Ulcerative Colitis
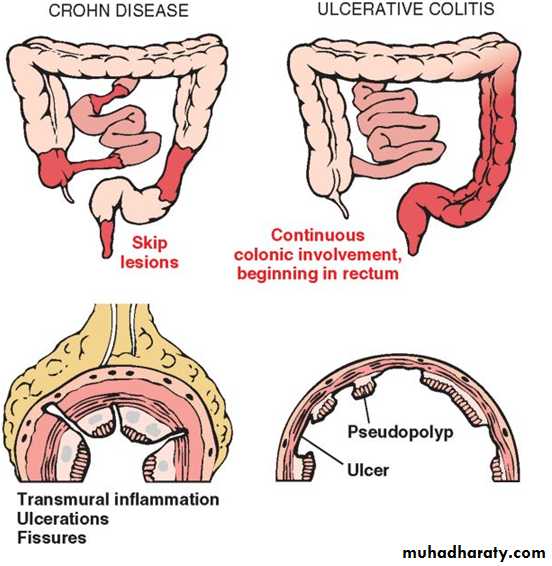
Ulcerative colitis (UC) is an ulceroinflammatory disease affecting the colonlimited to the mucosa and submucosa except in the most severe cases.
UC begins in the rectum and extends proximally in a continuous fashion, sometimes involving the entire colon.
Like CD, UC is a systemic disorder associated in some patients with migratory polyarthritis, sacroiliitis, ankylosing spondylitis, uveitis, erythema nodosum, and hepatic involvement (pericholangitis and primary sclerosing cholangitis).
There are several important differences between UC and CD:
• In UC, well-formed granulomas are absent. • UC does not exhibit skip lesions. • The mucosal ulcers in UC rarely extend below the submucosa,and there is surprisingly little fibrosis. • Mural thickening does not occur in UC.
the serosal surface is usually completely normal. • Patients with UC are at greater risk for carcinoma.
Epidemiology.
UC is more common than CD in the United States and Western countries, but it is infrequent in Asia, Africa, and South America.Incidence between ages 20 and 25 years.
MORPHOLOGY
Grossly:• always involves the rectum and extends proximally.
• Skip lesions are not seen .
• pancolitis , ulcerative proctitis or ulcerative proctosigmoiditis.
• The small intestine is normal, although mild mucosal inflammation of the distal ileum, backwash ileitis, may be present in severe cases of pancolitis.
Active disease :
inflammatory destruction of the mucosa, with macroscopic hyperemia, edema.With severely active disease:
there is extensive and broad-based ulceration of the mucosa in the distal colon or throughout its length . Isolated islands of regenerating mucosa bulge upward to create pseudopolyps.
However, inflammation and inflammatory mediators can damage the muscularis propria and disturb neuromuscular function leading to colonic dilation and toxic megacolon, which carries a significant risk of perforation.
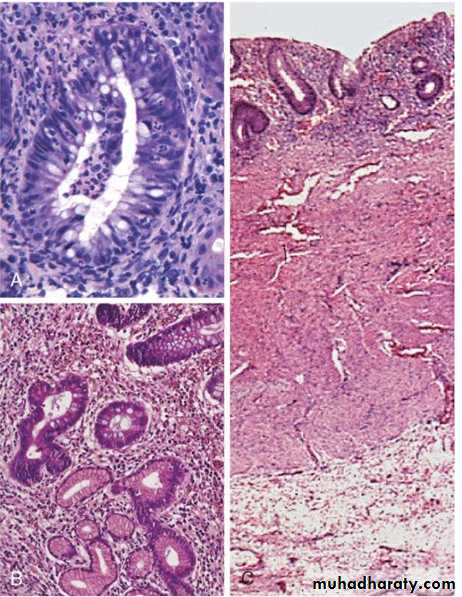
Microscopical features of UC
inflammatory infiltrates, crypt abscessesepithelial metaplasia
the inflammatory process is diffuse and generally limited to the mucosa and superficial submucosa
In severe cases, extensive mucosal destruction may be accompanied by ulcers that extend more deeply into the submucosa, but the muscularis propria is rarely involved.
Uncommon but life-threatening complications include:
* severe diarrhea and electrolyte derangements,*massive hemorrhage,
* severe colonic dilation (toxic megacolon) with potential rupture, and perforation with peritonitis.
*The most feared long-term complication of UC is cancer.
Clinical Features
UC is a chronic relapsing and remitting disorder marked by attacks of bloody mucoid diarrhea that may persist for days, weeks, or months and then subside, only to recur after an asymptomatic interval of months to years or even decades. Presentation is usually insidious, with cramps, tenesmus, and colicky lower abdominal pain. that is relieved by defecation.Feature
Crohn DiseaseUlcerative Colitis
MACROSCOPIC
Bowel region
Ileum ± colonColon only
Distribution
Skip lesions
Diffuse
Stricture
Yes
Rare
Wall appearance
Thick
Thin
MICROSCOPIC
Inflammation
Transmural
Limited to mucosa
Pseudopolyps
Moderate
Marked
Ulcers
Deep, knife-like
Superficial, broad-based
Lymphoid reaction
Marked
Moderate
Fibrosis
Marked
Mild to none
Serositis
MarkedMild to none
Granulomas
Yes (∼35%)
No
Fistulae/sinuses
Yes
No
CLINICAL
Perianal fistula
Yes (in colonic disease)
No
Fat/vitamin malabsorption
Yes
No
Malignant potential
With colonic involvement
Yes
Recurrence after surgery
Common
No
Toxic megacolon
No
Yes
COLONIC DIVERTICULOSIS
A diverticulum is a blind pouch leading off the alimentary tract,lined by mucosa, that communicates with the lumen of the gut.
Congenital diverticula have all three layers of the bowel wall (mucosa, submucosa, and most notably the muscularis propria) and are distinctly uncommon. The prototype is Meckel diverticulum, described earlier.
Acquired diverticula
lack or have an attenuated muscularis propria.It occurs at anywhere in the alimentary tract, but by far the most common location is the colon, giving rise to diverticular disease of the colon, also called diverticulosis.
PATHOGENESIS
consumption of a refined, low-fiber diet in Western societies, resulting in reduced stool bulk with increased difficulty in passage of intestinal contents.Exaggerated spastic contractions of the colon isolate segments of the colon (segmentation) in which the intraluminal pressure becomes markedly elevated, with consequent herniation of the bowel wall through the anatomic points of weakness.
TUMORS OF THE SMALL AND LARGE INTESTINES
The colon, including rectum, is host to more primary neoplasms than any organ in the body. Colorectal cancer ranks second to bronchogenic carcinoma among the cancer killers. Adenocarcinoma constitute the vast majority of colorectal cancers and represent 70% of all malignancies arising in the GIT.Terminology
A polyp is a tumorous mass that protrudes into the lumen of the gut;traction on the mass may create a stalked, or pedunculated, polyp.
the polyp may be sessile, without a definable stalk.
Polyps may be formed as the result of abnormal mucosal maturation, inflammation, or architecture. These polyps are non-neoplastic and do not have malignant potential; an example is the hyperplastic polyp
polyps that arise as the result of epithelial proliferation and dysplasia are termed adenomatous polyps or adenomas. They are true neoplastic lesions (“new growth”) and are precursors of carcinoma
Adenomas
Adenomas are neoplastic polyps that range from small, often pedunculated tumors to large lesions that are usually sessile.40% to 50% after age 60.
Males and females are affected equally.
There is a well- defined familial predisposition.
All adenomatous lesions arise as the result of epithelial proliferation and dysplasia, which may range from mild to so severe.
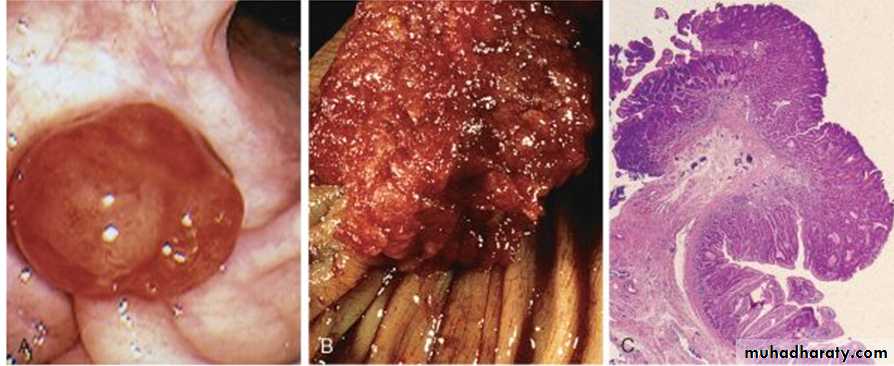
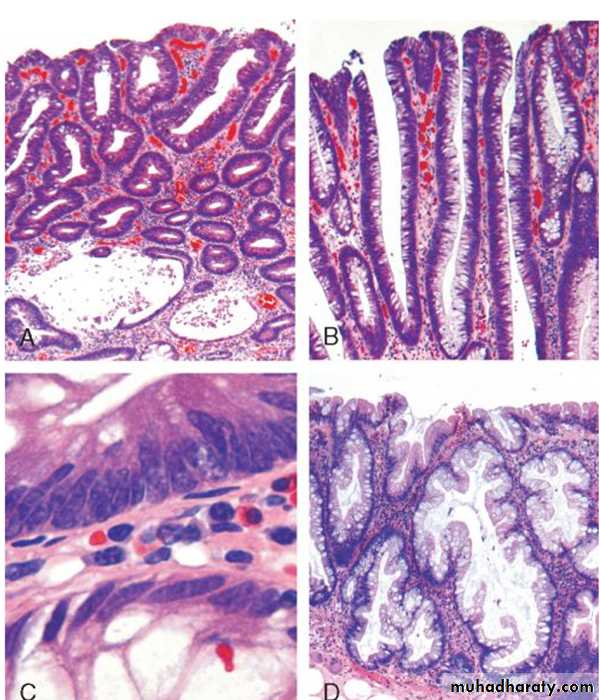
Adenomatous polyps are segregated into three subtypes on the basis of the epithelial architecture:
• Tubular adenomas: mostly tubular glands. • Villous adenomas: villous projections • Tubulovillous adenomas: a mixture of the above Tubular adenomas are by far the most common; 5% to 10% of adenomas are tubulovillous, and only 1% are villous.
The malignant risk with an adenomatous polyp is correlated with three interdependent features: polyp size, histologic architecture, and severity of epithelial dysplasia, as follows:
• Cancer is rare in tubular adenomas smaller than 1 cm in diameter.
• The likelihood of cancer is high (approaching 40%) in sessile villous adenomas more than 4 cm in diameter.
MORPHOLOGY
Tubular adenomasHistologically the stalk is covered by normal colonic mucosa
but the head is composed of neoplastic epithelium
all degrees of dysplasia may be encountered, ranging up to cancer confined to the mucosa (intramucosal carcinoma) or invasive carcinoma-like masses.
Villous adenomas
are larger and more ominous of the epithelial polyps.They tend to occur in older persons,
most commonly in the rectum and rectosigmoid.
They generally are sessile, up to 10 cm in diameter,
velvety or cauliflower extensions of the mucosa covered by dysplastic, columnar epithelium.
tubulovillous adenomos
are composed of a broad mix of tubular and villous areas.Colonic adenomas. A, Pedunculated adenoma (endoscopic view). B, Adenoma with a velvety surface. C, Low-magnification photomicrograph of a pedunculated tubular adenoma.
Histologic appearance of colonic adenomas. A, Tubular adenoma with a smooth surface and rounded glands.B, Villous adenoma with long, slender projections that are reminiscent of small intestinal villi. C, Dysplastic epithelial cells (top) with an increased nuclear-to-cytoplasmic ratio, hyperchromatic and elongated nuclei, and nuclear pseudostratification. Compare to the nondysplastic epithelium below.