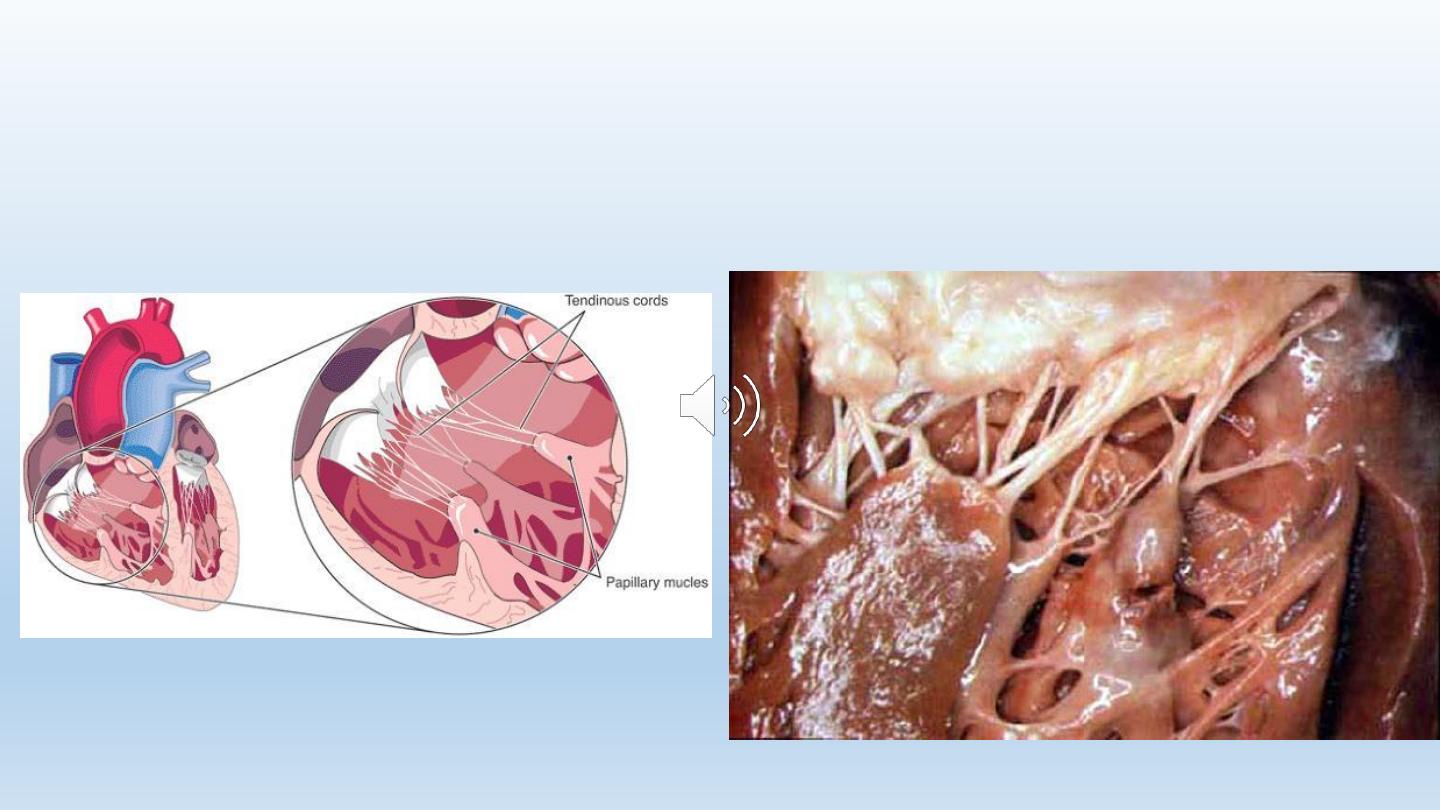
Papillary Muscle Rupture
93
Papillary muscle rupture
• Sudden severe mitral regurgitation (MR)
• Presents with pulmonary edema & shock
• O/E: pansystolic murmur at the apical area radiating to the
axilla or back. S3 & S4
• The murmur is frequently faint or even absent
• Dx: echo and Doppler
• Treatment: urgent surgery
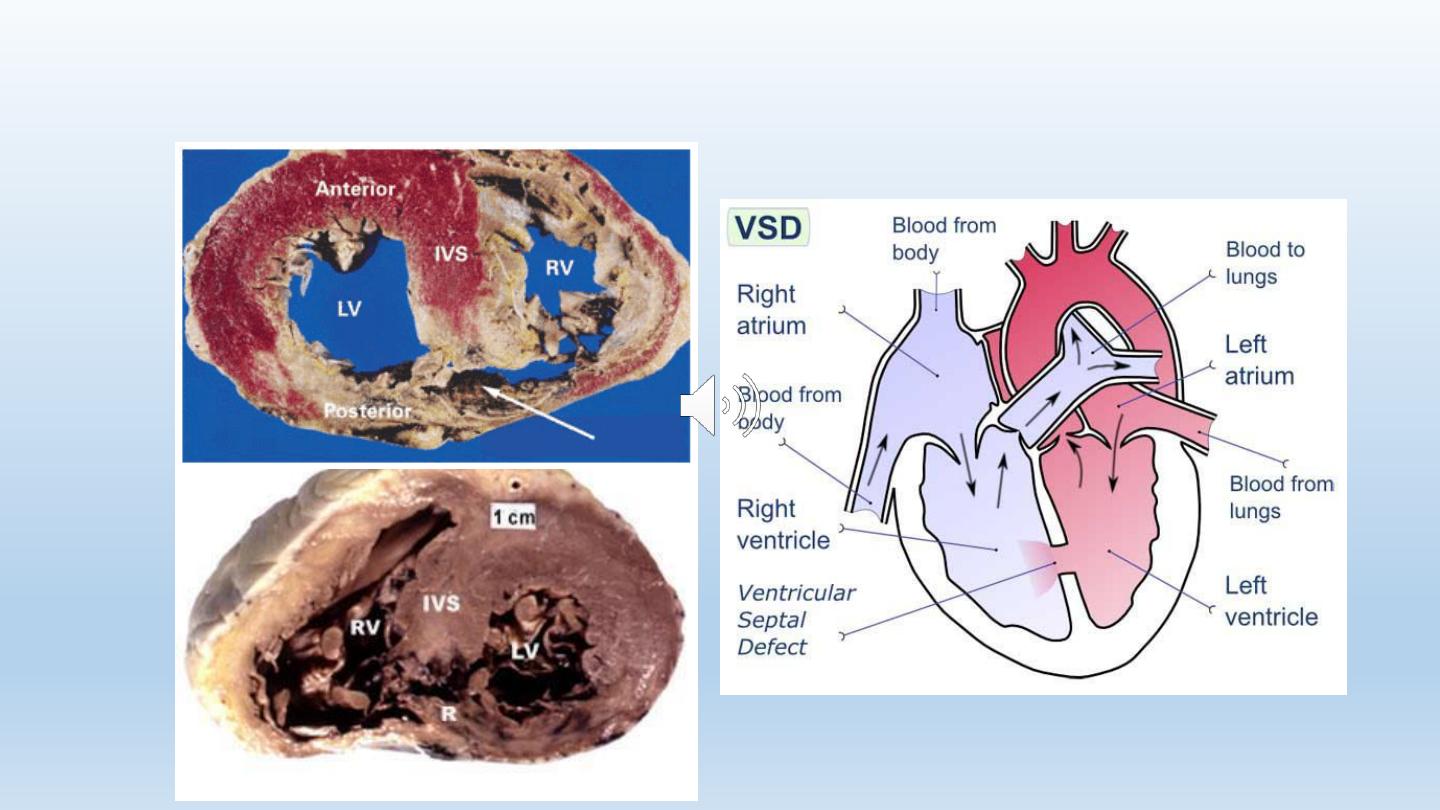
Ventricular Septal Rupture
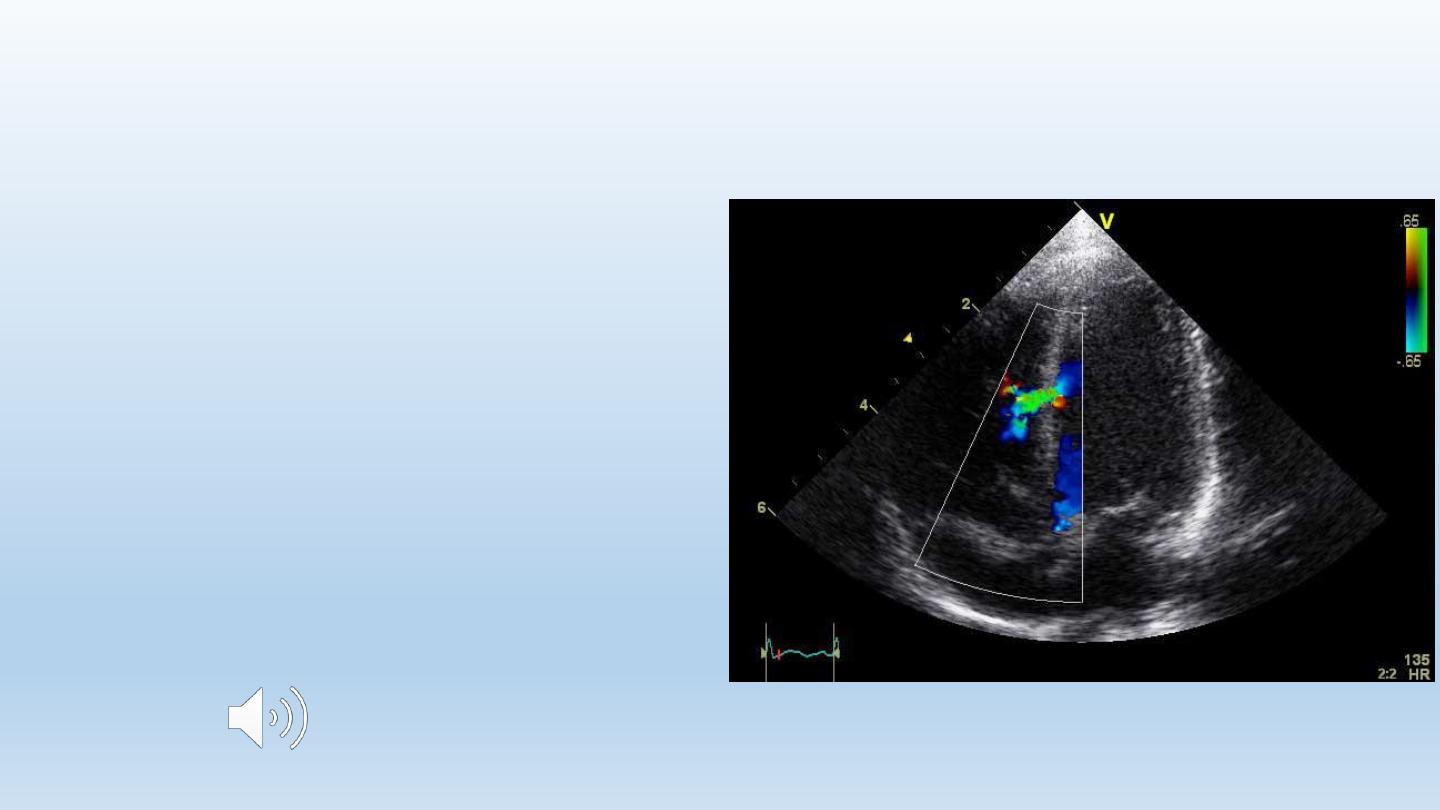
Ventricular Septal rupture
• Sudden deterioration:
hypotension, right ventricular
failure, shock
• Clinically: pansystolic murmur at
the left sternal border
• Diagnosis: echo and Doppler
• Treatment: surgery
95

96
complications
• Arrhythmias
• Mechanical complications
• Acute circulatory failure
• Residual ischemia
• Pericarditis
• Embolism
97
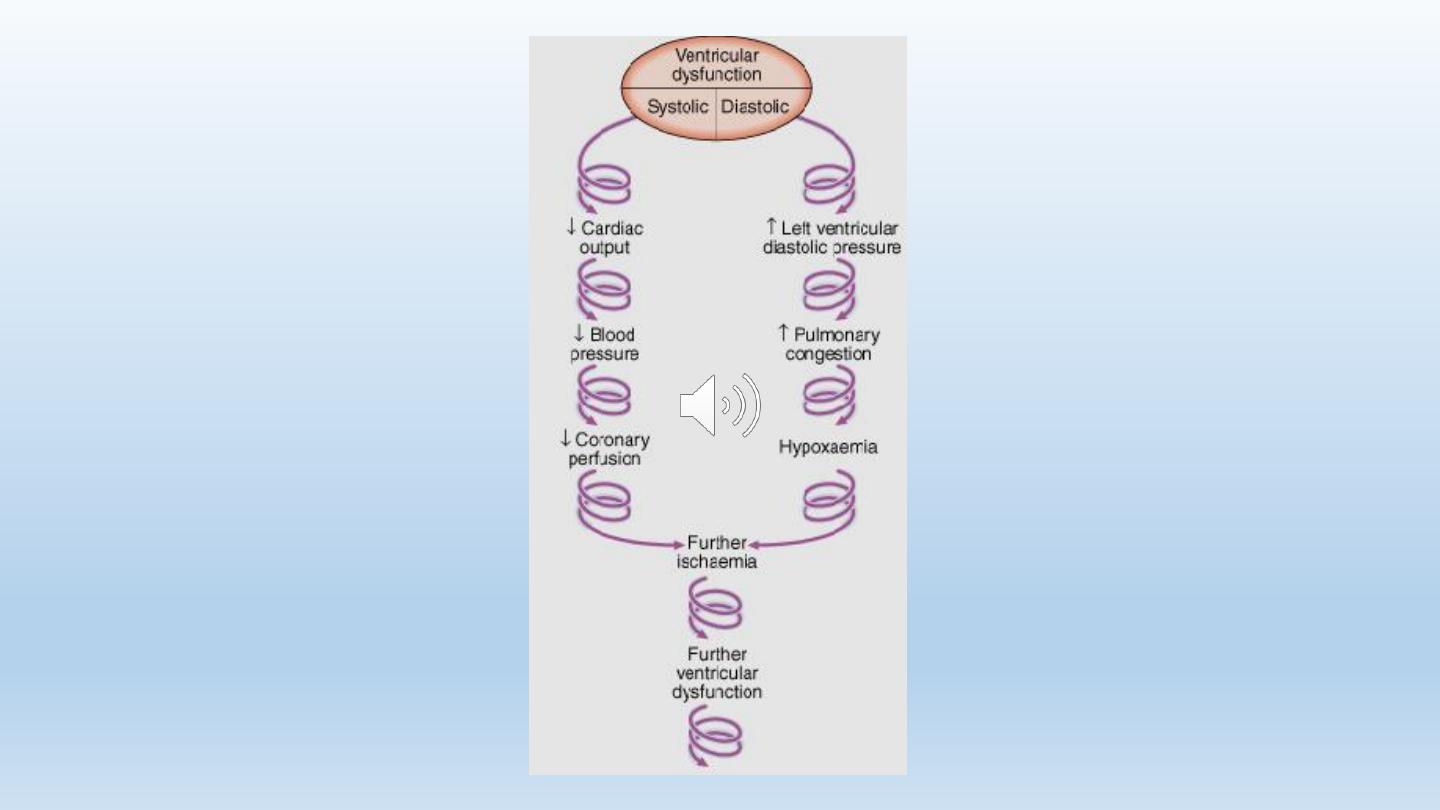
Acute circulatory failure
(Cardiogenic Shock)
• Indicates extensive myocardial damage
• Usually fatal without intervention
• Mortality of 90% if untreated
• With primary PCI: can be reduced to 25%
98
99
Management of cardiogenic shock
• Calculating cardiac output & systemic vascular resistance
(Swan-Ganz catheter)
• The use of inotropic drugs, diuretics, &/or vasodilators
according to the calculations
• Circulatory assistance with intra-aortic balloon pump
• Primary PCI

100
complications
• Arrhythmias
• Mechanical complications
• Acute circulatory failure
• Residual ischemia
• Pericarditis
• Embolism
101
Residual Ischemia
• Presents as post infarction angina
• Causes of residual ischemia:
• Significant stenosis of an artery after successful thrombolysis
• Blockage of an artery that was responsible for the collateral supply of another
coronary artery
• Occurs in ~ 50% of patients with AMI
102
Residual Ischemia: Management
High risk group of unstable angina
• i.v. nitrates, β-blockers, Oxygen (if necessary)
• Aspirin
• Clopidogrel
• Anticoagulation
• Invasive strategy (PCI or CABG)

103
complications
• Arrhythmias
• Mechanical complications
• Acute circulatory failure
• Residual ischemia
• Pericarditis
• embolism
Pericarditis Following STEMI
• Acute pericarditis
• Post MI syndrome (Dressler’s Syndrome)
105
Acute Pericarditis
• Usually occurs in the 2
nd
& 3
rd
days
• Chest pain of different quality than ischemic:
• Sharp
• Localized
• Positional
• Related to breathing: worse on inspiration
• Pericardial friction rub
• ECG changes of acute pericarditis
106
Acute Pericarditis: Management
• The use of steroids or NSAID is contraindicated in AMI:
• Weakening of scar
• Increase the risk of aneurysm formation
• Aspirin in high dose
• colchicine
• Opiate-based analgesia
107
Post-MI-Pericarditis
(Dressler’s syndrome)
• Auto-immune reaction
• May occur 6 days-6 months after MI
• Pain (pleuro-pericarditis)
• Pyrexia
• Pericarditis
• Pleurisy
• Treatment: High dose ASA, NSAID, colchicine,
or even steroids
108
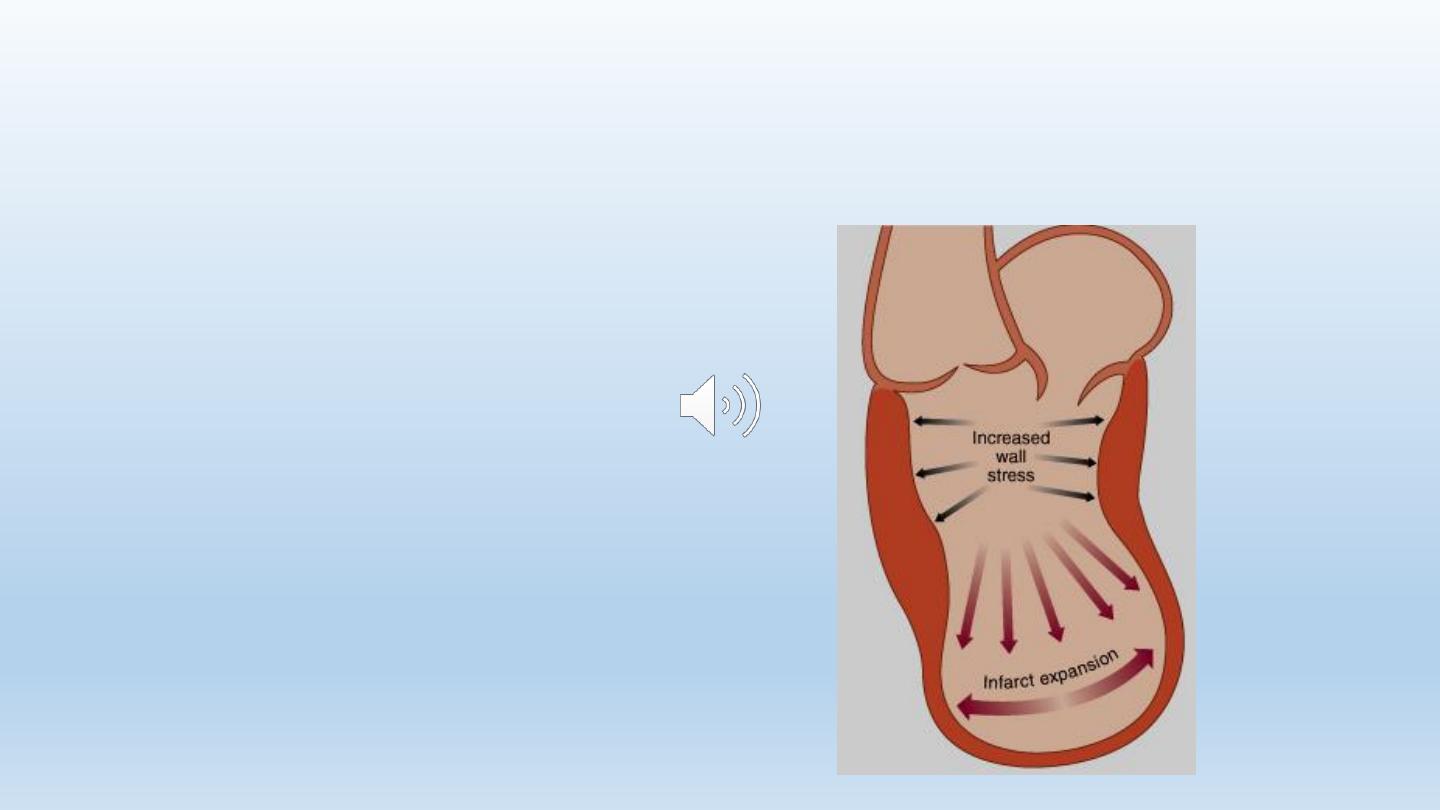
Complications: Ventricular
Remodelling
• Infarct expansion: thinning
& stretching of the
infarcted segment
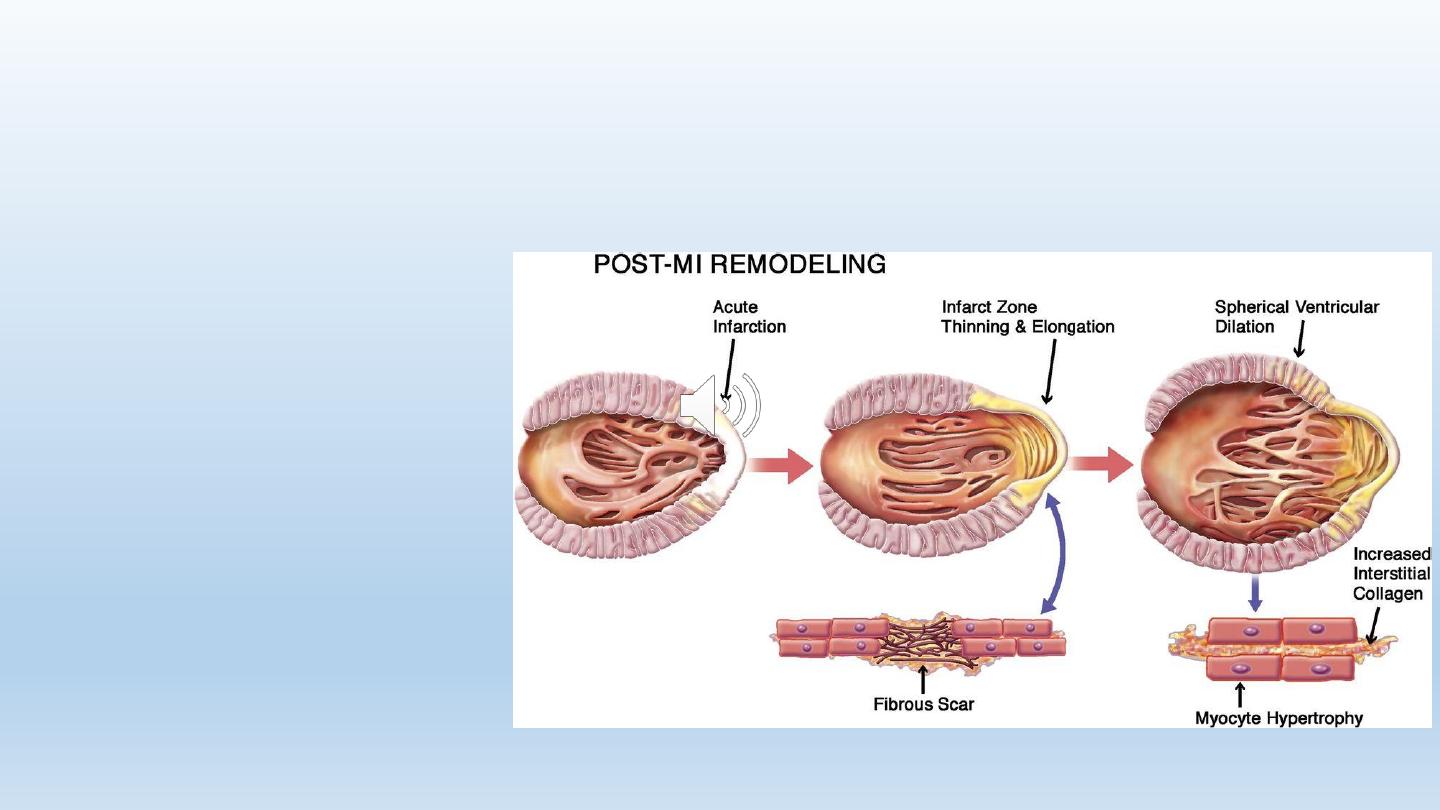
Complications: Ventricular Remodelling
• Compensatory hypertrophy
of the remaining muscle
• Increased myocardial wall
tension
109
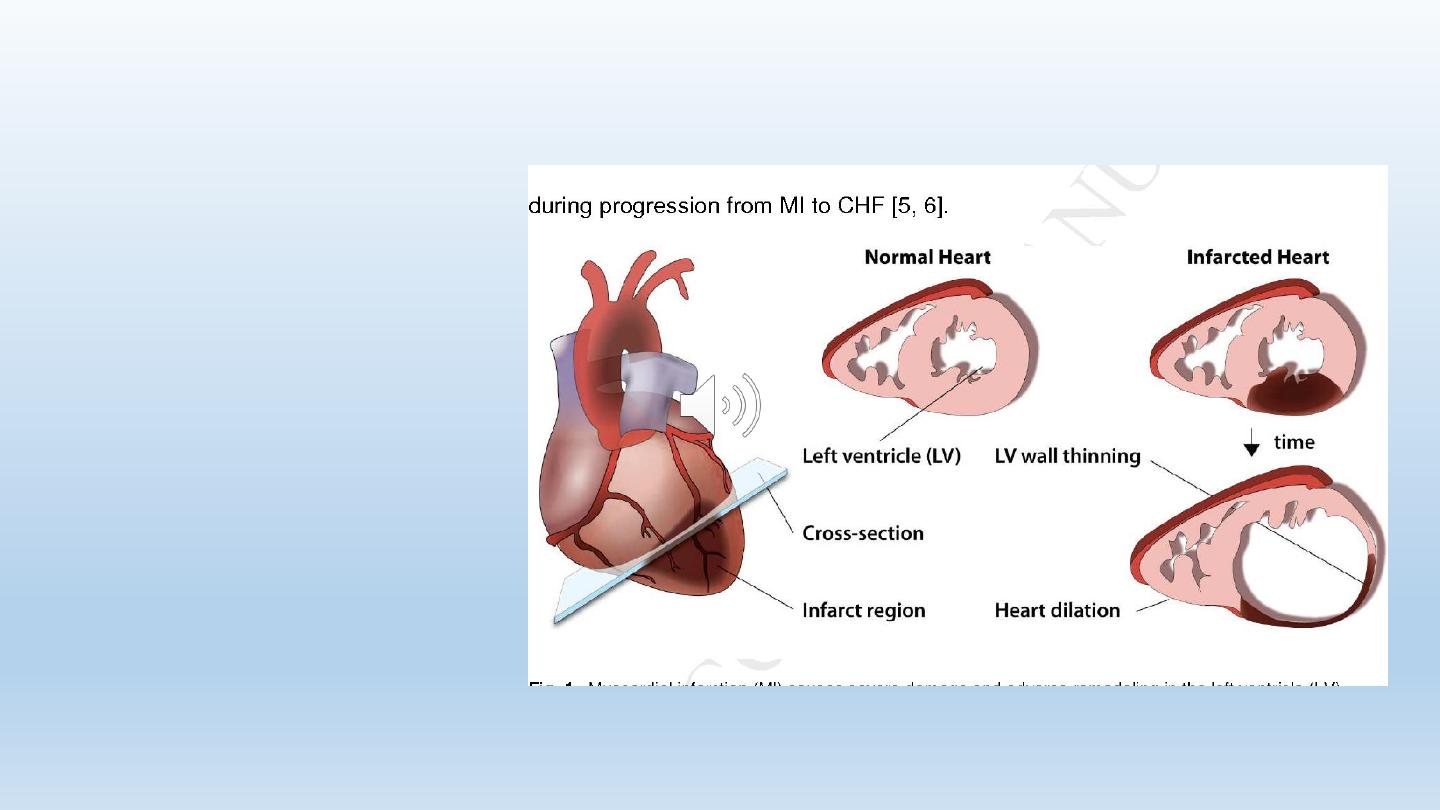
Complications: Ventricular Remodelling
• Eventual dilatation and
dysfunction of LV,
with the formation
of aneurysm
110
Drugs Used to Prevent Remodelling
• Angiotensin converting enzyme inhibitors
• Angiotensin receptor blockers
• Beta receptor blockers
• Mineralocorticoid antagonists
• Neprilysin inhibitors (sacubitril)
112
Management After Discharge From
Hospital
• Risk stratification
• Secondary prevention
• Rehabilitation
113
Risk Stratification after MI
Assessment for
•Residual ischemia
•Left ventricular function
•arrhythmias
114
Residual Ischemia
• Symptomatic patient: Coronary angio with a view to
revascularization
• Asymptomatic:
• Stress testing: routinely done after 4 weeks
• If high risk criteria coronary angio
• If not repeat ETT every year or if new
symptoms appear
115
Assessment of LV function
• Clinically
• ECG
• CXR
• Echo
• Radioisotope study
116
In Patients with LV dysfunction
• Look for reversible ischemia: coronary angio
• ACE inhibitors (captopril, enalapril, lisinopril)
• Angiotensin receptor blocker (ARBs) (valsartan,
losartan, candisartan) in patients who can’t
tolerate ACEI
• β-blockers: metoprolol, bisoprolol, & carvedilol
• Aldosterone receptor antagonist:
spironolactone, eplerenone
• ARB/neprilysin inhibitor (valsartan/sacubitril)

117
Arrhythmias
• Recurrent ventricular arrhythmias, causes:
• Residual ischemia
• LV dysfunction
• The presence of scar tissue
• Significant ventricular arrhythmias:
mangement
• Treatment of LV dysfunction, residual ischemia
• Electrophysiological study
• Specific anti-arrhythmic therapy
• Implantable cardiovertor-defibrillator (ICD)
118
Natural history & prognosis
• 25% of patients die within a few minutes
• 40% die within first month
• Early death is usually caused by arrhythmia
• Later on: the outcome is determined by the extent of
myocardial damage

119
Determinants of poor prognosis
• Poor LV function
• Arrhythmias
• Persistent AV block
• Anterior infarction > inferior infarction
• Old age
• Depression
• Social isolation
