Small and large intestine
Developmental anomaliesAtresia and stenosis:
A: atresia is complete failure of development of the intestinal lumen
B-Stenosis:only narrowing.
Duplication: well developed saccular to
tubular cystic structures, which may not communicate with the lumen of the small intestine.Meckel diverticulum
Failure of involution of the omphalomesentric duct.Persistent of blind ended tubular protrusion up to 5-6 cm long.
Usually in the ileum within about 2 feets of the cecum.
Composed of all layers of the normal small intestine.
Usually asymptomatic.
Hirchsprung disease
Distention of the colon to greater than 6-7 cm in diameter. Congenital or acquired.There is aganglionic segment lack both Meissner submucosal and Auerbach myenteric plexus.
Functional obstruction and progressive distention of the colon proximal to the affected segment.
50% mutation in RET gene.
Male:female 4:1.In most instances only the rectum and the sigmoid colon are aganglionic.
20% of cases a longer segment or entire colon involved.
C/P: Delay in the passage of the meconium followed by vomiting.
Life threatening disease. death caused by enterocolitis, or fluid and electrolytes disturbances.
Rarely death due to colonic perforation.
Acquired megacolon
• Chagas disease.• Organic obstruction.
• toxic megacolon.(due to UC).
• Functional.
•
angiodysplasia
Tortuous dilatation of submucosal and mucosal blood vessels, most often in the cecum or right colon.Usually only after the 6th decade.
hemorrhoids
It is variceal dilitation of the anal and perianal submucosal venous plexus.Pathogenesis:
Persistently elevated venous pressure within hemorrhoidal plexus.
Predisposing conditions
• Chronic constipation.• Pregnancy.
• Rarely portal hypertention.
malabsorption syndromes
Is characterized by suboptimal absorption of fat, fat soluble and other vit, proteins, carbohydrates, electrolytes and minerals, and water.
Chronic malabsorption can be accompanied by weight loss, anorexia, abdominal distention. A hallmark of malabsorption is steatorrhea, characterized by excessive fecal fat and bulky, frothy, greasy, yellow or clay-colored stools.
Celiac disease
Sensitivity to gluten, the component of wheat and related grain(oat, barley, and rye) , that contain the water insoluble protein gliadin.There is strong genetic susceptibility.
Immune response to gluten.
SI mucosa when exposed to gluten, accumulate large no of plasma cell and sensitize B cell, damage to epithelial cells, flattening of villi.
Affecting proximal small intestine.
Clinical presentation
• The age of presentation with symptomatic diarrhea and malnutrition varies from infancy to midadulthood.• Treatment: removal of gluten from diet.
• Compx:
• Intestinal lymphoma, and other GIT malignancies.
• Malignancies outside the GIT, e.g. breast
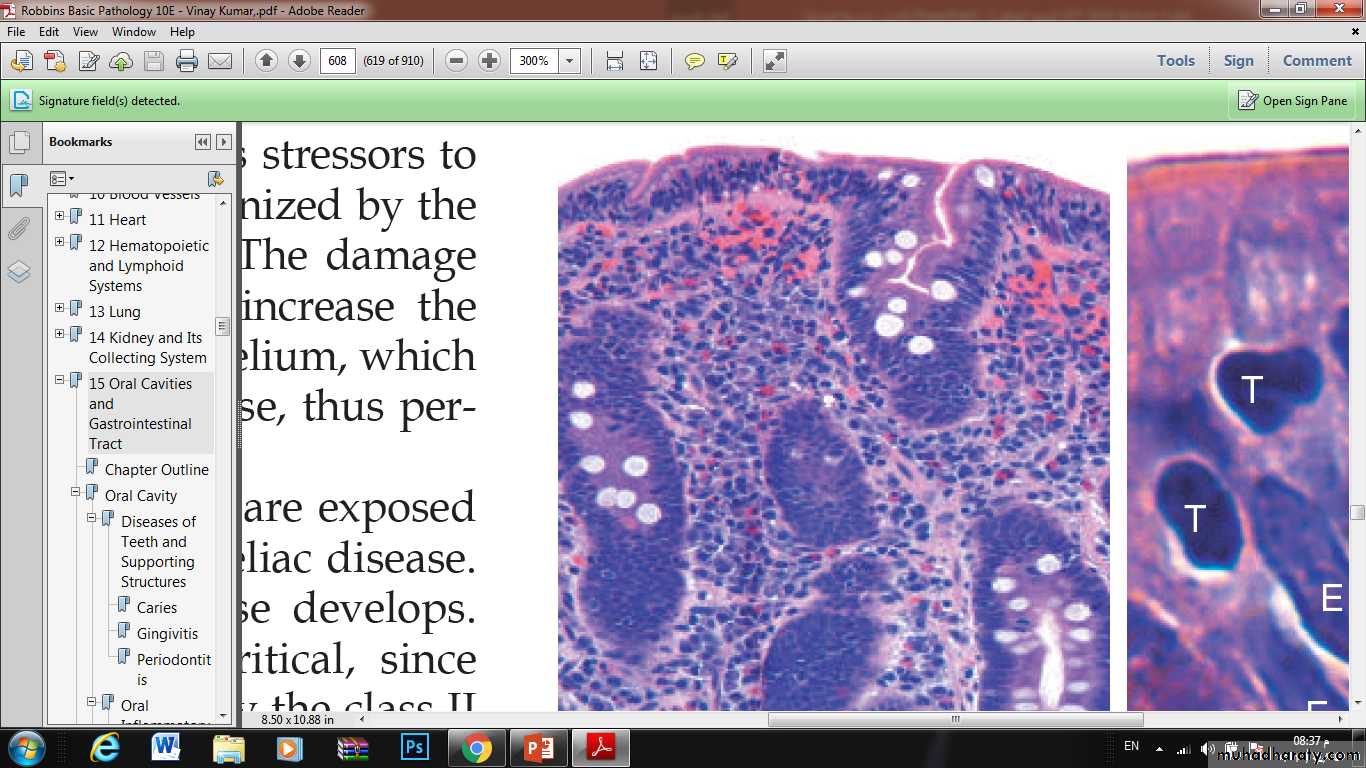
• Advanced cases of celiac disease show completeloss of villi, or total villous atrophy. Note the dense plasma cell infiltratesin the lamina propria.
Tropical sprue
◘ intestinal infection.◘ like ciliac disease in symptoms but occur almost exclusively in person living or visiting the tropic areas.
◘ no specific causal agent.
◘ injury present at all levels of the small intestine.
◘ there is a good response to AB therapy.
Idiopathic inflammatory bowel diseases
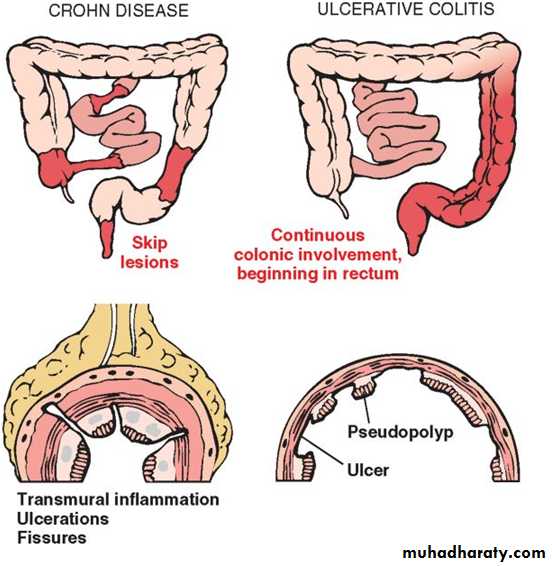
• Crohn's disease.• Ulcerative colitis.
Crohn's disease
It is systemic inflammatory disease with predominant GIT involvement.May affect any level of the GIT.
Active cases of CD are often accompanied by extraintestinal manifestations of immune origin. E.g.:Iritis uvitis, sacroilitis, migratory polyarthritis, erythema nodosum, sclerosing cholangitis.
epidemiology
Worldwide in distribution.Rare in Asia and Africa.
Common in US, Britain, Scandinavia.
It occurs at any age from young childhood to advanced age, peak incidence between 2nd-3rd decades of life.
Female slightly more than male.
Whites: nonwhites 2-5:1.
MORPHOLOGY
♦There is gross involvement of the small intestine alone in about 30% of Cases,
♦ of small intestine and colon in 40%,
♦ and of the colon alone in about 30%.
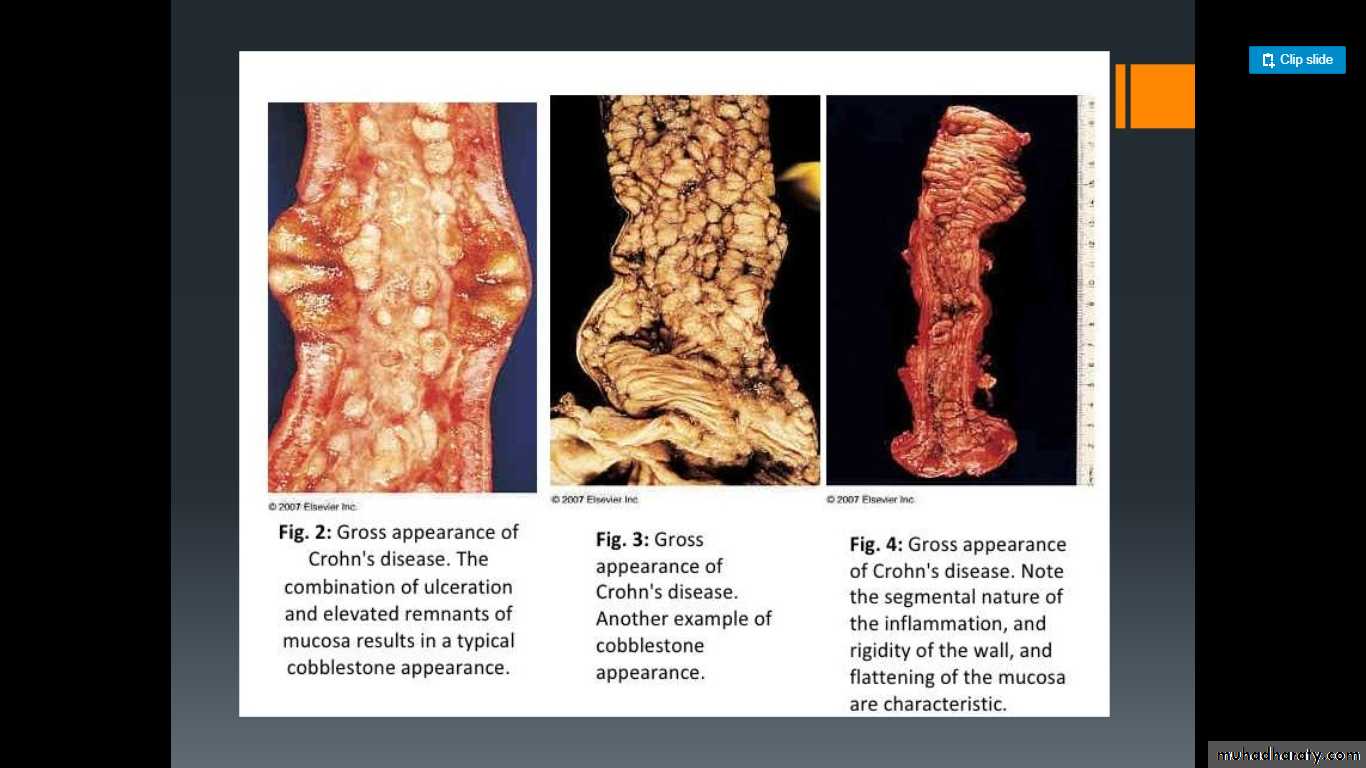
When fully developed, CD is characterized by:
(1) sharply delimited and typically transmural involvement of the bowel by an inflammatory process with mucosal damage,
(2) noncaseating granulomas in 35%
(3) fissuring with formation of fistulae.
4- A classic feature of CD is the sharp demarcation of diseased bowel segments from adjacent uninvolved bowel. When multiple bowel segments are involved, the intervening bowel is essentially normal (“skip” lesions).
In the intestinal mucosa
early disease exhibits: focal mucosal ulcers resembling canker sores (aphthaus ulcers), edema, and loss of the normal mucosal texture.
progressive disease, ulcers coalesce into long, serpentine linear ulcers, which tend to be oriented along the axis of the bowel, because the intervening mucosa tends to be relatively spared, it acquires a coarsely textured, cobblestone appearance.
long, serpentine linear ulcers, which tend to be oriented along the axis of the bowel, because the intervening mucosa tends to be relatively spared, it acquires a coarsely textured, cobblestone appearance.
By microscopic examination
the mucosa exhibits several characteristic features :(1) Inflammation, with neutrophilic infiltration into the epithelial layer and accumulation within crypts to form crypt abscesses;
(2) ulceration, which is the usual outcome of active disease
(3) chronic mucosal damage in the form of architectural distortion, atrophy, and metaplasia
(4)Granulomas may be present anywhere in the alimentary tract. However, the absence of granulomas does not preclude a diagnosis of CD.
(5)the muscularis mucosae and muscularis propria are usually markedly thickened, and fibrosis affects all tissue layers.
(6)Lymphoid aggregates scattered through the various tissue layers also are characteristic.
(7)Particularly important in patients with long-standing chronic disease are dysplastic changes appearing in the mucosal epithelial cells. These may be focal or widespread, tend to increase with time, and are thought to be related to a five-fold to six-fold increased risk of carcinoma, particularly of the colon.
Clinical Features
*recurrent episodes of diarrhea, crampy abdominal pain, and fever lasting days to weeks.Microscopic pathology of Crohn disease. (A) Haphazard crypt organization results from repeated injury and regeneration. (B) Noncaseating granuloma. (C) Transmural Crohn disease with submucosal and serosal granulomas (arrows).