1
ADRENAL GLAND
The adrenal gland is divided into two embryological and functionally
distinct parts.
Adrenal cortex is part of hypothalamic – pituitary – adrenal endocrine
system
It consists of 3 layers
Outer thin layer zona glomerulosa secret aldosterone
Inner layers zona fasciculata
Form functional unit and secret most of
adrenocortical hormones
Zona reticularis
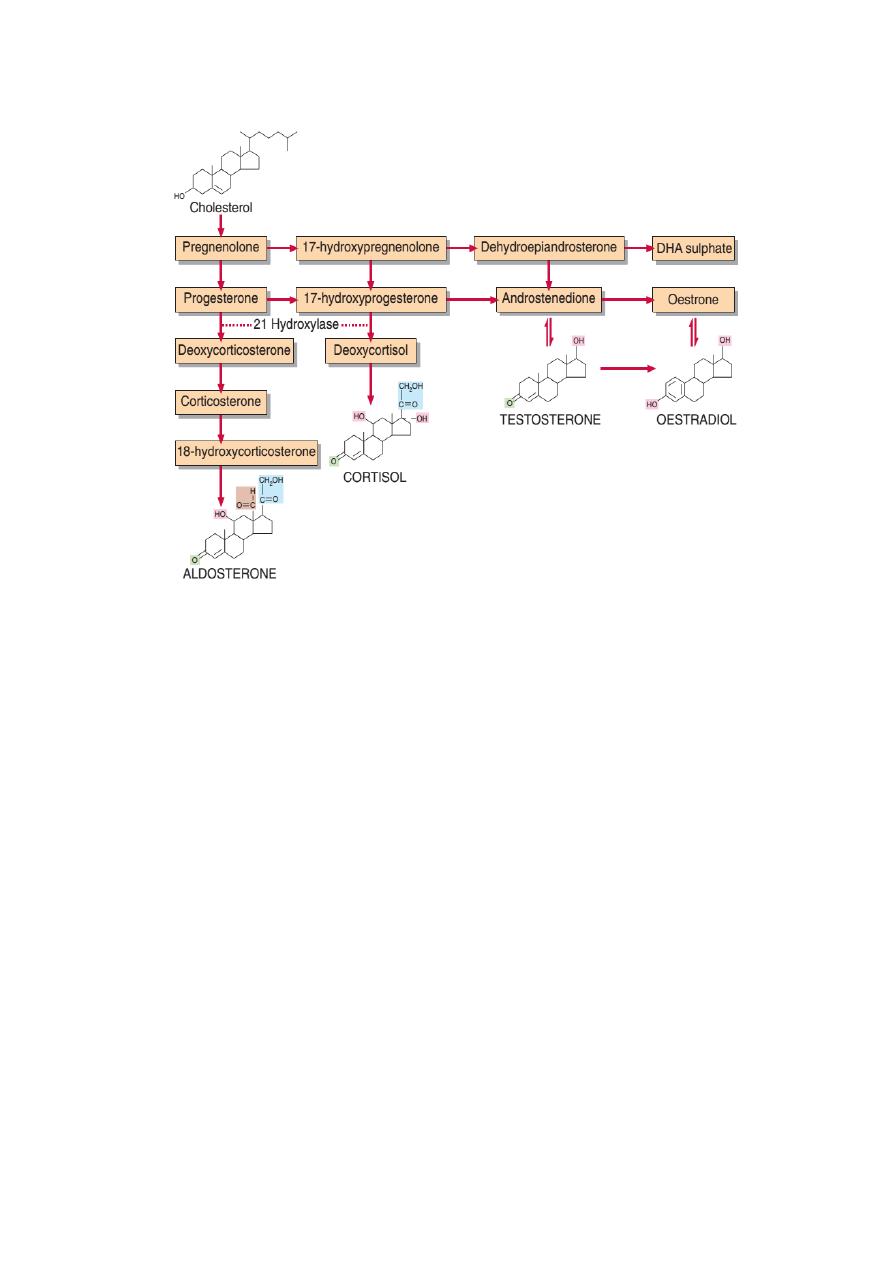
Biosynthesis
The steroid hormones derived from lipid cholesterol
It consists of 27 carbon atom. The side chain on C17 is the main
determinant of type of hormonal activity. Substitutions in other positions
modify the activity within particular group
The first product is pregnenolone. Several synthetic pathways diverge
from it.
The
Zona Glomerulosa
secretes aldosterone, produced by 18-
hydroxylation
Control: renin – Angiotensin System Not ACTH,
Zona Fasiculata and Zona reticularis
Cortisol ,
a glucocorticoid formed by progressive addition of hydroxyl
group at C17, C21 and C11
Androgens
formed by removal of side chain and formation of C19
steriods.
2
Glucocorticoids
Cortisol and corticosterone are naturally occurring Circulate bound to
cortisol binding globulin and albumin, 5% unbound and physiological
active .
Inactivated in the liver by conjugation with glucoronate and sulphate in
liver and excreted in urine.
Effect of glucocorticoids :-
1- Effect on intermediary metabolism :-
a. Increase glucose production by increase gluconeogenesis.
b. Increase hepatic glycogen deposition by promoting the
activation of glycogen synthase.
c. Promote lipolysis (in extremities) but can cause lipogenesis
in other sites (face & trunk) especially at higher than
physiologic levels.
d. Promote protein and RNA metabolism.
2- Effect on host metabolism:-
a. Suppress the immune response.
b. Suppress the inflammatory response.
3-
Other effects :-
a. Necessary for maintenance of normal blood pressure and
cardiac output.
b. Required for maintenance of normal water and electrolyte
balance.
c. Necessary with the hormones of the adrenal medulla in
allowing the organism to respond to stress.
Mineralocorticoids
The most active member of these hormones is aldosterone. is induced by
a decrease in the plasma Na
+
/K
+
ratio, and by the hormone, angiotensin
II. Stimulate the exchange of sodium for potassium and hydrogen ions
across the cell membranes and its renal action important in sodium and
water homeostasis
.

3
Mechanism of action:
1. When the body is subjected to hypotension, any combination of
factors that decreases fluid volume (dehydration, decreased blood
pressure, fluid or blood loss) or decreases NaCl concentration
stimulates renin release from the kidney.
2.
Renin
acts upon the substrate angiotensinogen to produce the
decapeptide angiotensin I. Angiotensin-converting enzyme, a
glycoprotein found in lung, endothelial cells, and plasma, convert
angiotensin I to form angiotensin II.
3. Angiotensin
II
increases
blood
pressure
by
causing
vasoconstriction of the arteriole and is a very potent vasoactive
substance. It inhibits renin release from the juxtaglomerular cells
and is a potent stimulator of aldosterone production. This results in
Na+ retention, volume expansion, increased blood pressure , and
K
+
excretion.
Andrenal androgens
Dehydroepiandrosterone (DHEA) and its sulphate (DHEAS) and
androstenedione .
Promote protein synthesis and week androgenic at physiological
concentration .
Bound to sex hormone binding globulin and albumin
.
4
Synthesis of Steroids Hormones
inherent rhythms and stress
ACTH secreted episodically each pulse being followed 5 -10 min later by
cortisol secretion the most frequent secretion happen in morning and least
before sleep.
Plasma cortisol usually Highest 07:00 – 9:00 am
Lowest 23:00 pm
The high concentration of cortisol at any time of day suppress ACTH
secretion Loss of circadian rhythm is one earliest feature of Cushing
syndrome.
Stress whether physical or mental may override the control mechanism
and cause sustained secretion of ACTH.

5
Congenital adrenal hyperplasia (CAH)
CAH is the result of an inherited enzyme defect in corticosteroid
biosynthesis. The adrenals cannot secrete cortisol and electrolyte
disturbances may involve severe hyponatraemia and hyperkalaemia if
aldosterone biosynthesis is also affected. because of the lack of cortisol,
negative feedback to the pituitary is absent and ACTH secretion
continues to drive steroid biosynthesis.
The 21-hydroxylase is the deficient enzyme in 95% of cases of CAH.
Here, large amounts of 17-hydroxyprogesterone are secreted.
Adrenocortical Hyperfunction
This include overproduction of the three main product
Cortisol
Adrenal Androgens
Aldosterone
Cortisol excess
Prolonged exposure of body tissues to cortisol or other glucocorticoids
gives rise to the clinical features that collectively are known as
Cushing’s
syndrome
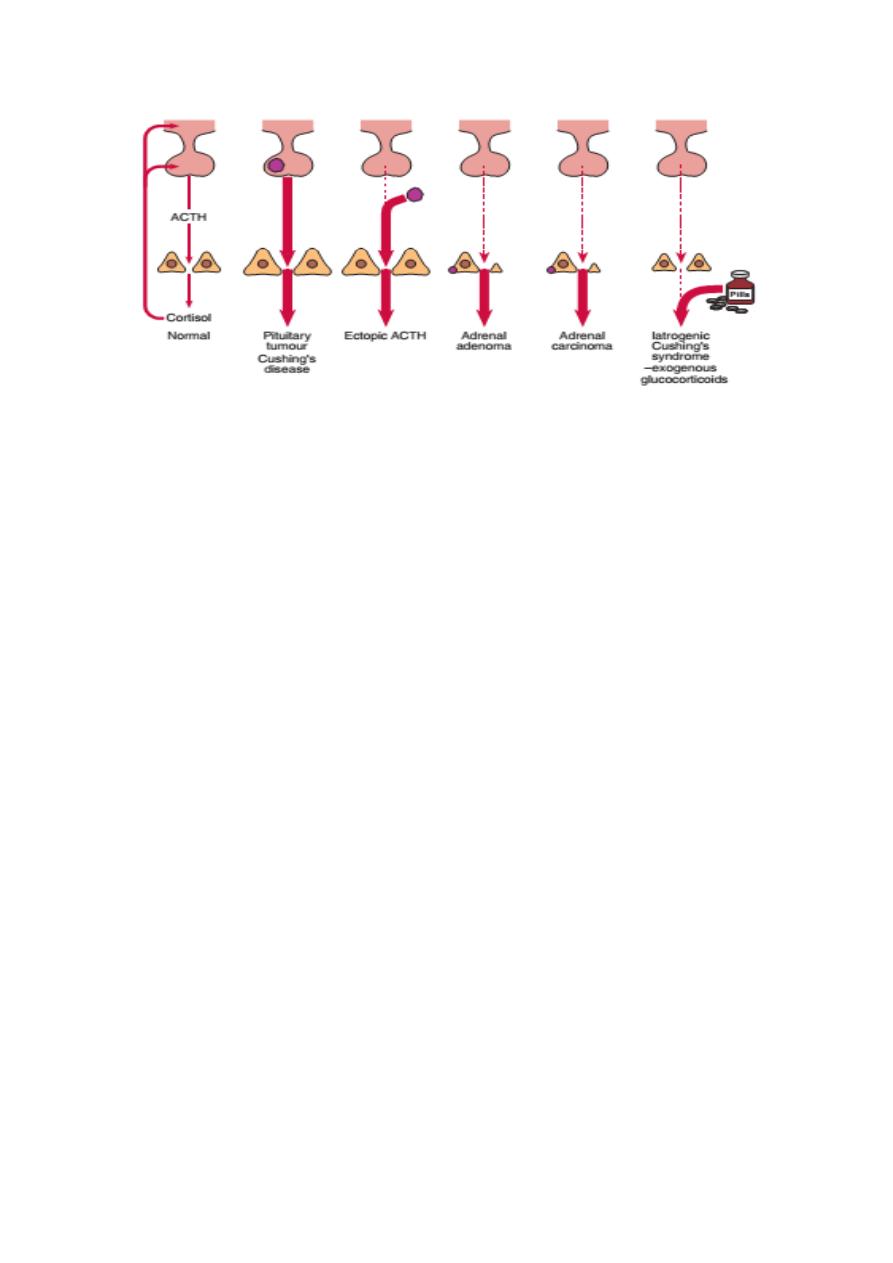
Causes
Iatrogenic steroid medications.
Tumour that secrete either cortisol or ACTH.
Cushing’s disease
It is associated with bilateral adrenal hyperplasia,
often secondary to a basophil adenoma of the anterior pituitary gland.
Ectopic ACTH secretion
in this condition, usually from a small-cell
carcinoma of the bronchus, ACTH concentrations may be high enough to
cause skin pigmentation.
6
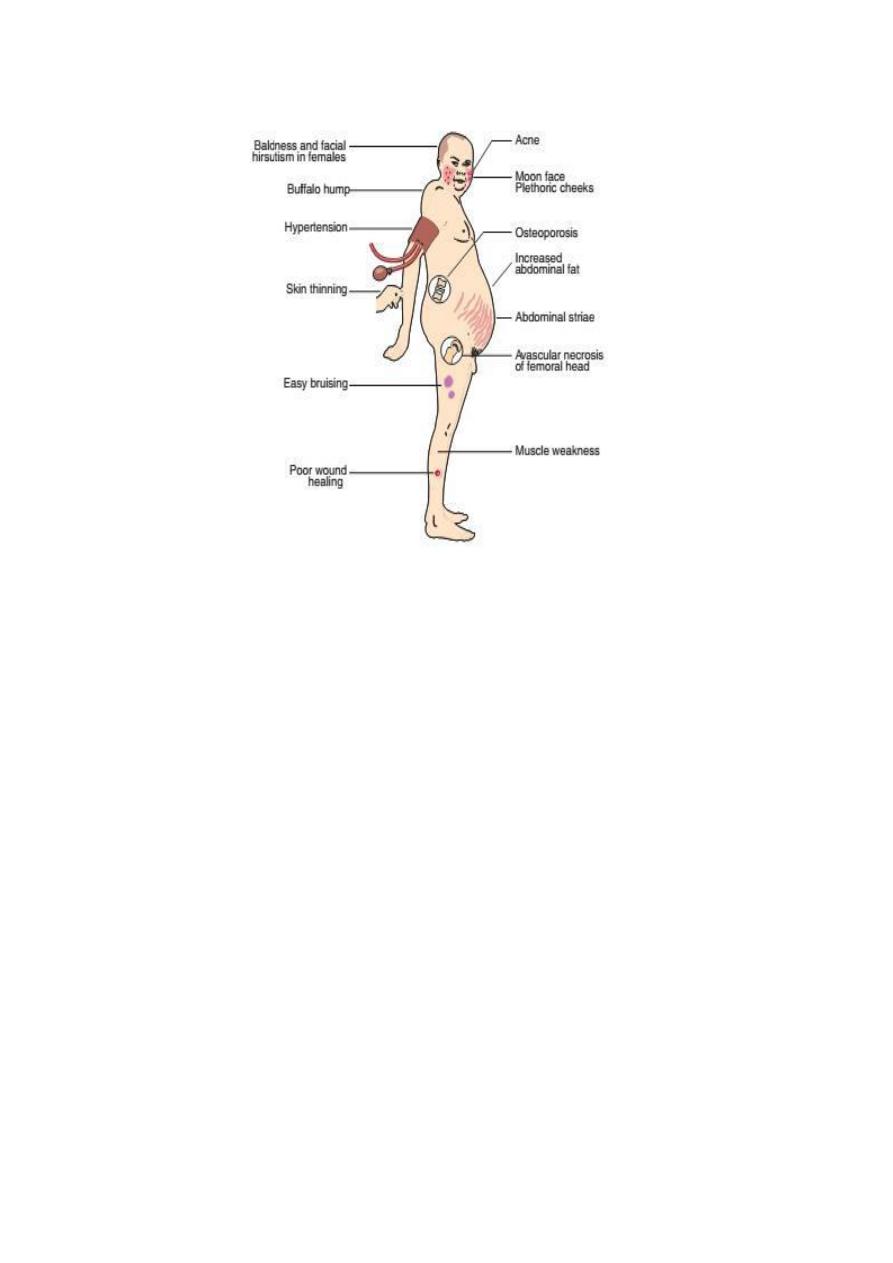
Clinical Features of Cushing syndrome
The clinical and metabolic features may include the following:
Obesity
, typically involving the trunk and face, and a characteristic
round, red ‘cushingoid’ face
Impaired glucose tolerance and hyperglycaemia. Cortisol has the
opposite
action
to
that
of
insulin,
causing
increased
gluconeogenesis, and some patients may have diabetes mellitus.
Increased protein catabolism, which also increases urinary protein
loss. Thus, there is a negative nitrogen balance associated with
proximal muscle wasting with weakness, thinning of the skin and
osteoporosis. The tendency to bruising and the purple striae (most
obvious on the abdominal wall) are probably due to this thinning.
Hypertension, caused by urinary retention of sodium and therefore
of water, which are due to the mineralocorticoid effect of cortisol.
Increased urinary potassium loss may cause hypokalaemia.

7
Androgen excess, which may account for the common findings of
greasy skin with acne vulgaris and hirsutism, and menstrual
disturbances in women.
Psychiatric disturbances, such as depression
.
Investigation of Cushing syndrome
The following questions should be asked
● Is there abnormal cortisol secretion?
● If so, does the patient have any other condition that may cause it?
● If Cushing’s syndrome is confirmed, what is the cause?
Is there abnormal cortisol secretion?
One of the earliest features of Cushing’s syndrome is the loss of the
diurnal variation in cortisol secretion, with high concentrations in the late
evening
Estimation of 24-h urinary free cortisol
Increase level of urinary cortisol
Low-dose overnight dexamethasone suppression test
A small dose, for example 1 mg, of this synthetic steroid inhibits ACTH,
and thereby cortisol secretion by negative feedback. This is usually given
at midnight and blood is taken for cortisol assay at 09.00 h the following
morning.
Failure of suppression is sensitive test but not specific
.
Is there another cause for the abnormal cortisol secretion?
Stress
over-rides the other mechanisms controlling ACTH secretion,
Endogenous depression
may be associated with sustained high plasma
cortisol and ACTH concentrations that may not be suppressed even by a
high dose of dexamethasone.
Severe alcohol abuse
can cause hypersecretion of cortisol that mimics
Cushing’s syndrome clinically and biochemically.
8
possible causes of Cushing syndrome
What is the cause of Cushing’s syndrome?
pituitary adenoma .
ectopic ACTH .
adrenal adenoma .
adrenal carcinoma.
Adrenal hypofunction
Acute adrenal insufficiency is a rare condition that if unrecognized is
potentially fatal. Most of the time is overlooked. Treatment is simple
once diagnosis made
Causes
1. The main cause is autoimmune destruction of primary adrenal
failure.
2. Tuberculosis is also cause of adrenal destruction in endemic area .
3. Secondary adrenal failure is more common due long standing
suppression and subsequent impairment of the hypothalamic –
9
pituitary adrenal axis from therapeutic administration of
corticosteroid.
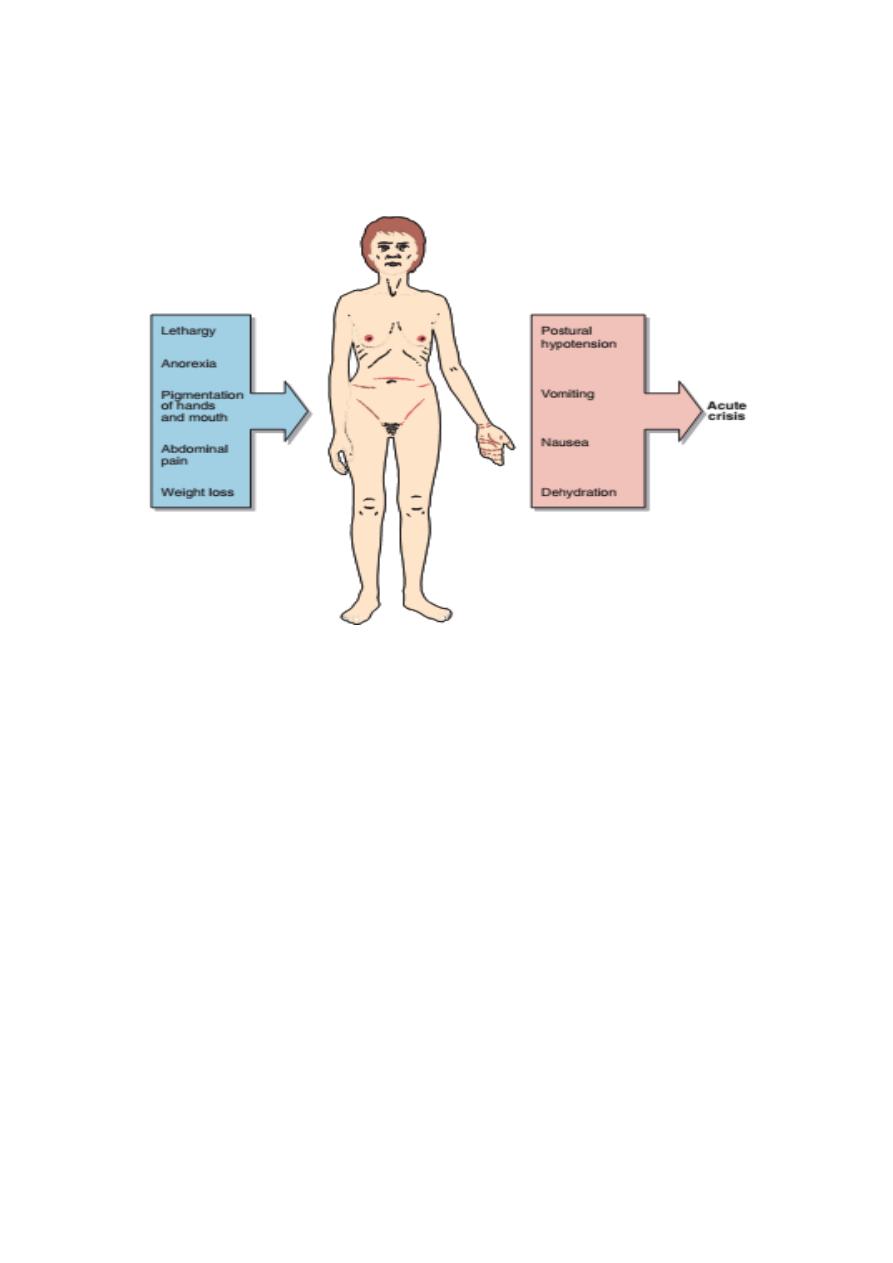
Clinical features of adrenal hypofunction
Biochemical features
Hyponatraemia
The lack of aldosterone leads to pathological sodium loss by the kidney
that results in a contraction of the extracellular fluid volume
In the absence of cortisol, the kidneys’ ability to excrete a water load is
impaired,thus exacerbating hyponatraemia.
Hyperkalemia
darkening of the skin and mucous membranes.

10
Lack of negative feedback of cortisol on the anterior pituitary results in
an excessive secretion of ACTH. The structure of this hormone contains
part of the amino acid sequence of melanocyte stimulating hormone.
1. Excessive mineralocorticoid secretion:-
a. primary hyperaldosteronism ( Conn ̓s syndrome):-
Which is due to small adenoma of the glomerulosa cells. The
classic manifestations are hypertension, hypokalemia, hypernatremia and
alkalosis.
b- Secondary hyperaldosteronism :- Which occur in :-
1- Liver Cirrhosis.
2- Severe cardiac failure.
3- Renal artery stenosis.
4- Nephrotic syndrome.
** Insufficiency of the adrenal cortex:-
1- Primary adrenal insufficiency (Addisson ̓s disease):-
Which is due to acquired disease of the adrenal cortex . It is
characterized by:-
a- Low blood pressure. b- Decreased GFR.
c- Decreased ability to excrete a water load
d- Low plasma Na levels and K levels are high.
c- Increased pigmentation of skin and mucous membranes.
