Non-Hodgkin lymphoma
• Non-Hodgkin lymphoma (NHL) represents a
monoclonal proliferation of lymphoid cells of B cell
(70%) or T cell (30%) origin.
• The incidence of these tumours increases with age,
The current WHO classification stratifies according
to cell lineage (T or B cells) and incorporates clinical
features, histology, chromosomal abnormalities and
cell surface markers of the malignant cells.
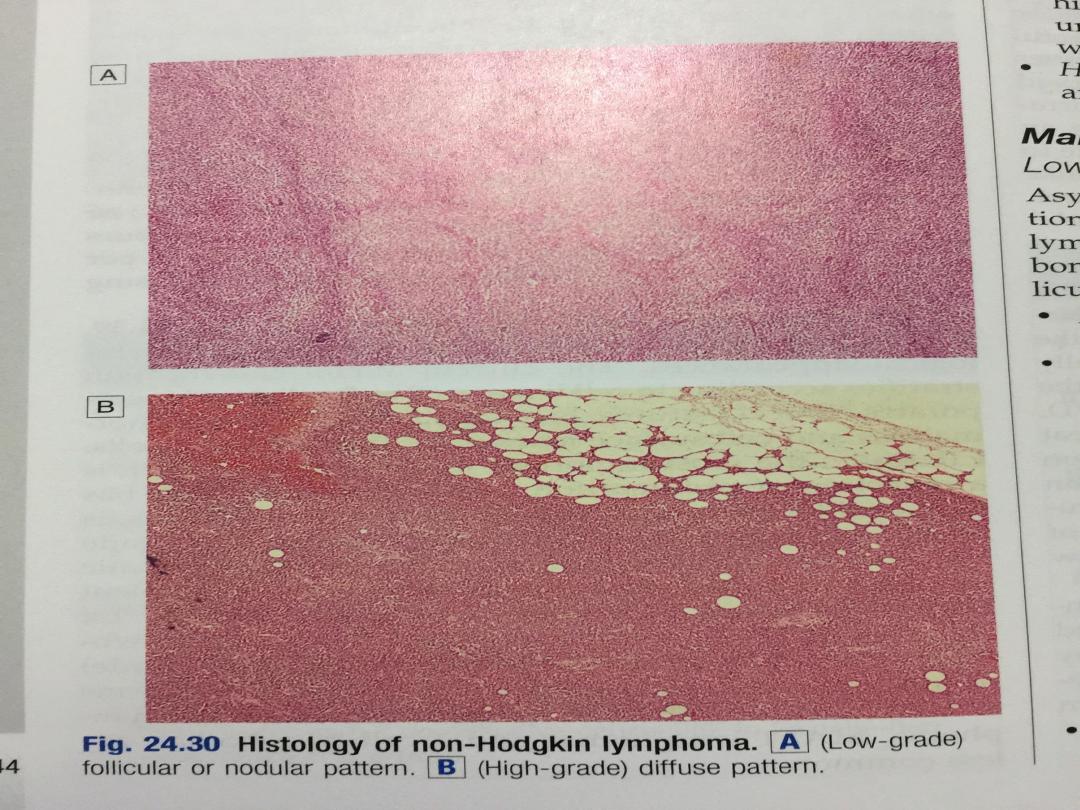
• Clinically, the most important factor is grade, which
is a reflection of proliferation rate. High-grade NHL
has high proliferation rates, rapidly produces
symptoms, is fatal if untreated, but is potentially
curable.

• Low-grade NHL has low proliferation rates, may
be asymptomatic for many months before
presentation, runs an indolent course, but is not
curable by conventional therapy.
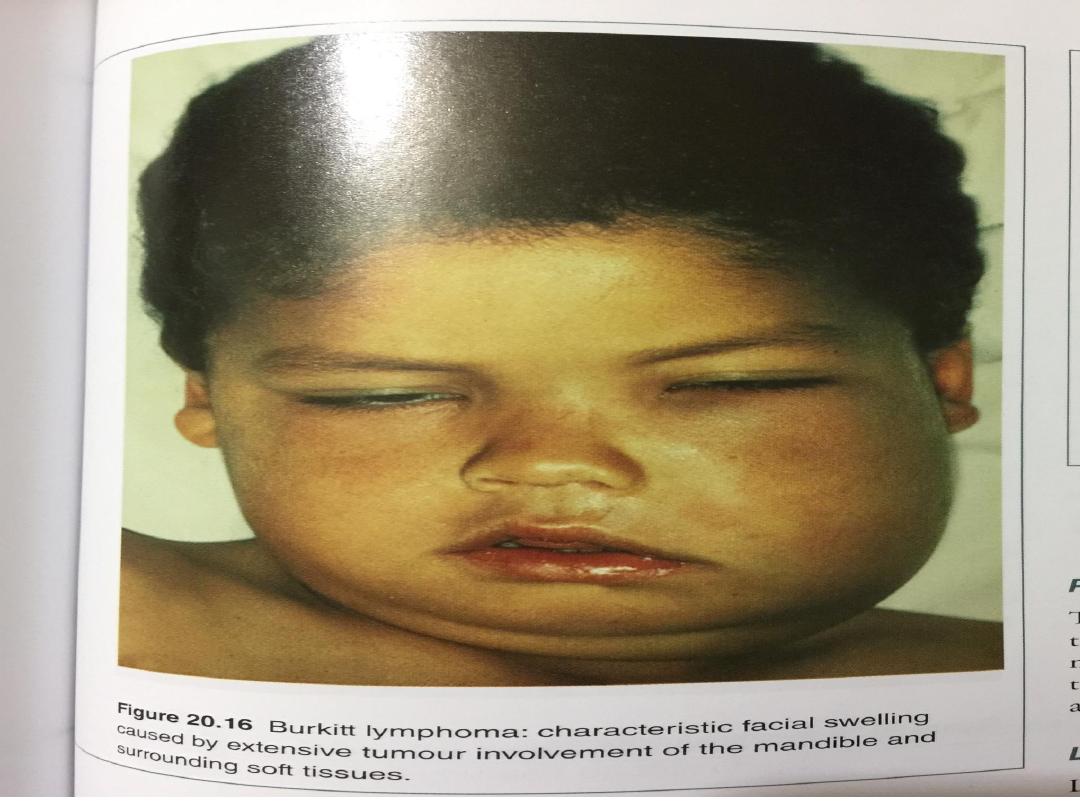
• Other forms of NHL, including Burkitt lymphoma,
mantle cell lymphoma, MALT lymphomas and T-
cell lymphomas, are less common.

• Of all cases of NHL in the developed world, over
twothirds are either diffuse large B-cell NHL (high-
grade) or follicular NHL (low-grade)
• Other forms of NHL, including Burkitt lymphoma,
mantle cell lymphoma, MALT lymphomas and T-cell
lymphomas, are less common.

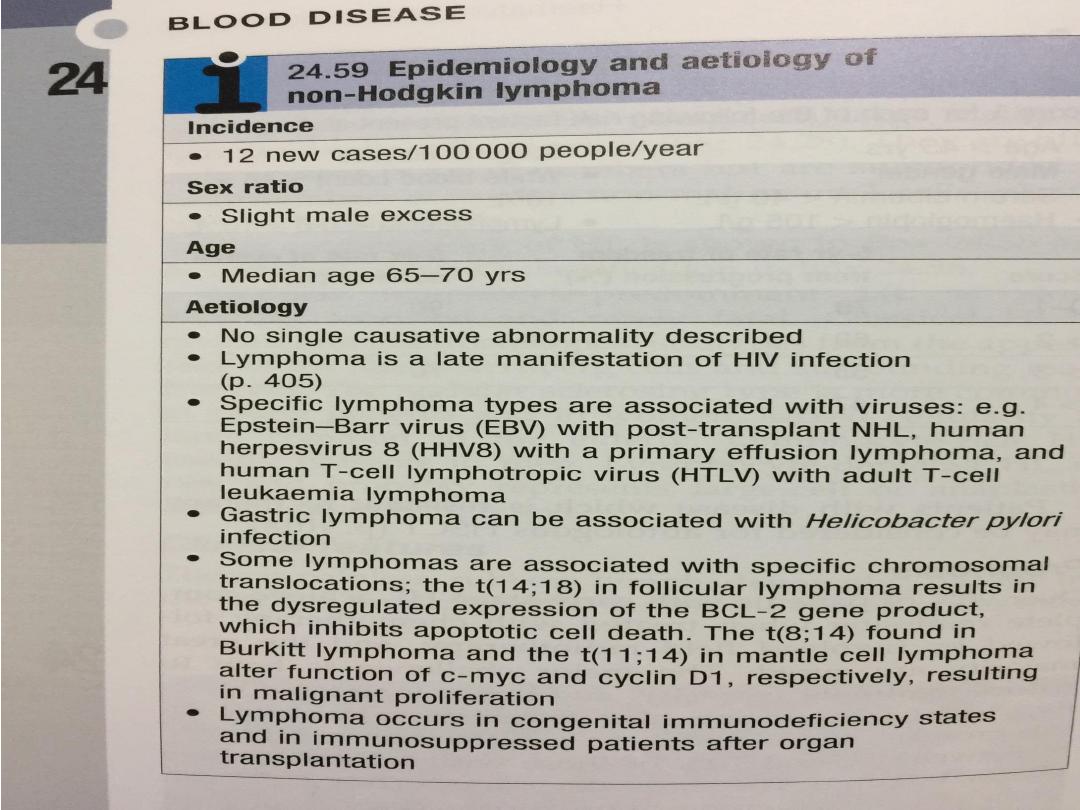
• Epidemiology of non-Hodgkin
lymphoma
• Incidence 12 new cases/100 000
people/year
• Sex ratio Slight male excess
• Age Median age 65–70 yrs

Aetiology
• No single causative abnormality described
• Lymphoma is a late manifestation of HIV infection
• Specific lymphoma types are associated with
viruses: e.g. Epstein–Barr virus (EBV) with post-
transplant NHL, human herpesvirus 8 (HHV8) with a
primary effusion lymphoma, and human T-cell
lymphotropic virus (HTLV) with adult T-cell
leukaemia lymphoma
• Gastric lymphoma can be associated with
Helicobacter pylori infection

• Some lymphomas are associated with specific
chromosomal translocations; the t(14;18) in
follicular lymphoma The t(8;14) found in Burkitt
lymphoma and the t(11;14) in mantle cell
lymphoma , resulting in malignant proliferation
• Lymphoma occurs in congenital immunodeficiency
states and in immunosuppressed patients after
organ transplantation

Clinical features
• Unlike Hodgkin lymphoma, NHL is often widely
disseminated at presentation, including in
extranodal sites.
• Patients present with lymph node enlargement,
which may be associated with systemic upset:
weight loss, sweats, fever and itching.
Hepatosplenomegaly may be present
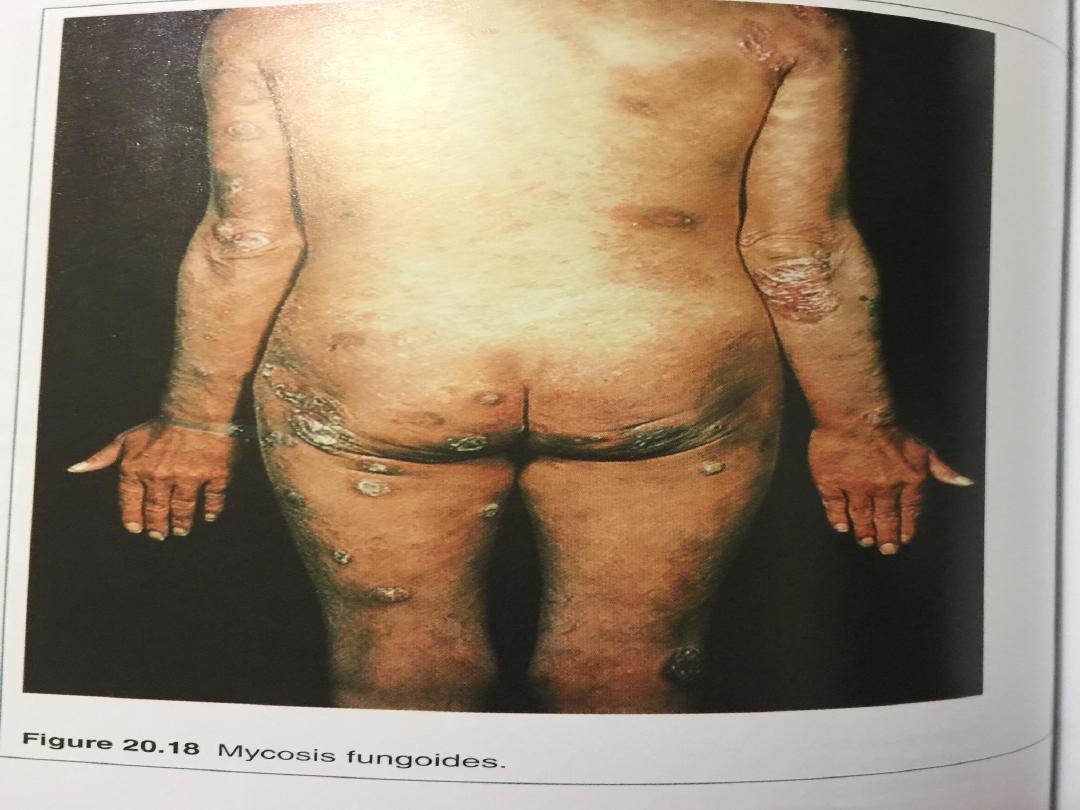
• Sites of extranodal involvement include the bone
marrow, gut, thyroid, lung, skin, testis, brain and,
more rarely, bone.
• Bone marrow involvement is more common in low-
grade (50–60%) than high-grade (10%) disease.

• Compression syndromes may occur, including gut
obstruction, ascites, superior vena cava obstruction
and spinal cord compression
• The same staging system is used for both HL and
NHL, but NHL is more likely to be stage III or IV at
presentation.

Investigations
• These are as for HL, but in addition the following
should be performed:
•
Bone marrow aspiration and trephine
.
• Immunophenotyping of surface antigens to distinguish
T from B cell tumours. This may be done on blood,
marrow or nodal material.
• Cytogenetic analysis to detect chromosomal
translocations and molecular testing for T cell receptor
immunoglobulin gene rearrangements, if available
• Immunoglobulin determination. Some lymphomas are
associated with IgG or IgM paraproteins, which serve as
markers for treatment response.

•
Measurement of uric acid levels
. Some very
aggressive high-grade NHLs are associated with very
high urate levels, which can precipitate renal failure
when treatment is started.
• HIV testing. This may be appropriate if risk factors
are present

Management

Low-grade NHL
• Asymptomatic patients may not require therapy.
Indications for treatment include marked systemic
symptoms, lymphadenopathy causing discomfort or
disfigurement, bone marrow failure or compression
syndromes.
• In follicular lymphoma, the options are:
• Radiotherapy. This can be used for localised stage I
disease, which is rare.
• Chemotherapy. Most patients will respond to oral
therapy with chlorambucil, which is well tolerated
but not curative.

• Transplantation. Particular interest centres on the
role of high-dose chemotherapy and HSCT in
patients with relapsed disease.

High-grade NHL
•
Patients with diffuse large B-cell NHL need treatment at
initial presentation
•
Chemotherapy. The majority (> 90%) are treated with
intravenous combination chemotherapy, typically with the
CHOP regimen (cyclophosphamide, doxorubicin, vincristine
and prednisolone).
•
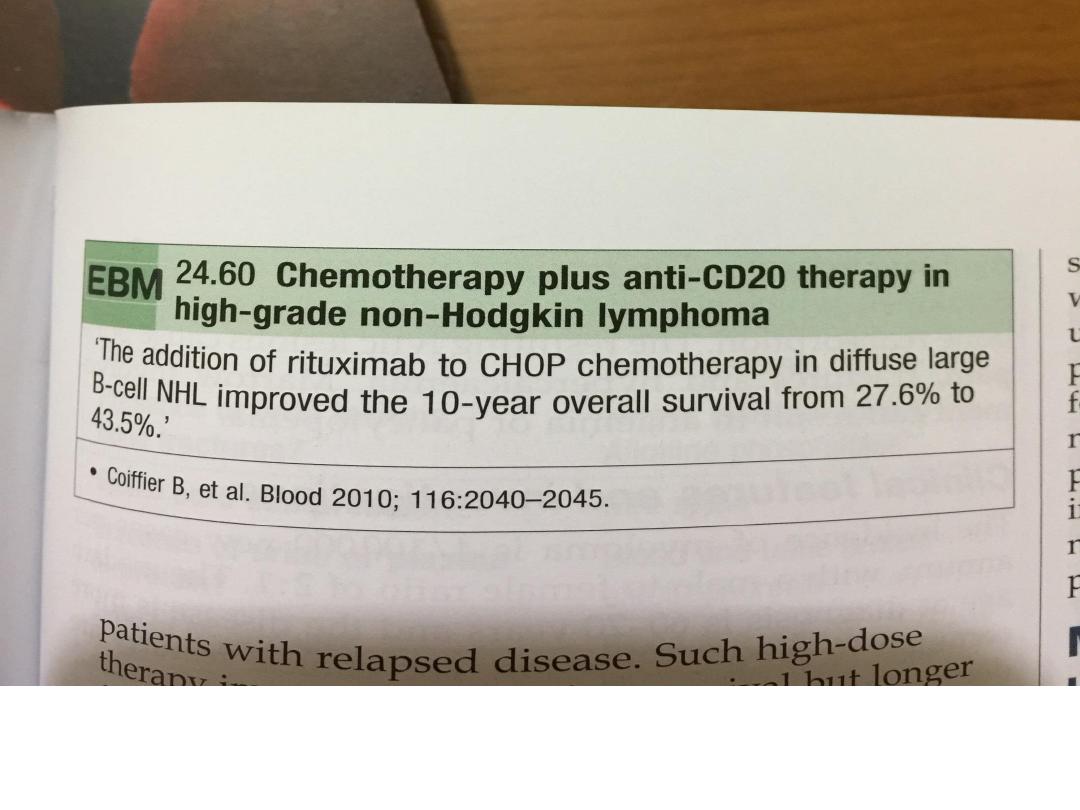
When combined with CHOP chemotherapy,
•
the biological therapy rituximab (R) increases the complete
response rates and improves overall survival.
•
R-CHOP is currently recommended as first-line therapy for
those with stage II or greater diffuse large B-cell lymphoma
•
Radiotherapy. A few stage I patients without bulky disease
may be suitable for radiotherapy

• Radiotherapy is also indicated for a residual
localised site of bulk disease after chemotherapy,
and for spinal cord and other compression
syndromes.
• HSCT. Autologous HSCT benefits patients with
relapsed chemosensitive disease

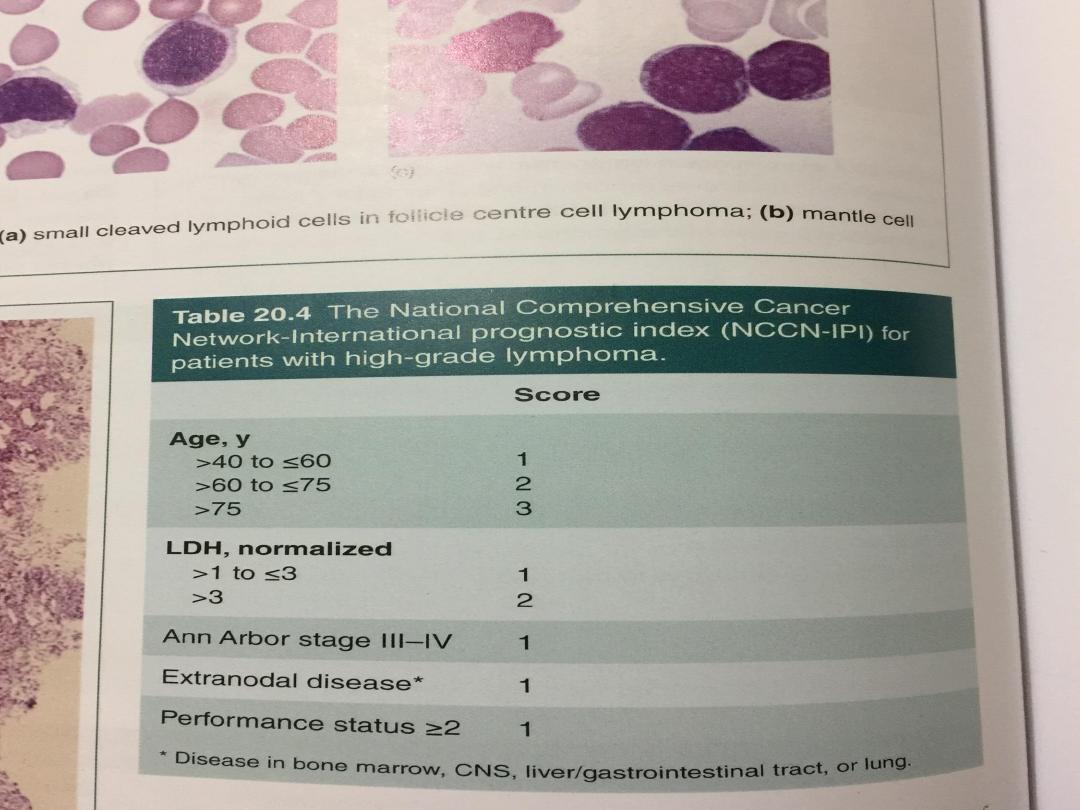
Prognosis
• Low-grade NHL runs an indolent remitting and
relapsing course, with an overall median survival of 10
years.
• Transformation to a high-grade NHL occurs in 3% per
annum and is associated with poor survival
• In diffuse large B-cell high-grade NHL treated with R-
CHOP, some 75% of patients overall respond initially to
therapy and 50% will have disease-free survival at 5
years.
• For high-grade NHL, 5-year survival ranges from 75% in
those with low-risk scores (age < 60 years, stage I or II,
one or fewer extranodal sites, normal LDH and good
performance status)

• to 25% in those with high-risk scores (increasing
age, advanced stage, concomitant disease and a
raised LDH).
• Relapse is associated with a poor response to
further chemotherapy (< 10% 5-year survival), but
in patients under 65 years, HSCT improves survival