
Talaro−Talaro: Foundations
in Microbiology, Fourth
Edition
17. Disorders in Immunity
Text
© The McGraw−Hill
Companies, 2002
502
CHAPTER 17 Disorders in Immunity
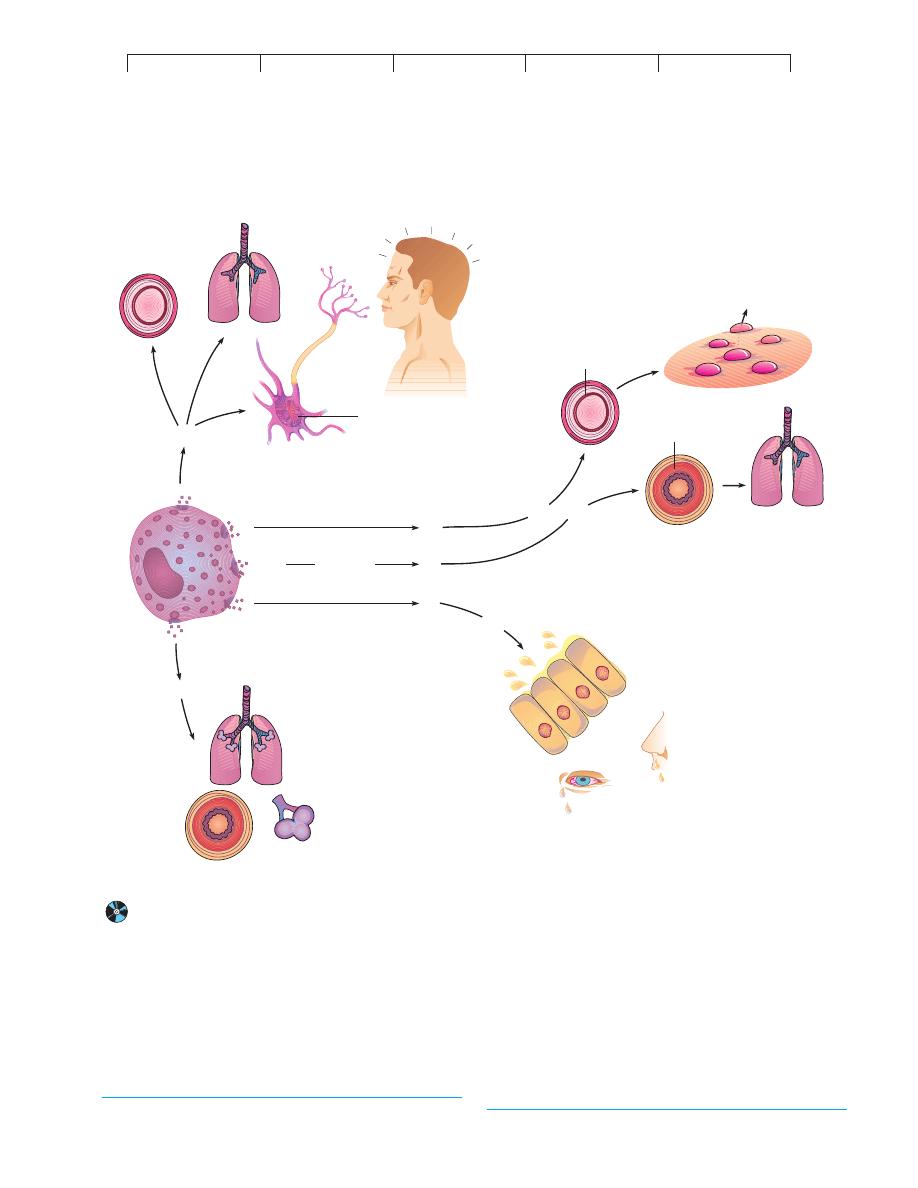
CYTOKINES, TARGET ORGANS,
AND ALLERGIC SYMPTOMS
Numerous substances involved in mediating allergy (and inflam-
mation) have been identified. The principal chemical mediators
produced by mast cells and basophils are histamine, serotonin, leu-
kotriene, platelet-activating factor, prostaglandins, and bradykinin
(figure 17.4). These chemicals, acting alone or in combination, ac-
count for the tremendous scope of allergic symptoms. For some
theories pertaining to this function of the allergic response, see
Medical Microfile 17.1. Targets of these mediators include the skin,
upper respiratory tract, gastrointestinal tract, and conjunctiva. The
general responses of these organs include rashes, itching, redness,
rhinitis, sneezing, diarrhea, and shedding of tears. Systemic targets
include smooth muscle, mucous glands, and nervous tissue. Be-
cause smooth muscle is responsible for regulating the size of blood
vessels and respiratory passageways, changes in its activity can
profoundly alter blood flow, blood pressure, and respiration. Pain,
anxiety, agitation, and lethargy are also attributable to the effects of
mediators on the nervous system.
Histamine* is the most profuse and fastest-acting allergic
mediator. It is a potent stimulator of smooth muscle, glands, and
eosinophils. Histamine’s actions on smooth muscle vary with lo-
cation. It
constricts the smooth muscle layers of the small bronchi
and intestine, thereby causing labored breathing and increased
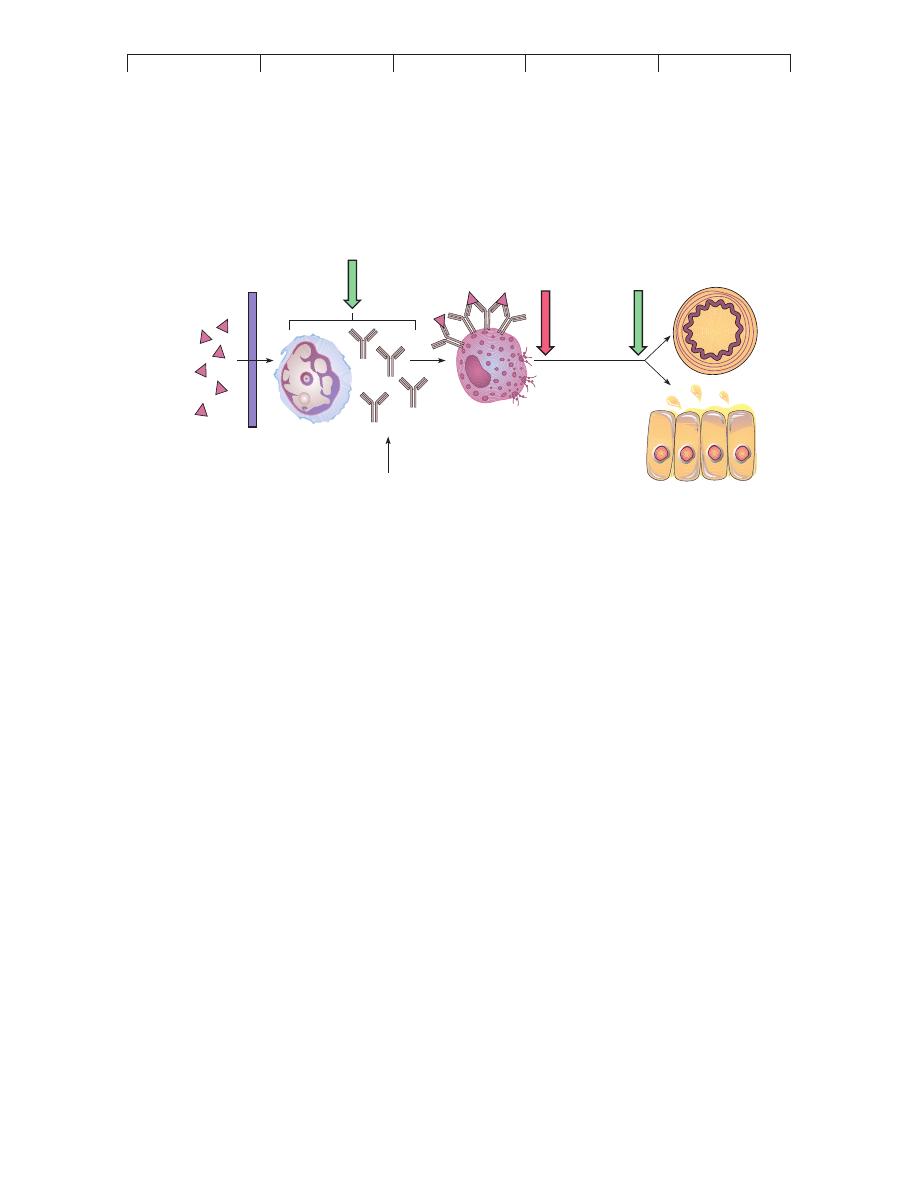
Allergen particles enter
Lymphatic vessel
carries them to
Lymph node
B cell recognizes
allergen
Fc fragments
Mast cell in tissue
IgE binds to
mast cell surface
Granules
with
inflammatory
mediators
Time
Sensitization/IgE Production
Degranulation
st
im
ul
at
es
Mast cells
trigg
ers
Allergen particle is encountered again
End result: Symptoms in various organs
Red, itchy eyes
Hives
Runny
nose
Subsequent Exposure to Allergen
Systemic distribution of
mediators in bloodstream
proliferates
into
Plasma cells
Synthesize
IgE
B cell
(b)
(a)
FIGURE 17.3
A schematic view of cellular reactions during the type I allergic response.
(a) Sensitization (initial contact with sensitizing dose).
(b) Provocation (later contacts with provocative dose).
*
histamine
(his´-tah-meen) Gr.
histio, tissue, and amine.
Talaro−Talaro: Foundations
in Microbiology, Fourth
Edition
17. Disorders in Immunity
Text
© The McGraw−Hill
Companies, 2002
Type I Allergic Reactions: Atopy and Anaphylaxis
503
intestinal motility. In contrast, histamine
relaxes vascular smooth
muscle and dilates arterioles and venules. It is responsible for the
wheal* and flare reaction in the skin (see figure 17.6a), pruritis
(itching), and headache. More severe reactions (such as anaphy-
laxis) can be accompanied by edema and vascular dilation, which
lead to hypotension, tachycardia, circulatory failure, and, fre-
quently, shock. Salivary, lacrimal, mucous, and gastric glands are
also histamine targets.
Although the role of
serotonin* in human allergy is uncer-
tain, its effects appear to complement those of histamine. In exper-
imental animals, serotonin increases vascular permeability, capil-
lary dilation, smooth muscle contraction, intestinal peristalsis, and
respiratory rate, but it diminishes central nervous system activity.
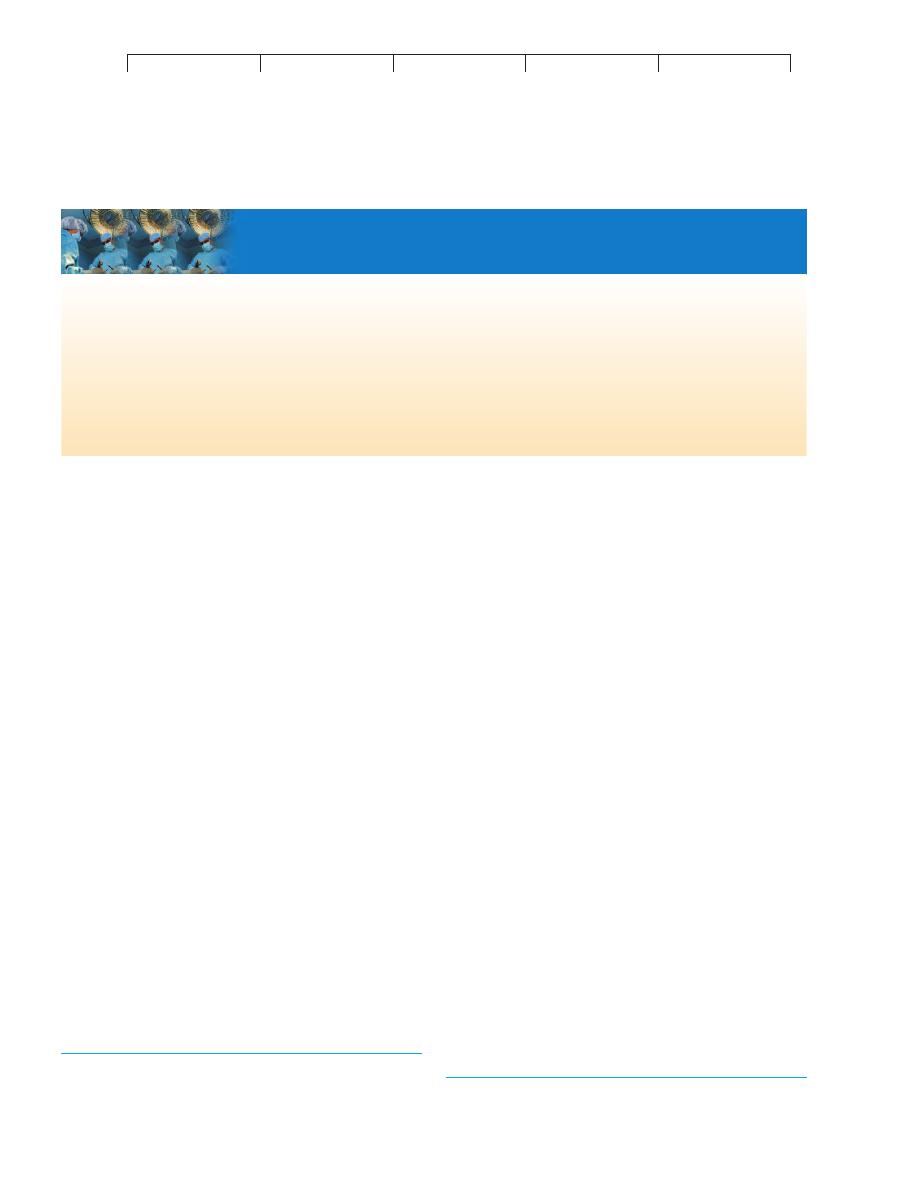
Dilated blood vessel
Constricted
bronchiole
Smooth muscle
Leukotriene
Glands
Prostaglandin
Typical
response
in asthma
Nerve cell
Dilated
blood vessel
Constricted bronchioles
Headache
Wheal and flare
reaction, itching
Wheezing,
difficult breathing
Excessive mucus and
glandular secretions
Constriction
of bronchioles
Plugged
alveoli
D
e
g
ra
n
u
la
ti
o
n
Histamine
Serotonin
Bradykinin
FIGURE 17.4
The spectrum of reactions to inflammatory cytokines and the common symptoms they elicit in target tissues and organs.
Note the
extensive overlapping effects.
*
serotonin
(ser
-oh-toh-nin) L. serum, whey, and tonin, tone.
*
wheal
(weel) A smooth, slightly elevated, temporary welt that is surrounded by a
flushed patch of skin (flare).
Talaro−Talaro: Foundations
in Microbiology, Fourth
Edition
17. Disorders in Immunity
Text
© The McGraw−Hill
Companies, 2002
504
CHAPTER 17 Disorders in Immunity
Before the specific types were identified,
leukotriene* was
known as the “slow-reacting substance of anaphylaxis” for its
property of inducing gradual contraction of smooth muscle. This
type of leukotriene is responsible for the prolonged bronchospasm,
vascular permeability, and mucous secretion of the asthmatic indi-
vidual. Other leukotrienes stimulate the activities of polymor-
phonuclear leukocytes.
Platelet-activating factor is a lipid released by basophils,
neutrophils, monocytes, and macrophages that causes platelet
aggregation and lysis. The physiological response to stimulation by
this factor is similar to that of histamine, including increased
vascular permeability, pulmonary smooth muscle contraction,
pulmonary edema, hypotension, and a wheal and flare response in
the skin.
Prostaglandins* are a group of powerful inflammatory
agents. Normally, these substances regulate smooth muscle con-
traction (for example, they stimulate uterine contractions during
delivery). In allergic reactions, they are responsible for vasodila-
tion, increased vascular permeability, increased sensitivity to pain,
and bronchoconstriction. Certain anti-inflammatory drugs work by
preventing the actions of prostaglandins.
Bradykinin* is related to a group of plasma and tissue
peptides known as kinins that participate in blood clotting and
chemotaxis. In allergy, it causes prolonged smooth muscle contrac-
tion of the bronchioles, dilatation of peripheral arterioles, increased
capillary permeability, and increased mucous secretion.
SPECIFIC DISEASES ASSOCIATED WITH IgE-
AND MAST CELL-MEDIATED ALLERGY
The mechanisms just described are basic to hay fever, allergic
asthma, food allergy, drug allergy, eczema, and anaphylaxis. In this
section, we cover the main characteristics of these conditions, fol-
lowed by methods of detection and treatment.
Atopic Diseases
Hay fever is a generic term for allergic rhinitis,* a seasonal reac-
tion to inhaled plant pollen or molds, or a chronic, year-round
reaction to a wide spectrum of airborne allergens or inhalants (see
table 17.2). The targets are typically respiratory membranes, and
the symptoms include nasal congestion; sneezing; coughing; pro-
fuse mucous secretion; itchy, red, and teary eyes; and mild bron-
choconstriction.
Asthma* is a respiratory disease characterized by episodes
of impaired breathing due to severe bronchoconstriction. The air-
ways of asthmatic people are exquisitely responsive to minute
amounts of inhalant allergens, food, or other stimuli, such as in-
fectious agents. The symptoms of asthma range from occasional,
annoying bouts of difficult breathing to fatal suffocation. Labored
breathing, shortness of breath, wheezing, cough, and ventilatory
rales* are present to one degree or another. The respiratory tract
of an asthmatic person is chronically inflamed and severely over-
reactive to allergy chemicals, especially leukotrienes and sero-
tonin from pulmonary mast cells. Other pathologic components
are thick mucous plugs in the air sacs and lung damage that can
result in long-term respiratory compromise. An imbalance in the
nervous control of the respiratory smooth muscles is apparently
involved in asthma, and the episodes are influenced by the psy-
chological state of the person, which strongly supports a neuro-
logical connection.
The number of asthma sufferers in the United States is esti-
mated at 10 million, with nearly one-third of them children. For
reasons that are not completely understood, asthma is on the in-
crease, and deaths from it have doubled since 1982, even though
effective agents to control it are more available now than they
have ever been before. A recent study of inner-city children has
correlated high levels of asthma to contact with cockroach anti-
gens in their living quarters. Nearly 40% of children age 10 or
younger showed extreme sensitivity to the droppings and remains
of these insects.
MEDICAL MICROFILE
17.1
Of What Value Is Allergy?
this system is to defend against helminth worms that are ubiquitous
human parasites. In chapter 14, we learned that inflammatory mediators
serve valuable functions, such as increasing blood flow and vascular
permeability to summon essential immune components to an injured site.
They are also responsible for increased mucous secretion, gastric motil-
ity, sneezing, and coughing, which help expel noxious agents. The
difference is that, in allergic persons, the quantity and quality of these
reactions are excessive and uncontrolled.
Why would humans and other mammals evolve an allergic response that
is capable of doing so much harm and even causing death? It is unlikely
that this limb of immunity exists merely to make people miserable; it
must have a role in protection and survival. What are the underlying bio-
logical functions of IgE, mast cells, and the array of potent cytokines?
Analysis has revealed that, although allergic persons have high levels of
IgE, trace quantities are present even in the sera of nonallergic individu-
als, just as mast cells and inflammatory chemicals are also part of normal
human physiology. It is generally believed that one important function of
*
leukotriene
(loo
-koh-try-een) Gr. leukos, white blood cell, and triene, a chemical
suffix.
*
prostaglandin
(pross
-tah-glan-din) From prostate gland. The substance was
originally isolated from semen.
*
bradykinin
(brad
-ee-kye-nin) Gr. bradys, slow, and kinein, to move.
*
rhinitis
(rye-nye
-tis) Gr. rhis, nose, and itis, inflammation.
*
asthma
(az
-muh) The Greek word for gasping.
*
rales
(rails) Abnormal breathing sounds.
Talaro−Talaro: Foundations
in Microbiology, Fourth
Edition
17. Disorders in Immunity
Text
© The McGraw−Hill
Companies, 2002
Type I Allergic Reactions: Atopy and Anaphylaxis
505
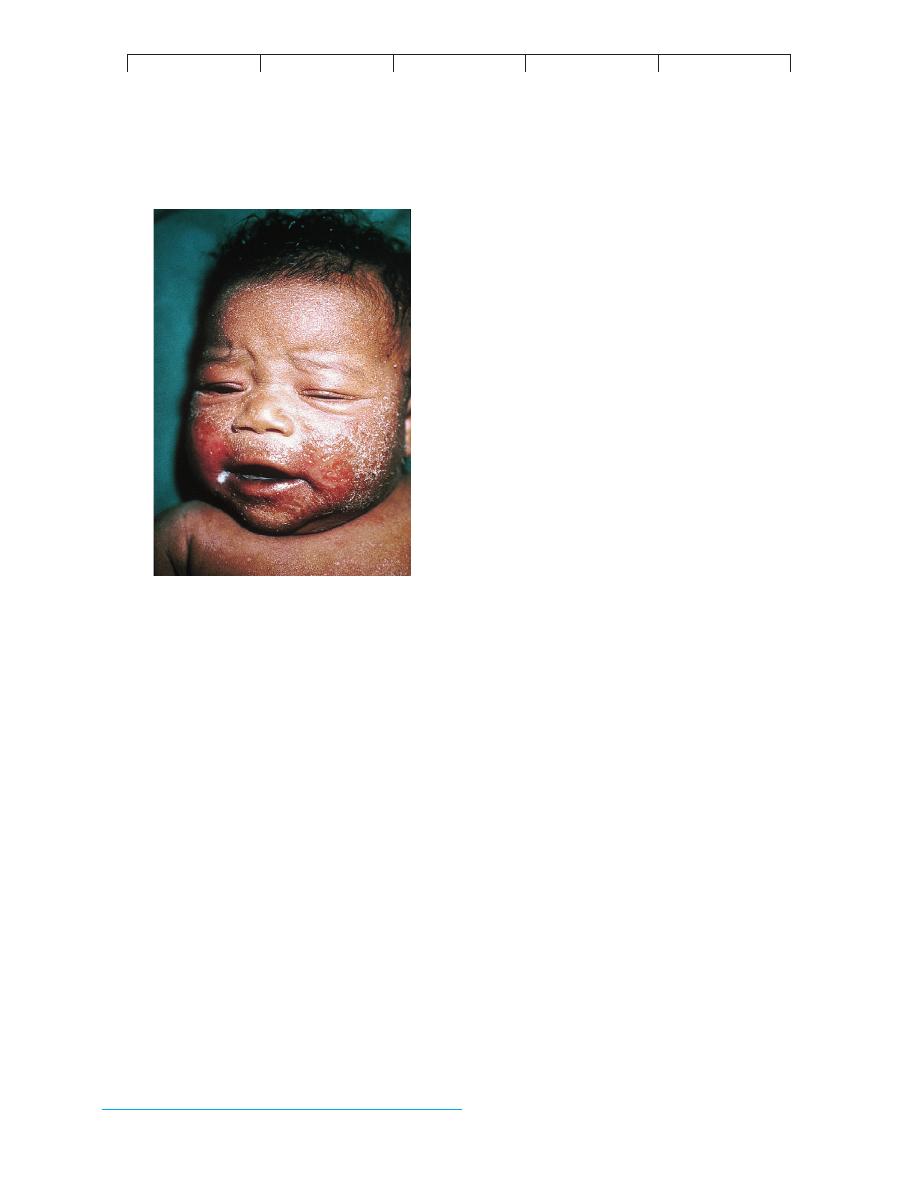
Atopic dermatitis is an intensely itchy inflammatory condi-
tion of the skin, sometimes also called
eczema.* Sensitization
occurs through ingestion, inhalation, and, occasionally, skin con-
tact with allergens. It usually begins in infancy with reddened,
vesicular, weeping, encrusted skin lesions. It then progresses in
childhood and adulthood to a dry, scaly, thickened skin condition
(figure 17.5). Lesions can occur on the face, scalp, neck, and inner
surfaces of the limbs and trunk. The itchy, painful lesions cause
considerable discomfort, and they are often predisposed to second-
ary bacterial infections. An anonymous writer once aptly described
eczema as “the itch that rashes’’ or “one scratch is too many but one
thousand is not enough.’’
Food Allergy
The ordinary diet contains a vast variety of compounds that are po-
tentially allergenic. It is generally believed that food allergies are
due to a digestive product of the food or to an additive (preservative
or flavoring). Although the mode of entry is intestinal, food aller-
gies can also affect the skin and respiratory tract. Gastrointestinal
symptoms include vomiting, diarrhea, and abdominal pain. In se-
vere cases, nutrients are poorly absorbed, leading to growth retar-
dation and failure to thrive in young children. Other manifestations
of food allergies include eczema, hives, rhinitis, asthma, and occa-
sionally, anaphylaxis. Classic food hypersensitivity involves IgE
and degranulation of mast cells, but not all reactions involve this
FIGURE 17.5
Atopic dermatitis, or eczema.
Vesicular, encrusted lesions are typical
in afflicted infants. This condition is prevalent enough to account for 1%
of pediatric care.
*
eczema
(eks
-uh-mah; also ek-zeem-uh) Gr. ekzeo, to boil over.
mechanism. The most common food allergens come from peanuts,
fish, cow’s milk, eggs, shellfish, and soybeans.
Drug Allergy
Modern chemotherapy has been responsible for many medical ad-
vances. Unfortunately, it has also been hampered by the fact that
drugs are foreign compounds capable of stimulating allergic
reactions. In fact, allergy to drugs is one of the most common side
effects of treatment (present in 5–10% of hospitalized patients).
Depending upon the allergen, route of entry, and individual sensi-
tivities, virtually any tissue of the body can be affected, and reac-
tions range from mild atopy to fatal anaphylaxis. Compounds im-
plicated most often are antibiotics (penicillin is number one in
prevalence), synthetic antimicrobics (sulfa drugs), aspirin, opiates,
and anaesthetics. The actual allergen is not the intact drug itself but
a hapten given off when the liver processes the drug. Some forms
of penicillin sensitivity are due to the presence of small amounts of
the drug in meat, milk, and other foods and to exposure to
Penicil-
lium mold in the environment.
ANAPHYLAXIS: AN OVERPOWERING
SYSTEMIC REACTION
The term
anaphylaxis, or anaphylactic shock, was first used to
denote a reaction of animals injected with a foreign protein. Al-
though the animals showed no response during the first contact,
upon reinoculation with the same protein at a later time, they ex-
hibited acute symptoms—itching, sneezing, difficult breathing,
prostration, and convulsions—and many died in a few minutes.
Two clinical types of anaphylaxis are distinguished in humans.
Cu-
taneous anaphylaxis is the wheal and flare inflammatory reaction to
the local injection of allergen.
Systemic anaphylaxis, on the other
hand, is characterized by sudden respiratory and circulatory disrup-
tion that can be fatal in a few minutes. In humans, the allergen and
route of entry are variable, though bee stings and injections of an-
tibiotics or serum are implicated most often. Bee venom is a com-
plex material containing several allergens and enzymes that can
create a sensitivity that can last for decades after exposure.
The underlying physiological events in systemic anaphylaxis
parallel those of atopy, but the concentration of chemical mediators
and the strength of the response are greatly amplified. The immune
system of a sensitized person exposed to a provocative dose of al-
lergen responds with a sudden, massive release of chemicals into
the tissues and blood, which act rapidly on the target organs. Ana-
phylactic persons have been known to die in 15 minutes from com-
plete airway blockage.
DIAGNOSIS OF ALLERGY
Because allergy mimics infection and other conditions, it is impor-
tant to determine if a person is actually allergic. If possible or nec-
essary, it is also helpful to identify the specific allergen or allergens.
Allergy diagnosis involves several levels of tests, including non-
specific, specific,
in vitro, and in vivo methods.
A new test that can distinguish whether a patient has experi-
enced an allergic attack measures elevated blood levels of tryptase,
an enzyme released by mast cells that increases during an allergic
response. Several types of specific
in vitro tests can determine
Talaro−Talaro: Foundations
in Microbiology, Fourth
Edition
17. Disorders in Immunity
Text
© The McGraw−Hill
Companies, 2002
506
CHAPTER 17 Disorders in Immunity
the allergic potential of a patient’s blood sample. The leukocyte
histamine-release test measures the amount of histamine released
from the patient’s basophils when exposed to a specific allergen.
Serological tests that use radioimmune assays (see chapter 16) to
reveal the quantity and quality of IgE are also clinically helpful.
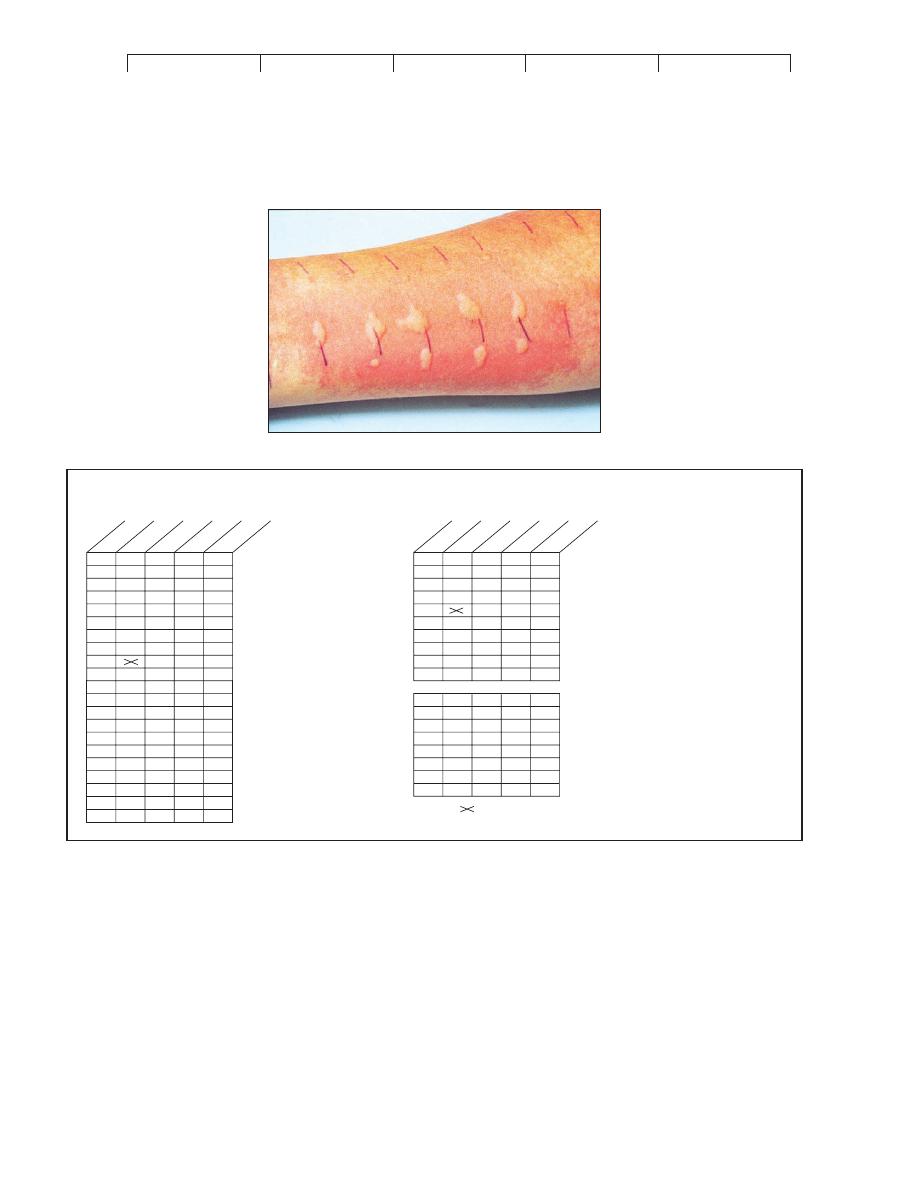
Skin Testing
A useful
in vivo method to detect precise atopic or anaphylactic
sensitivities is skin testing. With this technique, a patient’s skin is
injected, scratched, or pricked with a small amount of a pure al-
lergen extract. Hundreds of these allergen extracts contain com-
mon airborne allergens (plant and mold pollen) and more unusual
allergens (mule dander, theater dust, bird feathers). Unfortu-
nately, skin tests for food allergies using food extracts are unreli-
able in most cases. In patients with numerous allergies, the aller-
gist maps the skin on the inner aspect of the forearms or back and
injects the allergens intradermally according to this predeter-
mined pattern (figure 17.6
a). Approximately 20 minutes after
antigenic challenge, each site is appraised for a wheal response
indicative of histamine release. The diameter of the wheal is
(a)
Environmental Allergens
1. Acacia gum
2. Cat dander
3. Chicken feathers
4. Cotton lint
5. Dog dander
6. Duck feathers
7. Glue, animal
8. Horse dander
9. Horse serum
10. House dust #1
11. Kapok
12. Mohair (goat)
13. Paper
14. Pyrethrum
15. Rug pad, ozite
16. Silk dust
17. Tobacco dust
18. Tragacanth gum
19. Upholstery dust
20. Wool
No. 1 Standard Series
1. Ant
2. Aphis
3. Bee
4. Housefly
5. House mite
6. Mosquito
7. Moth
8. Roach
9. Wasp
10. Yellow jacket
Airborne mold spores
11.
Alternaria
12.
Aspergillus
13.
Cladosporium
14.
Hormodendrum
15.
Penicillium
16.
Phoma
17.
Rhizopus
18. .........................
No. 2 Airborne Particles
+++
+++
++++
++++
++
+
+
++
+++
+
+
+
++++
+++
+
+
+
+++++
+++
ID 8/85
+++
+++++
++++
++++
+++
++++
+++
++
0
ID 8/85
++
+++
++
+++
0
+
+++
0
+
++
+++
++++
- not done
- no reaction
- slight reaction
- mild reaction
- moderate reaction
- severe reaction
FIGURE 17.6
A method for conducting an allergy skin test.
The forearm (or back) is mapped and then injected with a selection of allergen extracts.
The allergist must be very aware of potential anaphylaxis attacks triggered by these injections. (a) Close-up of skin wheals showing a number of
positive reactions (dark lines are measurer’s marks). (b) An actual skin test record for some common environmental allergens with a legend for
assessing them.
(b)
Talaro−Talaro: Foundations
in Microbiology, Fourth
Edition
17. Disorders in Immunity
Text
© The McGraw−Hill
Companies, 2002
Type I Allergic Reactions: Atopy and Anaphylaxis
507
measured and rated on a scale of 0 (no reaction) to 4
" (greater
than 15 mm). Figure 17.6
b shows skin test results for a person
with extreme inhalant allergies.
TREATMENT AND PREVENTION OF ALLERGY
In general, the methods of treating and preventing type I allergy in-
volve (1) avoiding the allergen, though this may be very difficult in
many instances; (2) taking drugs that block the action of lympho-
cytes, mast cells, or chemical mediators; and (3) undergoing desen-
sitization therapy.
It is not possible to completely prevent initial sensitization,
since there is no way to tell in advance if a person will develop an
allergy to a particular substance. The practice of delaying the intro-
duction of solid foods apparently has some merit in preventing food
allergies in children, though even breast milk can contain allergens
ingested by the mother. Although rigorous cleaning and air condi-
tioning can reduce contact with airborne allergens, it is not feasible
to isolate a person from all allergens, which is the reason drugs are
so important in control.
Therapy to Counteract Allergies
The aim of antiallergy medication is to block the progress of the
allergic response somewhere along the route between IgE produc-
tion and the appearance of symptoms (figure 17.7). Oral anti-
inflammatory drugs such as corticosteroids inhibit the activity of
lymphocytes and thereby reduce the production of IgE, but they also
have dangerous side effects and should not be taken for prolonged
periods. Some drugs block the degranulation of mast cells and
reduce the levels of inflammatory cytokines. The most effective of
these are diethylcarbamazine and cromolyn. Asthma and rhinitis
sufferers can find relief with a new drug that blocks synthesis of
leukotriene and a monoclonal antibody that inactivates IgE (Xolair).
Widely used medications for preventing symptoms of
atopic allergy are
antihistamines, the active ingredients in most
over-the-counter allergy-control drugs. Antihistamines interfere
with histamine activity by binding to histamine receptors on tar-
get organs. Most of them have major side effects, however, such
as drowsiness. Newer antihistamines lack this side effect because
they do not cross the blood-brain barrier. Other drugs that relieve
inflammatory symptoms are aspirin and acetaminophen, which
reduce pain by interfering with prostaglandin, and theophylline, a
bronchodilator that reverses spasms in the respiratory smooth
muscles. Persons who suffer from anaphylactic attacks are urged
to carry at all times injectable epinephrine (adrenaline) and an
identification tag indicating their sensitivity. An aerosol inhaler
containing epinephrine can also provide rapid relief. Epinephrine
reverses constriction of the airways and slows the release of aller-
gic mediators.
Approximately 70% of allergic patients benefit from con-
trolled injections of specific allergens as determined by skin tests.
This technique, called
desensitization or hyposensitization, is a
therapeutic way to prevent reactions between allergen, IgE, and
mast cells. The allergen preparations contain pure, preserved sus-
pensions of plant antigens, venoms, dust mites, dander, and molds
(but so far, hyposensitization for foods has not proved very effec-
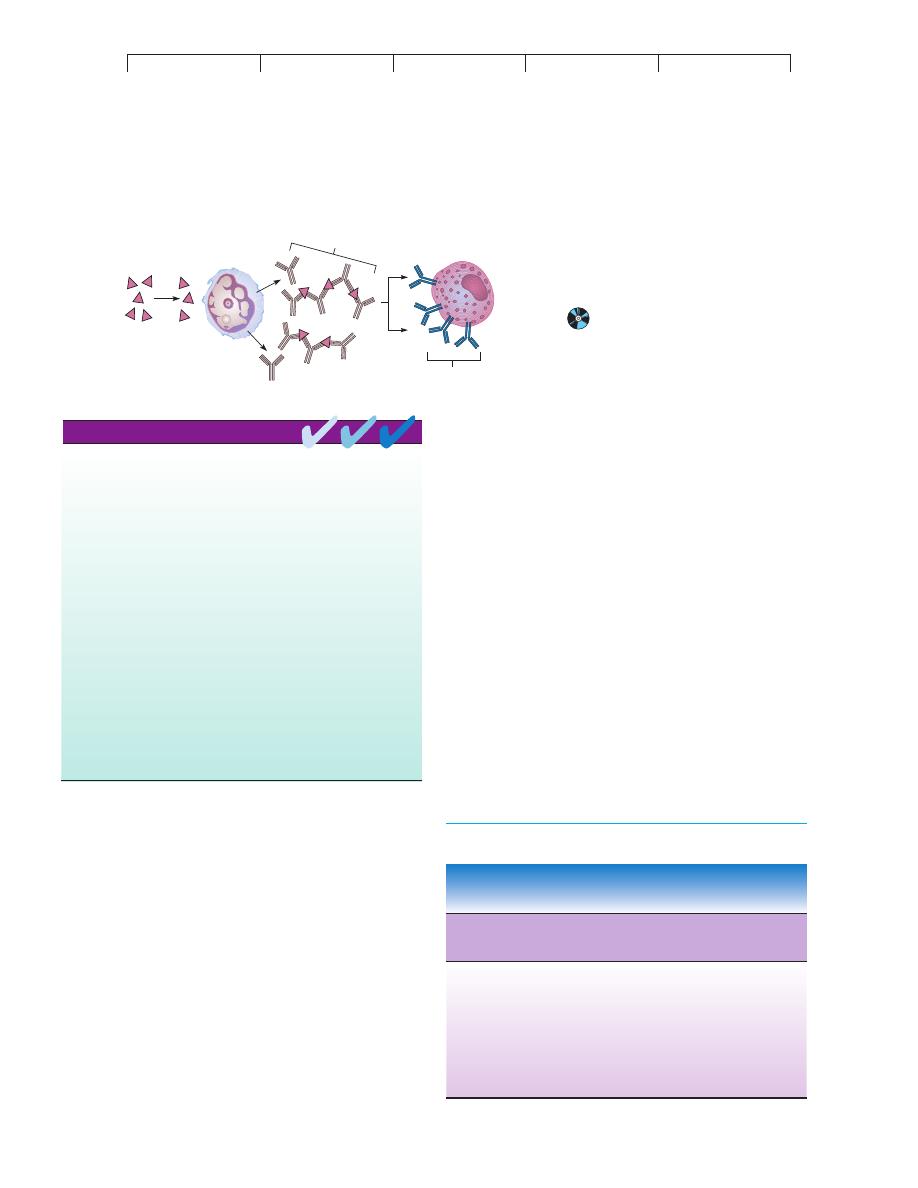
tive). The immunologic basis of this treatment is open to differ-
ences in interpretation. One theory suggests that injected aller-
gens stimulate the formation of high levels of allergen-specific
IgG (figure 17.8). It has been proposed that these IgG
blocking
antibodies remove allergen from the system before it can bind to
IgE, thus preventing the degranulation of mast cells. It is also pos-
sible that allergen delivered in this fashion combines with the IgE
itself and prevents it from reacting with the mast cells. Some ex-
perts suggest that the therapy induces specific clones of suppres-
sor T cells to block the production of IgE by B cells.
Avoidance
of allergen
Corticosteroids
keep the plasma cell
from synthesizing IgE
and inhibit T cells.
Allergen
Cromolyn acts
on the surface
of mast cell;
no degranulation
IgE
Antihistamines, aspirin,
epinephrine, theophylline
counteract the effects
of cytokines on targets.
Monoclonal drugs
that inactivate IgE
FIGURE 17.7
Strategies for circumventing allergic attacks.
Talaro−Talaro: Foundations
in Microbiology, Fourth
Edition
17. Disorders in Immunity
Text
© The McGraw−Hill
Companies, 2002
508
CHAPTER 17 Disorders in Immunity
Type II Hypersensitivities: Reactions
That Lyse Foreign Cells
The diseases termed type II hypersensitivities are a complex group
of syndromes that involve complement-assisted destruction (lysis)
of cells by antibodies (IgG and IgM) directed against those cells’
surface antigens. This category includes transfusion reactions and
some types of autoimmunities (discussed in a later section). The
cells targeted for destruction are often red blood cells, but other
cells can be involved.
HUMAN BLOOD TYPES
Chapters 14 and 15 described the functions of unique surface re-
ceptors or markers on cell membranes. Ordinarily, these receptors
play essential roles in transport, recognition, and development, but
they become medically important when the tissues of one person
are placed into the body of another person. Blood transfusions and
organ donations introduce alloantigens (molecules that differ in the
same species) on donor cells that are recognized by the lympho-
cytes of the recipient. These reactions are not really immune dys-
functions as allergy and autoimmunity are. The immune system is
in fact working normally, but it is not equipped to distinguish
between the desirable foreign cells of a transplanted tissue and the
undesirable ones of a microbe.
THE BASIS OF HUMAN ABO
ANTIGENS AND BLOOD TYPES
The existence of human blood types was first demonstrated by an
Austrian pathologist, Karl Landsteiner, in 1904. While studying in-
compatibilities in blood transfusions, he found that the serum of one
person could clump the red blood cells of another. Landsteiner iden-
tified four distinct types, subsequently called the ABO blood groups.
Like the MHC antigens on white blood cells, the ABO anti-
gen markers on red blood cells are genetically determined and com-
posed of glycoproteins. These ABO antigens are inherited as two
(one from each parent) of three alternative
alleles:* A, B, or O. A
and B alleles are dominant over O and codominant with one an-
other. As table 17.3 indicates, this mode of inheritance gives rise to
four blood types (phenotypes), depending on the particular combi-
nation of genes. Thus, a person with an
AA or AO genotype has
type A blood; genotype BB or BO gives type B; genotype AB
Type I hypersensitivity reactions result from excessive IgE production in
response to an exogenous antigen.
The two kinds of type I hypersensitivities are atopy, a chronic, local
allergy, and anaphylaxis, a systemic, potentially fatal allergic response.
The predisposition to type I hypersensitivities is inherited, but age,
geographic locale, and infection also influence allergic response.
Type I allergens include inhalants, ingestants, injectants, and contactants.
The portals of entry for type I antigens are the skin, respiratory tract,
gastrointestinal tract, and genitourinary tract.
Type I hypersensitivities are set up by a sensitizing dose of allergen and
expressed when a second provocative dose triggers the allergic
response. The time interval between the two can be many years.
The primary participants in type I hypersensitivities are IgE, basophils,
mast cells, and agents of the inflammatory response.
Allergies are diagnosed by a variety of in vitro and in vivo tests that
assay specific cells, IgE, and local reactions.
Allergies are treated by medications that interrupt the allergic response at
certain points. Allergic reactions can often be prevented by
desensitization therapy.
CHAPTER CHECKPOINTS
Allergen
IgG
"blocking
antibodies"
B Cell / Plasma Cell
Mast Cell
IgE
No IgE
FIGURE 17.8
The blocking antibody theory for allergic
desensitization.
An injection of allergen
causes IgG antibodies to be formed instead of
IgE; these blocking antibodies cross-link and
effectively remove the allergen before it can react
with the IgE in the mast cell.
TABLE 17.3
Characteristics of ABO Blood Groups
Phenotype A
or B* RBC
Prevalence in
Serum Content
Genotype
Antigen
Population**
of Antibodies
OO
Neither
Most common
Both anti-a
and anti-b
AA, AO
A
Second most
Anti-b
common
BB, BO
B
Third most
Anti-a
common
AB
AB
Least common
Neither
antibody
*Capital letters generally denote antigen; lowercase denotes antibody.
**True of most large populations of mixed racial and ethnic groups.
*
allele
(ah-leel
) Gr. allelon, of one another. An alternate form of a gene for a given trait.
