Principles of oncology
Dr. Ali JafferGI surgeon
DAdvSurg (GI), C.A.B.S, M.B.Ch.B
Features of malignant transformation
Establish an autonomous lineageCells develop independence from the normal signals that control supply and demand.
Cancer cells escape from this normal system of checks and balances.
Oncogenes, aberrant forms of normal cellular genes, are key factors in this process.They were previously thought to be of viral origin, but, surprisingly, turned out to be parts of the normal genome that were hitchhiking between cells, using the virus as a vector.
we all carry within us the seeds of our own destruction: genetic sequences that, through mutation, can turn into active oncogenes and thereby cause malignant transformation.
Obtain immortality
The Hayflick hypothesis; normal cells are permitted to undergo only a finite number of divisions. For humans this number is between 40 and 60.The cancer cell has achieved immortality.
Features of malignant transformationEvade apoptosis
Apoptosis is a form of programmed cell death which occurs as the direct result of internal cellular events instructing the cell to die.
Cells that find themselves in the wrong place normally die by apoptosis and this is
an important self-regulatory mechanism in growth and development.Cancer cells will be able to evade apoptosis, which means that the wrong cells can be in the
wrong places at the wrong times.
Features of malignant transformation
Acquire angiogenic competenceThe ability of a tumour to form blood vessels is termed ‘angiogenic competence’ and is a key feature of malignant transformation.
Acquire ability to invade
They acquire the ability to breach the basement membrane and gain direct access to blood and lymph vessels.
Cancer cells use three main mechanisms to facilitate invasion:
they cause a rise in the interstitial pressure withina tissue.they secrete enzymes such as (collagenases and proteases) that dissolve extracellular matrix.
they become mobile.
Features of malignant transformation
Acquire ability to disseminate and implant, evocation of inflammationEvade detection/elimination
Develop ability to change energy metabolismCompared with the corresponding normal cells, some cancer cells may be better able to survive in hypoxic conditions.
This ability may enable tumours to grow and develop despite an impoverished
blood supply.
Malignant transformation
The characteristics of the cancer cell arise as a result of mutation, multiple mutations are usually required.* Cancer is usually regarded as a clonal disease.
Two mechanisms may help to sustain and accelerate the process of malignant transformation:
Genomic instability
The cancer cell as it evolves, it contains an increasing variety and number of genetic aberrations. The greater the number of such abnormalities, the greater the chance of increasingly deviant behaviour, and the pace of malignant transformation accelerates.
Tumour-related inflammation
Growth factors, mutagenic ROS (reactive oxygen species), angiogenic factors and antiapoptotic factors may all be produced as part of an inflammatory process and all may contribute to the progression of a tumour.The growth of a tumour
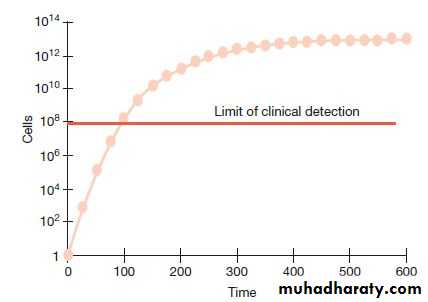
The division of a cell produces two daughter cells. The relationship 2n will describe the number of cells produced after n generations of division.A tumour 10 mm in diameter will contain about 109 cells. Since 230 = 109 this implies that it would take 30 generations to reach the threshold of clinical detectability
The growth of a typical human tumour can be described by an exponential relationship, the doubling time of which increases exponentially– so-called Gompertzian growth
The Gompertzian curve
The implications of Gompertzian growthThe majority of the growth of a tumour occurs before it is clinically detectable. By the time they are detected, tumours have passed the period of most rapid growth, that period when they might be most sensitive to antiproliferative drug.
There has been plenty of time, before diagnosis, for individual cells to detach, invade, implant, and form distant metastases.
In many patients cancer may, at the time of presentation, be a systemic disease
THE CAUSES OF CANCERTables 10.1&10.2 p144-146
Baily&Love 27th edition
THE MANAGEMENT OF CANCER
Prevention (table 10.2)Screening
Screening involves the detection of disease in an asymptomatic population in order to improve outcomes by early diagnosis.Criteria for screening
The disease:
Recognisable early stage
Treatment at early stage more effective than at later stage
Sufficiently common to warrant screening
The test:
Sensitive and specificAcceptable to the screened population
Safe
Inexpensive
The programme:
Adequate diagnostic facilities for those with a positive test
High quality treatment for screen-detected disease to minimise morbidity and mortality
Screening repeated at intervals if disease of insidious onset
Benefit must outweigh physical and psychological harm
THE MANAGEMENT OF CANCER
Diagnosis and classificationCancer is a disease of cells and, for accurate diagnosis, the abnormal cells need to be seen.
Only rarely can a diagnosis of cancer be confidently made in the absence of tissue for pathological or cytological examination.
Precise and accurate subtyping of tumours enables appropriate selection of treatment and, in turn, this is associated with better outcome.
Different tumours are classified in different ways:
* Most squamous epithelial tumours are simply classed as well (G1), moderate (G2) or poorly (G3) differentiated.* Adenocarcinomasare also often classified as G1, 2 or 3 but prostate cancer is an exception, with widespread use of the Gleason system.
THE MANAGEMENT OF CANCER
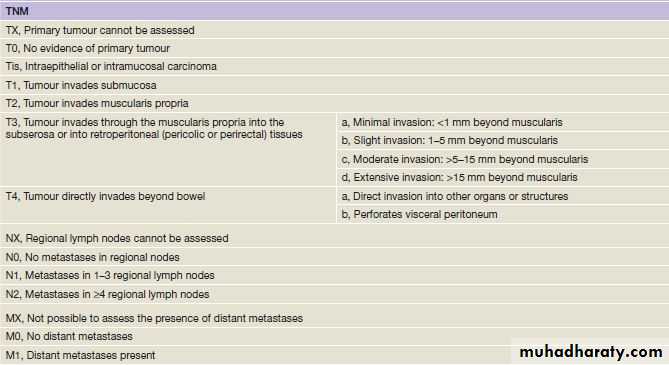
Investigation and stagingStaging is the process whereby the extent of disease is mapped out
The UICC (International Union against Cancer) is responsible for the TNM (tumour, nodes, metastases) staging system for cancer. This system is compatible with, and relates to, the American Cancer Society (AJCC) system for stage grouping of cancer.
Therapeutic decision making and the multidisciplinary team
THE MANAGEMENT OF CANCER
Principles of cancer surgeryFor most solid tumours, surgery remains the definitive treatment and the only realistic hope of cure.
A. Diagnosis and staging
B. Removal of primary diseaseRadical surgery for cancer involves removal of the primary tumour and as much of the surrounding tissue and lymph node drainage as possible in order not only to ensure local control but also to prevent spread of tumour through the lymphatics.
C. Removal of metastatic disease
liver metastases arising from colorectal cancerpulmonary resection for isolated lung metastases, particularly from renal cell carcinoma.
D. Palliation
The surgery does not have an effect on the ultimate outcome and survival but it can achieves symptomatic control or mange certain complication such as bypass surgery.THE MANAGEMENT OF CANCER
RadiotherapyX-rays radiation had been discovered in 1895, after one month were used to treat cancer.
Radiation can, both directly and indirectly, influence gene expression: over 100 radiation inducible effects on gene expression have now been described.
These changes in gene expression are responsible for a considerable proportion of the biological effects of radiation upon tumours and normal tissues. In this sense, radiotherapy is a precisely targeted form of gene therapy for cancer.
The practicalities of radiation therapy:
A- define the target to treat.
B- design the optimal technical set up to provide uniform irradiation of that target.
C- choose that schedule of treatment.
Modern radiotherapy
Techniques such as intensity-modulated radiation therapy (IMRT) and image-guided radiation therapy (IGRT), it is possible safely to deliver high doses to irregularly shaped target volumes.
stereotactic ablative radiotherapy (SABR) in which a small number of fractions can be used to treat primary tumours, or isolated metastases, to curative dose levels.
THE MANAGEMENT OF CANCER
Chemotherapy and biological therapiesSelective toxicity is the fundamental principle underlying the use of chemotherapy in clinical practice.
Chemotherapy is often a palliative rather than a curative intervention.
There are now over 120 different drugs licensed by the US Food and Drug Administration (FDA) for the treatment of cancer The majority are cytotoxic drugs, hormonal therapies account for around 10%, and an increasing number have been designed to interact with specific molecular targets – so-called targeted therapies.The next decade will see a major shift in the medical management of cancer – from cell killing to cellular reprogramming.
THE MANAGEMENT OF CANCER
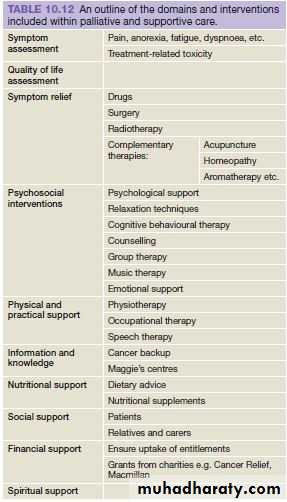
Palliative therapy
End-of-life care
Patients treated palliatively maysurvive
for many years; end-of-life care concerns
the last few months of a patient’s life
Tumour Markers
What are Tumour Markers?Tumour markers are substances that are produced by cancer or by other cells of the body in response to cancer or certain benign (noncancerous) conditions
.
Most tumour markers are made by normal cells as well as by cancer cells; however, they are produced at much higher levels in cancerous conditions. These substances can be found in the blood, urine, stool, tumour tissue, or other tissues or bodily fluids of some patients with cancer.
Most tumour markers are proteins. However, more recently, patterns of gene expression and changes to DNA have also begun to be used as tumour markers.
How Are Tumour Markers Used?
• For Screening and Early Detection of Cancer• ex. Calcitonin in Medullary thyroid carcinoma
• (II) Diagnosing Cancer
• ex. HCG in germ cell tumours , catecholamine in pheochromocytoma
• (III) Determining the Prognosis (Outlook) for Certain Cancers
• ex. CA125 in ovarian cancer
• (IV) Determining the Effectiveness of Cancer Treatment
• One of the most important uses for tumour markers is to monitor patients being treated for cancer. If the initially raised tumour marker level goes down with treatment, it indicates that the treatment is working and is having a beneficial effect. On the other hand, if the marker level goes up, then the treatment is probably not working and change of treatment should be considered.
• (V) Detecting Recurrent Cancer
• Markers are also used to detect cancers that recur after initial treatment. Some tumour markers can be useful once treatment has been completed and with no evidence of residual cancer left. These include PSA (for prostate cancer), HCG (for gestational trophoblastic tumours & germ cell tumours of ovaries & testicles), and CA 125 (for epithelial ovarian cancer).
Examples of Markers In Use
Alpha-fetoprotein (AFP) • Elevated in hepatocellular carcinoma of liver and is useful to monitor response to treatment .
• AFP is also elevated in certain testicular cancers (embryonal cell & endodermal sinus types).
CA125
• CA 125 is the standard tumour marker to follow patients with epithelial ovarian cancer during or after treatment.
• CA 125 can also be raised in patients with endometrial and pancreatic cancer as well as in benign conditions such as endometriosis, pelvic inflammatory disease and benign ovarian cysts.
CA19-9
• CA 19-9 is considered the best tumour marker for following patients with pancreatic cancer.
• CA 19-9 can also be raised in other cancers such as stomach and bile ducts cancer and in some non-cancerous conditions such as pancreatitis.
Calcitonin
• Calcitonin is a hormone secreted by parafollicular C cells of thyroid.
Carcinoembryonic antigen (CEA)
• CEA is the preferred tumour marker to monitor patients with colorectal cancer during treatment, but it is not useful as a screening or diagnostic test.
• It can also be elevated in non-cancerous diseases and in chronic smokers.