Hodgkin lymphoma

Hodgkin lymphoma
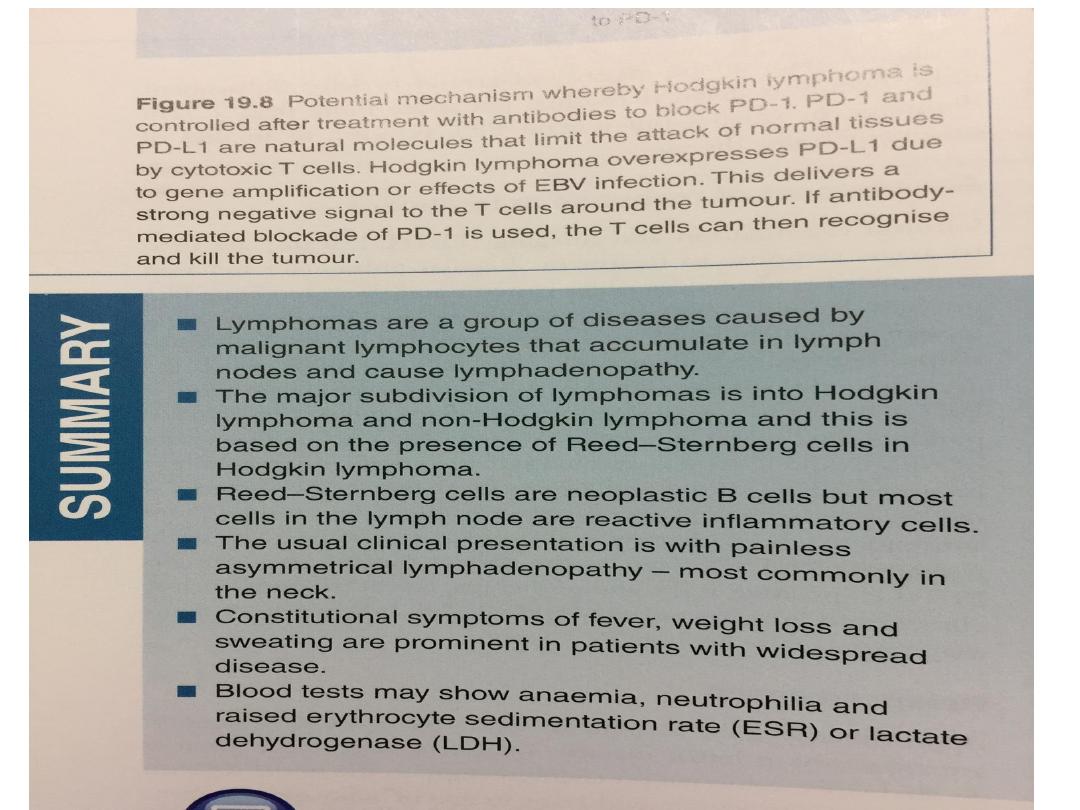
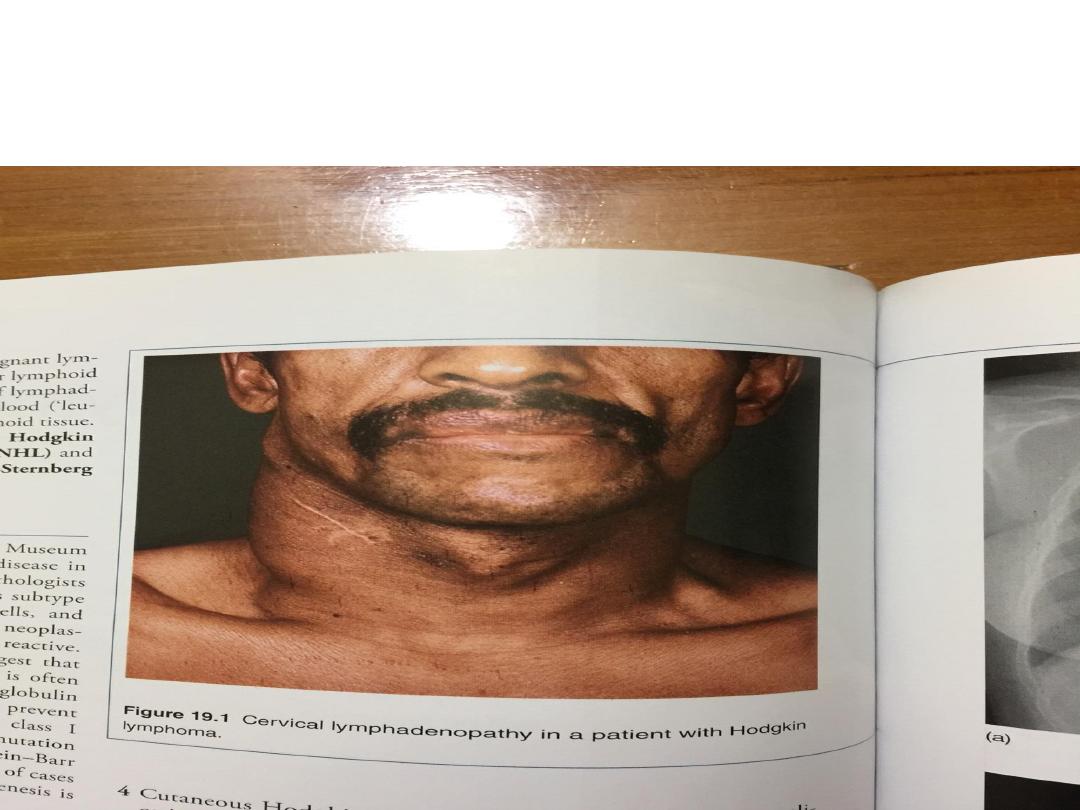
• The histological hallmark of Hodgkin lymphoma (HL) is
the presence of Reed–Sternberg cells, large malignant
lymphoid cells of B cell origin
• WHO pathological classification of Hodgkin lymphoma
Nodular lymphocytepredominant HL 5%
Classical HL
Nodular sclerosing 70%
Mixed cellularity 20%
Lymphocyte-rich 5%
Lymphocyte-depleted Rare

• Nodular lymphocyte-predominant HL is
slowgrowing, localised and rarely fatal..
• Classical HL is divided into four histological subtypes
from the appearance of the Reed–Sternberg cells
and surrounding reactive cells
• The nodular sclerosing type is more common in
young patients and in women.
• Mixed cellularity is more common in the elderly.
• Lymphocyte-rich HL usually presents in men.
• Lymphocyte-depleted HL is rare and probably
represents large-cell or anaplastic non-Hodgkin
lymphoma.

• Epidemiology and aetiology of Hodgkin lymphoma
• Slight male excess (1.5 : 1)
• Median age 31 yrs; first peak at 20–35 yrs and second
at 50–70 yrs
Aetiology
• Unknown
• More common in patients from well-educated
backgrounds and small families
• Three times more likely with a past history of infectious
mononucleosis but no definitive causal link to Epstein–
Barr virus infection is proven
•

Clinical features
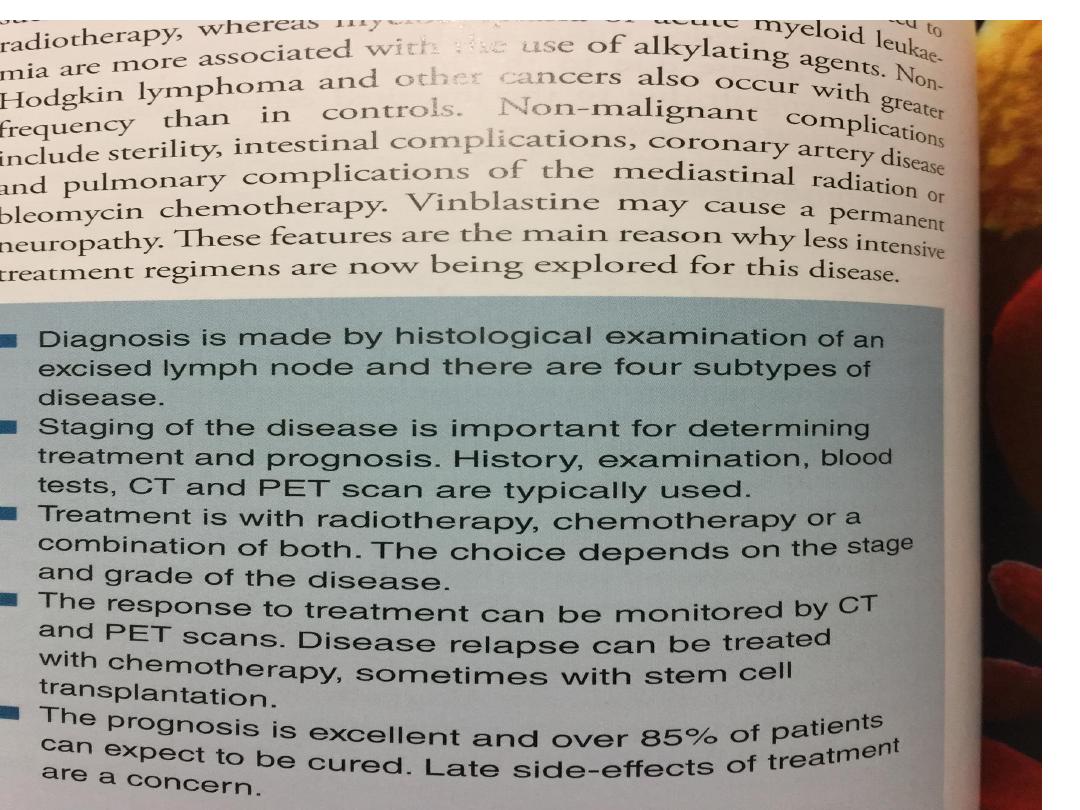
• There is painless, rubbery lymphadenopathy, usually in
the neck or supraclavicular fossae; the lymph nodes
may fluctuate in size.
• Young patients with nodular sclerosing disease may
have large mediastinal masses which are surprisingly
asymptomatic but may cause dry cough and some
breathlessness.
• Hepatosplenomegaly may be present but does not
always indicate disease in those organs. Spread is
contiguous from one node to the next and extranodal
disease, such as bone, brain or skin involvement, is
rare.

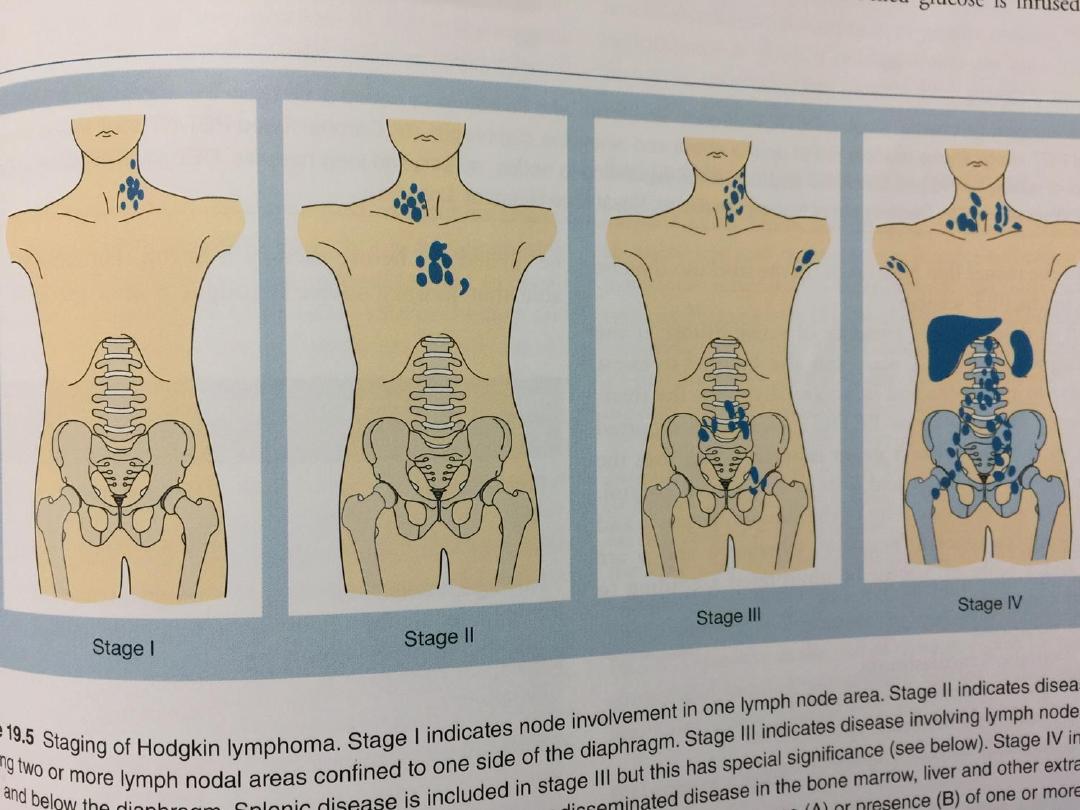
Clinical stages of Hodgkin lymphoma (Ann Arbor
classification)
Stage I: Involvement of a single lymph node region (I) or
extralymphatic site (IE)
Stage II: Involvement of two or more lymph node regions
(II) or an extralymphatic site and lymph node regions on
the same side of (above or below) the diaphragm (IIE)
Stage III :Involvement of lymph node regions on both
sides of the diaphragm with (IIIE) or without (III) localized
extralymphatic involvement or involvement of the spleen
(IIIs), or both (IIISE)
Stage IV: Diffuse involvement of one or more
extralymphatic tissues, e.g. liver or bone marrow
• Each stage is subclassified:
A No systemic symptoms
B Weight loss > 10%, drenching sweats, fever

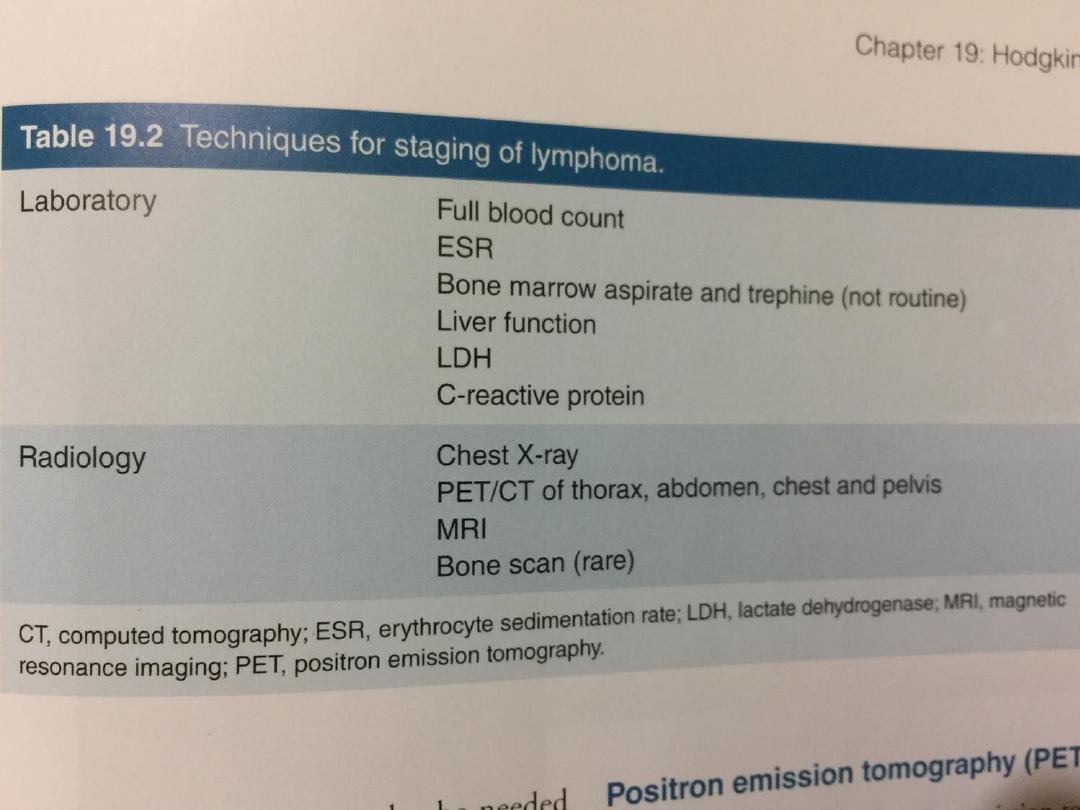
Investigations
• Treatment of HL depends upon the stage at presentation;
therefore investigations aim not only to diagnose
lymphoma but also to determine the extent of disease
• FBC may be normal. If a normochromic, normocytic
anaemia or lymphopenia is present, this is a poor
prognostic factor. An eosinophilia or a neutrophilia may be
present.
• ESR may be raised.
• Renal function tests are required to ensure function is
normal prior to treatment.
• Liver function may be abnormal in the absence of disease
or may reflect hepatic infiltration. An obstructive pattern
may be caused by nodes at the porta hepatis.

• LDH measurements showing raised levels are an
adverse prognostic factor.
• Chest X-ray may show a mediastinal mass.
• CT scan of chest, abdomen and pelvis permits
staging. Bulky disease (> 10 cm in a single node
mass) is an adverse prognostic feature.
• Lymph node biopsy may be undertaken surgically or
by percutaneous needle biopsy under radiological
guidance

Management
• Historically, radiotherapy to lymph nodes alone has been used
to treat localised stage IA or stage IIA disease effectively, with
no adverse prognostic features.
• Fertility is usually preserved after radiotherapy. Young women
receiving breast irradiation during the treatment of chest
disease have an increased risk of breast cancer and should
participate in a screening programme.
• Patients continuing to smoke after lung irradiation are at
particular risk of lung cancer.
• The majority of HL patients are now treated with chemotherapy
and adjunctive radiotherapy. The ABVD regimen (doxorubicin,
vinblastine, bleomycin and dacarbazine) is widely used.
• Patients with advanced-stage disease are most commonly
managed with chemotherapy alone. Patients with disease which
is resistant to therapy may be considered for autologous HSCT

Prognosis
• Over 90% of patients with early-stage HL achieve
complete remission when treated with
chemotherapy followed by involved field
radiotherapy, and the great majority are cured.
• Between 50 and 70% of those with advanced-stage
HL can be cured.