1
hemodynamic 1 DR. LAMIEA pathology
The health of cells and tissue depends not only on an intact circulation to deliver oxygen and
nutrients and to remove wastes but also on normal fluid balance (homeostasis).
Normal homeostasis encompasses maintenance of vessel wall integrity as well as
intravascular pressure and osmolality within certain physiologic ranges.
Hemodynamic Disorders
Edema
Hyperemia and congestion
Hemorrhage
Hemostasis and thrombosis
Disseminated intravascular coagulation
Embolism
Infarction
Shock
Edema
Approximately
60%
of lean body weight is water, of which
2/3
is intracellular,
1/3
extracellular (mainly interstitial), only
5%
of total body water is plasma
Edema
: means pathological accumulation of fluid in the interstitial tissue spaces or body
cavities..
Collection of fluid in the different body cavities are variously designated:
•
Peritoneal cavity
→ ascites (hydroperitoneum)
•
→hydrothorax
Pleural cavity
•
→hydro pericardium
pericardium
•
→ means severe & generalized edema with profound subcutaneous
anasarca
tissue swelling.
2
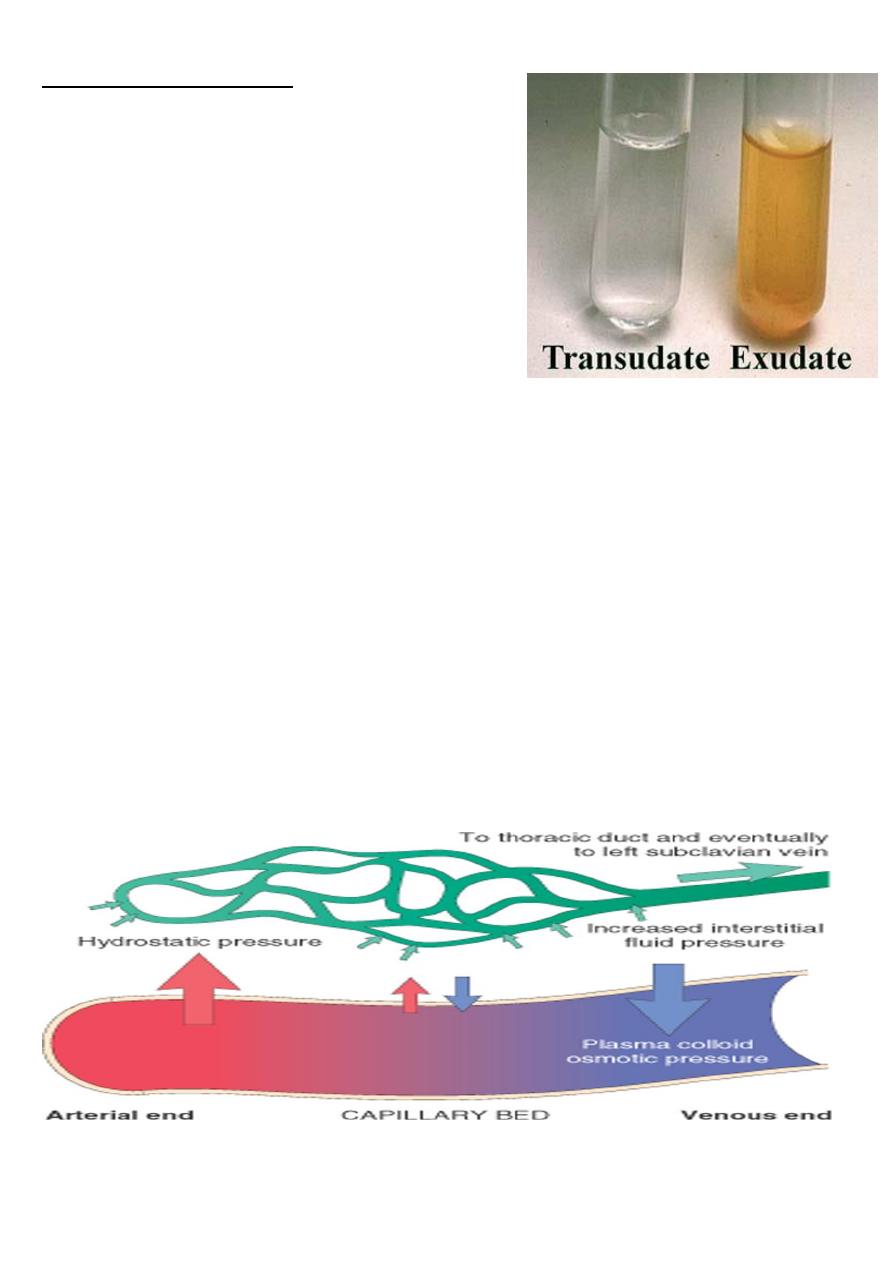
Nature of accumulated fluid:
•
Transudate:
this is serous (thin), protein poor
fluid with specific gravity < 1.012, due to
intravascular
volume or pressure overload or
reduced plasma protein
(e.g. in heart failure,
nephrotic syndrome).
•
Exudate:
it is protein rich fluid, specific gravity
>1.020 due to
↑vascular permeability
leads to
escape of intravascular fluid with protein
especially albumin.
e.g. in inflammation.
There are
2 opposing factors
which govern the movement of the fluid between vascular &
interstitial spaces:
•
hydrostatic pressure
(intravascular pressure) encouraging the passage of fluid through
the capillary wall to the extra vascular compartment.
•
osmotic pressure
(plasma protein) encourages the↑ retention of the fluid to the
capillaries .
Normally
, At the arterial end the hydrostatic pressure is greater than the osmotic
pressure → fluid is forced out the capillaries , of the microcirculation.
The reverse occurs at the venous end & the fluid is attracted into the vessels.
So the exit of fluid into the interstitium from the arteriolar end of the microcirculation is
nearly balanced by inflow at the venular end; a small residual amount of excess interstitial
fluid is drained by the lymphatics, then to the blood stream via thoracic duct
Factors affecting fluid transit across capillary walls
3
Pathophysiology of edema(causes):
Edema results from:
1. Increased hydrostatic pressure.
2. Reduced plasma osmotic pressure (hypoproteinemia).
3. Lymphatic obstruction.
4. Sodium and water retention.
5. Increased capillary permeability.
1-Increased hydrostatic pressure
a. Generalized edema:
It occurs most commonly in
congestive heart failure (CHF
), affecting Rt. ventricular function.
The heart fails to pump the blood, that is received from the Rt atrium, this causes
accumulation of blood that is reflect back into the systemic veins, as an increase in systemic
venous pressure → generalized chronic venous congestion, this
↑
in
hydrostatic pressure
elicits edema formation.
CHF is associated with ↓ cardiac output and therefore reduced renal perfusion → stimulate
renin –angiotensin -aldosterone axis , inducing
Na+ and water retention
by the kidney
(secondary aldosteronism).
This mechanism normally functions to ↑intravascular volume and
improve cardiac out put
to
restore normal renal perfusion
, however if the condition untreated the extra fluid load causes
increased venous pressure and eventually ↑ edema .
B.Localized edema :
As a result of impared venous return →↑ intravascular pressure → transudation of fluid e.g.
**deep venous thrombosis(DVT)→edema restricted to the affected leg .
**during pregnancy due to pressure on the veins by the gravid uterus → edema of the legs.
**acute Lt ventricular failure →acute pulmonary edema.
2-reduced plasma osmotic pressure:
(Hypoproteinemia)
Reduced plasma osmotic protein→ movement of fluid into the interstitial tissue (edema).
4
Reduced plasma volume→↓renal perfusion → 2'ry aldosteronism (Na+ and water retention)
and edema precipitated by low protein is exacerbated by 2'ry Na+ and water retention.
Causes of reduced plasma oncotic pressure::
1) protein malnutrition as in kwashiorkor.
2) Malabsorption
3) reduced albumin synthesis as in liver cirrhosis.
4) excessive loss of albumin e.g. nephrotic syndrome, also in protein – losing
gastroenteropathy.
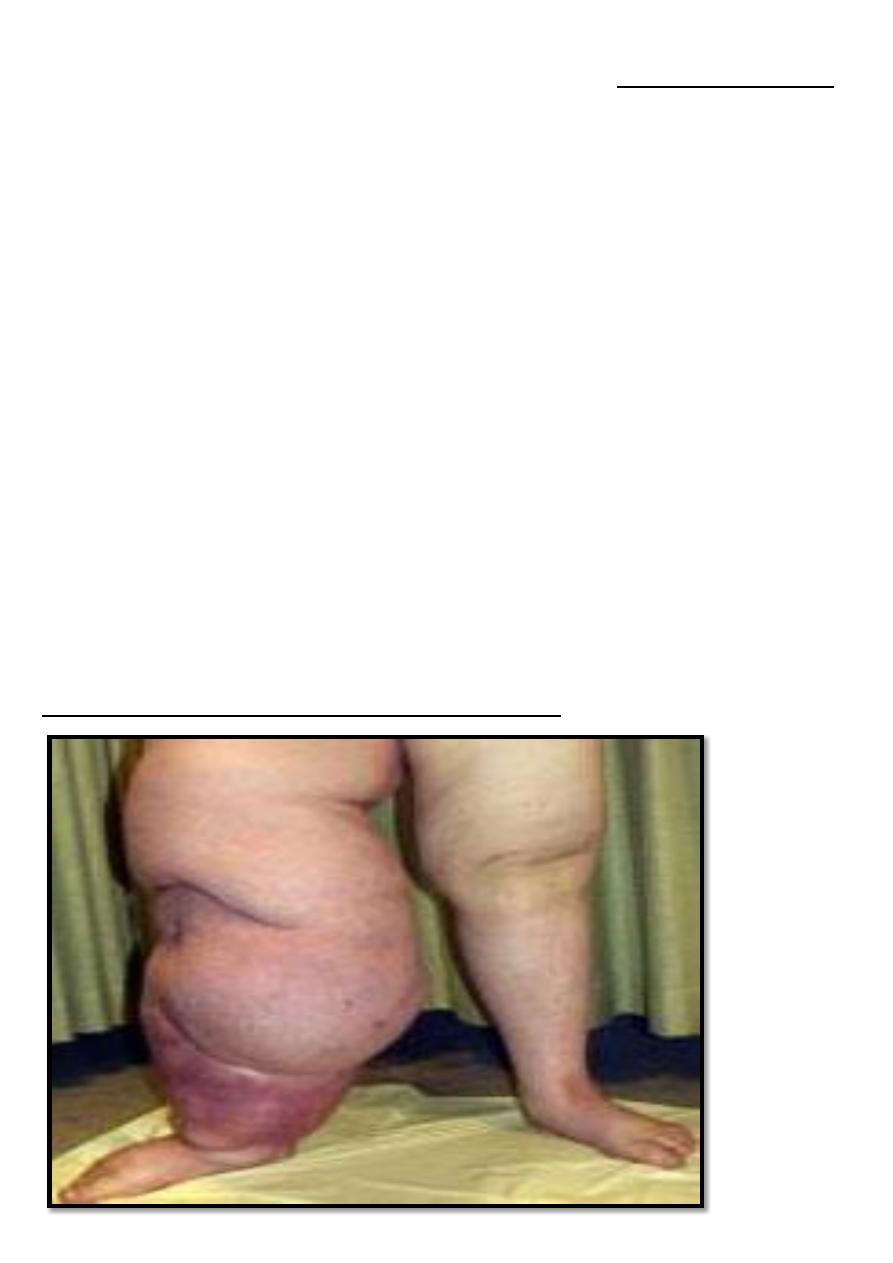
3-lymphatic obstruction
:
Impaired lymphatic drainage to area of the body →localized
edema of the affected part (lymphedema). It is characteristically a
non pitting edema
. Causes:
*inflammation: certain parasitic infestation
e.g. filariasis →fibrosis of lymphatic vessels & L.N.
of the inguinal region → edema of external genitalia &lower limbs (elephantiasis).
*tumor invasion
e.g. in carcinoma of breast → infiltration & obstruction of superficial
lymphatics → edema of overlying skin → "peau d 'orange“.
*
resection of lymphatic channels or scarring related to
surgery
and
radiation
.
Lymphadema : (elephantiasis) non pitting edema of the legs

5
4. Sodium and water retention
: e.g. acute renal failure and acute poststreptococcal
glumerulonephritis.
5. increase capillary permeability
: e.g. inflammation.
Morphology
:
Grossly : the edema is most easily recognized .
Microscopically →edema fluid generally manifested as subtle cell swelling with clearing
&separation of the extracellular matrix elements
Although any organ or tissue may be involved,
edema most commonly encountered in
subcutaneous tissues lungs
,
and
brain
.
Subcutaneous edema:
it can be:
**
dependent edema :
edema more prominent in depended part of the body, the region with
highest hydrostatic pressures (influenced by gravity) e.g. HF (Rt side HF) (in the legs when
standing, in the sacrum when recumbent),
**
diffuse edema:
Generalized and more severe edema, is usually due to renal failure or
nephrotic syndrome.
Finger pressure over significantly edematous subcutaneous tissue will displace the interstitial
fluid and leaving a finger-shaped depression (pitting edema)
6
Pulmonary edema:
Is a common clinical problem and frequently follow Left side heart failure.
The lungs are typically 2-3 times their normal weight. On sectioning frothy, sometimes blood-
tinged fluid representing a mixture of air and edema fluid and extra-vasated RBCs.
Clinical Consequences of edema:-
1. Subcutaneous tissue edema is important primarily because it signals potential underlying
cardiac or renal disease; however, when significant, it can also impair wound healing or
the clearance of infection.
2. Pulmonary edema Not only does fluid collect in the alveolar septa around capillaries and
impede oxygen diffusion, but edema fluid in the alveolar spaces also creates a favorable
environment for bacterial infection.
3. Brain edema is life-threatening; if severe, brain substance can herniate (extrude) through
the foramen magnum, or the brain stem vascular supply can be compressed. Either
condition can injure the medullary centers and cause death
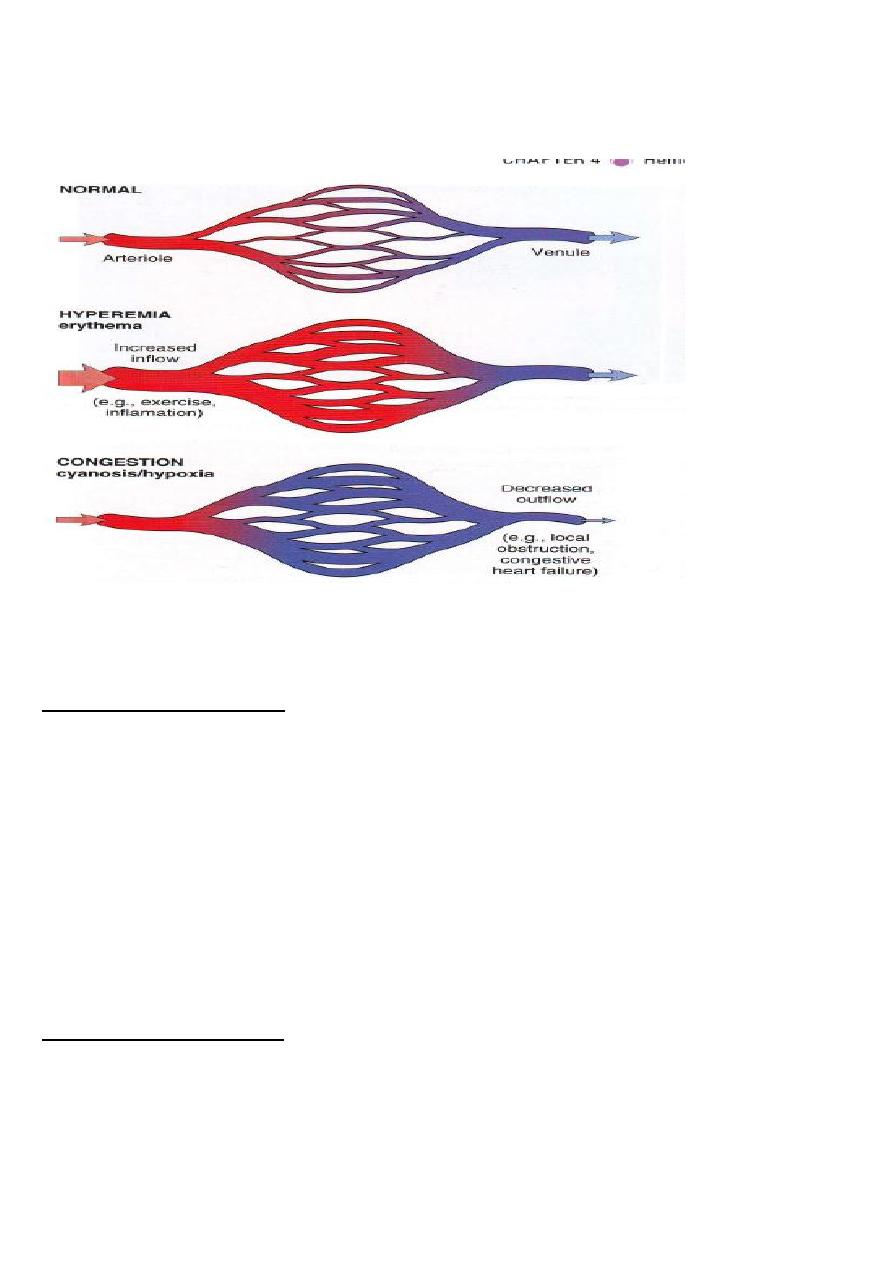
Hyperemia and congestion
Both terms indicate a local increased volume of blood in a particular tissue.
Hyperemia
• It is an active process.
• resulting from augmented blood flow due to arteriolar dilation.
• the affected tissue is redder than normal because of engorgement with oxygenated blood.
e.g. - physiological as in skeletal muscle during exercise
- pathological as in acute inflammation
Congestion :
• it is a
passive
process
• resulting from partial
obstruction
to the
venous return from a tissue.
• the tissue has
blue –red color (cyanosis)
due to accumulation of
deoxygenated blood
in
the affected tissue.
Morphology:
Grossly, the cut surface is hemorrhagic and wet.
Microscopically, there is engorgement of capillaries by blood.
7
Hyperemia and congestion
General venous congestion:
Where the whole venous return is impaired by chronic obstructions. Combined Rt and Lt
sided heart failure(CHF) causes systemic congestion, Rt sided heart failure alone causes also
systemic congestion but here the lungs are spared.
Causes of Rt sided heart failure:
1. Lt sided heart failure, as it eventually leads to Rt sided heart failure.
2. Chronic obstructive airway disease such as emphysema, chronic bronchitis.
3. Pulmonary valve disease e.g. stenosis and /or incompetence.
Local venous congestion:
Follows mechanical interference with the venous drainage from an organ e.g.
---pulmonary congestion occurs in mitral stenosis, Lt sided heart failure, systemic
hypertension.
---thrombosis of the vein as in deep venous thrombosis (DVT).

8
--- mechanical compression of the veins by tumor or bandage, strangulated hernias, volvulus
of intestine
venous
congestion
→
edema
then may →
ischemic necrosis
.
