1
Human Immunodeficiency Virus
(HIV)
/ اﻟﻤﺮﺣﻠﮫ اﻟﺜﺎﻟﺜﮫ
ﻓﺎﯾﺮوﺳﺎت
د. اﻧﺘﻈﺎر ﻋﻼوي ﺟﻌﻔﺮ / ﻓﺮع اﻻﺣﯿﺎء اﻟﻤﺠﮭﺮﯾﮫ / ﻛﻠﯿﮫ اﻟﻄﺐ / ﺟﺎﻣﻌﮫ ذي ﻗﺎر
PhD. M.Sc. Microbiology
Classification
Human immunodeficiency virus (HIV) is a a Lentivirus , a sub family of
Lentiviridae in the family Retrovirus that causes
Acquired immunodeficiency syndrome (AIDS).
HIV is this family includes the viruses known for: (i) Poor host immune
responses, (ii ) Latency. (iii ) Persistent viremia and (iv) Infection of the central
nervous system.
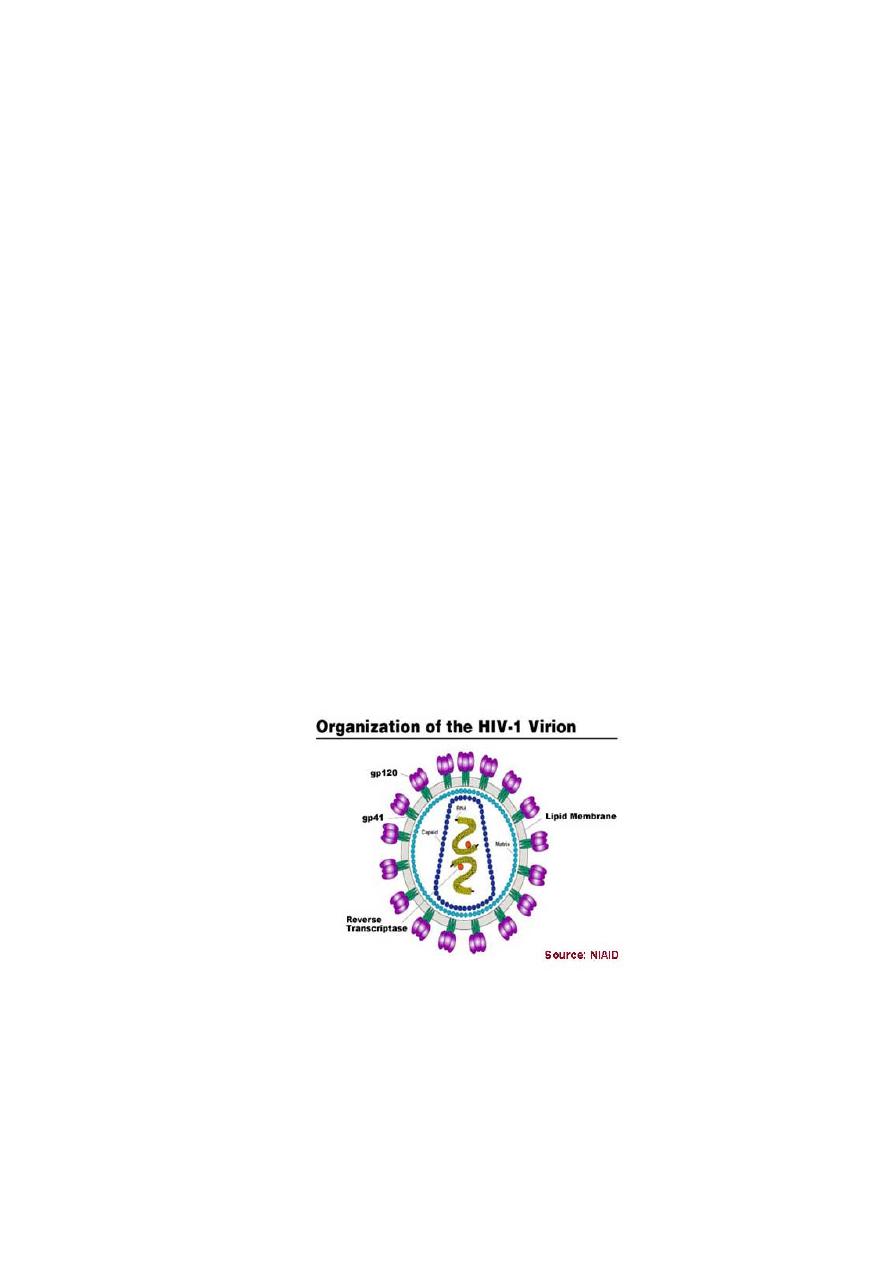
Morphology
HIV is a spherical, enveloped virus, which measures up to 120 nm in diameter
(See-Fig). HIV, is an enveloped RNA viruses, possessing an RNA-dependent DNA
polymerase called Reverse transcriptase. It has a unique three-layered
structure:
(i) The innermost genome layer, (ii) Middle cone shaped nucleocapsid
(iii) An outer membrane of glycoprotein surrounded by lipoprotein envelope.
Viral genome
HIV genome is most complex of human retroviruses. The genome consists of two
identical copies of single-stranded positive-sense RNA genome. The HIV contains
three major genes gag , pol , and env , characteristic of all retroviruses. All these
genes encode for the structural proteins.
2
The gag gene encodes for internal capsid and matrix “core” proteins (p15, p18,
and p24).
Of these three proteins, p24 is the major antigen, which is demonstrated in
serum of HIV patients during the early stage of infection and persists till the
appearance of serum antibodies. Detection of p24 antigen in serum, therefore, is
of diagnostic value.
The pol gene encodes for several proteins, including the enzymes reverse
transcriptase, integrase, and protease. The enzyme reverse transcriptase
synthesizes DNA by using the genome RNA as a template. The enzyme integrase
integrates the viral DNA into the cellular DNA, and the enzyme protease cleaves
various viral precursor proteins.
The env gene codes gp160, a precursor glycoprotein that is split to form two
envelope glycoproteins, gp120 and gp41, which form the surface spikes and
transmembrane tissue proteins, respectively.
HIV also consists of six other regulatory genes (tat , rev , nef , vif , and vpr).
These genes encode several proteins, which are essential for transcription and
invasion of virion into host cells.
tat gene is the most important one, which encodes a protein called Tat protein
that facilitates viral gene transcription. Tat protein along with other HIV-
encoded regulatory protein called Nef suppresses the synthesis of class I MHC
proteins thereby reducing the ability of cytotoxic T cells to kill the HIV-infected
cells.
Nucleocapsid: The viral genome is surrounded by a nucleocapsid consisting of
proteins. Three enzymes are located in the nucleocapsid:
(i) Reverse transcriptase, which transcribes the RNA genome into the proviral
genome. (ii) Integrase and (iii) Protease.
3
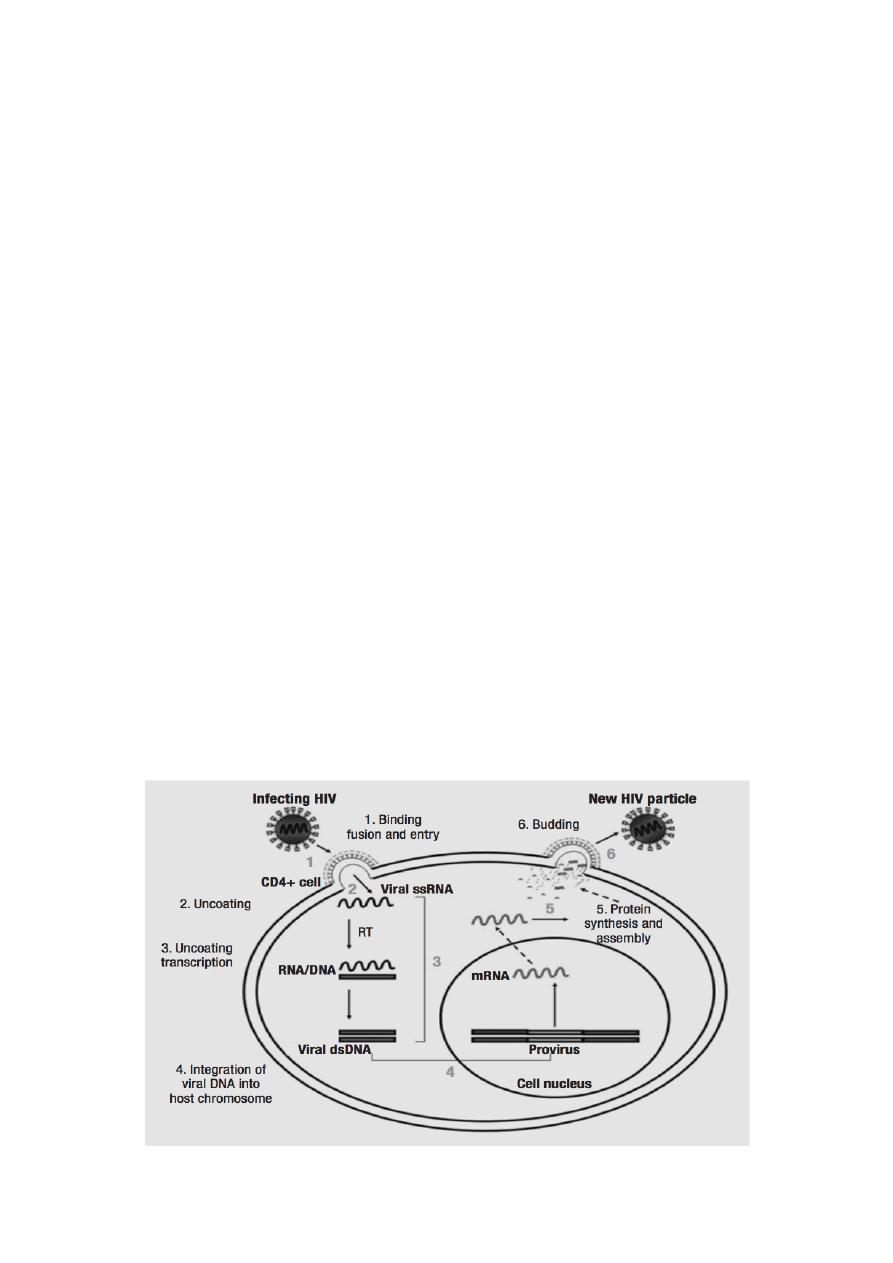
Viral replication
The virus binds to the CD4 proteins on the cell surface (T lymphocytes and
macrophages) with the help of its gp120 envelope protein (See-Fig). This
protein also interacts with chemokine receptors on the cell surface including the
CXCR4 and CCR5, which are essential for entry of HIV into CD4 cells.
Then gp41 of the virus mediates fusion of the viral envelope with the cell
membrane followed by entry of the virus into the cell.
Once inside the cell, after uncoating, the virion RNA-dependent DNA
polymerase transcribes the genome RNA into double-stranded DNA, which
subsequently integrates with the host cell DNA. Integration is mediated by the
viral enzyme integrase. The host cell RNA polymerase transcribes the viral
mRNA from the proviral DNA.
The viral mRNA encodes several proteins, protease to form the main core
protein (p24), the matrix protein (p17), and several smaller proteins. Such as
reverse transcriptase, integrase, and protease.
The immature virions containing the precursor polyproteins are assembled in
the cytoplasm, and cleavage by the viral protease occurs as the immature virion
buds from the cell membrane, resulting in the production of mature infectious
HIV.

4
Pathogenesis and Immunity
HIV is primarily a sexually transmitted pathogen transmitted by high-risk
behaviors, such as unprotected intercourse, male homosexual intercourse, and
also by intravenous (IV) drug abuse.
he tropism of the HIV for CD4-expressing T-cells and macrophages is the
principal determinant of the pathogenicity of HIV.
The CD4 antigens act as receptors for HIV. The virus infects helper T cells and
kills them, resulting in HIV-induced immunosuppression, leading to full-blown
AIDS—a key feature of the pathogenesis of HIV infection. This makes the patient
most susceptible to opportunistic infections and certain cancerous conditions,
such as Kaposi’s sarcoma and lymphoma. However, the virus does not directly
cause any tumor, because HIV genes are not found in these tumor cells.
The virus replicates continuously in the lymph nodes, thereby releasing the
virions and infected T cells into the blood.
During the course of infection, the virus causes a drastic reduction in the number
of CD4 T cells, which may occur due to direct HIV mediated cytopathic effect,
virus specific immune response, or apoptosis induced by viral proteins.
The deficiency or reduction of CD4 T cells leads to depression of cellular immune
response and impairment of humeral responses. The reduction of CD4 T cells is
responsible for producing delayed-type hypersensitivity reaction that leads to
opportunistic infections caused by many opportunistic pathogens.
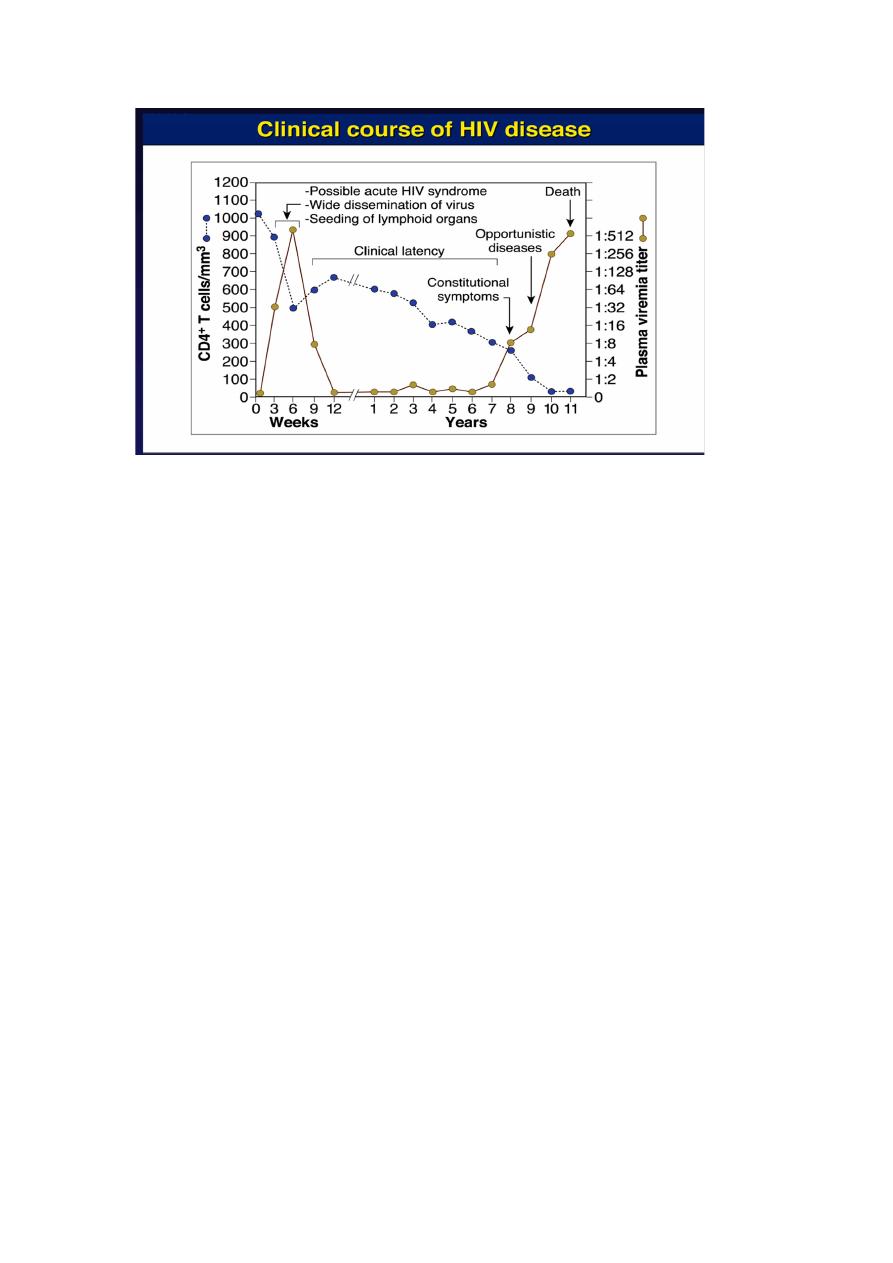
Clinical Syndromes
The course of untreated HIV infection is usually 10 ears or longer. The disease
progresses through the stages of
(a) Primary infection (flu like disease).
(b) Dissemination of virus to lymphoid organs.
(c) Clinical latency.
(d) A late stage of profound immunosuppression known as full-blown Acquired
Immune Deficiency Syndrome (AIDS).
Acute HIV infection
Is characterized by rapid rise in plasma viremia with a concomitant drop in CD4
count after an incubation period of 3–6 weeks. The symptoms of HIV are

5
nonspecific and include low-grade fever, fatigue, malaise, rash, headache, and
lymphadenopathy; spontaneous resolution may occur within weeks.
Asymptomatic HIV infection
This period is followed by an asymptomatic or clinically latent stage during
which the patient continues to remain asymptomatic for several months to years.
This stage is characterized by a low level of viral replication and a gradual fall in
CD4 count. The serum is positive for HIV antibodies in these patients. Another
characteristic of the stage of latency is persistent generalized lymphadenopathy,
which may last for several years or a period of asymptomatic infection. During
this stage, virus continues to replicate in the lymph node.
Acquired Immune Deficiency Syndrome (AIDS)
Is characterized by lymphadenopathy and fever. AIDS is the end-stage disease of
the HIV infection. It denotes the irreversible breakdown of immune system of the
host, making the infected host highly susceptible to a wide range of progressive
opportunistic infections such as tuberculosis, Pneumocystis carinii pneumonia,
toxoplasmosis, cryptococcal meningitis or unusual malignancies, such as
Kaposi’s sarcoma, non- Hodgkin’s lymphoma, Hodgkin’s lymphoma, cervical
cancer, and Burkitt’s lymphoma.
AIDS is characterized by deterioration of immune response as evidenced by CD4
T cell decrease response. The onset of clinical manifestations correlates with:
v
A reduction in number of CD4 T cells to less than 450/L.
v
Increased level of virus in the blood.
v
Presence of p24 antigen in the blood.
6
Transmission of infection
HIV is primarily a human infection. Humans infected with HIV and AIDS are the
reservoir of infection. The high titer of HIV is found in the body fluids including
blood, semen, and vaginal secretions of the infected people; hence these are
important sources of infection. HIV transmission occurs in following ways
Sexual transmission.
Transmission by blood transfusion.
Parenteral transmission occurs largely among IV drug users through the
use of contaminated needles.
Mother-to-child transmission: can occur by vertical transmission
through the placenta or through the amniotic membrane or by perinatal
transmission during delivery through infected birth canal.
Breast feeding
Laboratory Diagnosis
Specimens: these include serum and plasma for HIV serology and lymphocytes
for isolation of HIV.
• Serodiagnosis: Detection of specific antibodies to envelope glycoproteins
gp41, gp120, and gp160 and to viral core p24 antigens using ELISA
assay. The level of these antibodies is demonstrated in most individuals
within 6–12 weeks after infection and in all the individuals within 6
months of infection.

7
Molecular Diagnosis: The circulating virus count (viral load) is
determined by means of quantitative RT-PCR. It can also be used to
monitor the success of therapy with RT and protease inhibitors
Treatment
There is no cure for HIV infection. However, effective antiretroviral drugs (ARVs)
can control the virus and help prevent onward transmission to other people.
The anti-HIV drugs can be broadly classified as:
(a) Nucleoside analoge reverse transcriptase inhibitors (NRTIs) e.g Zidovudine,
Didanosine, Zalcitabine and Lamivudine.
(b) Nonnucleoside reverse transcriptase inhibitors (NNRTIs) e.g Nevirapine,
Delaviridine, Efavirenz.
(c) Protease inhibitors e.g Ritonavir and Indinavir.
Therapy with combination of Highly active antiretroviral therapy, referred to
as HAART, is effective in inhibition of HIV replication.
HAART has improved efficacy of the therapy, minimized toxicity following
therapy, and delayed emergence of drug resistance. It is usually recommended to
initiate double and triple drug therapy with two NRTIs Or two NRTIs an NNRTI
or a protease inhibitor.
