1
Hepatitis Viruses
اﻟﻤﺮﺣﻠﮫ اﻟﺜﺎﻟﺜﮫ
/
ﻓﺎﯾﺮوﺳﺎت
د. اﻧﺘﻈﺎر ﻋﻼوي ﺟﻌﻔﺮ / ﻓﺮع اﻻﺣﯿﺎء اﻟﻤﺠﮭﺮﯾﮫ / ﻛﻠﯿﮫ اﻟﻄﺐ / ﺟﺎﻣﻌﮫ ذي ﻗﺎر
PhD. M.Sc. Microbiology
Introduction
Hepatitis is a clinical syndrome caused by many pathogens including viruses.
There are six medically important viruses that are called hepatitis viruses
because their main site of infection is liver. These viruses are hepatitis A virus
(HAV), hepatitis B virus (HBV), hepatitis C virus (HCV), hepatitis D virus
(HDV), hepatitis E virus (HEV), and newly described G virus (HGV).
Although these viruses infect the liver as common target organ, they however,
differ greatly in their morphology, replication pattern, and course of infection.
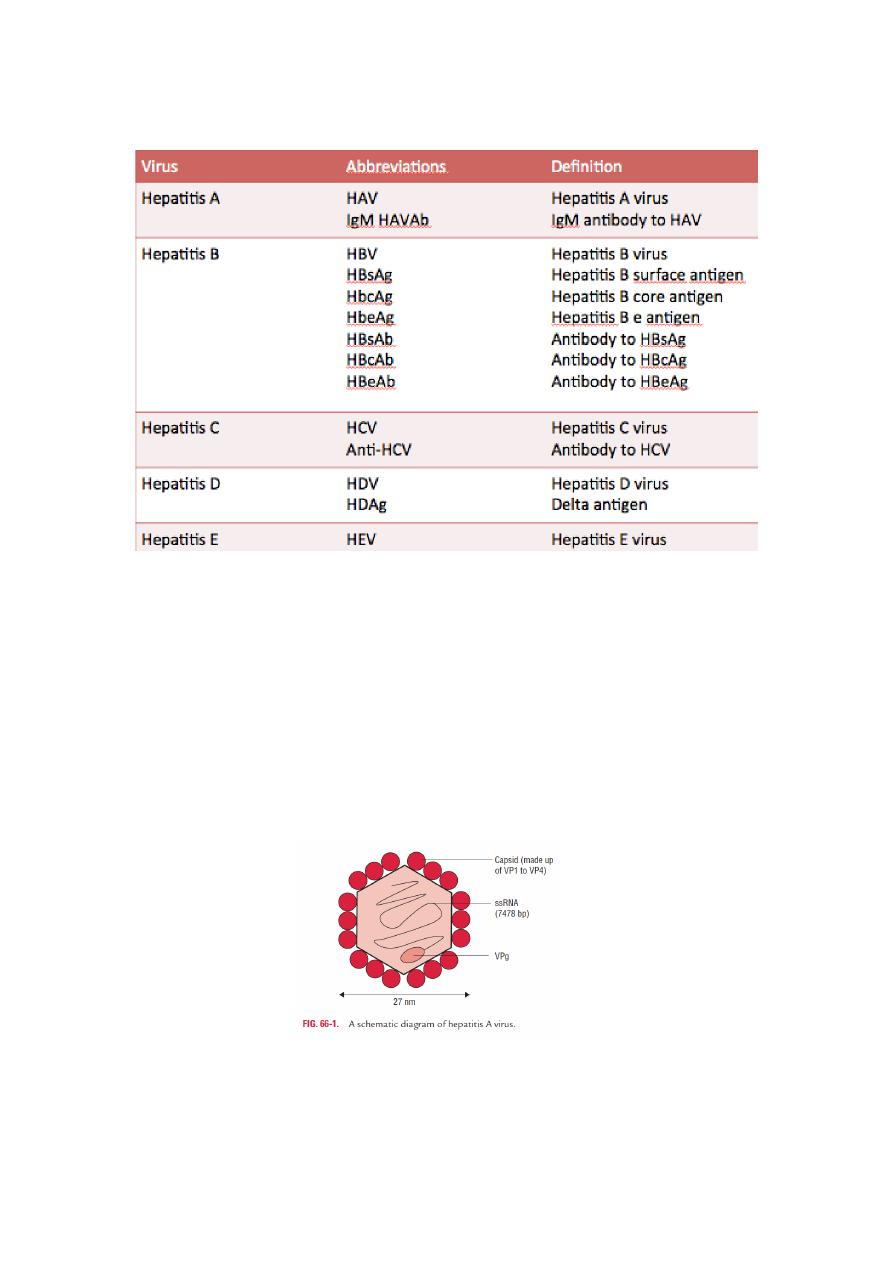
Nomenclature and definitions of different hepatitis viruses, antigens, and
antibodies are listed in Table 1&2.
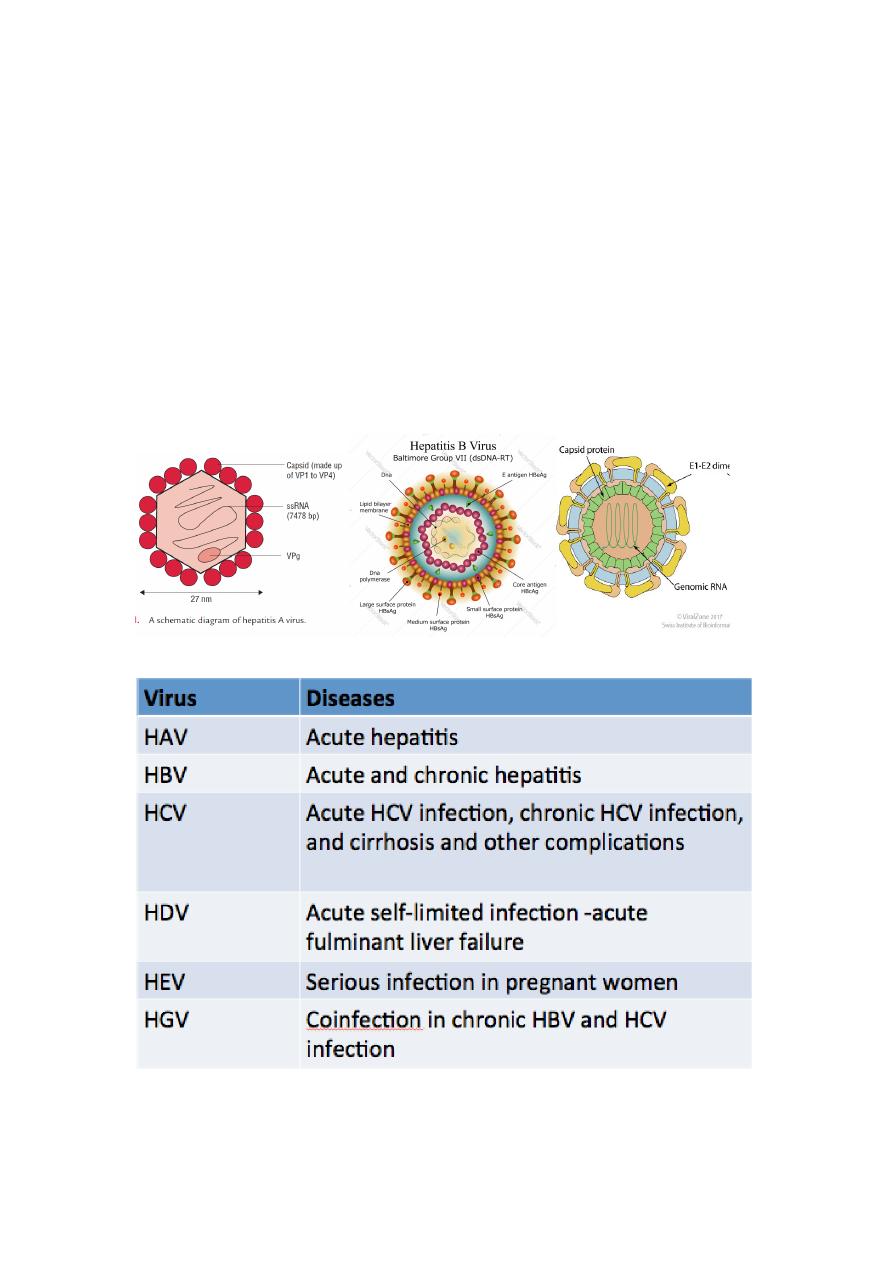
Table 1:Diseases associated with hepatitis viruses
2
Table 2: Nomenclature and definitions of hepatitis viruses, antigens, and
antibodies.
These viruses infect the liver and cause distinct clinical pathology by producing
characteristic symptoms of jaundice and production and release of liver enzymes
in the serum. Most of these diseases spread very fast because infected
individuals are contagious not only during stage of manifestation of the disease
but also during the phase of incubation.
Hepatitis A Virus
Hepatitis A virus (HAV) is a picornavirus that is most commonly transmitted by
fecal–oral route. It has an incubation period of 3–4 weeks after which jaundice
starts suddenly. It is unique in that it does not cause chronic disease or fatal
disease. Humans are only natural host.

3
Morphology
Is a typical enterovirus in the family Picornaviridae, a small, non
enveloped virus measuring 27 nm in diameter. It has a single-stranded positive-
sense RNA genome (See-Figure).
Viral replication
•
Hepatitis A virus replicates in the cytoplasm of the infected cell.
•
Briefly, it combines specifically with a receptor expressed on liver cells
and few other cells. However, unlike other picornaviruses, It is not
cytolytic and is released by exocytosis.
Pathogenesis and Immunity
The virus appears to replicate first in the gastrointestinal tract and then spreads
to the liver. The viruses in the liver infect hepatocytes and cause damage to
hepatocytes.
But the mechanism by which HAV causes cytopathic effect is not known.
Cytotoxic T cells appear to cause damage to hepatocytes; hence once the
infection is cleared, the cell damage is repaired and no chronic infection occurs.
The classic findings in the hepatocytes include mononuclear infiltrate,
ballooning, degeneration, and acidophilic bodies.
The liver pathology caused by HAV cannot be distinguished histologically from
that caused by other hepatitis viruses.
Clinical Syndrome
Acute hepatitis A
The incubation period of HAV is 15–45 days, with an average of 4 weeks. It is
relatively short compared to long incubation period of HBV infection.
•
Fatigue, nausea, vomiting, fever, hepatomegaly, jaundice, anorexia, and
rash are the most common signs and symptoms of the disease. The
condition is also associated with passing of dark-colored urine, pale feces,
and elevated serum transaminase levels.
•
HAV infection is usually a self-limiting mild disease and in most cases
resolves spontaneously in 2–4 weeks. HAV infection confers lifelong
immunity to HAV.
Chronic hepatitis or chronic carrier state does not occur with HAV infection.
Hepatitis A virus also never causes hepatocellular carcinoma. Acute hepatitis
A is relatively more serious and has high mortality in adults than in children.
The exact cause for this is unknown. Acute liver failure and cholestatic
hepatitis are some of the rare complications.

4
The mortality caused by HAV is very low, approximately 0.01%.
Reservoir, source, and transmission of infection
•
Humans are the reservoirs for HAV.
•
Contaminated food or water is the main source of infection.
•
Wide outbreak can occur from a single contaminated source, such as
uncooked vegetables, infected shellfish, and contaminated food and
water.
Treatment :
No antiviral therapy is available against HAV infection. Treatment
of the condition is always supportive.
Prevention
(
a ) Vaccines.
(b ) Prophylaxis with immune serum globulin.
(c ) Measures to prevent feco-oral spread of infection.
Inactivation of HAV.
•
The virus is inactivated by formalin (0.35%) at 37°C during a period of 24
hours.
•
By treatment with peracetic acid (2%) for 4 hours.
•
Beta-propiolactone (0.25%) for 1 hour.
•
It is also inactivated by exposure to ultraviolet radiation.
•
The virus is inactivated by routine chlorine treatment of drinking water.
Hepatitis A virus is highly resistant to environmental factors.
•
It is stable at 60°C for 1 hour, 56°C for 30 minutes, and 4°C for weeks.
•
It is stable to acidic pH, at pH 1.
•
It is resistant to inactivation by lipid solvents, such as ether and
chloroform, to action of detergents, and to drying.
Laboratory Diagnosis
•
Specimens These include:
a) Serum for antibody detection test.
b) Liver, bile, stool, and blood for HAV antigen and genome.
1-Direct antigen detection
HAV is present in stools during 2 weeks prior to the onset of jaundice and up to 2
weeks after the onset of jaundice. The virus can be demonstrated in the stool
during this period by using immunoelectron microscopy.
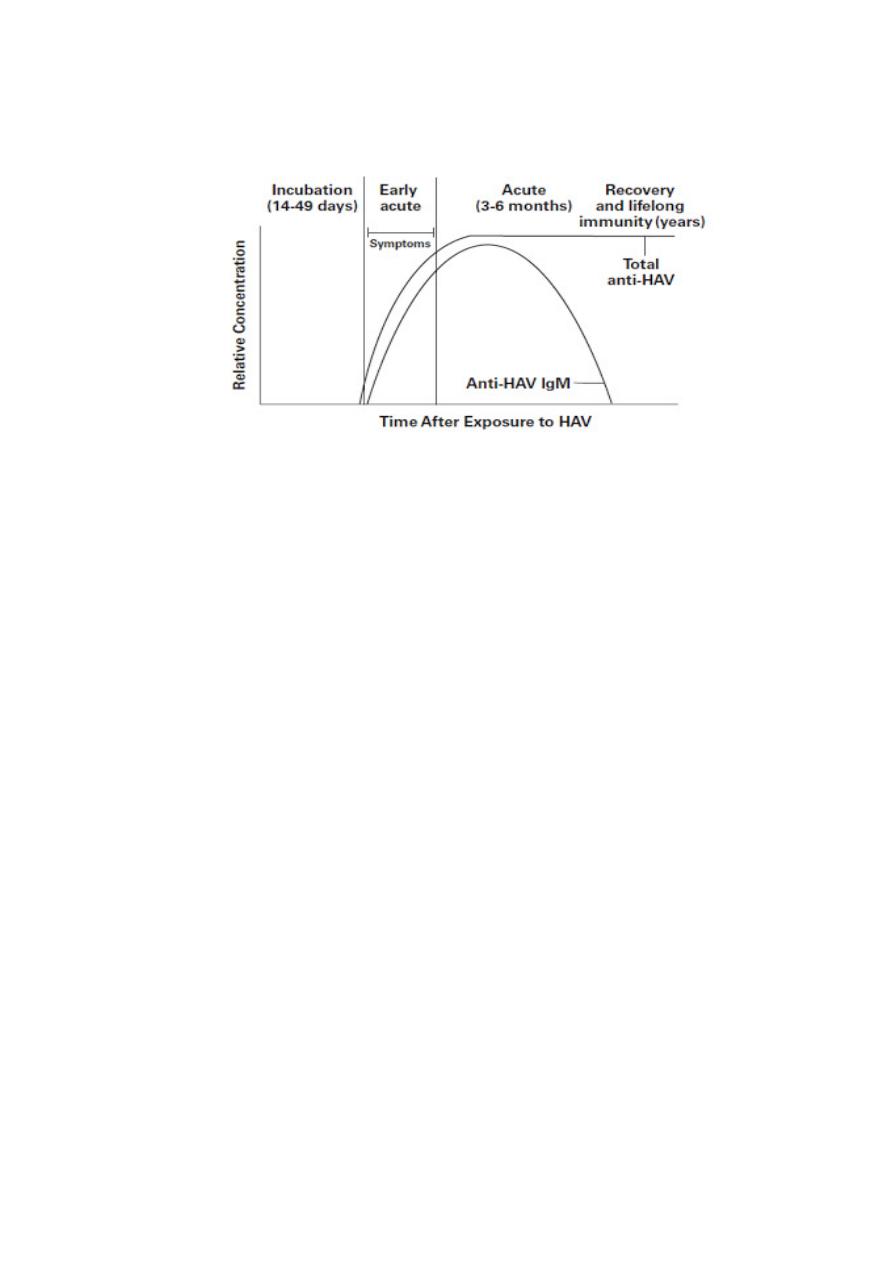
2-Serodiagnosis
Serological tests demonstrating these anti-HAV antibodies in the serum are the
most widely used to confirm the diagnosis of HAV infection.
Enzyme-linked immunosorbent assay (ELISA) is the method of choice for
detection of IgM and IgG antibodies in the serum.
IgM antibody is the first antibody to appear at the onset of symptoms and
continues to persist at a high level for 1–2 months. It usually disappears by 4–6
months but occasionally persists longer. Hence, demonstration of IgM antibody
is diagnostic of a recent infection. IgG antibody appears in the serum shortly
after the appearance of IgM antibodies and usually increases as the IgM level
decreases. A fourfold rise in IgG antibody titers is also diagnostic of infection. See
Fig
5
Laboratory testing for IgM anti-HAV is typically positive at the time of onset of
symptoms (detectable 5/6 days prior to onset of system). It remains positive for
3-6 months after primary infection.
3-Molecular Diagnosis
DNA probes and polymerase chain reaction (PCR) are used to demonstrate HAV
genome in stool as well as in the serum of infected patient.
6
Hepatitis B Virus (HBV)
Hepatitis B virus is a major cause of infectious hepatitis worldwide. It is a
hepadnavirus, which shows restricted host range and limited tissue tropism. The
virus usually causes chronic disease and is associated with hepatocellular
carcinoma.
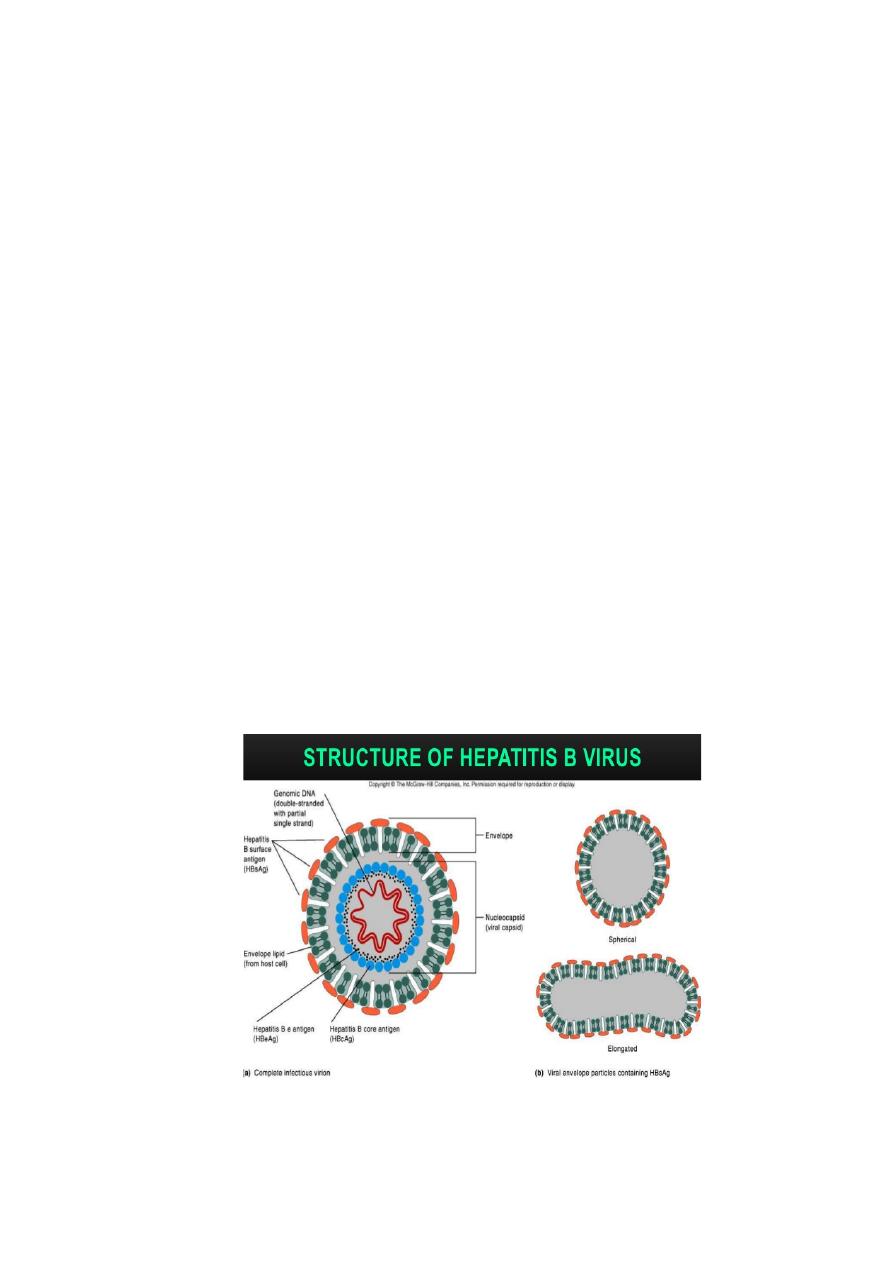
Morphology
•
HBV shows following features:
•
It is a small (3.2 kb), enveloped DNA virus.
•
The genome is a small, circular, partially double-stranded DNA.
•
It is partially double stranded, because its positive strand is incomplete.
The complete negative strand possesses four genes: genes S, C, P, and X.
The gene S codes for HBsAg and also for HBeAg (hepatitis B e antigen).
The virion is a double-walled, spherical structure and measures 42 nm in
diameter. By EM three types of particles can be seen in the serum from patients
with hepatitis B. These are
(i) Spherical particles measuring 22 nm in diameter.
(ii)Filamentous or tubular particles with a diameter of 22 nm and of varying
length.
(iii) Double-walled, spherical structures measuring 42 nm in diameter.
The former two particles are antigenically identical and are known as hepatitis B
surface antigen , or HBsAg. The latter particle is the complete hepatitis viral
particle known as Dane particle
The HBV consists of nucleocapsid which surrounds HBV DNA and DNA
polymerase with reverse transcriptase and ribonuclease activity. The
nucleocapsid also encloses a protein attached to genome, which is surrounded by
hepatitis B core antigen (HBcAg). The envelope which encloses the virus consists
of HBsAg and also HBeAg.
7
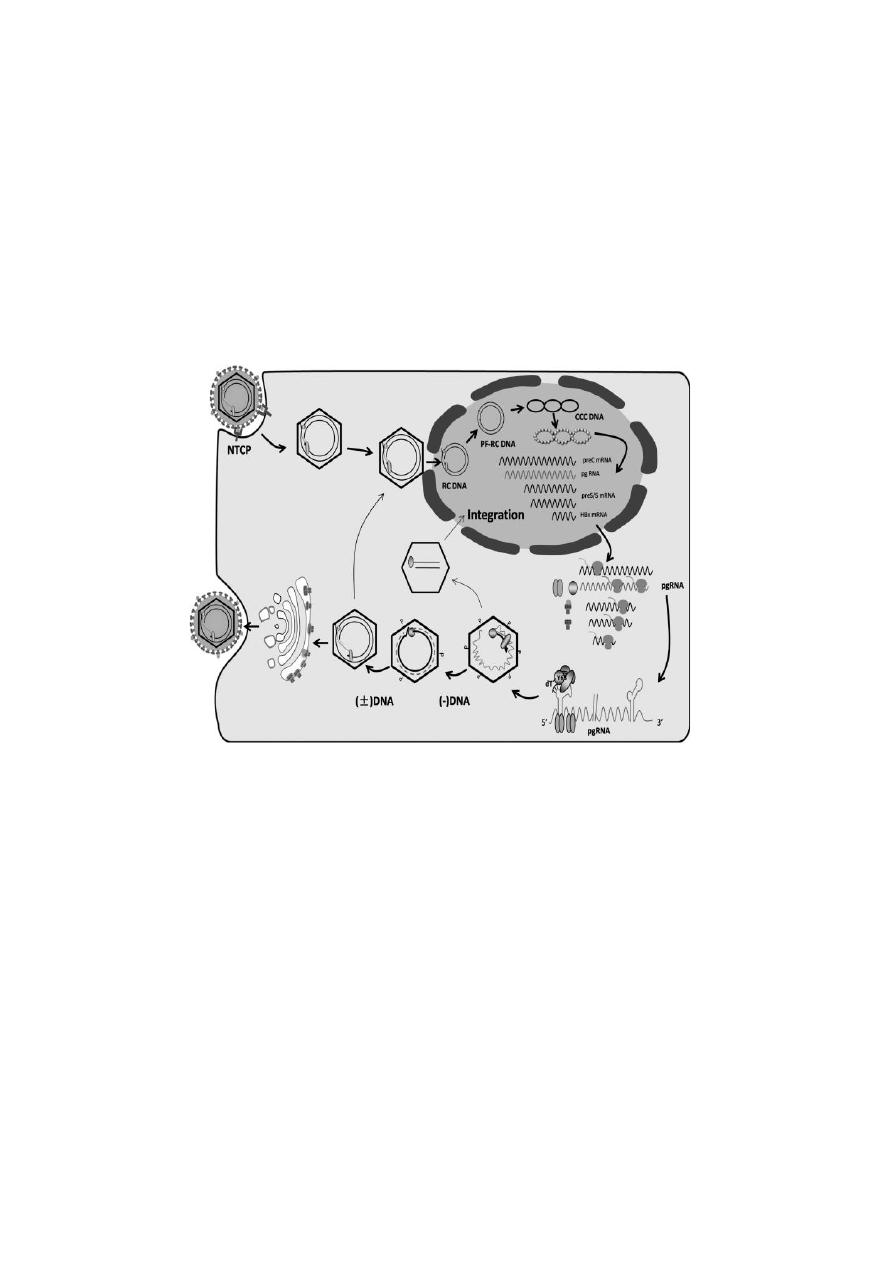
Hepatitis B virus replication
It shows many unique features.
•
First, the virus shows a well-defined tropism for replication in the liver.
•
Second, although a DNA virus, it encodes reverse transcriptase and
replicates though RNA intermediates.
The virus replicates in the nucleus of the cell. The virus infects hepatocytes, the
attachment of which is mediated by HBsAg glycoprotein. The infection is
initiated by the binding of HBsAg to serum albumin and other serum proteins,
which subsequently causes the virus to infect the liver. Inside hepatocytes, the
partial DNA strand of the genome is converted to covalently closed circular
double-stranded DNA (ccc DNA). Later on, this genome is transported to the
nucleus of the cell.
Antigenic and genomic properties
•
HBsAg is antigenically complex. The HBsAg glycoprotein contains a
group-specific antigen termed a and type-specific antigens termed d or y
and w or r. Combination of these antigens results in four major subtypes
of HBV (adw , adr , ayw , and ayr ).
•
These subtypes show distinct geographic distributions: Subtype ayw is
common in Asia, Middle East, and western and northern India.
•
Total of eight genotypic variants (genotypes A, B, C, D, E, F, G, and H) of
HBV have also been described. The prevalence of different genotypes
varies in different countries.
Other virus properties
•
HBV is sensitive to higher temperature and is killed rapidly after heating
at 100°C for 1 minute and at 60°C for 10 hours.
•
HBsAg is also destroyed by treatment with 0.5% sodium hypochlorite
within 3 minutes.
•
The HBsAg is, however, not destroyed by ultraviolet irradiation of plasma
or other blood products, thereby retaining the infectivity of the virus.

8
Pathogenesis of HBV infection
HBV, after entering the blood, infects the hepatocytes in the liver with the
expression of viral antigen on the surface of infected cells. Cytotoxic T cells, such
as activated CD4 and CD8 lymphocytes, recognize various HBV-derived proteins
present on the surface of hepatocytes resulting in an immunological reaction.
A chronic carrier stage with HBV infection is an important event in the
pathogenesis of HBV infection. A person with chronic carrier stage has HBsAg
persisting in the blood for at least 6 months. This stage is caused by a persistent
infection of the hepatocytes that leads to the presence of HBV and HBsAg in the
blood. This chronic carrier stage occurs in about 5% of patients with HBV
infection.
During the chronic stage, the HBV DNA is present in the cytoplasm of
persistently infected cells, and in some cells the viral DNA is integrated with
cellular DNA.
•
Chronic carrier state is more likely to occur when infection occurs in a
newborn than in adult. It has been observed that
•
approximately 90% of the infected neonates become chronic carriers.
•
Approximately 20% of HBsAg carriers, nearly 1% of all adult patients
infected with HBV, and high percentage of neonates infected with the
virus progress to develop hepatocellular carcinoma or cirrhosis.
•
Very Important!!!
•
The hepatocellular carcinoma appears to be the result of persistent
cellular regeneration that tends to replace the dead hepatocytes. Also it is
suggested that the integration of HBV DNA with hepatocytes DNA could
activate a cellular oncogene, resulting in loss of control of the growth of
hepatocytes. However, the HBV genome has no oncogene which can be
responsible directly for causing hepatocellular carcinoma.
Key Points
•
The virus by itself does not cause any cytopathic effect in the infected
liver cells.
•
The injury or cytopathic effects most probably occur as a result of cell-
mediated injury.
•
The formation of antigen–antibody complexes is responsible for some of
the symptoms, such as arthralgia, arthritis seen during early stage of the
disease.
•
Hepatitis B virus natural infection induces a lifelong immunity.
Clinical Syndromes
•
Hepatitis B virus is one of the most important causes of acute and chronic
hepatitis. The clinical manifestations vary from subclinical hepatitis to
symptomatic and icteric hepatitis. The incubation period varies from 6
weeks to 6 months.
•
The clinical manifestations of HBV infection depend on
•
(a) age of infection
•
(b ) immune status of the host.
•
(c ) the level of HBV.

9
Acute hepatitis B virus infection
Is characterized by
•
Gradual onset of anorexia, malaise, and fatigue.
•
During the icteric phase, the liver becomes tender with development of
jaundice.
•
Nausea, vomiting, and pruritus with passing of dark-colored urine are the
symptoms noted in this stage.
Clinical manifestations of acute hepatitis B are similar to that of hepatitis A but
with the difference that the symptoms tend to be more severe and life-
threatening with HBV infection.
Chronic hepatitis B virus infection
Is one of the major complications of HBV infection.
The risk of chronic infection is also higher in
•
Those infected at birth (90%).
•
In patients who are immunocompromised.
Only 5–10% of older children or adults progress to develop chronic infection.
Complications of Hepatitis B virus infection
•
Cirrhosis and hepatocellular carcinoma are the long-term but rare
complications of hepatitis B.
•
Perinatal transmission or infection in children is associated with few or
no symptoms.
•
Fulminant hepatic failure is another major complication of HBV infection.
Patients with chronic HBV infection have a very high risk of developing
hepatocellular carcinoma. The cancer appears to be due to repeated episodes of
chronic inflammation and cellular regeneration. The cancer that develops an
average of 25–30 years after initial infection is the leading cause of cancer-
related deaths in areas where HBV is endemic.
Reservoir, source, and transmission of infection
Individuals with chronic HBV infection are the major reservoir of HBV infections.
These people with HBeAg in their serum tend to have high viral titers and thus
greater infectivity.
Hepatitis B virus is present at a high level in serum. The virions are also present
at very low levels in semen, vaginal mucosa, saliva, and tears, and all are
infectious.
The hepatitis B virus can be transmitted in the following ways:
•
Perinatal transmission: The transmission occurs from infected mother
to child due to contact with mother’s infected blood during the time of
delivery.
•
Although HBV is found in breast milk, the role of breast-feeding in
transmission is unclear.
•
Parenteral transmission: This transmission occurs due to transfusion of
HBV-infected blood and blood products.
•
Sexual transmission of HBV: Hepatitis B virus is transmitted sexually
more easily than Hepatitis C virus (HCV) or Hepatitis D virus (HDV).
Laboratory Diagnosis

10
•
Serodiagnosis:
Diagnosis of acute infection is made by demonstration of
HBsAg as well as HBeAg in the serum. They indicate viral replication.
When viral replication slows, HBeAg disappears and anti-HBeAg is detected.
Hepatitis B surface antibody (HBsAb) produced may persist for many years.
Key Points
•
HBsAg:
•
The antigen appears in blood during incubation period and is detectable
in most patients during acute phase of the disease.
•
Persistent presence of HBsAg in blood for at least 6 months indicates the
carrier state and also indicates the risk of chronic hepatitis and hepatic
carcinoma.
•
Serological Diagnosis of Hepatitis B virus Infection
•
HBsAg and hepatitis B e antigen (HBeAg) are the first markers identified
in the serum of patients acutely infected with HBV.
•
HBeAg is generally considered to be a marker of HBV replication and
infectivity.
Table: Interpretation of common serological markers in HBV infection
HBsAg generally appears before symptom onset and peaks during overt disease.
In patients who successfully clear the HBV infection and do not progress to the

11
chronic carrier stage, HBsAg typically is undetectable 4 to 6 months after
infection.
Molecular Diagnosis
•
HBV PCR for demonstration of HBV DNA is highly valuable to monitor the
treatment of chronic HBV infection with antiviral therapy. This is also
useful to identify HBV as the cause of liver infection in HBsAg-negative
patients.
•
The detection of viral DNA in the serum indicates acute infection.
Other tests
•
These tests include elevation of ALT and AST. High levels are found in
acute hepatitis (1000–2000 IU/mL).
•
Estimation of serum bilirubin indicates the intensity of jaundice.
Treatment
•
No specific antiviral treatment is available for patients with acute HBV
infection. Supportive and symptomatic care continues to be the mainstay
of therapy for most of the patients.
•
Therapy is recommended for patients with chronic hepatitis B infection.
•
Interferon and nucleoside analogs, such as lamivudine, adefovir, and
telbivudine are the antiviral drugs used widely.
•
These antiviral drugs achieve viral suppression as demonstrated by loss
of HBeAg in serum and suppression of HBV DNA.
Vaccines
Hepatitis B is preventable with currently available safe and effective vaccines.
WHO recommends that all infants should receive their first dose of vaccine as
soon as possible after birth, preferably within 24 hours.
The birth dose should be followed by 2 or 3 doses to complete the primary
series.
Hepatitis C Virus
•
Morphology
•
Hepatitis C virus is the only member of the genus Hepacivirus in the
family Flaviviridae of RNA-containing virus.
•
Most patients infected with HCV have chronic liver disease, which
progresses to cirrhosis and hepatocellular carcinoma.
•
It is a spherical, enveloped, 9.4 kb, single-stranded RNA virus with a
diameter of 55 nm. The genome is approximately 9500 base pairs that
encode 10 structural and regulatory proteins.
•
Structural proteins include the core and two envelope proteins, namely,
E1 and E2.
•
The viruses are ether sensitive and acid sensitive.

12
Hepatitis C Virus replication
•
These viruses like other flaviviruses replicate in the endoplasmic
reticulum of hepatocytes.
•
Hepatitis C virus shows a considerable degree of genomic variations.
There are six major genotypes (genotypes 1–6) and numerous subtypes,
which differ, in their worldwide distribution.
•
This genetic variability is the main stumbling block against the effort to
develop an anti-HCV vaccine.
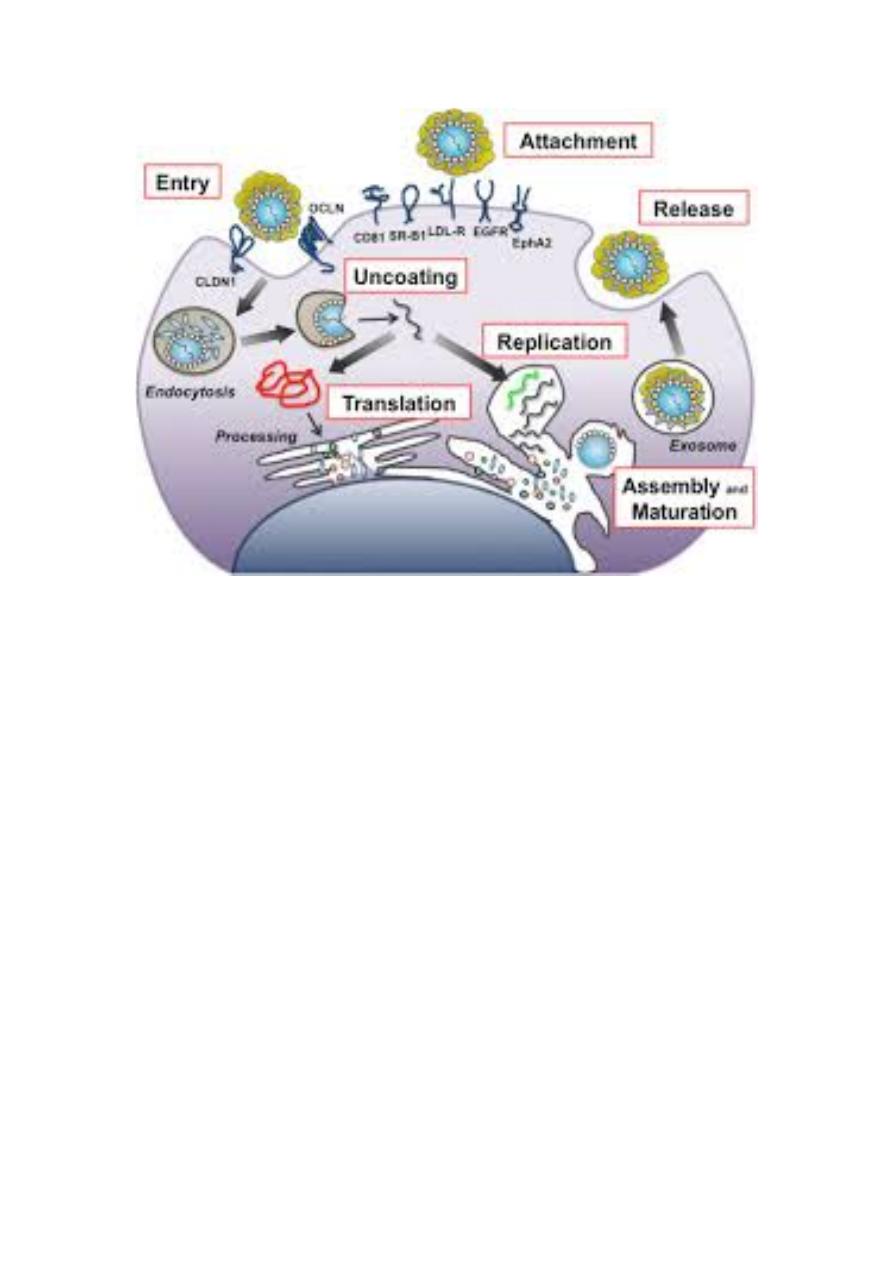
REPLICATION
1-Attachement of the viral envelope protein E to host receptors mediates
internalization into the host cell by endocytosis.
2-The positive-sense genomic ssRNA is translated into a polyprotein, which is
cleaved into all structural and non structural proteins .
3-Replication takes place at the surface of endoplasmic reticulum in cytoplasmic
viral factories. A dsRNA genome is synthesized from the genomic ssRNA(+).
4-The dsRNA genome is transcribed thereby providing viral mRNAs/new
ssRNA(+) genomes.
5-Virus assembly occurs at the endoplasmic reticulum.
6-The virion buds at the ER and is transported to the Golgi apparatus.
7-Release of new virions by exocytosis.
13
Pathogenesis and Immunity
The ability of HCV to remain cell associated and prevent host cell death is the
main determinant of viral pathogenicity, which causes persistent infection in the
liver.
•
Hepatocytes and possibly B lymphocytes are the natural targets of HCV.
•
Chronics hepatitis is characterized by portal inflammation, interphase
hepatitis, and lobular necrosis are the main histopathological features of
chronic hepatitis caused by HCV.
Clinical Syndromes
Hepatitis C virus can cause:
(a ) Acute HCV infection.
(b ) Chronic HCV infection.
(c ) Cirrhosis and other complications induced by hepatitis.
The incubation period of hepatitis C varies from 15 to 60 days with an average
period of approximately 8 weeks.
Hepatitis C resembles hepatitis B in many aspects.
•
One major difference is that it much more frequently produces a
persistent infection (85 %) and, in 70% of cases, develops into a chronic
hepatitis,
•
Resulting in cirrhosis of the liver within 20 years and a hepatocellular
carcinoma (HCC) in a further 10 years. The reason for the high level of
viral persistence is thought to be a pronounced mutability facilitating
evasion of the immune defenses.
14
Diagnosis
•
Diagnosis of hepatitis C is done with antibody immunoassay (EIA) like
ELISA using genetically engineered viral proteins. Western blot can be
used to confirm the result.
•
The RNA can be detected by means of RT-PCR and is the most specific test
for HCV infection and useful in diagnosing acute HCV infections before
antibodies are developed and the course of therapy can be monitored
with quantitative PCR.
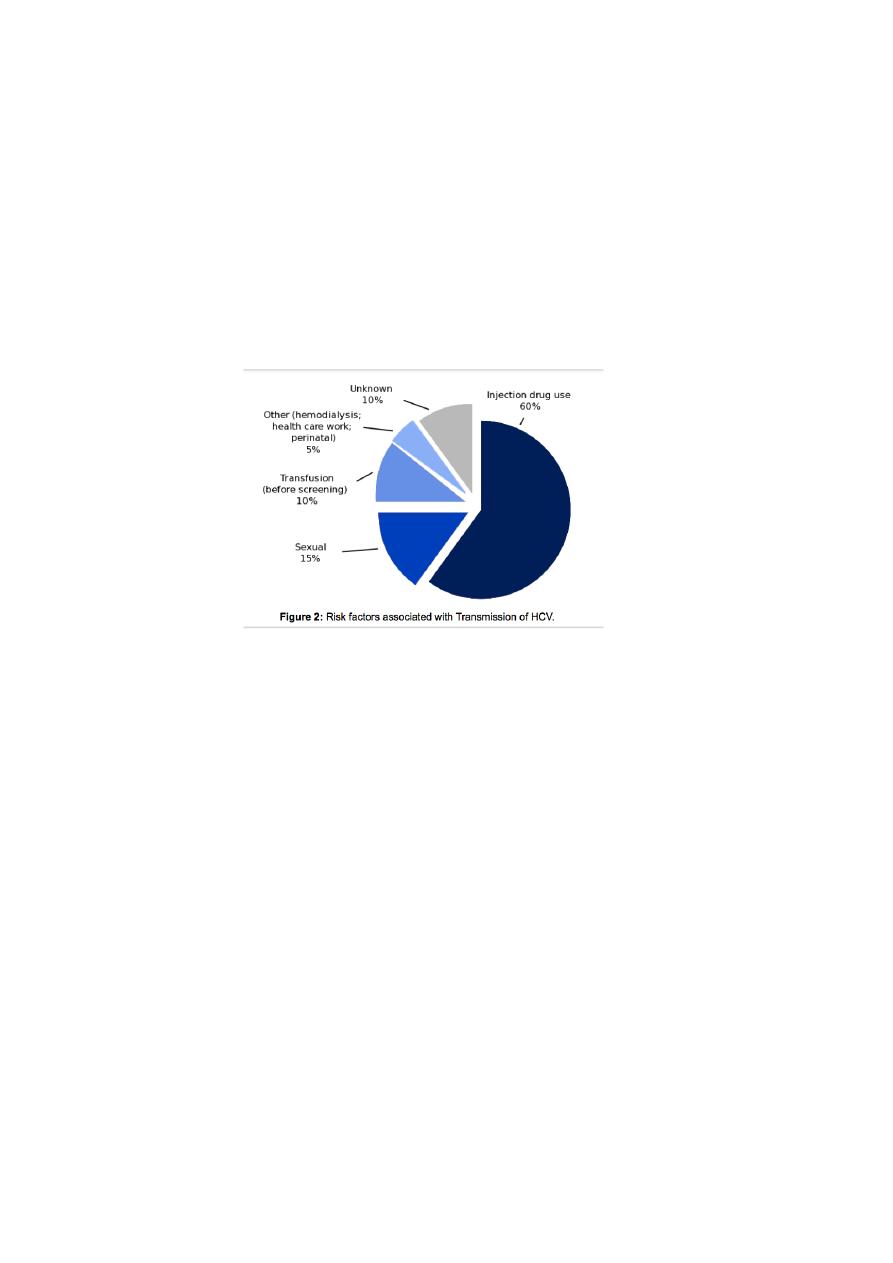
Transmission and prevention: Transmission is by:
•
Blood and blood products. High-risk persons include dialysis patients,
healthcare staff, and needle-sharing drug consumers. Perinatal
transmission is possible.
Treatment
A combination therapy of interferon and antiviral agent ribavirin is the current
option of treatment for patients with chronic HCV infections.
