Talaro−Talaro: Foundations
in Microbiology, Fourth
Edition
17. Disorders in Immunity
Text
© The McGraw−Hill
Companies, 2002
497
umans possess a powerful and intricate system of defense,
which by its very nature also carries the potential to cause
injury and disease. In most instances, a defect in immune
function is expressed in commonplace, but miserable, symptoms such
as those of hay fever and dermatitis. But abnormal or undesirable
immune functions are also actively involved in debilitating or life-
threatening diseases such as asthma, anaphylaxis, rheumatoid arthri-
tis, graft rejection, and cancer.
Chapter Overview
• The immune system is subject to several types of dysfunctions termed
immunopathologies.
• Some dysfunctions are due to abnormally heightened responses to
antigens as manifested in allergies, hypersensitivities, and
autoimmunities.
• Some dysfunctions are due to the reduction or loss in protective immune
reactions due to genetic or environmental causes, as exemplified by
immunodeficiencies and cancer.
• Some immune damage is caused by normal actions that are directed at
foreign tissues placed in the body for therapy, such as transfusions and
transplants.
• Hypersensitivities are divided into immediate, antibody-mediated,
immune complex, and delayed allergies.
• Allergens are the foreign molecules from the environment, other
organisms, or even from the body that cause a hypersensitive or allergic
response.
• Most hypersensitivities require an initial sensitizing event, followed by a
later contact that causes symptoms.
• The immediate type of allergy is mediated by special types of B cells
that produce an antibody called IgE. IgE can cause mast cells to
release allergic chemicals such as histamine that stimulate symptoms.
• Examples of immediate allergies are atopy, asthma, food allergies, and
anaphylaxis.
• Another type of hypersensitivity arises from the action of other
antibodies (IgG and IgM) that can fix complement and lyse foreign
cells. An example is the reaction due to incompatible blood transfusions
or placental transfer.
• Immune complex reactions are caused by large amounts of circulating
antibodies against foreign molecules accumulating in tissues and
organs.
• Autoimmune diseases are due to the production of B and T cells that
are abnormally sensitized to react with the body’s natural molecules and
H
thus can damage cells and tissues. Some examples of these diseases
include rheumatoid arthritis, systemic lupus erythematosus, myasthenia
gravis, and multiple sclerosis.
• T cells are involved in delayed-type hypersensitivities wherein allergens
cause damage to cells and graft rejection.
• Immunodeficiencies are pathologies in which B and T cells and other
immune cells are missing or destroyed. They may be inborn and
genetic or acquired.
• The primary outcome of immunodeficiencies is manifest in recurrent
infections and lack of immune competence.
• Cancer is an abnormal overgrowth of cells due to a genetic defect and
the lack of effective immune surveillance.
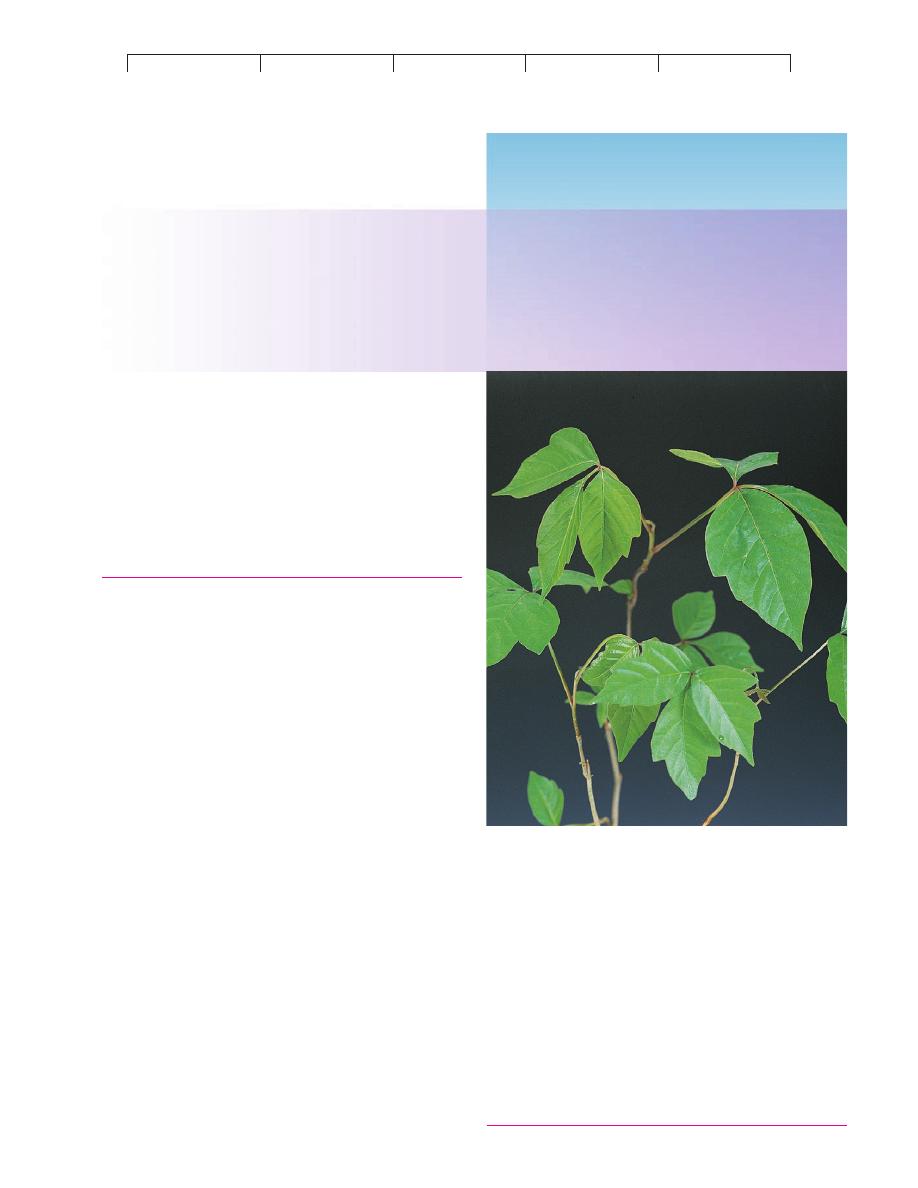
This delicate poison ivy plant, along with its close relatives poison oak and
sumac, is one of the most common causes of allergy in the United States.
Its leaves contain an oil that many people are sensitive to. The nature of its
effects are covered in this chapter.
CHAPTER
17
Disorders in Immunity
Talaro−Talaro: Foundations
in Microbiology, Fourth
Edition
17. Disorders in Immunity
Text
© The McGraw−Hill
Companies, 2002
498
CHAPTER 17 Disorders in Immunity
The Immune Response:
A Two-Sided Coin
With few exceptions, our previous discussions of the immune re-
sponse have centered around its numerous beneficial effects. The
precisely coordinated system that seeks out, recognizes, and de-
stroys an unending array of foreign materials is clearly protective,
but it also presents another side—a side that promotes rather than
prevents disease. In this chapter, we will survey
immunopathol-
ogy, the study of disease states associated with overreactivity or un-
derreactivity of the immune response (figure 17.1). In the cases of
allergies and autoimmunity, the tissues are innocent bystanders
attacked by excessive immunologic functions. In
grafts and trans-
fusions, a recipient reacts to the foreign tissues and cells of another
individual. In
immunodeficiency diseases, immune function is in-
completely developed, suppressed, or destroyed.
Cancer falls into
a special category, because it is both a cause and an effect of im-
mune dysfunction. As we shall see, one fascinating by-product of
studies of immune disorders has been our increased understanding
of the basic workings of the immune system.
Overreactions to Antigens:
Allergy/Hypersensitivity
The term
allergy* means a condition of altered reactivity or
exaggerated immune response that is manifested by inflammation.
Although it is sometimes used interchangeably with
hypersensitiv-
ity, some experts refer to immediate reactions such as hay fever as
allergies and to delayed reactions as hypersensitivities. Allergic
individuals are acutely sensitive to repeated contact with antigens,
called
allergens, that do not noticeably affect nonallergic individu-
als. Although the general effects of hyperactivity are detrimental,
we must be aware that it involves the very same types of immune
reactions as those at work in protective immunities. These include
humoral and cell-mediated actions, the inflammatory response,
phagocytosis, and complement. Such an association means that all
humans have the potential to develop hypersensitivity under
particular circumstances.
Immunodeficiency
T
B
U
n
de
rre
actio
n
Over
rea
ct
io
n
B
T
Cancer
A
n
tig
enic
Stimu
la
tio
n
L
o
ss
of
Im
m
unity
Hyper
sen
sit
iv
iti
es
Type I.
Immediate
(hay fever,
anaphylaxis)
Type II.
Antibody-mediated (blood type
incompatibilities)
Type III.
Immune complex
(rheumatoid arthritis, serum
sickness)
Type IV.
Cell-mediated, cytotoxic
(contact dermatitis, graft rejection)
*
allergy
(al
-er-jee) Gr. allos, other, and ergon, work.
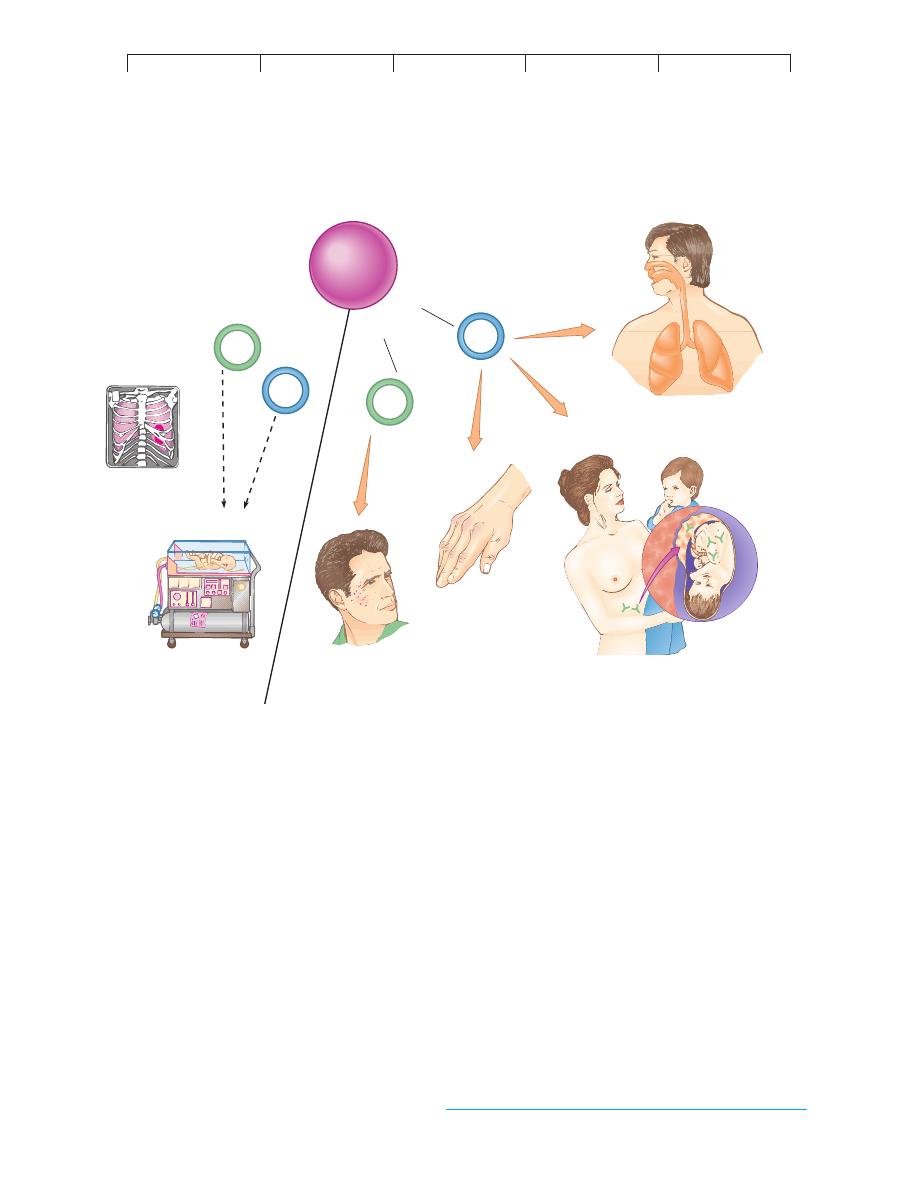
FIGURE 17.1
Overview of diseases of the immune system.
Just as the system of T cells and B cells provides necessary protection against infection and
disease, the same system can cause serious and debilitating conditions by overreacting or underreacting to immune stimuli.
Talaro−Talaro: Foundations
in Microbiology, Fourth
Edition
17. Disorders in Immunity
Text
© The McGraw−Hill
Companies, 2002
Type I Allergic Reactions: Atopy and Anaphylaxis
499
Originally, allergies were defined as either immediate or
delayed, depending upon the time lapse between contact with the
allergen and onset of symptoms. Subsequently, they were differ-
entiated as humoral versus cell-mediated. But as information on
the nature of the allergic immune response accumulated, it be-
came evident that, although useful, these schemes oversimplified
what is really a very complex spectrum of reactions. The most
widely accepted classification, first introduced by immunologists
P. Gell and R. Coombs, includes four major categories: type I
(atopy and anaphylaxis), type II (IgG- and IgM-mediated cell
damage), type III (immune complex), and type IV (delayed hyper-
sensitivity) (table 17.1). In general, types I, II, and III involve a
B-cell–immunoglobulin response, and type IV involves a T-cell re-
sponse (figure 17.1). The antigens that elicit these reactions can be
exogenous, originating from outside the body (microbes, pollen
grains, and foreign cells and proteins), or endogenous, arising from
self tissue (autoimmunities).
One of the reasons allergies are easily mistaken for infections
is that both involve damage to the tissues and thus trigger the
inflammatory response (see figure 14.18). Many symptoms and
signs of inflammation (redness, heat, skin eruptions, edema, and
granuloma) are prominent features of allergies.
Type I Allergic Reactions:
Atopy and Anaphylaxis
All type I allergies share a similar physiological mechanism, are
immediate in onset, and are associated with exposure to specific
antigens. However, it is convenient to recognize two subtypes:
Atopy* is any chronic local allergy such as hay fever or asthma;
anaphylaxis* is a systemic, often explosive reaction that involves
airway obstruction and circulatory collapse. In the following sec-
tions, we will consider the epidemiology of type I allergies, aller-
gens and routes of inoculation, mechanisms of disease, and specific
syndromes.
EPIDEMIOLOGY AND MODES OF
CONTACT WITH ALLERGENS
Allergies exert profound medical and economic impact. Allergists
(physicians who specialize in treating allergies) estimate that about
10% to 30% of the population is prone to atopic allergy. It is gener-
ally acknowledged that self-treatment with over-the-counter medi-
cines accounts for significant underreporting of cases. The 35 million
people afflicted by hay fever (15–20% of the population) spend
about half a billion dollars annually for medical treatment. The
monetary loss due to employee debilitation and absenteeism is im-
measurable. The majority of type I allergies are relatively mild, but
certain forms such as asthma and anaphylaxis may require hospi-
talization and cause death. About 2 million people in the United
States suffer from asthma.
The predisposition for type I allergies is inherited. Be aware
that what is hereditary is a generalized susceptibility, not the allergy
to a specific substance. For example, a parent who is allergic to rag-
weed pollen can have a child who is allergic to cat hair. The
prospect of a child’s developing atopic allergy is at least 25% if one
parent is atopic, increasing up to 50% if grandparents or siblings
are also afflicted. The actual basis for atopy appears to be a genetic
TABLE 17.1
Hypersensitivity States
Type
Systems and Mechanisms Involved
Examples
I.
Immediate hypersensitivity
IgE-mediated; involves mast cells,
Anaphylaxis, atopic allergies such as hay
basophils, and allergic mediators
fever, asthma
II.
Antibody-mediated
IgG, IgM antibodies act upon cells with
Blood group incompatibility, pernicious
complement and cause cell lysis; includes
anemia; myasthenia gravis
some autoimmune diseases
III.
Immune complex–mediated
Antibody-mediated inflammation; circulating
Systemic lupus erythematosus; rheumatoid
IgG complexes deposited in basement
arthritis; serum sickness; rheumatic fever
membranes of target organs; includes
some autoimmune diseases
IV.
T cell–mediated
Delayed hypersensitivity and cytotoxic
Infection reactions; contact dermatitis; graft
reactions in tissues
rejection; some types of autoimmunity
such as diabetes
Immunopathology is the study of diseases associated with excesses and
deficiencies of the immune response. Such diseases include allergies,
autoimmunity, grafts, transfusions, immunodeficiency disease, and
cancer.
An allergy or hypersensitivity is an exaggerated immune response that
injures or inflames tissues.
There are four categories of hypersensitivity reactions: type I (atopy and
anaphylaxis), type II (transfusion reactions), type III (immune complex
reactions), and type IV (delayed hypersensitivity reactions).
Antigens that trigger hypersensitivity reactions are allergens. They can be
either exogenous (originate outside the host) or endogenous (involve the
host’s own tissue).
CHAPTER CHECKPOINTS
*
atopy
(at
-oh-pee) Gr. atop, out of place.
*
anaphylaxis
(an
-uh-fih-lax-us) Gr. ana, excessive, and phylaxis, protection.
Talaro−Talaro: Foundations
in Microbiology, Fourth
Edition
17. Disorders in Immunity
Text
© The McGraw−Hill
Companies, 2002
500
CHAPTER 17 Disorders in Immunity
program that favors allergic antibody (IgE) production, increased
reactivity of mast cells, and increased susceptibility of target tissue
to allergic mediators. Allergic persons often exhibit a combination
of syndromes, such as hay fever, eczema, and asthma.
Other factors that affect the presence of allergy are age,
infection, and geographic locale. New allergies tend to crop up
throughout an allergic person’s life, especially as new exposures
occur after moving or changing life-style. In some persons, atopic
allergies last for a lifetime; others “outgrow” them, and still others
suddenly develop them later in life. Some features of allergy are not
yet completely explained.
THE NATURE OF ALLERGENS AND
THEIR PORTALS OF ENTRY
As with other antigens, allergens have certain immunogenic char-
acteristics. Not unexpectedly, proteins are more allergenic than
carbohydrates, fats, or nucleic acids. Some allergens are haptens,
non-proteinaceous substances with a molecular weight of less than
1,000 that can form complexes with carrier molecules in the body
(see figure 15.11). Organic and inorganic chemicals found in indus-
trial and household products, cosmetics, food, and drugs are com-
monly of this type. Table 17.2 lists a number of common allergenic
substances.
Allergens typically enter through epithelial portals in the res-
piratory tract, gastrointestinal tract, and skin. The mucosal surfaces
of the gut and respiratory system present a thin, moist surface that
is normally quite penetrable. The dry, tough keratin coating of skin
is less permeable, but access still occurs through tiny breaks,
glands, and hair follicles. It is worth noting that the organ of aller-
gic expression may or may not be the same as the portal of entry.
Airborne environmental allergens such as pollen, house dust,
dander (shed skin scales), or fungal spores are termed inhalants.
Each geographic region harbors a particular combination of air-
borne substances that varies with the season and humidity (figure
17.2a). Pollen, the most common offender, is given off seasonally
by the reproductive structures of pines and flowering plants (weeds,
trees, and grasses). Unlike pollen, mold spores are released
throughout the year and are especially profuse in moist areas of the
home and garden. Airborne animal hair and dander, feathers, and
the saliva of dogs and cats are common sources of allergens. The
component of house dust that appears to account for most dust al-
lergies is not soil or other debris, but the decomposed bodies of tiny
mites that commonly live in this dust (figure 17.2b). Some people
are allergic to their work, in the sense that they are exposed to al-
lergens on the job. Examples include florists, beauty operators,
woodworkers, farmers, drug processors, welders, and plastics man-
ufacturers whose work can aggravate inhalant allergies.
Allergens that enter by mouth, called ingestants, often cause
food allergies: Injectant allergies are an important adverse side
effect of drugs or other substances used in diagnosing, treating, or
preventing disease. A natural source of injectants is venom from
stings by hymenopterans, a family of insects that includes honey-
bees and wasps. Contactants are allergens that enter through the
skin. Many contact allergies are of the type IV, delayed variety
discussed later in this chapter.
MECHANISMS OF TYPE I ALLERGY:
SENSITIZATION AND PROVOCATION
What causes some people to sneeze and wheeze every time they
step out into the spring air, while others suffer no ill effects? In
order to answer this question, we must examine what occurs in the
tissues of the allergic individual that does not occur in the normal
person. In general, type I allergies develop in stages (figure 17.3).
The initial encounter with an allergen provides a
sensitizing dose
that primes the immune system for a subsequent encounter with
that allergen but generally elicits no signs or symptoms. The mem-
ory cells and immunoglobulin are then ready to react with a subse-
quent
provocative dose of the same allergen. It is this dose that
precipitates the signs and symptoms of allergy. Despite numerous
anecdotal reports of people showing an allergy upon first contact
with an allergen, it is generally believed that these individuals un-
knowingly had contact at some previous time. Fetal exposure to
allergens from the mother’s bloodstream is one possibility, and
foods can be a prime source of “hidden” allergens such as penicillin.
The Physiology of IgE-Mediated Allergies
During primary contact and sensitization, the allergen penetrates the
portal of entry (figure 17.3a). When large particles such as pollen
grains, hair, and spores encounter a moist membrane, they release
molecules of allergen that pass into the tissue fluids and lymphatics.
The lymphatics then carry the allergen to the lymph nodes, where
specific clones of B cells recognize it, are activated, and proliferate
into plasma cells. These plasma cells produce
immunoglobulin E
(IgE), the antibody of allergy. IgE is different from other im-
munoglobulins in having an Fc receptor region with great affinity
for mast cells and basophils. The binding of IgE to these cells in the
tissues sets the scene for the reactions that occur upon repeated ex-
posure to the same allergen (see figures 17.3b and 17.6).
The Role of Mast Cells and Basophils
The most important characteristics of mast cells and basophils
relating to their roles in allergy are:
1. Their ubiquitous location in tissues. Mast cells are
located in the connective tissue of virtually all organs, but
particularly high concentrations exist in the lungs, skin,
gastrointestinal tract, and genitourinary tract. Basophils
circulate in the blood but migrate readily into tissues.
TABLE 17.2
Common Allergens, Classified by Portal of Entry
Inhalants
Ingestants
Injectants
Contactants
Pollen
Food
Hymenopteran
Drugs
Dust
(chocolate,
venom (bee,
Cosmetics
Mold spores
wheat, eggs,
wasp)
Heavy metals
Dander
milk, nuts,
Drugs
Detergents
Animal hair
strawberries;
Vaccines
Formalin
Insect parts
fish)
Serum
Rubber
Formalin
Food additives
Enzymes
Glue
Drugs
Drugs (aspirin,
Hormones
Solvents
Enzymes
penicillin)
Dyes
Talaro−Talaro: Foundations
in Microbiology, Fourth
Edition
17. Disorders in Immunity
Text
© The McGraw−Hill
Companies, 2002
Type I Allergic Reactions: Atopy and Anaphylaxis
501
2. Their capacity to bind IgE during sensitization (figure
17.3). Each cell carries 30,000 to 100,000 cell receptors
that attract 10,000 to 40,000 IgE antibodies.
3. Their cytoplasmic granules (secretory vesicles), which
contain physiologically active cytokines (histamine,
serotonin—introduced in chapter 14).
4. Their tendency to degranulate (figures 17.3b and 17.4),
or release the contents of the granules into the tissues
when properly stimulated by allergen.
Let us now see what occurs when sensitized cells are challenged
with allergen a second time.
The Second Contact with Allergen
After sensitization, the IgE-primed mast cells can remain in the tis-
sues for years. Even after long periods without contact, a person
can retain the capacity to react immediately upon reexposure. The
next time allergen molecules contact these sensitized cells, they
bind across adjacent receptors and stimulate degranulation. As
chemical mediators are released, they diffuse into the tissues and
bloodstream. Cytokines give rise to numerous local and systemic
reactions, many of which appear quite rapidly (figure 17.3b). The
symptoms of allergy are not caused by the direct action of allergen
on tissues but by the physiological effects of mast cell mediators on
target organs.
Pollen in Los Angeles
Outlook for January
Trees
: Alder and walnut are blooming extremely early this year.
Black walnut is the worst allergy offender of the walnut family.
Weeds
: Weed season has finally ended.
Grasses
: Grasses will be mostly dormant until late February,
early March.
Molds
: Molds will continue to be sporadic and with major increases
following periods of precipitation.
Weekly Levels for December
Major
Moderate
Minor
Trees
Weeds
Grasses
Mold spores
Week 1
Week 2
Week 3
Week 4
(a)
(b)
(c)
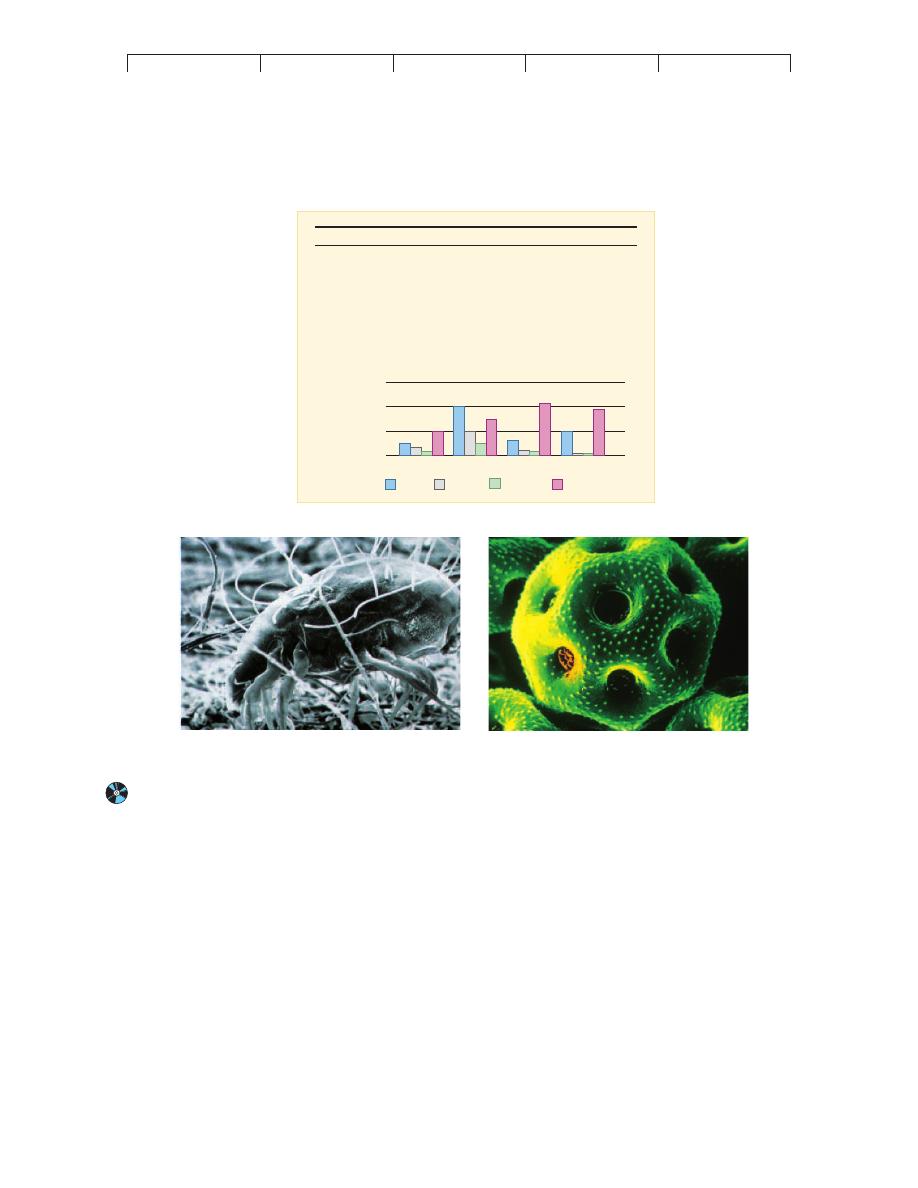
FIGURE 17.2
Monitoring airborne allergens.
(a) The air in heavily vegetated places with a mild climate is especially laden with allergens such as pollen and
mold spores. In just one month in southern California, weed pollen subsided to near zero and mold spore levels doubled. (b) Because the dust mite
Dermatophagoides feeds primarily on human skin cells in house dust, these mites are found in abundance in bedding and carpets. Airborne mite feces
and particles from their bodies are an important source of allergies. (c) Scanning electron micrograph of a single pollen grain from a rose (6,000!).
Millions of these are released from a single flower.
(a) Source: Data from the Asthma and Allergy Foundation of America, Los Angeles, CA.

Talaro−Talaro: Foundations
in Microbiology, Fourth
Edition
17. Disorders in Immunity
Text
© The McGraw−Hill
Companies, 2002
502
CHAPTER 17 Disorders in Immunity
CYTOKINES, TARGET ORGANS,
AND ALLERGIC SYMPTOMS
Numerous substances involved in mediating allergy (and inflam-
mation) have been identified. The principal chemical mediators
produced by mast cells and basophils are histamine, serotonin, leu-
kotriene, platelet-activating factor, prostaglandins, and bradykinin
(figure 17.4). These chemicals, acting alone or in combination, ac-
count for the tremendous scope of allergic symptoms. For some
theories pertaining to this function of the allergic response, see
Medical Microfile 17.1. Targets of these mediators include the skin,
upper respiratory tract, gastrointestinal tract, and conjunctiva. The
general responses of these organs include rashes, itching, redness,
rhinitis, sneezing, diarrhea, and shedding of tears. Systemic targets
include smooth muscle, mucous glands, and nervous tissue. Be-
cause smooth muscle is responsible for regulating the size of blood
vessels and respiratory passageways, changes in its activity can
profoundly alter blood flow, blood pressure, and respiration. Pain,
anxiety, agitation, and lethargy are also attributable to the effects of
mediators on the nervous system.
Histamine* is the most profuse and fastest-acting allergic
mediator. It is a potent stimulator of smooth muscle, glands, and
eosinophils. Histamine’s actions on smooth muscle vary with lo-
cation. It constricts the smooth muscle layers of the small bronchi
and intestine, thereby causing labored breathing and increased
Allergen particles enter
Lymphatic vessel
carries them to
Lymph node
B cell recognizes
allergen
Fc fragments
Mast cell in tissue
IgE binds to
mast cell surface
Granules
with
inflammatory
mediators
Time
Sensitization/IgE Production
Degranulation
st
im
ul
at
es
Mast cells
trigg
ers
Allergen particle is encountered again
End result: Symptoms in various organs
Red, itchy eyes
Hives
Runny
nose
Subsequent Exposure to Allergen
Systemic distribution of
mediators in bloodstream
proliferates
into
Plasma cells
Synthesize
IgE
B cell
(b)
(a)
FIGURE 17.3
A schematic view of cellular reactions during the type I allergic response.
(a) Sensitization (initial contact with sensitizing dose).
(b) Provocation (later contacts with provocative dose).
*
histamine
(his´-tah-meen) Gr. histio, tissue, and amine.
