
Hemodynamic Patho. Lec. 3
Disseminated Intravascular Coagulation (DIC),
It is a sudden or insidious onset of widespread thrombi formation in the micro-circulation,
which are causing diffuse circulatory insufficiency, especially in brain, lungs, heart and
kidneys.
The multiple thrombi will lead to rapid consumption of platelets and coagulation proteins
(consumption coagulopathy) that results in activation of fibrinolytic mechanisms.
So, a thrombotic disorder evolves into a serious bleeding disorder.
DIC is not a primary disease but rather a potential complication of many conditions (e.g.
obstetric complications, infections, advanced malignancy, massive tissue injury).
Embolism:
Is a detached intravascular solid, liquid, or gaseous mass that is carried by the blood to a
site distant from its point of origin with subsequent impaction .
The site of impaction depends on the source of the embolus.
The potential effect of embolism is ischemic necrosis (infarction).
There are many types of emboli:
1. Thrombo-embolism (99%).
2. Fat.
3. Gas (air, nitrogen).
4. Amniotic fluid.
5.Atherosclerotic debris.
6. Tumor fragments.
7. Bone marrow.
8. Foreign body (bullet).
Pulmonary thrombo-embolism:
In more than 95% of instances, venous emboli originate from DVT, (above the level of the
knee).
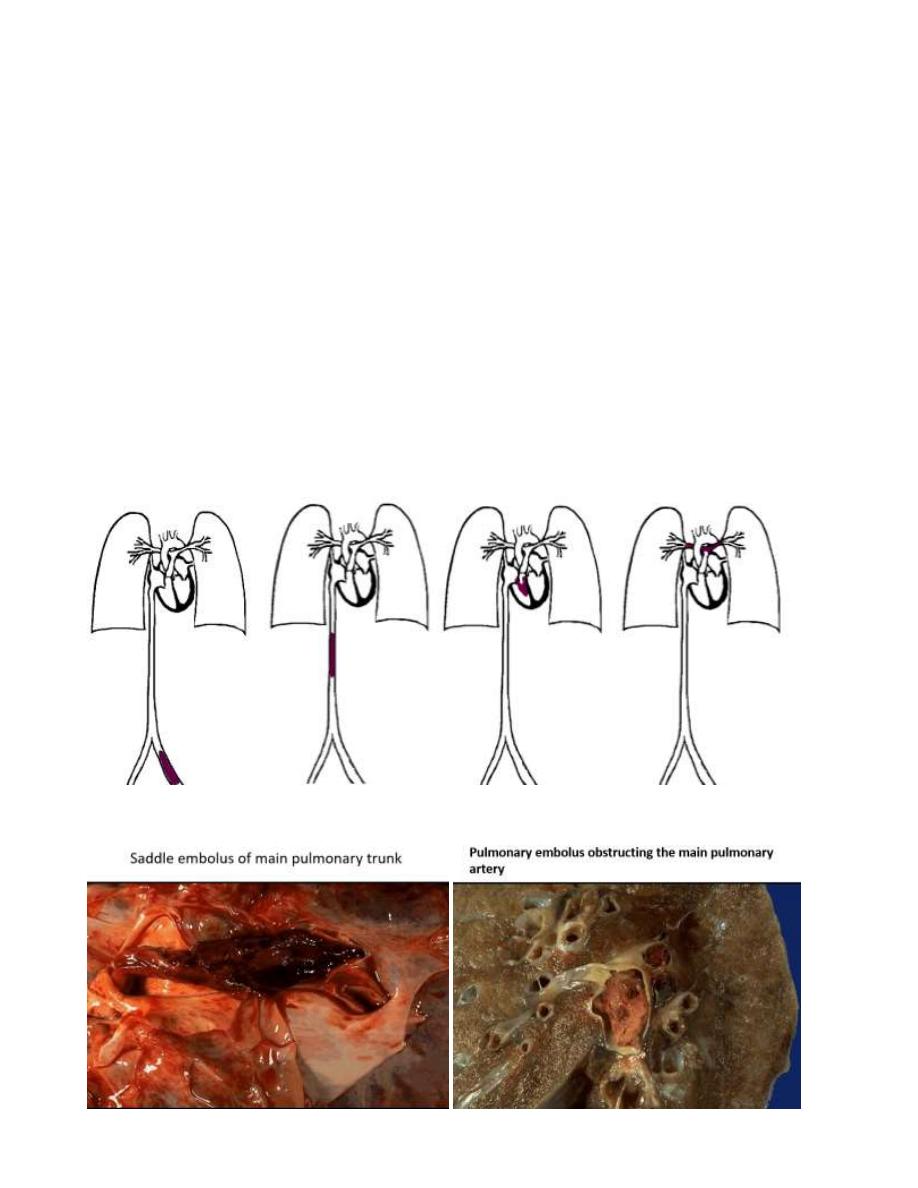
Depending on the size of the embolus:
1. It may occlude the main pulmonary artery.
2. Impact across the bifurcation (saddle embolus).
3. Or pass out into the smaller branching arterioles. Frequently there are multiple emboli.
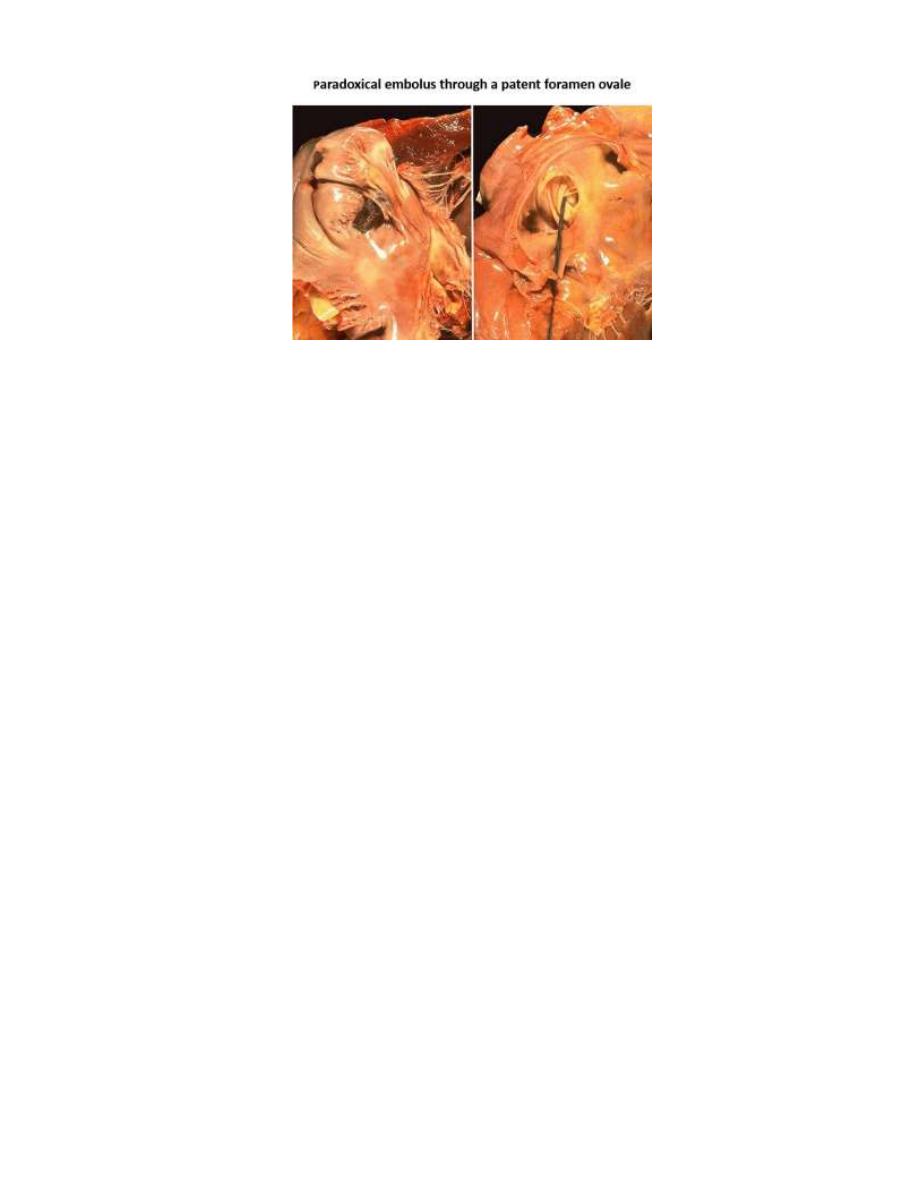
Rarely, an embolus may pass through an inter-atrial ( patent foramen ovale) or inter-
ventricular defect to gain access to the systemic circulation (paradoxical embolism).
Pulmonary embolism
Clinical consequences include:
a) Pulmonary thromboembolism (PTE)
PTE is refers to the impaction of an embolus in the pulumonary arteries & their branches.
Such an embolus is derived from a thrombus in the systemic veins or the right side of the
heart
1. Most pulmonary emboli are silent.
2.Sudden death, cardiovascular collapse or acute Rt. ventricular failure (more than 60% of
pulmonary circulation is obstructed).
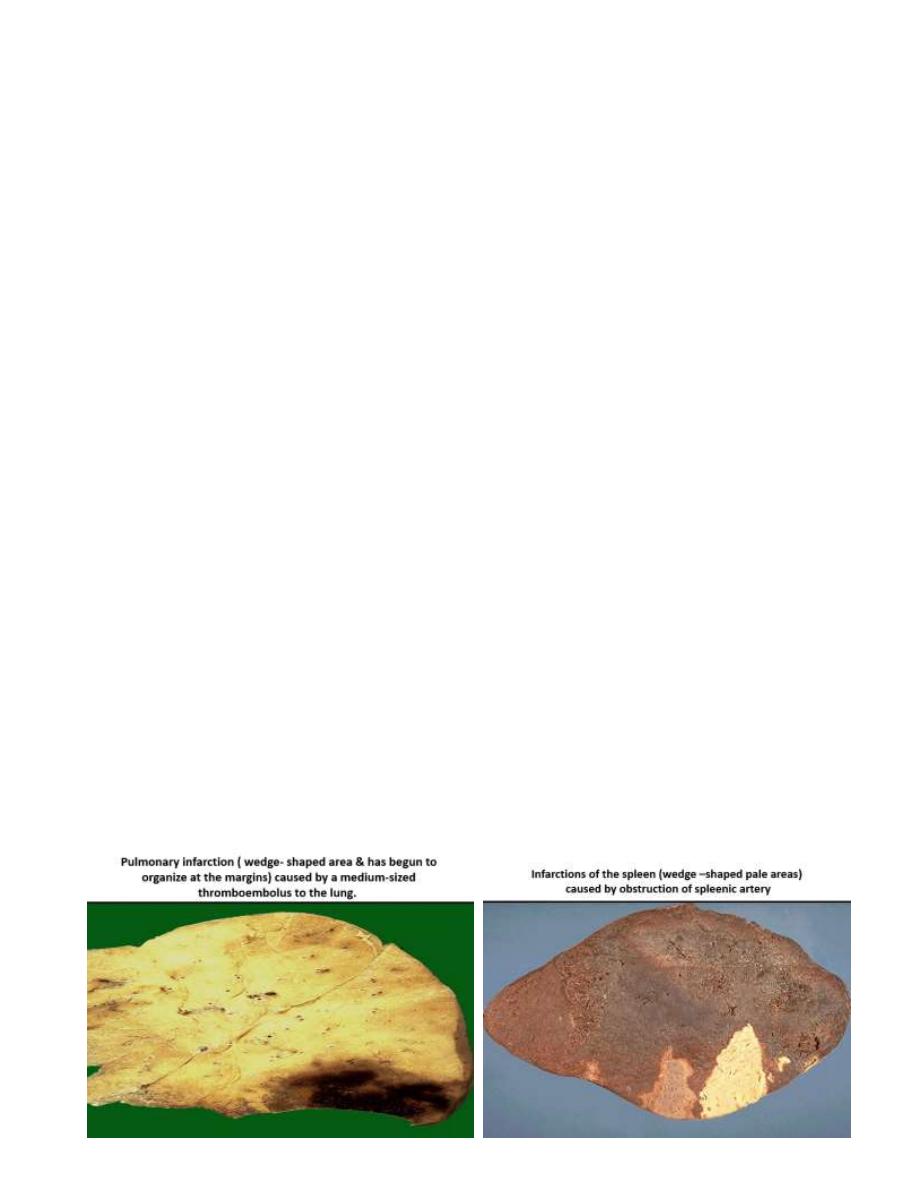
3. Obstruction of medium-sized arteries may result in pulmonary hemorrhage.
4. Obstruction of small end-arterioles result in infarction.
5. Multiple emboli over time → pulmonary hypertension → Rt. ventricular failure.
b) Systemic thromboembolism
Systemic emboli arise from the left side of the heart or from thrombi &atheromatous debris
in large arteries. And they impact in the systemic arteries. They may originate from:
1. Intra-cardiac mural thrombi (about 80% of emboli).
2. Thrombi on ulcerated atherosclerotic plaques
3. Aortic aneurysm.
4. Fragmentation of a valvular vegetation.
5. Very small % from Paradoxical emboli.

The main sites involved are;
In contrast to venous emboli which lodge primarily in the (lung), arterial emboli can travel
to wide variety of sites:
1. Lower extremities (75%).
2. Brain (10%).
3. Intestines.
4. Kidneys.
5. Spleen.
Fat embolism,
it may result from;
1. Fractures of long bones (most common).
2. Soft tissue trauma and burns (rare).
Gas embolism,
Air embolism may enter the circulation during:
1. Obstetric procedures.
2. Chest wall injury.
More than 100 ml of air are required to produce a clinical effect, bubbles can coalesce to
form frothy mass sufficiently large to occlude major vessels.
***Decompression sickness***
Is a particular form of gas embolism occurring in individuals
who are exposed to sudden changes in atmospheric pressure
(deep sea divers). When air is breathed at high pressure,
increased amounts of gas (particularly nitrogen) become
dissolved in the blood and tissues. If the diver ascends
(depressurizes) too rapidly, the nitrogen expands in the
tissues and bubbles out of solution in the blood to form gas
emboli.

Clinically, the diver suffers from;
1. Muscle and joint pain.
2. Infarctions in various tissues.
3. Respiratory distress(chokes).
Amniotic fluid embolism:
Is a grave but uncommon complication of labor.
The underlying cause is the infusion of amniotic fluid or fetal tissue into the maternal
circulation via a tear in the placental membranes or rupture of uterine veins.
1. Sudden severe dyspnea.
2. Cyanosis.
3. Hypotensive shock.
4. Seizure and coma.
5. If the patient survives, pulmonary edema and DIC develop.
Infarction :
It is an ischemic necrosis caused by occlusion of either the arterial supply or the venous
drainage in a particular tissue.
Causes, include:
1. Thrombosis or embolism (99%).
2. Local vasospasm.
3. Expansion of atheroma due to hemorrhage in plaque
4. Extrinsic compression of a vessel e.g. tumor, twisting, edema, hernia).
5. Traumatic rupture of blood supply.
Morphology
Infarcts are classified on the basis of their color and the presence or absence of infection,
into;
1) Red (hemorrhagic).
2) White (anemic)
And 1) Septic.
2) Sterile.
Red infarcts: occur in the following situations;
1. Venous occlusion (ovarian torsion).
2. Loose tissue (lung).
3. Tissues with dual circulation(lung, small intestine).
4. Previously congested tissues.
5. Re-established blood flow to site of necrosis.
White infarcts: Occur in
1. arterial occlusions.
2. solid organs with end-arterial circulation (e.g. heart, spleen, kidney).

Clinical correlation
The development & the size of an infarct are determined by the following factors:
A. The nature of the vascular supply
B. The rate of development of occlusion
C. Suceptibility of the tissue for hypoxia
D. Oxygen content of the blood
E. The severity & duration of ischemia
A.The nature of vascular supply
The following organs have a dual blood supply.
- Lung
→ pulumonary artery
→ Bronchial artery
- Liver
→ hepatic artery
→ Portal vein
• Hand & forearm
→ Radial arteries
→ Ulnar arteries.

The effect of such a dual blood supply is that if there is obsrtuction of one of the arterial
supplies, the other one may offset the rapid occurrence of infarction in these organs unlike
the renal & splenic circulations which have end arterial supply.
Infarction caused by venous thrombosis is more likely to occur in organs with single venous
outflow channels, such as testis &ovary.
B: Rate of development occlusion
Slowly developing occlusions are less likely to cause infraction since they provide time for
the development of collaterals.
C: Tissue suceptibility to hypoxia:
The susceptibility of a tissue to hypoxia influences the likelihood of infarction. Neurons
undergo irreversible damage when deprived of their blood supply for only 3 to 4 minutes.
Myocardial cells die after 20-30 minutes of ischemia. Fibroblasts are more resistant,
especially those in the myocardium.
D: Oxygen content of blood
Partial obstruction of the flow of blood in an anaemic or cyanotic patient may lead to tissue
infarction.
E: The severity & duration of ischemia
