GASTROINTESTINAL TRACT PATHOLOGY
Prof. Dr. Maha Shakir HasanSTOMACH
stomach
Gastric disorders give rise to symptoms similar to esophageal disorders, but color of hematemesis is brown.??Congenital disorders:
PYLORIC STENOSISCongenital hypertrophic pyloric stenosis generally presents in the second or third week of life as new-onset regurgitation and persistent, projectile vomiting.
Physical examination reveals hyperperistalsis and a firm, ovoid abdominal mass.
Diaphragmatic hernia
incomplete formation of the diaphragm allows the abdominal viscera to herniate into the thoracic cavity.When severe, pulmonary hypoplasia that is incompatible with life after birth. GASTRITIS
• Inflammation is simply defined as inflammation of gastric mucosa, either acute or chronic.
•
Acute Gastritis
It is an acute mucosal inflammatory process, usually of a transient nature.The inflammation may be accompanied by
hemorrhage
erosion
ETIOLOGY
Heavy use of nonsteroidal anti-inflammatory drugs (NSAIDs), particularly aspirin.Excessive alcohol consumption
Heavy smoking
Treatment with cancer chemotherapeutic drugs
Uremia
Severe stress (e.g., trauma, burns, surgery)
ACUTE GASTRIC ULCERATION
Focal, acutely developing gastric mucosal defects are a well-known complication of therapy with NSAIDs. They may also appear after severe physiologic stress. Some of these are given specific names, based on location and clinical associations. For example:Stress ulcers are most common in individuals with shock, sepsis, or severe trauma.
Ulcers occurring in the proximal duodenum and associated with severe burns or trauma are called Curling ulcers.Gastric, duodenal, and esophageal ulcers arising in persons with intracranial disease are termed Cushing ulcers and carry a high incidence of perforation
Chronic Gastritis
The most common cause of chronic gastritis is infection with the bacillus Helicobacter pylori.Autoimmune gastritis, the most common cause of atrophic gastritis, represents less than 10% of cases of chronic gastritis and is the most common form of chronic gastritis in patients without H. pylori infection.
Less common etiologies include radiation injury, chronic bile reflux.
H. pylori Gastritis.
in most patients, gastritis is limited to the antrum with occasional involvement of the cardia.
In a subset of patients the gastritis progresses to involve the gastric body and fundus.
This pangastritis is associated with multifocal mucosal atrophy, reduced acid secretion, intestinal metaplasia, and increased risk of gastric adenocarcinoma.
Four features are linked to H. pylori virulence:
Flagella, which allow the bacteria to be motile in viscous mucusUrease, which generates ammonia from endogenous urea and thereby elevates local gastric pH
Adhesins that enhance bacterial adherence to surface foveolar cells
Toxins, that may be involved in ulcer or cancer development by poorly defined mechanisms.
Morphology.
The organisms are concentrated within the superficial mucus overlying epithelial cells.
The inflammatory infiltrate includes:
•variable numbers of neutrophil within the: lamina propria.
intraepithelial location
accumulate in the lumen of gastric pits to create pit abscesses.
•the superficial lamina propria includes large numbers of plasma cells, and increased numbers of lymphocytes and macrophages.
Lymphoid aggregates, some with germinal centers, risk of lymphoma.
Clinical Features.
Diagnosishistologic identification of the organism.
Serologic test for antibodies to H. pylori.
fecal bacterial detection
treatments
combinations of antibiotics
Individuals with H. pylori gastritis usually improve after treatment, although relapses can occur after incomplete eradication or re-infection.
AUTOIMMUNE GASTRITIS
accounts for less than 10% of cases of chronic gastritis.typically spares the antrum
and includes hypergastrinemia .
Autoimmune gastritis is characterized by:
Antibodies to parietal cells that can be detected in serum and gastric secretionsReduced serum pepsinogen I concentration
Antral endocrine cell hyperplasia
Vitamin B12 deficiency
Defective gastric acid secretion (achlorhydria)
Pathogenesis.
loss of parietal cells, which are responsible for secretion of gastric acid and intrinsic factor.
The absence of acid production stimulates gastrin release, resulting in hypergastrinemia and hyperplasia of antral gastrin-producing G cells.
Lack of intrinsic factor disables ileal vitamin B12 absorption, leading to B12 deficiency and a slow-onset megaloblastic anemia (pernicious anemia).
The reduced serum pepsinogen I concentration results from chief cell destruction.
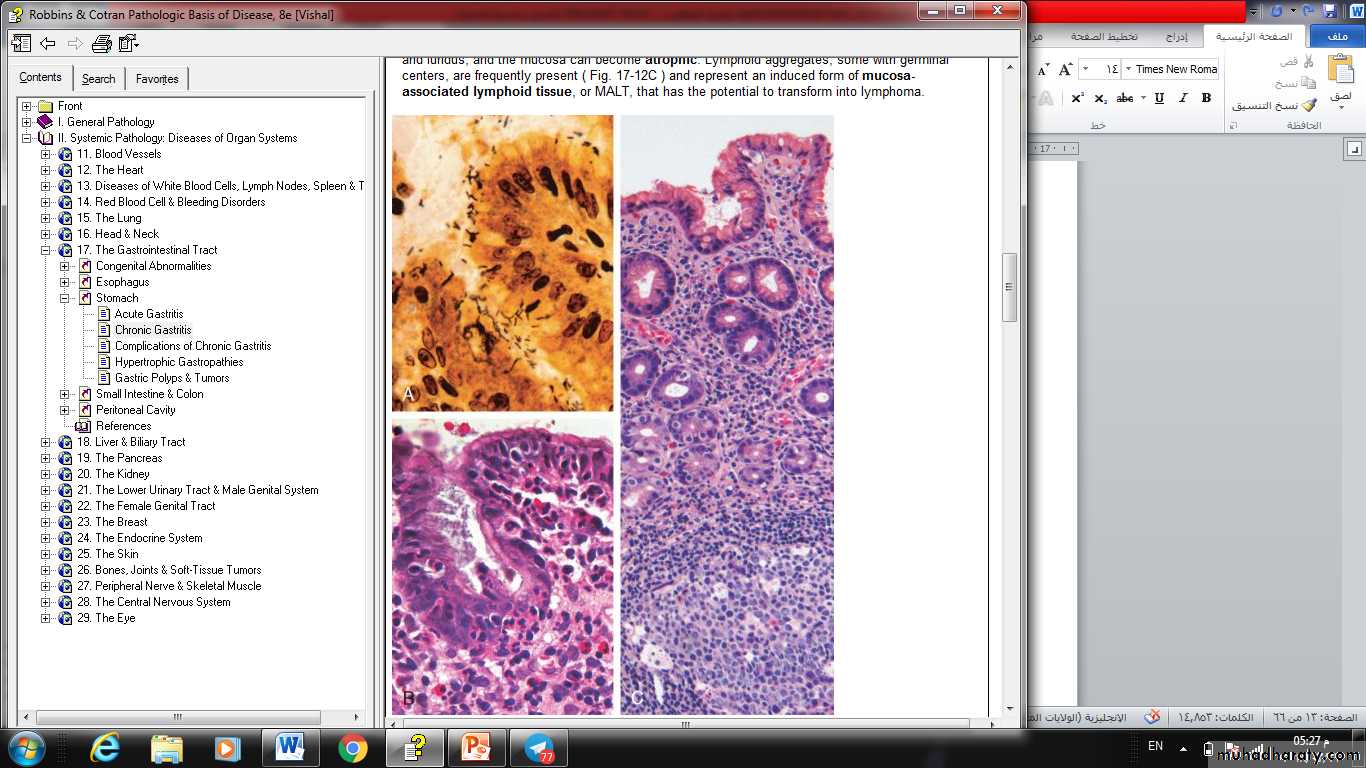
Helicobacter pylori gastritis. A, Spiral-shaped H. pylori are highlighted in this Warthin-Starry silver stain. Organisms are abundant within surface mucus. B, Intraepithelial and lamina propria neutrophils are prominent. C, Lymphoid aggregates with germinal centers and abundant subepithelial plasma cells within the superficial lamina propria are characteristic of H. pylori gastritis.
peptic ulcer disease
Ulcers are defined as a breach in the mucosa of the alimentary tract that extends through the muscularis mucosae into the submucosa or deeper.
Peptic ulcer disease (PUD) is most often associated with H. pylori–induced hyperchlorhydric chronic gastritis
Peptic ulcer
PUD may occur in any portion of the GI tract exposed to acidic gastric juices, but is most common in the gastric antrum and first portion of the duodenum.PUD may also occur in the esophagus as a result of GERD or acid secretion by ectopic gastric mucosa.
Gastric mucosa within a Meckel diverticulum can result in peptic ulceration of adjacent mucosa.
Pathogenesis:
2 key factors:1- mucosal exposure to gastric acid and pepsin.
2- Aggressive forces like H- pylori.
Ulcer are developed by an imbalance between the gastro duodenal mucosal defenses and the countervailing aggressive forces that overcome such defenses.
Defense mechanisms:
◘ secretion of mucous by surface epithelial cells.◘ secretion of bicarbonate into the surface mucus.
◘ sec. of acid and pepsin as a jet with mucus material.
◘ rapid epith cell regeneration.
etiology
H. pylori infectionNSAID use
MORPHOLOGY
Peptic ulcers are four times more common in the proximal duodenum than in the stomach.Duodenal ulcers usually occur within a few centimeters of the pyloric valve and involve the anterior duodenal wall.
Gastric peptic ulcers are predominantly located along the lesser curvature near the interface of the body and antrum.
morphology
Peptic ulcers are solitary in more than 80% of patients.Lesions less than 0.3 cm in diameter tend to be shallow while those over 0.6 cm are likely to be deeper ulcers.
The classic peptic ulcer is a round to oval, sharply punched-out defect.
The mucosal margin is usually level with the surrounding mucosa. In contrast, heaped-up margins are more characteristic of cancers.
The depth of ulcers may be limited by the thick gastric muscularis propria or by adherent pancreas, omental fat, or the liver.
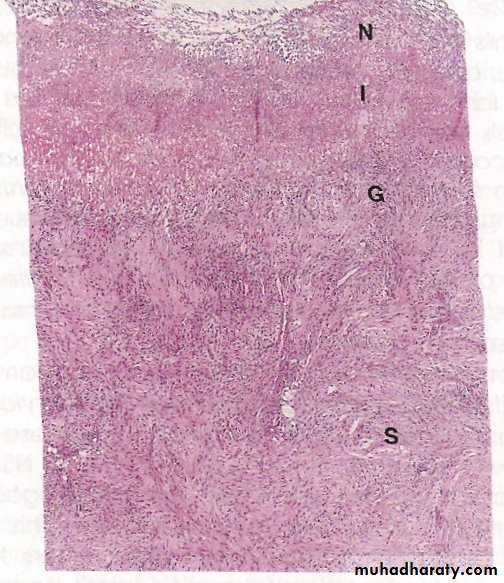
microscopically
• 4 zones distinguished:• The base and margins have a thin layer of necrotic fibrinoid debris.
• Underlain by zone of active nonspecific infl infiltrate, with neutrophils predominate.
• Underlain by granulation tissue.
• Fibrous collagenous scar that fans out widely from the margin of the ulcer.
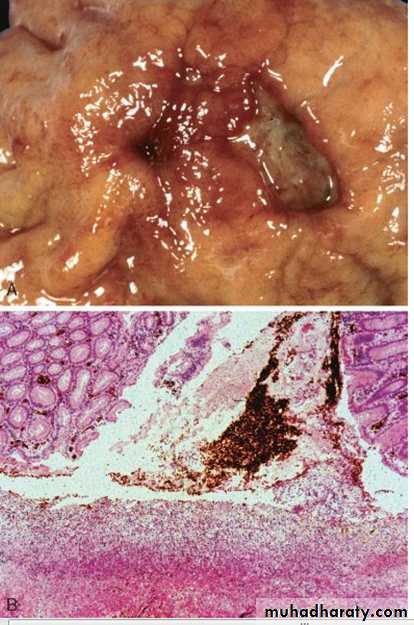
FIGURE Acute gastric perforation in a patient presenting with free air under the diaphragm. A, Mucosal defect with clean edges. B, The necrotic ulcer base is composed of granulation tissue.